Abstract
Abdominal aortic aneurysm is a potentially fatal vascular inflammatory disease characterized by infiltration of various inflammatory cells.The GABA-A receptor is expressed in many inflammatory cells such as macrophages and T cells and has anti-inflammatory and antioxidant effects. Therefore, the GABA-A receptor may become a potential therapeutic target for abdominal aortic aneurysms. The purpose of this study was to investigate the effect of regulating the activity of the GABA-A receptor on the formation of experimental abdominal aortic aneurysm in rats. In this study, the abdominal aortic aneurysm model of rats was established by aorta intracavitary perfusion of elastase combined with aorta extracavitary infiltration of calcium chloride. GABA-A receptor agonist (topiramate) and antagonist (bicuculline) were used to treating the abdominal aortic aneurysm model rats, which were divided into sham operation group, model group, topiramate group, and bicuculline group(n = 10). Histopathology, immunohistochemistry, fluorescence quantitative PCR, Western blotting, ELISA and Gelatine zymogram were used to study. Regulation of GABA-A receptor activity can interfere with the development and severity of abdominal aortic aneurysms in rats. The GABA-A receptor agonist topiramate reduces the infiltration of inflammatory cells, particularly T cells, into the abdominal aortic wall, while also modulating the balance of Th1/Th2 cytokines in peripheral blood, leading to a significant reduction in inflammatory responses. Additionally, topiramate decreases the secretion of matrix metalloproteinases MMP2 and MMP9, thereby inhibiting extracellular matrix degradation and slowing the progression of aneurysms. In contrast, the GABA-A receptor antagonist bicuculline exacerbates inflammation and promotes aneurysm development. At the molecular level, the mechanisms of action of the GABA-A receptor agonist topiramate and the antagonist bicuculline may involve inhibition or activation of the p38 MAPK signaling pathway. Regulation of GABA-A receptor activity can effectively intervene in the occurrence and development of abdominal aortic aneurysms in rats.
Similar content being viewed by others
Introduction
The word aneurysm comes from the Greek ανευρυσµα, which means dilatation. Abdominal aortic dilatation is a complex dynamic process, which eventually leads to the formation and even rupture of abdominal aortic aneurysm (AAA)1. AAA is defined as the diameter of the abdominal aorta greater than 1.5 times the normal diameter or the diameter of the infrarenal abdominal aorta greater than 3 cm2. The pathogenesis of AAA is complex and unclear at present. Its main pathological changes are inflammatory cell infiltration, extracellular matrix degradation, and vascular smooth muscle cell apoptosis, in which the activation of inflammatory cells induces immune-inflammatory reaction throughout, which leads to abdominal aortic lumen dilatation or dissection formation, and even rupture, resulting in severe bleeding and life-threatening3,4. Therefore, how to inhibit the activation of inflammatory cells is the main measure to prevent AAA, and it is also an unsolved clinical problem at present. Existing studies have shown that macrophage-mediated innate immunity and T, B cell-mediated adaptive immunity play a key role in the formation of AAA5,6. Recent studies have shown that gamma-aminobutyric acid (GABA) ligand-gated ion channel A receptor (GABA-A) expressed on macrophages, T cells, and other cell membranes can regulate its activity, which may be the intervention target of AAA7,8. Therefore, we hypothesized that regulation of GABA-A receptor activity could interfere with the occurrence and development of experimental AAA, and explore its potential pathophysiological molecular mechanism, expecting to develop an effective drug treatment.
Methods
Experimental animals and ethical statement
Forty healthy Sprague-Dawley (SD) rats, aged 8 to 10 weeks and weighing 250–300 g, were sourced from the Experimental Animal Center of North Sichuan Medical College. They were freely fed and provided water, housed at a temperature of 22 ~ 25℃, with regular ventilation. Five rats were group-housed before the surgery, and postoperatively, five rats were individually housed. The experiments involving animals were approved by the Animal Care and Use Ethics Committee of North Sichuan Medical College and adhered to the ‘Guide for the Care and Use of Laboratory Animals’ guidelines set by the National Institutes of Health, United States. Additionally, all methods were reported in accordance with the Animal Research: Reporting In Vivo Experiments (ARRIVE) guidelines. At the end of the experiment, euthanasia was carried out in rats by cervical dislocation.
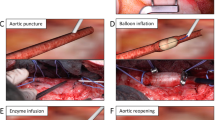
Establishment of AAA model in rats
A rat infrarenal AAA model was established using a retroperitoneal approach. Rats were anesthetized with 2% pentobarbital sodium at a dose of 30 mg/kg. Once satisfactory anesthesia was achieved, the infrarenal segment of the abdominal aorta was isolated via the retroperitoneal route. The morphology of the aorta was observed and photographed. The diameter was measured using a vernier caliper, with two individuals recording the measurements and the average value taken. Intraluminal perfusion of 0.1 mL elastase9 (approximately 5 U, Sigma, E1250) was performed for 20 min, followed by extraluminal infiltration of 1.0 mol/L calcium chloride9 (Nobolaiden Beijing, R0447) for 10 min. The diagnosis of AAA was based on an aortic diameter increase of more than 50% or aneurysm rupture within 28 days post-surgery. For detailed methodology, refer to the previous research by our group9.
Experimental grouping
40 healthy adult SD rats, Weight 250–300 g, According to the male-female ratio of 1: 1. Randomly divided into sham operation group (saline perfusion + saline infiltration, n = 10), Model group (Elastase 5U perfusion + 1.0 mmol/L calcium chloride infiltration, n = 10), topiramate group (Elastase 5U perfusion + 1.0 mmol/L calcium chloride infiltration + topiramate10 100 mg/kg/d intragastric administration, Janssen Pharmaceutical Xian, H20020555, n = 10), bicuculline group (Elastase 5U perfusion + 1.0 mmol/L calcium chloride infiltration + bicuculline11 2 mg/kg/d intraperitoneal injection, MCE, HY-N0219, n = 10). Topiramate and bicuculline were used on the first day after the operation until the end of the experiment on the 28th day. On the 28th day postoperatively, rats were re-anesthetized and the perfused segment of the abdominal aorta was isolated through a laparotomy approach. The morphology was observed and photographed, the diameter was measured using a vernier caliper, and the results were recorded (with measurements taken by two individuals and the average value was taken).
HE, Masson, EVG staining and immunohistochemical detection (IHC)
Paraffin-embedded sections, 5-µm thick, underwent haematoxylin and eosin (HE) staining for general histology. Evaluation of collagen fiber integrity utilized Masson staining, while elastic fiber integrity was assessed through EVG staining specifically on the abdominal aorta. Detection of target protein expression involved the use of primary antibodies against CD312 (1:1000, Proteintech, 17617-1-AP), CD2013 (1:100, Invitrogen, MA1-7634), CD6814 (1:1000, Proteintech, 28058-1-AP), GABA-α515 (1:100, HUABIO, ET7107-08), and smooth muscle actin (SMA)16 (1:3000; Proteintech,14395-1-AP). The quantification of positive areas included all vessel-positive regions, with results normalized to the total vessel area of the sample. Marker-positive cells were counted across the aortic cross-section (ACS) for each aortic slice.
Multiplex immunofluorescence staining
Multiplex immunofluorescence staining was performed using a 7-color Opal Multiplex IHC kit17 (Akoya Biosciences). Abdominal aortic sections were incubated overnight at 4 °C with anti-CD3 antibody18 (1:200, Proteintech, 17617-1-AP) and anti-GABA-α5 antibody15 (1:100, HUABIO, ET7107-08). The sections were then incubated for 1 h at room temperature with fluorescently conjugated secondary antibodies. After staining, fluorescence microscopy was used to assess the expression and localization of the fluorescent signals.
Fluorescence quantitative PCR assay (qPCR)
Total RNA from the perfused abdominal aorta in each experimental group was extracted following the TRIzol kit instructions19 (Thermo Fisher, 15596026CN), and cDNA was synthesized through reverse transcription as per the reverse transcription kit guidelines20 (Takara, RR047A). The primer sequences can be found in Table 1. PCR conditions were as follows: initial denaturation at 95 °C for 30 s for one cycle, followed by PCR at 95°C for 5 s → 60 °C for 30 s for 40 cycles. The second step involved a melting curve at 95 °C for 6 s → 65 °C for 5 s → 95 °C for 30 s for one cycle. Utilizing β-Actin as the internal reference, the ∆Ct was calculated by subtracting the Ct value of the internal reference from the Ct value of the target gene. The 2-∆∆Ct value represented the mRNA expression of the target gene (Table 1).
Enzyme-linked immunosorbent assay (ELISA)
The contents of IL-4, INF-γ, IL-6 in rat plasma and abdominal aorta were quantitatively detected by ELISA kit (Fine Biotech Wuhan, ER0041, ER0012, ER0042), and the operation was carried out according to the instructions of the kit.
Western blotting assay (WB)
Aortic tissues were homogenized, and extracted proteins were prepared at a ratio of 1 mg of tissue to 10 µL of lysate RIPA, 0.2 µL of phosphatase inhibitor, and 0.2 µL of protease inhibitor PMSF. Primary antibodies against MMP221 (1:1000, Proteintech, 66366-1-Ig), MMP922 (1:500, Proteintech, 10375-2-AP), P-p3823 (1:1000, HUABIO, ER2001-52), p3824 (1:1000, HUABIO, ET1702-65), and GAPDH25 (1:20000, Proteintech, 10494-1-AP) were employed to assess target protein expression. Subsequent to image acquisition using a Bio–Rad imaging system, grey value density was analyzed using ImageJ. The relative protein expression levels of p38、P-p38、MMP2 and MMP9 in the perfused abdominal aorta were determined with GAPDH serving as the internal reference.
Gelatine zymogram
The activities of MMP-2 and MMP-9 in the abdominal aortae of rats were assessed using an MMP Zymography Assay Kit26 (Applygen, P1700). The procedures outlined in the kit instructions were adhered to.
Statistical analysis
Statistical analysis was performed using SPSS 21 software. Measurement data were expressed as mean ± standard deviation (\(\bar{x}\) ± s). An independent sample t-test was used for comparison of measurement data between two groups, while one-way ANOVA was employed for comparison among multiple groups. The LSD method was used for post hoc multiple comparisons. Categorical data were analyzed using the chi-square test or Fisher’s exact test. A P-value of less than 0.05 was considered statistically significant. Image analysis and vascular parameter measurements were conducted using Image J and Image Pro Plus 6.0 software.
Results
Animal survival rate
There was no death in Sham Group and Topiramate Group, and the survival rate was 100%. In Model Group, there was no death during operation, and one died on the 4th day after operation, with a survival rate of 90%. In Bicuculline Group, there was no death during operation, and one died on the 13th and 16th day after operation, with a survival rate of 80%. There was no significant difference in survival rate among rats in each group (P > 0.05).
The effect of GABA-A receptor modulating drugs on the incidence of AAA in rats
The preoperative aortic diameters of the rats in each group showed no statistically significant differences (P > 0.05). At 28 days post-surgery, comparisons of aortic diameters and expansion rates revealed that the diameters in the Sham and Topiramate groups were significantly smaller than those in the Model group, with markedly lower expansion rates (P < 0.05). In contrast, the Bicuculline group exhibited significantly larger aortic diameters and higher expansion rates compared to the Model group (P < 0.05). These differences remained statistically significant in male rats but were not significant in female rats. Furthermore, the expansion rates in male rats were significantly greater than those in female rats within both the Model and Bicuculline groups (P < 0.05). However, no significant difference in expansion rates was observed between male and female rats in the Sham and Topiramate groups (P > 0.05). The Sham group had no aneurysms, with an aneurysm formation rate of 0%. The Topiramate group had two aneurysms (0 females, 2 males), with an aneurysm formation rate of 20%. The Model group had eight aneurysms (5 males, 3 females), with an aneurysm formation rate of 80%, and the Bicuculline group had nine aneurysms (5 males, 4 females), with an aneurysm formation rate of 90%. Compared to the Model group, the aneurysm formation rates in the Sham and Topiramate groups were significantly lower (P < 0.05), while the difference in aneurysm formation rate between the Model and Bicuculline groups was not statistically significant (P > 0.05). ( Table 2; Fig. 1)
Dilatation degree of abdominal aorta and appearance of aneurysm in each group. (A) No dilation was observed in the perfused segment of the abdominal aorta in the Sham group. (B) Localized saccular aneurysm formation was observed in the perfused segment of the abdominal aorta in the Model group. (C) Localized mild dilation was observed in the perfused segment of the abdominal aorta in the Topiramate group. (D) Irregular aneurysm formation was observed in the perfused segment of the abdominal aorta in the Bicuculline group.
The effect of GABA-A rceptor modulating drugs on the severity of AAA in rats
In the Model group, the perfused segment of the abdominal aorta exhibited saccular dilation, while in the Bicuculline group, the abdominal aorta displayed irregular dilation with significant perivascular adhesions. In the Topiramate group, mild dilation of the abdominal aorta was observed with slight perivascular adhesions. Histological examination revealed that the vessel walls in the Model and Bicuculline groups were significantly thinned, with degradation of the extracellular matrix, formation of dissection, and discontinuous, partially ruptured or absent elastic fibers. A marked reduction in smooth muscle cells and significant infiltration of inflammatory cells in the media and adventitia were noted, with the Bicuculline group showing more severe changes. In the Topiramate group, the vessel wall was partially thinned, but the internal and external elastic layers remained intact, clearly separating the intima, media, and adventitia. The smooth muscle cells were arranged orderly, and there was only mild infiltration of inflammatory cells in the media and adventitia. No such changes were observed in the Sham group. Compared to the Model group, the vascular thickness, elastic fiber content, collagen fiber content, and smooth muscle cell density were significantly higher in the Sham and Topiramate groups (P < 0.05). In contrast, the Bicuculline group showed reduced vascular thickness (P > 0.05) and significantly lower elastic fiber content, collagen fiber content, and smooth muscle cell density (P < 0.05). (Table 3; Fig. 2).
Histopathological changes of abdominal aorta of rats in each group. (A) The vascular wall structure in the Sham group remains intact. (B) In the Model group, the vessel wall is thinned, with discontinuous, partially lost or fragmented elastic and collagen fibers, and a reduction in smooth muscle cells. (C) In the Topiramate group, the vessel wall is partially thinned, but clear inner and outer elastic layers are still visible, and smooth muscle cells are arranged in an orderly fashion. (D) In the Bicuculline group, the vessel wall is significantly thinned, with degradation of the extracellular matrix, smooth muscle cell loss, and dissection formation. (E) Quantitative analysis of normalized vascular wall thickness. (F) Differences in vascular wall thickness across individual rats.
Regulation of immune cell infiltration and immune microenvironment by GABA-A receptor modulating drugs
Immune inflammatory responses play a critical role in the development of aneurysms, with the accumulation of inflammatory cells being a key pathological feature of AAA. Therefore, we conducted relevant research to explore whether GABA-A receptor modulating drugs exert their effects by regulating the infiltration of inflammatory cells and the expression of various cytokines. Our results showed that macrophages, T cells, and B cells infiltrated the media and adventitia to varying degrees in the Model, Topiramate, and Bicuculline groups. Topiramate significantly reduced the numbers of macrophages, T cells, and B cells (P < 0.05), while Bicuculline significantly increased the number of T cells (P < 0.05). Although Bicuculline also increased the numbers of macrophages and B cells, the differences were not statistically significant (P > 0.05). (Fig. 3) Therefore, we speculate that T cells may be the primary target cells for the modulation of inflammatory responses by GABA-A receptor modulating drugs.
Activated CD4 + T lymphocytes can differentiate into various polarized effector T cells, including Th1, Th2, Th17, and Treg cells. We focused on examining typical Th1 (IFN-γ) and Th2 (IL-4、IL-6) cytokines. The results showed that, compared to the Model group, the concentrations of IFN-γ and IL-6 in plasma, as well as IFN-γ, IL-4, and IL-6 in the abdominal aorta, were significantly reduced in the Topiramate group (P < 0.05). In the Bicuculline group, plasma IFN-γ levels increased (P > 0.05), and IL-6 levels significantly increased (P < 0.05), while IFN-γ, IL-4, and IL-6 levels in the abdominal aorta were significantly elevated (P < 0.05). No statistically significant differences were observed in plasma IL-4 levels among the groups (P > 0.05) (Table 4).
Expression of GABA α5 subunit in inflammatory cells of the abdominal aortic wall
Previous studies have shown that GABA-A receptors are expressed on peripheral inflammatory cells, such as macrophages27. Our study demonstrated that the infiltrating inflammatory cells in the Model, Topiramate, and Bicuculline groups widely expressed the GABA α5 subunit, while no expression of the GABA α5 subunit was observed in the Sham group. Compared with the Model group, the Topiramate group showed a significant reduction in the number of inflammatory cells expressing the GABA α5 subunit (P < 0.05), whereas the Bicuculline group showed a significant increase (P < 0.05) (Fig. 4A, B). Given that T cells are likely the key inflammatory cells modulated by GABA-A receptor modulating drugs, we performed immunofluorescence co-localization experiments to confirm the presence of GABA-A receptors on T cells. The results revealed co-localized expression of the T cell marker CD3 and the GABA α5 subunit in the adventitia of the abdominal aorta in the Model, Topiramate, and Bicuculline groups at varying degrees (Fig. 4C).
Expression of GABA α5 subunit in inflammatory cells in the abdominal aortic wall across different groups. (A) Widespread expression of the GABA α5 subunit in infiltrating inflammatory cells in the Model, Topiramate, and Bicuculline groups. (B) Quantitative analysis of GABA α5 subunit-positive inflammatory cells, *P < 0.05 compared to the Model group, n = 10. ACS, aortic cross section. (C) Representative immunofluorescence images showing colocalization of CD3 and GABA α5 subunit.
GABA-A receptor modulating drugs influence the expression and activity of MMP2/9 by regulating the p38 MAPK signaling pathway
MMP2 and MMP9 are important proteolytic enzymes involved in vascular inflammation and tissue repair, playing a role in the formation and progression of aneurysms28. The p38 MAPK signaling pathway plays a crucial role in regulating MMP expression, primarily through the downstream targeting of transcription factor binding sites on the most MMP promoters29. To further investigate whether MMP2/9 is regulated by the p38 MAPK pathway in AAA, we measured the expression of related proteins. The results showed no statistically significant differences in p38 expression levels among the groups (P > 0.05). Compared to the Model group, the Sham and Topiramate groups exhibited significantly reduced P-p38 MAPK expression and P-p38 MAPK/p38 MAPK ratios (P < 0.05), along with significantly downregulated mRNA and protein expression and activity of MMP2/9 (P < 0.05). In contrast, the Bicuculline group showed significantly elevated P-p38 MAPK expression and P-p38 MAPK/p38 MAPK ratios (P < 0.01), with significantly upregulated mRNA and protein expression and activity of MMP2/9 (P < 0.05) (Fig. 5).
Phosphorylation levels of the p38 MAPK signaling pathway and expression and activity of MMP2/MMP9 in the abdominal aortic wall. (A) Representative Western blot bands showing expression of p38, P-p38, MMP2, and MMP9 proteins in each group. (B) Representative zymography images of MMP2 and MMP9 enzyme activities in each group. (C) Relative quantitative analysis of MMP2 and MMP9 mRNA expression; n = 6. (D) Relative quantitative analysis of MMP2 and MMP9 protein expression; n = 4. (E) Quantitative analysis of MMP2 and MMP9 protein activity; n = 4. (F) Relative quantitative analysis of p38 and P-p38 protein expression; n = 4. *P < 0.05, **P < 0.01 compared to the Model group.To present the data clearly and concisely, gels/blots were cropped. Uncropped original gels/blots are shown in Supplementary Figures S1-S2.
Discussion
The role of inflammation in the pathogenesis of AAA is undeniable, with macrophage-mediated innate immunity and T- and B-cell-mediated adaptive immunity playing crucial roles in the formation of AAA6. Inflammation can induce MMP-mediated extracellular matrix degradation and apoptosis of vascular smooth muscle cells. The interplay of these three factors leads to thinning and dilation of the abdominal aortic wall, ultimately resulting in the formation of an arterial aneurysm30 .The GABA-A receptor is one of the ligand-gated chloride ion channel superfamily members, composed of α, β, γ, δ, ε, π, θ, ρ8 subunits, forming a pentameric heteropentameric structure31. Among these subunits and their various combinations, α5 subunit is indispensable in regulating cell migration during the movement process32,33. Previous research on GABA has primarily focused on the field of the nervous system, where GABA excites the GABA-A receptor to regulate inhibitory signal transmission between neural synapses34,35. Existing studies have found that the GABA-A receptor is also expressed on the membranes of peripheral macrophages, T cells, and other immune cells, inhibiting the activity of inflammatory immune cells and regulating immune responses, thereby delaying the progression of immune-inflammatory diseases7,8,27. As the inflammatory immune response is central to the occurrence and development of AAA, and GABA exciting the GABA-A receptor has anti-inflammatory and immune-regulatory effects, this study chose an AAA animal model to explore the role of regulating GABA-A receptor activity in AAA and its potential mechanisms.
Studies on the types and distribution of inflammatory cells in human AAA specimens have revealed extensive infiltration of inflammatory cells, particularly in the medial and adventitial layers of the aneurysm wall. Macrophages, T cells, and B cells make up over 90% of all inflammatory cells, with T cells and B cells being the most prominently infiltrated36. In this study, the Model group showed extensive infiltration of inflammatory cells in the abdominal aortic wall, primarily in the medial and adventitial layers, with B cells being the most abundant, followed by T cells, and a relatively lower proportion of macrophages. This finding is consistent with the observations of Blassova37 and Bobryshev38, suggesting that the AAA animal model used in this study closely mimics human disease in terms of inflammatory cell infiltration, making it suitable for studying the role of inflammation in AAA. Our results showed that, compared to the Model group, the Topiramate group exhibited a significantly lower aneurysm formation rate, reduced aortic dilation, and inflammatory adhesion in the gross specimens. Histological observations also revealed significantly decreased infiltration of inflammatory cells, including macrophages, T cells, and B cells, in the abdominal aortic wall of the Topiramate group. In contrast, the Bicuculline group demonstrated a significant increase in T cell infiltration in the abdominal aortic wall, while the increases in macrophage and B cell infiltration were observed but did not reach statistical significance. Therefore, we reasonably hypothesize that T cells may be the key inflammatory cells modulated by GABA-A receptor modulating drugs. Additionally, we confirmed the co-localization of T cells with GABA α5 subunits, further supporting our hypothesis that the GABA-A receptor agonist Topiramate may exert its anti-inflammatory effects by activating GABA α5 subunits in T cells, thereby inhibiting T cell infiltration. Conversely, the GABA-A receptor antagonist Bicuculline has the opposite effect. Interestingly, there may be sex differences in the modulation of AAA by GABA-A receptor modulating drugs. Our results demonstrated that the extent of aortic expansion in male rats was greater than in female rats in the Model group. After treatment with Topiramate, this difference disappeared, suggesting that Topiramate may have a more pronounced therapeutic effect on AAA in male rats than in females. Some studies suggest that Topiramate may influence the hypothalamic-pituitary-gonadal axis, reducing estrogen levels39,40,41. It is well known that estrogen is a protective factor against AAA, and the attenuation of this advantage by Topiramate might explain its less effective treatment in females. However, the exact mechanism requires further investigation.
There is ongoing debate regarding the nature of inflammatory factors released by immune cells that contribute to the formation of AAA. In this study, the AAA animal model is characterized by a predominance of adaptive immunity mediated by T and B cells, with T cells likely being the key inflammatory cells modulated by GABA-A receptor modulating drugs. Therefore, we focused on CD4 + T helper cells. CD4 + T helper cells are primarily divided into two major subsets: Th1 and Th2. Th1 cells secrete IFN-γ but not IL-442, whereas Th2 cells secrete IL-4 but not IFN-γ43. Thus, IFN-γ and IL-4 serve as markers to differentiate Th1 and Th2 cytokines. Th1 cytokines mediate cytotoxic effects by promoting the activation and proliferation of cytotoxic T cells, macrophages, and NK cells. Th2 cytokines primarily function to stimulate B cell proliferation, antibody production, and mediate humoral immunity. Since Th1 and Th2 cells regulate cellular and humoral immunity, any disruption in the balance between Th1 and Th2 inevitably leads to alterations in immune function. In this study, the Model group exhibited a significant increase in peripheral blood IFN-γ levels, with no significant change in IL-4 levels, while both IFN-γ and IL-4 were significantly elevated in the local aneurysm wall. This suggests that the development of AAA involves a disruption of Th1/Th2 cell function and activation of a systemic immune-inflammatory response. The GABA-A receptor agonist Topiramate was able to regulate the balance of Th1/Th2 cytokines in peripheral blood, reducing Th1 cytokines and alleviating systemic inflammation, while also decreasing Th1 and Th2 cytokines in the local aneurysm wall, thereby reducing local inflammation. Conversely, the GABA-A receptor antagonist Bicuculline produced the opposite effects.
These findings align with the inflammatory regulatory effects reported by Chen27 et al. (2020), though the mechanisms differ. Chen et al. demonstrated that topiramate promotes the polarization of M1 macrophages to M2 macrophages, reducing inflammation and enhancing tissue repair, ultimately lowering the incidence of AAA. In comparison, our study reveals that topiramate exerts its protective effects in AAA through the regulation of T cell mediated immune responses. This suggests that topiramate may exert its protective effects via the coordinated regulation of multiple immune cell types. Despite differences in study models and the immune cells examined, both studies highlight the critical role of inflammation in AAA formation. Future research should further explore the interaction between macrophages and T cells to comprehensively elucidate the anti-inflammatory mechanisms of topiramate.
In addition, this study also investigated the molecular mechanisms of GABA/GABA-A receptor pathway intervention in the formation of AAA. Inflammatory stimuli can lead to the activation of the MAPK signaling pathway, which is regulated by ERK, JNK, and p38, with the p38 pathway considered a major signaling hub and a key regulator of inflammation44,45. p38MAPK is an intracellular signaling protein kinase that acts on various transcription factors, activating the expression of multiple genes, mediating various biological effects within cells, and participating in the regulation of various pathophysiological functions46. Recent research has found that the p38MAPK signaling pathway is involved in the remodeling of the extracellular matrix (ECM) in AAA47,48. In studies related to GABA and the extracellular matrix, it was found that in rheumatoid arthritis patients, the GABA/GABA-A receptor pathway inhibits p38 phosphorylation, suppresses MMP secretion, and maintains the integrity of the extracellular matrix49. So, does the GABA/GABA-A receptor pathway intervene in the formation of AAA by inhibiting the p38 signaling pathway? This study provided an answer: compared to the Model group, the expression of P-p38MAPK in the aneurysm tissue of the Topiramate group was significantly reduced, the P-p38MAPK/p38MAPK ratio decreased significantly, and the expression and activity of MMP2 and MMP9 were markedly downregulated, while the Bicuculline group showed the opposite results. It can be inferred that the GABA-A receptor agonist Topiramate slows down AAA progression by inhibiting p38MAPK phosphorylation and reducing MMP secretion, while the GABA-A receptor antagonist Bicuculline produces the opposite effects.
The results of this study are encouraging, but there are certain limitations in the experimental design. First, a vernier caliper was used to measure abdominal aortic dilation in this study. While this method is reliable for static measurements, it does not allow for real-time dynamic observation. In contrast, ultrasound imaging can provide more accurate monitoring of arterial dilation progression and offers the advantages of continuity and non-invasiveness. Therefore, the lack of ultrasound technology for monitoring AAA progression is a major limitation of this study. In future research, we will prioritize incorporating ultrasound imaging to address the shortcomings of the current method and enhance the monitoring of AAA progression. Second, although the elastase combined with calcium chloride model closely mimics inflammation, it lacks the atherosclerotic characteristics unique to human AAA. Thus, the results of this study still need to be validated in an angiotensin II-induced AAA model. Finally, this study found significant B-cell infiltration in the AAA rat model, and GABA-A receptor agonist Topiramate was shown to have an inhibitory effect on this infiltration. However, there are currently no reports of GABA-A receptor expression on B cells. Given that B cell responses require T cell assistance, it is hypothesized that the inhibition of T cells may indirectly affect B cell activation. Therefore, future research should verify whether the role of B cells in AAA is T cell-dependent or investigate whether B cells express GABA-A receptors at the cellular level, which will be a key focus of our future studies.
Conclusion
Regulating GABA-A receptor activity significantly impacts the development of AAAs in rats. The GABA-A receptor agonist topiramate reduces the infiltration of inflammatory cells, particularly T cells, and modulates the balance of Th1/Th2 cytokines, thereby decreasing the inflammatory response. Additionally, topiramate inhibits the secretion of matrix metalloproteinases MMP2 and MMP9, which reduces extracellular matrix degradation and slows the progression of aneurysms. In contrast, the GABA-A receptor antagonist bicuculline exacerbates inflammation and accelerates aneurysm development. These effects may be mediated through the inhibition or activation of the p38 MAPK signaling pathway.
Data availability
The datasets during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
De Freitas, S., D’Ambrosio, N. & Fatima, J. Infrarenal Abdominal aortic Aneurysm[J]. Surg. Clin. North. Am. 103 (4), 595–614 (2023).
Puertas-Umbert, L. et al. Novel pharmacological approaches in abdominal aortic aneurysm[J]. Clin. Sci. (Lond). 137 (15), 1167–1194 (2023).
Jeanmonod, D., Yelamanchili, V-S. & Jeanmonod, R. Abdominal Aortic Aneurysm Rupture[J]. (2023).
Melin, L-G. et al. Cycloastragenol Inhibits Experimental Abdom. Aortic Aneurysm Progression[J] Biomedicines, 10(2). (2022).
Liu, X. et al. Platelet protects angiotensin II-driven abdominal aortic aneurysm formation through inhibition of inflammation[J]. Exp. Gerontol., 159111703. (2022).
Marquez-Sanchez, A-C. & Koltsova, E-K. Immune and inflammatory mechanisms of abdominal aortic aneurysm[J]. Front. Immunol., 13989933. (2022).
Shan, Y. et al. Understanding the function of the GABAergic system and its potential role in rheumatoid arthritis[J]. Front. Immunol., 141114350. (2023).
Ngo, D-H. et al. GABA-enriched rice bran inhibits inflammation in LPS-stimulated macrophages via suppression of TLR4-MAPK/NF-kappaB signaling cascades[J]. J. Food Biochem. 46 (12), e14421 (2022).
Zhu, J. X. et al. Establishment of a New Abdominal aortic aneurysm model in rats by a Retroperitoneal Approach[J]. Front. Cardiovasc. Med., 9. (2022).
Kudin, A-P. et al. The mechanism of neuroprotection by topiramate in an animal model of epilepsy[J]. Epilepsia 45 (12), 1478–1487 (2004).
Ren, S. et al. A midbrain GABAergic circuit constrains wakefulness in a mouse model of stress[J]. Nat. Commun. 15 (1), 2722 (2024).
Yang, L-X. et al. C1Q labels a highly aggressive macrophage-like leukemia population indicating extramedullary infiltration and relapse[J]. Blood 141 (7), 766–786 (2023).
Ronkko, S. et al. Biocompatibility of different poly(lactide-coglycolide) polymers implanted into the subconjunctival space in rats[J]. Ophthalmic Res. 46 (2), 55–65 (2011).
Zhang, L. et al. Recombinant ACE2 protein protects against acute lung injury induced by SARS-CoV-2 spike RBD protein[J]. Crit. Care. 26 (1), 171 (2022).
Kaneko, Y. et al. Oxytocin modulates GABA(A)R subunits to confer neuroprotection in stroke in vitro[J]. Sci. Rep., 635659. (2016).
Liu, S. et al. Endoscopy Deliverable and Mushroom-Cap-inspired hyperboloid-shaped drug-Laden Bioadhesive Hydrogel for stomach perforation Repair[J]. ACS Nano. 17 (1), 111–126 (2023).
Chen, J-W. et al. Transient upregulation of EGR1 signaling enhances kidney repair by activating SOX9(+) renal tubular cells[J]. Theranostics 12 (12), 5434–5450 (2022).
Tang, H. et al. Injectable ultrasonic sensor for wireless monitoring of intracranial signals[J]. Nature 630 (8015), 84–90 (2024).
Lu, L. et al. New perspectives on YTHDF2 O-GlcNAc modification in the pathogenesis of intervertebral disc degeneration[J]. Mol. Med. 30 (1), 180 (2024).
Zhang, Y. et al. Increased expression of mesencephalic astrocyte-derived neurotrophic factor (MANF) contributes to synapse loss in Alzheimer’s disease[J]. Mol. Neurodegener. 19 (1), 75 (2024).
Wang, C. et al. SPOCK2 modulates neuropathic pain by interacting with MT1-MMP to regulate astrocytic MMP-2 activation in rats with chronic constriction injury[J]. J. Neuroinflammation. 21 (1), 57 (2024).
Tian, Z. et al. Gut microbiome dysbiosis contributes to abdominal aortic aneurysm by promoting neutrophil extracellular trap formation[J]. Cell. Host Microbe. 30 (10), 1450–1463 (2022).
Deak, M. et al. Mitogen- and stress-activated protein kinase-1 (MSK1) is directly activated by MAPK and SAPK2/p38, and may mediate activation of CREB[J]. EMBO J. 17 (15), 4426–4441 (1998).
Lv, L. et al. WT1-AS promotes cell apoptosis in hepatocellular carcinoma through down-regulating of WT1[J]. J. Exp. Clin. Cancer Res., 34119. (2015).
Li, Y. et al. 7-Dehydrocholesterol dictates ferroptosis sensitivity[J]. Nature 626 (7998), 411–418 (2024).
Zheng, H. et al. PDGFRalpha(+)ITGA11(+) fibroblasts foster early-stage cancer lymphovascular invasion and lymphatic metastasis via ITGA11-SELE interplay[J]. Cancer Cell. 42 (4), 682–700 (2024).
Chen, X. et al. Modulating Neuro-Immune-Induced Macrophage polarization with Topiramate attenuates experimental abdominal aortic Aneurysm[J]. Front. Pharmacol., 11565461. (2020).
Feige, T. et al. GP VI-Mediated platelet activation and procoagulant activity aggravate inflammation and aortic Wall Remodeling in Abdominal aortic Aneurysm[J]. Arterioscler. Thromb. Vasc Biol. 44 (11), 2294–2317 (2024).
Karayiannis, I. et al. Induction of MMP-3 and MMP-9 expression during Helicobacter pylori infection via MAPK signaling pathways[J]. Helicobacter 28 (4), e12987 (2023).
Zhu, J-X. et al. Establishment of a New Abdominal aortic aneurysm model in rats by a Retroperitoneal Approach[J]. Front. Cardiovasc. Med., 9808732. (2022).
Das, R. et al. Medroxyprogesterone acetate positively modulates specific GABA(A)-receptor subtypes - affecting memory and cognition[J]. Psychoneuroendocrinology, 141105754. (2022).
Giraudo, A. et al. Five-membered N-Heterocyclic scaffolds as novel amino bioisosteres at gamma-aminobutyric acid (GABA) type A receptors and GABA Transporters[J]. J. Med. Chem. 62 (12), 5797–5809 (2019).
Loebrich, S. et al. Activated radixin is essential for GABAA receptor alpha5 subunit anchoring at the actin cytoskeleton[J]. EMBO J. 25 (5), 987–999 (2006).
Backstrom, T. et al. The GABA system, a new target for medications against cognitive impairment-Associated with neuroactive steroids[J]. J. Intern. Med. 294 (3), 281–294 (2023).
Marcinkowska, M. et al. Dual molecules targeting 5-HT(6) and GABA-A Receptors as a New Approach to Combat Depression Associated with Neuroinflammation[J]. ACS Chem. Neurosci. 14 (8), 1474–1489 (2023).
Forester, N-D. et al. Functional characterization of T cells in abdominal aortic aneurysms[J]. Immunology 115 (2), 262–270 (2005).
Blassova, T. et al. Inflammatory cell infiltrates, hypoxia, vascularization, pentraxin 3 and osteoprotegerin in abdominal aortic aneurysms - a quantitative histological study[J]. PLoS One. 14 (11), e224818 (2019).
Bobryshev, Y-V., Lord, R-S. & Parsson, H. Immunophenotypic analysis of the aortic aneurysm wall suggests that vascular dendritic cells are involved in immune responses[J]. Cardiovasc. Surg. 6 (3), 240–249 (1998).
Kumar, S. & Kaur, G. Second generation anti-epileptic drugs adversely affect reproductive functions in young non-epileptic female rats[J]. Eur. Neuropsychopharmacol. 24 (10), 1709–1718 (2014).
Verrotti, A. et al. Epilepsy, sex hormones and antiepileptic drugs in female patients[J]. Expert Rev. Neurother. 9 (12), 1803–1814 (2009).
Bauer, J. et al. The impact of epilepsy surgery on sex hormones and the menstrual cycle in female patients[J]. Seizure 9 (6), 389–393 (2000).
Cunha, F. F. D. et al. Extracellular vesicles isolated from mesenchymal stromal cells modulate CD4 + T lymphocytes toward a Regulatory Profile[J]. Cells 9 (4), 1059 (2020).
Hirata, H. et al. Th2 cell differentiation from naive CD4(+) T cells is enhanced by autocrine CC chemokines in atopic diseases[J]. Clin. Exp. Allergy. 49 (4), 474–483 (2019).
Li, Z. & Kong, W. Cellular signaling in abdominal aortic Aneurysm[J]. Cell. Signal., 70109575. (2020).
Awasthi, A., Raju, M-B. & Rahman, M-A. Current insights of inhibitors of p38 mitogen-activated protein kinase in Inflammation[J]. Med. Chem. 17 (6), 555–575 (2021).
Maik-Rachline, G., Lifshits, L. & Seger, R. Nuclear P38: roles in physiological and pathological processes and regulation of Nuclear Translocation[J]. Int. J. Mol. Sci., 21(17). (2020).
Ping Gao, G. et al. MKL1 cooperates with p38MAPK to promote vascular senescence, inflammation, and abdominal aortic aneurysm[J]. Redox Biol., 41101903. (2021).
Liu, X. et al. DRD4 (dopamine D4 receptor) mitigate abdominal aortic aneurysm via decreasing P38 MAPK (mitogen-activated protein kinase)/NOX4 (NADPH oxidase 4) Axis-Associated oxidative Stress[J]. Hypertension 78 (2), 294–307 (2021).
Kelley, J-M., Hughes, L-B. & Bridges, S. L. J. Does gamma-aminobutyric acid (GABA) influence the development of chronic inflammation in rheumatoid arthritis[J]. J. Neuroinflammation, 51. (2008).
Acknowledgements
The authors express their gratitude to all participants for their valuable contributions.
Funding
This research was supported by the Sichuan Province Science and Technology Planning Project (2016JY0172) and the Scientific Research Project of Sichuan Provincial Health and Family Planning Commission (16PJ121).
Author information
Authors and Affiliations
Contributions
ZJX conducted experiments, interpreted the data, and drafted the manuscript. YY conceptualized the research design, devised the experimental plan, and revised the manuscript. ZC, GJW and HLZ participated in the experiments. YNP, YF, and ZDY contributed to data analysis. All authors reviewed and approved the final draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All experiments were performed according to guidelines established by the Institutional Animal Care and Use Ethical Committee of North Sichuan Medical College (Sichuan, China).
Consent for publication
The submission to this journal has been read and approved by all coauthors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhu, JX., Zhou, C., Huang, LZ. et al. Intervention effect of regulating GABA-A receptor activity on the formation of experimental abdominal aortic aneurysm in rats. Sci Rep 14, 31388 (2024). https://doi.org/10.1038/s41598-024-82913-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-82913-7
Keywords
This article is cited by
-
Multifunctional nanoparticles in abdominal aortic aneurysm management: from basic research to clinical transformation
Journal of Nanobiotechnology (2025)