Abstract
Poverty alleviation remains an urgent issue in China’s rural areas, with health poverty being a critical dimension. This study analyzed the multidimensional health poverty status of 9,052 rural residents in Ningxia in 2019 and 7,910 in 2022, aiming to provide a reference for optimizing health poverty alleviation strategies. The A-F dual cutoff method was used to identify and measure multidimensional health poverty through dimensions such as health status, health service utilization capacity poverty, and health spending and security poverty. Logistic regression analysis was further applied to examine the influencing factors of multidimensional health poverty. The results indicate that when the k-value is set at 0.3, the incidence of multidimensional health poverty was 22.3% in 2019 and 7.7% in 2022. The corresponding multidimensional health poverty indices were 0.091 and 0.028, respectively. Furthermore, the level of multidimensional health poverty was higher among women than men. Chronic diseases were identified as a significant indicator of multidimensional health poverty. At the individual level, gender, age, education, government subsidies, family size, housing, and digital divide significantly effected health poverty. Although multidimensional health poverty has improved in rural northwest China, targeted measures remain essential, especially for rural women, individuals with chronic illnesses, and those facing challenges in accessing healthcare and digital connectivity. Sustainable multidimensional health poverty alleviation should prioritize remote rural areas, especially by enhancing healthcare resource utilization for rural women and individuals with chronic diseases. Additionally, increasing medical subsidies for marginalized groups is essential. Improving rural housing conditions, strengthening digital infrastructure, and raising digital health literacy are also critical steps.
Similar content being viewed by others
Introduction
Poverty is a widespread economic issue. Reducing poverty has become a key goal for countries around the world. China, with its large population, has made substantial efforts to address this challenge. By the end of 2020, China announced the elimination of both absolute and regional poverty according to its current criteria. However, does this mean that absolute poverty has been completely eradicated? Regrettably, the answer is no. The eradication of absolute poverty shall not entail the utter vanishing of impoverished individuals, and the predicament of relative indigence will endure for a protracted duration1. Over time, poverty has evolved from a narrow focus on income deprivation during the initial phases of economic growth to a more all-encompassing state influenced by various multidimensional factors such as economics, healthcare, and education2.
Notably, health-related poverty stands out as a significant contributor to poverty in rural China3. Poverty caused by health factors is manifested not only in direct out-of-pocket impoverishment, but more importantly in the deprivation of residents’ ability to function by disease, leading to a reduction in individuals’ ability to earn income, thereby further forming a vicious cycle between health and poverty4. According to the “Tracking Universal Health Coverage: 2017 Global Monitoring Report” released by the World Health Organization, there are currently 100 million people in the world driven into poverty by diseases5. During the period from 1998 to 2016, the percentage of destitute households in China caused by ailments surged from 15.19% to a staggering 44.00%6. Research indicates that households with hospitalized, elderly, or chronically ill individuals, as well as those dwelling in rural or impoverished regions, are more susceptible to incurring exorbitant health expenses7. Significant factors inducing a return to poverty due to illness among rural inhabitants include exorbitant health expenses and inadequate utilization of healthcare services8.
Most studies currently measure health poverty from the perspective of the economic burden of disease, often using indicators such as catastrophic health expenditure or impoverishing health expenditure. Some researchers assess health poverty based on health shocks, physical functioning, and social support, but these measures tend to be relatively simple, with no established standards4,9. The indicators commonly used are basic physiological metrics, such as self-rated health, mortality, and life expectancy4,10,11. However, this approach overlooks multidimensional factors, such as the capacity to utilize healthcare services and access to health security12. The identification of health poverty through the lens of absolute poverty lines or catastrophic health expenditures, while seemingly comprehensive, neglects those who suffer from poor health and low income but have not experienced catastrophic health expenses13. It is precisely this faction of the rural populace that exists precariously on the cusp of impoverishment, susceptible to being plunged into poverty by ailments, catastrophes, and other perils6,14.
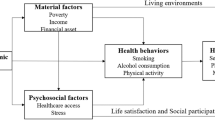
Amartya Sen’s capability poverty theory suggests that material poverty alone does not adequately explain the phenomenon of poverty; rather, it is the deprivation of essential capabilities that fundamentally causes poverty15. According to this theory, poverty arises when individuals lack the capability to improve themselves, manage risks, or participate in economic activities to secure benefits. These “capabilities” evolve with social and economic progress, with a focus on the erosion or loss of basic capacities. Therefore, this study draws on the capability poverty theory to comprehensively assess health poverty. Health poverty encompasses not only severe financial hardship caused by health issues but also the adverse cascading effects of economic deprivation, opportunity loss, impaired capabilities, insufficient security, and a lack of basic health assets8,15. By identifying key health-related functions and capabilities, this research quantifies individuals’ deprivation across these dimensions to construct a multidimensional health poverty index(MHPI). This index provides a more comprehensive reflection of individual health poverty status and serves as a theoretical foundation for designing more targeted health poverty alleviation strategies.
The state of health indigence and the outcomes and advancement of health poverty alleviation interventions in frontier regions, mountainous areas and ethnic minority inhabited districts call for special scrutiny7,16,17. Taking the Ningxia Hui Autonomous Region in China as an example, this area has complex terrain, limited resources, and is a national poverty alleviation priority18. Before the complete eradication of poverty, a substantial proportion of Ningxia’s population remained impoverished, with illness being a primary cause or trigger of poverty19. Trends in rural health service utilization in Ningxia from 2009 to 2019 show some progress in accessibility and equity, yet financial hardship continues to be the main barrier to healthcare access20,21. This study applies the MHPI to identify and measure the health poverty status of rural Ningxia residents, analyze its determinants, and provide a scientific basis for more targeted health poverty alleviation strategies.
This study applies Sen’s capability approach to health poverty assessment in rural China from a multidimensional and relative perspective. By constructing a MHPI, it provides a more comprehensive and detailed framework for identifying and measuring health poverty. This approach complements existing research on multidimensional health poverty assessment. Furthermore, the in-depth analysis of Ningxia offers regional insights into health poverty issues in impoverished areas of China and globally, carrying significant theoretical and practical implications for shaping and implementing health poverty alleviation policies.
Methods
Data source and sampling method
The data for this study were obtained from the “Innovative Payment System to Enhance Health Benefits” project, a collaboration between the Health Commission of Ningxia Hui Autonomous Region and Harvard University, utilizing unbalanced panel data from 2019 to 2022. To ensure accuracy, we conducted logical error corrections on the database and removed any samples with significant missing or ambiguous variable data, resulting in a final sample of 9,052 rural residents in 2019 and 7,910 rural residents in 2022.
We employed a multi-stage stratified random sampling method across four counties in Ningxia: Haiyuan, Yanchi, Xiji, and Pengyang. Within these sample counties, all administrative villages in each township were classified into three levels based on economic development: high, medium, and low. Using a random number table, we selected 40% of the villages as sample villages, comprising 76 administrative villages from Haiyuan, 40 from Yanchi, 20 from Pengyang, and 59 from Xiji. Systematic sampling was conducted based on the household registration list of each village, with 20 to 33 households selected as survey samples from each village. The participants were permanent residents (those residing in the area for more than six months). The questionnaires were administered through face-to-face interviews conducted by trained teachers and graduate students. Our survey addressed key determinants relevant to our research, including demographic and household characteristics, consumption habits, health status, and utilization of health services.
The sample size calculation formula for counting data in descriptive research is \(n = \frac{{\mathop \mu \nolimits_{{\alpha /2}}^{2} \pi (1 - \pi )}}{{\mathop \sigma \nolimits^{2} }}.\) The significance test level α = 0.05 is usually adopted, and the allowable error δ = 0.1 π is general. The incidence of health poverty in rural residents was 7.78%, means π = 7.78%. Thus, the sample size needed was calculated to be about 2747 people. The subjects included in this study meet the requirements of sample size.
Research Method
Construction of multidimensional health poverty index for rural residents
Within the realm of multidimensional poverty and health poverty research, the Dual-Cutoff Method22 coined by Alkire and Foster in 2011 has become widely adopted within academic circles for identifying impoverished populations23,24. we can proceed towards constructing a comprehensive index for multidimensional health poverty by employing the A-F Dual-Cutoff Method. The process of formulating this index can be segmented into three distinct steps: identification, measurement and decomposition22.
-
(1)
Identification of multidimensional healthy poverty
Suppose there are N samples of residents in a rural area, and each sample is assessed by D indicators for its multidimensional health poverty level. Let \(Y_{{N \times D}}\) denote the matrix formed by all sample values, and let \(y_{{ij}} \in Y_{{N \times D}}\) denote the value of rural resident i on dimension j (i = 1, 2, L, N; j = 1, 2, L, D).
First, set a poverty standard for each dimension \(Z_{j}\). If \(y_{{ij}} < Z_{j}\), then rural resident i is poor in dimension j; Otherwise, there is no poverty. To facilitate the calculation, make \(g_{{ij}}^{0} = \left\{ {\begin{array}{*{20}l} {1,} \hfill & {y_{{ij}} < {\text{z}}_{j} } \hfill \\ {0,} \hfill & {{\text{other}}} \hfill \\ \end{array} } \right.\), So the sample matrix \(g^{0} = \left[ {g_{{ij}}^{0} } \right]\) can be transformed into a deprivation matrix. In addition, the deprivation matrix g0 can be compensated by the normalized gap deprivation matrix \(g^{0} = \left[ {g_{{ij}}^{1} } \right]\), \(g_{{ij}}^{1} = g_{{ij}}^{0} \frac{{z_{j} - y_{{ij}} }}{{z_{j} }}\). Secondly, the dimension equal weight method was used to determine the weight wj of each index, and the total deprivation score of rural residents i in all dimensions was calculated, \(c_{i} = \sum\nolimits_{{j - 1}}^{D} {w_{j} g_{{ij}}^{\alpha } }\). Finally, a critical value k is set to determine whether rural residents are multidimensional healthy poor. If \(c_{j} \ge k\), the rural resident is in multidimensional healthy poverty; Otherwise, it is not multidimensional healthy poverty. Further, let \(c_{i} (k) = \left\{ {\begin{array}{*{20}l} {c_{i} ,} \hfill & {c_{i} \ge k} \hfill \\ {0,} \hfill & {{\text{other}}} \hfill \\ \end{array} } \right.\), the deprivation matrix g0 can then be transformed into a censoring deprivation matrix \(g^{\alpha } (k) = \left[ {g_{{ij}}^{\alpha } (k)} \right]\) and \(g_{{ij}}^{\alpha } (k) = g_{{ij}}^{\alpha } c_{i} (k)\).
-
(2)
Calculation of the MHPI
On the bedrock of identifying multidimensional health poverty among rural denizens, we have erected a composite index that appraises this very phenomenon. The calculated indicators include the following:
Incidence of multidimensional health poverty (H): Represents the rate of multidimensional healthy poverty in the population. Calculation formula is \(H = \sum\nolimits_{{i = 1}}^{N} {c_{i} (k)} /N = q/N\). Where, q is the number of people with multidimensional healthy poverty and N is the total sample number.
MHPI: Also known as the adjusted incidence of multidimensional health poverty, its formula is \(MHP_{0} = HA = {{{{\left| {g^{0} (k)} \right|} \mathord{\left/ {\vphantom {{\left| {g^{0} (k)} \right|} {q = \sum\nolimits_{{j = 1}}^{D} {\sum\nolimits_{{i = 1}}^{N} {g_{{ij}}^{0} (k)} } }}} \right. \kern-\nulldelimiterspace} {q = \sum\nolimits_{{j = 1}}^{D} {\sum\nolimits_{{i = 1}}^{N} {g_{{ij}}^{0} (k)} } }}} \mathord{\left/ {\vphantom {{{{\left| {g^{0} (k)} \right|} \mathord{\left/ {\vphantom {{\left| {g^{0} (k)} \right|} {q = \sum\nolimits_{{j = 1}}^{D} {\sum\nolimits_{{i = 1}}^{N} {g_{{ij}}^{0} (k)} } }}} \right. \kern-\nulldelimiterspace} {q = \sum\nolimits_{{j = 1}}^{D} {\sum\nolimits_{{i = 1}}^{N} {g_{{ij}}^{0} (k)} } }}} N}} \right. \kern-\nulldelimiterspace} N}\), Where A is the average missing share, and represents the ratio of the dimension of deprivation of rural residents to the number of people in multidimensional health poverty. A indicates the depth of multidimensional health poverty, also known as the poverty occurrence intensity index.
-
(3)
Calculation of the contribution rates of dimensions and indicators of the MHPI
To gauge the extent to which various dimensions and indicators contribute towards the overarching MHPI composite index, and to subsequently identify the primary factors underlying MHPI, it is imperative to deconstruct the MHPI composite index by its constituent dimensions and indicators. The MHPI decomposition formula for this study is as follows: Let MHPαj be the multidimensional health poverty contribution rate of dimension j, then \(MHP_{{\alpha j}} = {{\left( {q_{j}^{\alpha } \times w_{j} } \right)} \mathord{\left/ {\vphantom {{\left( {q_{j}^{\alpha } \times w_{j} } \right)} N}} \right. \kern-\nulldelimiterspace} N}\). \(q_{j}^{\alpha }\) is the multidimensional poverty incidence of dimension j in the case of multidimensional poverty, and wj is the weight of each index. Then the contribution of dimension j to the multidimensional poverty index wj is
\(\varphi _{j}^{\alpha } = {{MHP_{{\alpha j}} } \mathord{\left/ {\vphantom {{MHP_{{\alpha j}} } {MHP_{\alpha } }}} \right. \kern-\nulldelimiterspace} {MHP_{\alpha } }} = {{\left( {q_{j}^{\alpha } \times w_{j} } \right)} \mathord{\left/ {\vphantom {{\left( {q_{j}^{\alpha } \times w_{j} } \right)} {(N \times MHP_{\alpha } )}}} \right. \kern-\nulldelimiterspace} {(N \times MHP_{\alpha } )}},\alpha = 0,1,2\)
The aforementioned identification, quantification, and deconstruction procedures constitute the entire process for computing the MHPI. Figure 1 provides a more visually evocative representation of the identification and quantification of multidimensional health poverty.
Determination of dimensions, indicators and weights of multidimensional health poverty
Based on the characteristic factors of multidimensional healthy poverty, this study has devised a MHPI and constructed a system of identifying multidimensional health poverty through three core dimensions: “health status - ability to use health services - health expenditure and security”, which encompasses twelve sub-indicators. Drawing on prior approaches to multidimensional poverty and health poverty measurement22,23, we utilized an equal weighting approach (dimensional equal weighting) for analysis. Table 1 provides a detailed account of the dimensions, indicators, weights, and deprivation thresholds.
Due to the large number of indicators involved in this study, the variance inflation factor (VIF) was used to test the multicollinearity of variables in the multidimensionally healthy poverty system. Table 2 shows that VIF values range from 1.001 to 1.233, and the average VIF is 1.090. All VIF values are lower than 525. These results show that there is no significant collinearity between the variables.
Model construction and variable selection of determinants of multidimensional health poverty
Further analysis is imperative to delve into the underlying causes and effective mitigation strategies of the ostensibly salubrious poverty predicament afflicting rural denizens. Considering the aforementioned issues, a logistic regression model has been devised to scrutinize the determinants that effect the multidimensional health poverty among rural inhabitants in Ningxia.
Given the contemporaneity of the data, solely the data pertaining to the year 2022 have been culled for analysis in this section. The variable settings of the regression model and the description of the general characteristics of the sample are shown in Table 3. Multidimensional health poverty and one-dimensional health poverty (health status poverty, health service utilization poverty and health expenditure and security poverty) were used as dependent variables respectively. The dependent variables were dichotomized into categories of “poverty” and “non-poverty” using the A-F double critical value method, after which binary logistic regression was conducted. Among them, multidimensional health poverty is the result when k = 0.3. The dimensions of multidimensional health poverty – encompassing deprivation in health status, health service utilization capacity poverty, and health expenditure and security – are each constructed from four distinct indicators. In this context, experiencing deprivation in at minimum two out of the four indicators is deemed indicative of poverty within that particular dimension. Independent variables are individual characteristics, environmental characteristics, family and social characteristics of rural residents in Ningxia.
Results
Incidence of poverty by indicators of multidimensional health poverty
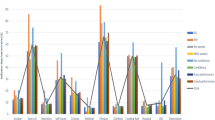
Table 4 exhibits the multidimensional health poverty prevalence among rural residents in Ningxia, as denoted by diverse indicators, prior to and following the comprehensive elimination of poverty. In the year of 2019, chronic diseases, ill debt, SRH, health-related quality of life and community health service utilization capacity were identified as the foremost indicators of relative poverty in rural communities. It is worth noting that the incidence of poverty associated with chronic diseases, ill debt, and SRH exceeded a staggering 25%, with rates of 37.87%, 28.03% and 26.39% respectively. Furthermore, poverty rates exceeding 10% were also observed for health-related quality of life, access to healthcare, accessibility to outpatient services, catastrophic health expenditures and relative poverty indicators, specifically at rates of 21.93%, 14.55%, 13.64%, 11.28% and 11.09% correspondingly. In 2022, the top five indicators of multidimensional health poverty among rural residents were chronic diseases, SRH, illness loans, health-related quality of life and hospitalization due to illness, with the poverty incidence rates of 38.53%, 21.09, 26.39%, 18.15% and 16.81%, respectively. Apart from a modest escalation in the prevalence of chronic ailments, there has been an overall decrease in poverty across all indices to some degree in the year 2022. Notably, the community health services witnessed the largest drop in poverty incidence, falling by a remarkable 12.01%.
To explore potential disparities in poverty incidence rates across rural male and female populations with respect to various indicators, we shall proceed with a more comprehensive analysis. Table 5 reports the incidence of poverty in various indicators of rural residents under gender characteristics. In 2019, across all indices of health status dimension, outpatient service utilization, borrowing due to illness, and impoverishment from medical expenses, females exhibited higher rates of poverty than males; for the remaining indices, males showed slightly higher poverty incidence than females. In 2022, across hospitalization due to illness, health-related quality of life, borrowing money due to illness, inpatient service utilization, community health service utilization, and impoverishment from medical expenses, females exhibited higher rates of poverty than males; for the remaining indices, males showed slightly higher poverty incidence than females.
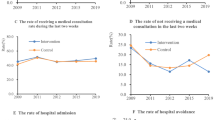
The measurement of multidimensional health poverty
Employing the A-F method, this study estimates the poverty incidence H(k), average deprivation A(k), and MHPI M(k) under different cutoff values. With k = 0.6, the multidimensional health poverty incidence was 0.5% in 2019, and 0.000 in 2022. The greater the value of the deprivation parameter k, the more indicators are considered when assessing multidimensional health poverty. However, this fails to capture differences among residents experiencing multidimensional health poverty, and the values of the MHPI and incidence rate become small and lack practical significance in identifying actual cases. Thus, we present in Table 6 the measurement results of multidimensional health poverty among rural residents in Ningxia for deprivation parameters ranging from 0.1 to 0.6. Longitudinally, regardless of the value of k, from 2019 to 2022 the the poverty incidence, average deprivation, and MHPI declined among rural residents. Viewed through the lens of gender characteristics, it becomes apparent that in rural areas, women demonstrate a multidimensional higher prevalence of health impoverishment across diverse indicators and years, as compared to their male counterparts. When k = 0.3, the incidence rates of multidimensional health poverty for rural residents were 22.3% and 7.7% in 2019 and 2022, respectively. The weighted average values of the MHPI were 0.091 and 0.028, while the shares of deprivation were 0.408 and 0.364, respectively. From a longitudinal perspective, regardless of the value of k, the incidence rates, MHPI, and average deprivation share of rural residents have all decreased from 2019 to 2022. When analyzed by gender, female rural residents exhibited higher incidence rates of multidimensional health poverty than males across different years and indicators.
Decomposition of MHPI-contribution rate analysis
Table 7 reports the contribution rates of each indicator to the MHPI when k = 0.3. In 2019 and 2022, chronic disease morbidity, SRH, health-related quality of life, and borrowing due to illness consistently ranked in the top four, each exceeding 10%. Among these, the contribution rate of chronic disease morbidity has consistently ranked first. From 2019 to 2022, the contribution rates of SRH, chronic disease, outpatient service utilization, health expenditure, and borrowing due to illness increased. Among these, the contribution rate of the chronic disease morbidity indicator increased the most, rising from 16.2% in 2019 to 19.6% in 2022, an increase of 3.6% points. The contribution rates of other indicators decreased to varying degrees. Among these, the contribution rate of inpatient service utilization decreased the most, dropping by 2.0%.
To delve deeper into the potential variations in the proportion of multidimensional health poverty within the context of rural Ningxia, as stratified by gender, this paper has scrutinized the 2022 dataset to ascertain the distribution of contribution rates with respect to diverse deprivation indicators among gender-stratified residents, under a specific threshold value (k = 0.3). Table 8 presents the contribution rates of different indicators to the multidimensional healthy poverty index under gender characteristics. The disparities in contribution rates between health expenditure and health security are multidimensional significant, both being 1.6%. Overall, there is little variation in the contribution of each indicator to the multidimensional healthy poverty index among rural residents of different genders.
Analyzing the determinants of multidimensional health poverty among rural residents
Table 9 provides an analysis of the marginal effects (ME) of various socio-demographic factors on multidimensional health poverty among rural residents. Compared to females, males show a slightly lower probability of experiencing health poverty (ME = -0.012, p < 0.05). Age groups demonstrate increasing risk with advancing age. Compared to individuals aged 0–29, those aged 30–44 have a 2.3% higher probability of health poverty (ME = 0.023, p < 0.05). For ages 60 and above, the probability further increases to 7.0% (ME = 0.070, p < 0.01), indicating a pronounced effect among older residents. Education appears protective against health poverty. Relative to illiterate individuals, those with primary school education experience a 2.8% lower probability (ME = -0.028, p < 0.01), junior high school graduates 2.9% lower (ME = -0.029, p < 0.01), and those with senior high school or higher 3.2% lower (ME = -0.032, p < 0.05). Individuals receiving government subsidies face an increased probability of health poverty by 1.4% (ME = 0.014, p < 0.05), potentially indicating a linkage with financial vulnerability. Larger family sizes correlate with decreased health poverty. Households of 4–5 members show a 5.0% lower probability (ME = -0.050, p < 0.01), and those with 6 or more members have a 5.2% reduction (ME = -0.052, p < 0.01). A larger housing area is also associated with reduced health poverty. Compared to those with the smallest housing area, individuals in a residence of 15 square meters or more exhibit a 2.2% reduction (ME = -0.022, p < 0.05), those with 30 square meters or more a 3.6% reduction (ME = -0.036, p < 0.01), and those with 45 square meters or more a 3.0% reduction (ME = -0.030, p < 0.05). Ownership of a television correlates with a 1.0% lower probability of health poverty (ME = -0.010, p < 0.01).
In terms of health status poverty, males have a slightly lower probability of experiencing health poverty than females (ME = -0.012, p < 0.05). Health poverty risk increases with age, reaching a 7.0% higher probability for those 60 and older (ME = 0.070, p < 0.01), while education serves as a protective factor, reducing health poverty by up to 3.2% for those with senior high school education or higher (ME = -0.032, p < 0.05). Family size and housing conditions also play a role; larger families and greater housing area are associated with reduced poverty. Additionally, television ownership is associated with a 1.0% decrease in health poverty (ME = -0.010, p < 0.01).
In terms of health service utilization capacity poverty, recipients of government subsidies have a slightly higher probability of experiencing poverty (ME = 0.007, p < 0.01). Larger family sizes, particularly those with 4–5 members, are associated with a reduced poverty risk, showing an 8.0% lower probability (ME = -0.008, p < 0.05). Housing conditions also play a role: separation of housing and kitchen areas is linked to a 0.9% decrease in poverty (ME = -0.009, p < 0.05), and television ownership corresponds to a 0.7% reduction in poverty risk (ME = -0.007, p < 0.05).
In terms of health spending and security poverty, males have a 1.7% lower probability of experiencing poverty compared to females (ME = -0.017, p < 0.01). Receiving government subsidies is associated with a higher likelihood of poverty, with a 1.6% increase in probability (ME = 0.016, p < 0.01), while family support reduces poverty risk by 1.1% (ME = -0.011, p < 0.05). Larger family sizes (6 or more members) show a protective effect, reducing poverty by 1.5% (ME = -0.015, p < 0.05). Housing conditions also play a role; households with separated kitchen facilities have a 1.1% lower probability of poverty (ME = -0.011, p < 0.05).
Discussion
Drawing on non-equilibrium panel data of rural residents in Ningxia from 2019 to 2022, this study has developed a MHPI to holistically assess changes in the region’s state of multidimensional health poverty, while also conducting a decomposition analysis. Furthermore, with respect to individuals, key factors contributing to multidimensional health poverty among rural residents have been explored through a logistic regression model. Meanwhile, the study also analyzed important components of multidimensional health poverty, including factors influencing health status poverty, health service utilization poverty, and health expenditure and security poverty. There were three critical findings from our study.
Though multidimensional health poverty among rural inhabitants of Ningxia is improving overall, but special attention should be paid to the female population.
Research indicates that while China has made strides in alleviating poverty in terms of absolute income and consumption, the issue of health poverty remains severe from a relative and multidimensional perspective. Notably, women in rural China are at a multidimensional higher risk of experiencing health poverty compared to men, a disparity rooted in various sociolect-cultural and economic constraints. This discrepancy is primarily rooted in the disadvantageous position of women with regards to their overall health status, access to healthcare opportunities, and capacity to achieve optimal well-being. These limitations are compounded by the dual burden of responsibilities in childbirth and household production that rural women often face, affecting their health outcomes and access to healthcare resources26,27. Gender roles in rural settings often require women to prioritize care giving-such as caring for children and elderly family members-over personal health needs, which reduces their ability to work outside the home, diminishes their financial autonomy, and limits their capacity to seek timely healthcare services28,29. Moreover, rural healthcare infrastructure may be less accessible to women, compounding existing disparities in health status and care accessibility30. The interaction between geographic isolation and gender roles intensifies women’s vulnerability, mirroring patterns observed in other regions where economic and social constraints shape health inequality31. Gender inequality in terms of health status, access to healthcare services, health expenditures and protection highlights rural women’s vulnerability to health poverty32. Given these findings, it is crucial to design targeted interventions that enhance rural women’s agency by improving access to high-quality health education and skill-building opportunities. Addressing gender-specific barriers could foster sustainable reductions in health poverty, empower rural women, and ultimately contribute to more equitable healthcare outcomes in under served regions.
Utilization of hospitalization services has improved, chronic disease-induced multidimensional health poverty poses the greatest threat
According to research findings, in both 2019 and 2022, the primary factor contributing to poverty among rural residents in Ningxia was the prevalence of chronic illness. Furthermore, the contributions of self-assessed health, healthcare expenditures, medical borrowing, and outpatient service utilization to the MHPI have increased. The long-term and recurrent nature of chronic diseases has led to increased medical expenses, which may exhaust the limited financial resources of rural families33. Additionally, chronic health conditions often impede work ability and reduce household income21. The increasing contribution of chronic illness highlights the growing threat it poses to multidimensional health poverty and underscores the need to improve the affordability and accessibility of long-term care for chronic disease patients34. The rise in healthcare expenditures and medical borrowing underscores the excessive burden placed on rural residents by medical costs, and thus requires more sustainable health financing solutions. Studies have shown that medical borrowing often leads to debt cycles and long-term difficulties, necessitating greater government assistance and subsidies for these households35. Moreover, the increase in both diagnosed and undiagnosed cases reflects lower health literacy among rural residents, which undermines their ability to manage their health and navigate the healthcare system, thereby increasing the risk of poor health outcomes and economic hardship36. This may also be related to fewer outpatient medical expense reimbursement programs and lower insurance coverage37,38. Finally, the decrease in the contribution of hospitalized patients is a reassuring sign, as hospitalization often has a significant financial effect on families. The reduction in the occurrence of hospitalization/non-hospitalization indicates that rural health conditions may be improving overall, albeit gradually. Continued investment in rural health infrastructure and strengthened efforts to improve rural residents’ health literacy are crucial for maintaining this hopeful trend36,39.
Multifaceted determinants of multidimensional health poverty among rural residents
The multidimensional health poverty of rural residents is influenced by a combination of individual characteristics, social and family support, environmental features, and the digital divide. Due to a higher prevalence of chronic diseases and physical frailty, the elderly often has greater health needs, which weaken their ability to work and earn money21. Insufficient social support exacerbates physical decline and social isolation, damaging the ability to access healthcare and making rural elderly people particularly vulnerable to health-related poverty24. Lower levels of education are often associated with poorer health literacy and health-seeking behaviors, limiting an individual’s ability to maintain good health and make effective use of healthcare systems40.
Rural residents who have received government economic assistance do not necessarily have enhanced financial resilience against health events, reducing the probability of health poverty23. This may be due to the scale and timeliness of government subsidies41. Current subsidy standards and frequencies may not meet the actual medical cost needs of residents, making it difficult to withstand the economic effect of major diseases38. To enhance rural residents’ ability to prevent multidimensional health poverty, government subsidy strategies need to take a broader and longer-term perspective, adopt targeted measures, and combine individual health capacity with community health assistance construction to maximize the dividends of health assistance policies42.
Poor housing environments increase the likelihood of disease exposure, increasing medical burden and possibly leading to health poverty43. In particular, whether the kitchen is separated from the living space directly affects residents’ environmental hygiene and health44, increasing the opportunity for multidimensional health poverty. Interestingly, we found that family size has a protective effect against multidimensional health poverty, but has no effect on health support and protection. This may be because the lifestyle of large families promotes stronger social interaction and cultural inheritance, which is conducive to disseminating health knowledge and forming beneficial healthy lifestyles45. However, larger families need to take care of more members’ medical needs, placing greater pressure on health support and protection46.
The digital divide further limits healthcare awareness and opportunities among populations with lower educational levels47. To bridge this gap, utilizing accessible and impactful digital tools like television can play a crucial role in reducing multidimensional health poverty among rural residents48. For example, targeted health education programs on public television channels could be scheduled at times most accessible to rural families, featuring information on preventive care, hygiene practices, and available health services. Television has proven effective as a health education tool, especially for those with limited digital skills, by providing ongoing health-related information and crisis assistance that can support populations in financial strain49. In remote rural areas, particularly among marginalized communities, strengthening the role of television in health-related public service broadcasting could help diminish health disparities and lower the risk of multidimensional health poverty50. Local governments could implement initiatives to collaborate with public health experts and local media to produce culturally tailored, easy-to-understand programs.
Limitation
Our study has various strengths and limitations. One notable forte lies in our endeavor to synthesize the MHPI through integrating multidimensional and relative elements, thus enabling a comprehensive evaluation of health paucity that is contextualized within the rural populace. To furnish a point of reference for further inquiry into the quandary of multidimensional health poverty among rural denizens. While this research is significant, there are some limitations. The factors influencing multidimensional health poverty among rural residents are complex and vary depending on the type of health-related poverty. This paper examines only a limited number of influencing variables and therefore requires further improvement in future research.
Conclusion
This study provides a new perspective for accurately identifying individuals experiencing relative health poverty in the southern mountainous region of Ningxia. We achieved this through the Multidimensional Health Poverty Index (MHPI). Our findings reveal that rural women and individuals with chronic diseases are high-risk groups for multidimensional health poverty. Key factors influencing this poverty include age, education level, government subsidies, household size, housing conditions, and the digital divide. To effectively address health poverty among vulnerable populations, targeted policy recommendations are crucial. First, increase investments in healthcare services for rural elderly individuals. Second, empower rural women through educational and economic support. Third, strengthen government assistance programs to ensure subsidies reach those in need. Fourth, improve housing conditions to promote healthy living environments. Lastly, bridge the digital divide by enhancing access to digital infrastructure and health literacy.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due [Data concerns privacy] but are available from the corresponding author on reasonable request.
Abbreviations
- MHPI:
-
Multidimensional Health Poverty Index
- SRH:
-
Self-rated health
References
Katikireddi, S. V. & Dundas, R. Relative poverty still matters. Lancet Public. Health. 2 (3), e126–e127 (2017).
Alkire, S., Nogales, R., Quinn, N. N. & Suppa, N. Global multidimensional poverty and COVID-19: A decade of progress at risk?. Soc. Sci. Med. 291, 114457 (2021).
Wang, Y. P. & Zhou, X. N. The year 2020, a milestone in breaking the vicious cycle of poverty and illness in China. Infect. Dis. Poverty. 9 (1), 11 (2020).
Clarke, P. & Erreygers, G. Defining and measuring health poverty. Soc. Sci. Med. 244, 112633 (2020).
World Health Organization and The World Bank. Tracking universal health coverage. In 2017 Global Monitoring Report (2017).
Chinese Academy of Social Sciences and Poverty Alleviation Office of the State Council. In China Poverty Alleviation and Development Report (2016).
Yuan, Q. et al. Economic status and catastrophic health expenditures in China in the last decade of health reform: A systematic review and meta-analysis. BMC Health Serv. Res. 21(1), 600 (2021).
Zhou, Y., Guo, Y. & Liu, Y. Health, income and poverty: Evidence from China’s rural household survey. Int. J. Equity Health 19(1), 36 (2020).
Hu, C. et al. Study on the health status and health service utilization of the elderly of a remote and poor village in a Mountainous Area in Jinzhai, Anhui. Int. J. Environ. Res. Public. Health 14(4). (2017).
Pascual-Sáez, M., Cantarero-Prieto, D. & Lanza-León, P. The dynamics of health poverty in Spain during the economic crisis (2008–2016). Health Policy. 123 (10), 1011–1018 (2019).
Brzezinski, M. Accounting for trends in health poverty: a decomposition analysis for Britain, 1991–2008. Eur. J. Health Econ. 16 (2), 153–159 (2015).
Anand, P. Capabilities and health. J. Med. Ethics. 31 (5), 299–303 (2005).
McIntyre, D., Thiede, M., Dahlgren, G. & Whitehead, M. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Soc. Sci. Med. 62 (4), 858–865 (2006).
Klasen, S. & Waibel, H. Vulnerability to poverty in South-East Asia: Drivers, measurement, responses, and policy issues. World Dev. 71, 1–3 (2015).
Sen, A. Editorial: human capital and human capability. World Dev. 25 (12), 1959–1961 (1997).
Li, C. & Tang, C. Income-related health inequality among rural residents in western China. Front. Public. Health. 10, 1065808 (2022).
Pham, A. T. Q. & Mukhopadhaya, P. Multidimensionl poverty and the role of social capital in poverty alleviation among ethnic groups in Rural Vietnam: A multilevel analysis. Soc. Indic. Res. 159(1), 281–317 (2022).
Fan, Z., Bai, X. & Zhao, N. Explicating the responses of NDVI and GDP to the poverty alleviation policy in poverty areas of China in the 21st century. PLoS One. 17 (8), e0271983 (2022).
Ran Ren, Z. H. The Development Framework and Strategies of China’s Medical Security System. (Economic Science Press, Beijing).
Guo, W. et al. The impact of healthcare reform on the dynamic changes in health service utilization and equity: A 10-year follow-up study. Sci. Rep. 12(1), 3576 (2022).
Ma, Y., Xiang, Q., Yan, C., Liao, H. & Wang, J. Poverty vulnerability and health risk action path of families of rural elderly with chronic diseases: Empirical analysis of 1,852 families in Central and Western China. Front. Public. Health 10, 776901 (2022).
Alkire, S. & Foster, J. Counting and multidimensional poverty measurement. J. Public. Econ. 95 (7), 476–487 (2011).
Li, Y. & Marquez, R. Can government subsidies and public mechanisms alleviate the physical and mental health vulnerability of China’s urban and rural residents? Int. J. Equity Health. 22 (1), 59 (2023).
Zeng, W., Zhao, P., Zhao, Y. & Saddique, R. The multidimensional relative poverty of rural older adults in China and the effect of the health poverty alleviation policy. Front. Public. Health. 10, 793673 (2022).
Kim, J. H. Multicollinearity and misleading statistical results. Korean J. Anesthesiol. 72 (6), 558–569 (2019).
Shannon, G. et al. Gender equality in science, medicine, and global health: where are we at and why does it matter? Lancet 393 (10171), 560–569 (2019).
Subham Roy, S. M., Bose, A. & Chowdhury, I. R. The rich-poor divide: Unravelling the spatial complexities and determinants of wealth inequality in India. Appl. Geogr. 166 (2024).
Moradhvaj, Saikia, N. Gender disparities in health care expenditures and financing strategies (HCFS) for inpatient care in India. SSM Popul. Health. 9, 100372 (2019).
Roy, S., Majumder, S., Bose, A. & Roy Chowdhury, I. Does geographical heterogeneity influence urban quality of life? A case of a densely populated Indian City. Papers Appl. Geogr. 9(4), 395–424 (2023).
Majumder, S., Roy, S., Bose, A. & Chowdhury, I. R. Understanding regional disparities in healthcare quality and accessibility in West Bengal, India: A multivariate analysis. Reg. Sci. Policy Pract. 15(5), 1086–1114 (2023).
Majumder, S., Kayal, P., Chowdhury, I. R. & Das, S. Regional disparities and development in India: Evidence from Wroclow Taxonomy and K-means clustering. GeoJournal 88(3), 3249–3282 (2023).
Ostlin, P., Sen, G. & George, A. Paying attention to gender and poverty in health research: content and process issues. Bull. World Health Organ. 82 (10), 740–745 (2004).
Sapkota, T., Houkes, I. & Bosma, H. Vicious cycle of chronic disease and poverty: a qualitative study in present day Nepal. Int. Health. 13 (1), 30–38 (2021).
Hu, H. et al. Health service underutilization and its associated factors for chronic diseases patients in poverty-stricken areas in China: A multilevel analysis. BMC Health Serv. Res. 21(1), 707 (2021).
Rahman, M. M., Gilmour, S., Saito, E., Sultana, P. & Shibuya, K. Self-reported illness and household strategies for coping with health-care payments in Bangladesh. Bull. World Health Organ. 91 (6), 449–458 (2013).
Du, W., Liu, P. & Xu, W. Effects of decreasing the out-of-pocket expenses for outpatient care on health-seeking behaviors, health outcomes and medical expenses of people with diabetes: evidence from China. Int. J. Equity Health. 21 (1), 162 (2022).
Miao, Y. et al. Improving the performance of social health insurance system through increasing outpatient expenditure reimbursement ratio: a quasi-experimental evaluation study from rural China. Int. J. Equity Health. 17 (1), 89 (2018).
Hu, M., Mao, W., Xu, R., Chen, W. & Yip, W. Have lower-income groups benefited more from increased government health insurance subsidies? Benefit incidence analysis in Ningxia, China. Health Policy Plan. 37 (10), 1295–1306 (2022).
Liu, C., Liu, Z. M., Nicholas, S. & Wang, J. Trends and determinants of catastrophic health expenditure in China 2010–2018: A national panel data analysis. BMC Health Serv. Res. 21(1), 526 (2021).
Huang, Y. et al. The effect of health literacy on health status among residents in Qingdao, China: a path analysis. Environ. Health Prev. Med. 26 (1), 78 (2021).
Shen, C. et al. Whether high government subsidies reduce the healthcare provision of township healthcare centers in rural China. BMC Health Serv. Res. 21 (1), 1184 (2021).
McCullough, J. M. Government health and social services spending show evidence of single-sector rather than multi-sector pursuit of population health. Inquiry 56, 46958019856977 (2019).
Rauh, V. A., Landrigan, P. J. & Claudio, L. Housing and health: Intersection of poverty and environmental exposures. Ann. N Y Acad. Sci. 1136, 276–288 (2008).
Nie, P., Li, Y., Ding, L. & Sousa-Poza, A. Housing poverty and healthy aging in China: Evidence from the China Health and Retirement Longitudinal Study. Int. J. Environ. Res. Public. Health 18(18). (2021).
Lesinski, J. Family size: its influence on family’s health, economic status and social welfare. Obstet. Gynecol. Surv. 31 (5), 421–452 (1976).
Turagabeci, A. R., Nakamura, K., Kizuki, M. & Takano, T. Family structure and health, how companionship acts as a buffer against ill health. Health Qual. Life Outcomes. 5, 61 (2007).
Saeed, S. A. & Masters, R. M. Disparities in health care and the digital divide. Curr. Psychiatry Rep. 23(9), 61 (2021).
Fu, L., Pei, T., Xu, J., Han, J. & Yang, J. Inspecting the health poverty trap mechanism: Self-reinforcing effect and endogenous force. BMC Public. Health 24(1), 917 (2024).
Gollust, S. E., Fowler, E. F. & Niederdeppe, J. Television news coverage of public health issues and implications for public health policy and practice. Annu. Rev. Public. Health 40, 167–185 (2019).
Sinha, C. & Schryer-Roy, A. M. Digital health, gender and health equity: invisible imperatives. J. Public. Health (Oxf). 40 (suppl_2), ii1–ii5 (2018).
Acknowledgements
Not applicable.
Funding
This paper is supported by National Natural Science Foundation of China (Grant No.72164033), Key Projects of Natural Science Foundation of Ningxia (Grant No.2022AAC02036), Ningxia Natural Science Foundation (NYG2022049, 2023AAC03224).
Author information
Authors and Affiliations
Contributions
H.Q. conceptualized the research idea and design. K.X.C. participated in the research design, drafted the manuscript, analyzed, and interpreted the data. J.W.Q. helped revise the manuscript and interpreted the data. W.L.W., Q.H., N.X. helped clean the data and merge databases. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Ningxia Medical University(2021-G152). All subjects gave their informed consent for inclusion before they participated in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, K., Qiu, J., Wang, W. et al. Identification and analysis of influencing factors of multidimensional health poverty in rural areas of Northwest China. Sci Rep 14, 28952 (2024). https://doi.org/10.1038/s41598-024-80628-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-80628-3