Abstract
Prostate cancer, a common malignancy in older men, often requires laparoscopic radical prostatectomy, considered the gold standard treatment. However, postoperative complications can significantly impact quality of life and psychological well-being. The emergence of mobile internet health management offers a promising approach for accessible and effective post-discharge care. This study evaluates the effectiveness of mobile internet management in postoperative care for prostate cancer patients, focusing on disease knowledge, psychological well-being, self-care capabilities, and quality of life. From September 2020 to September 2021, prostate cancer patients who underwent radical surgery at our Department of Urology were divided into a control group receiving standard care and an intervention group receiving mobile internet-based care. Patients were followed over six months, with assessments conducted at both 3 and 6 months post-intervention. We evaluated changes in disease knowledge, psychological status (using SAS/SDS scales), self-care ability (via the ESCA scale), and quality of life (measured by SF-36). A total of 112 patients were divided into two groups of 56 each. Repeated measures ANOVA indicated significant improvements in disease knowledge over time, between groups, and in their interaction (P < 0.05). Mastery scores of disease knowledge increased at both 3 and 6 months post-intervention compared to baseline (P < 0.05). The intervention group showed significantly reduced scores on the self-rating depression scale (SDS) and self-rating anxiety scale (SAS) compared to the control group (P < 0.05). Self-care capabilities—including self-directed concept, nursing responsibility, skills, and health knowledge level—also improved, with more pronounced gains in the intervention group (P < 0.05). Quality of life scores in domains such as social function, mental health, vitality, role emotional, bodily pain, role physical, physical function, and general health were higher in the intervention group than in the control group post-intervention (P < 0.05). Mobile internet management significantly enhances postoperative care for prostate cancer patients by improving disease knowledge, psychological well-being, self-care capabilities, and quality of life. These findings support further research to validate long-term benefits and broader application potentials.
Similar content being viewed by others
Introduction
Prostate cancer ranks as a prevalent malignancy within the male genitourinary tract, especially among older men1,2. Surgical intervention is frequently the preferred treatment option in clinical settings3. Robot-assisted or traditional laparoscopic radical prostatectomy, has been established as the gold standard for surgically addressing prostate cancer4,5. However, the comprehensive effects of such radical surgeries often lead to postoperative complications including urinary retention, incontinence, thrombosis, and sexual dysfunction6,7. Additionally, the endocrine therapy administered post-surgery can adversely impact a patient’s self-perception and quality of life, with delayed or inadequate guidance exacerbating physical discomfort and fostering negative psychological states like anxiety and depression8,9,10. Hence, extending multifaceted continuing care to patients post-radical prostatectomy discharge is crucial for enhancing their and their families’ disease management capabilities.
In China, ongoing care primarily revolves around telephonic follow-ups, a method that presents challenges for the less educated and older populations11. The COVID-19 pandemic has further complicated in-person follow-ups and visits due to heightened infection risks and general uncertainties surrounding the outbreak12. This scenario has paved the way for mobile internet health management models, which, free from temporal and geographical constraints, offer broad, convenient, and rapid services13,14. These platforms have proven themselves as safe, effective means of providing patient care during the pandemic, curtailing unnecessary movement and thus aiding in pandemic management. Moreover, internet-based nursing services, part of the broader telemedicine framework, promise to refine medical service delivery, alleviate hospital bed shortages, and address the imbalance between healthcare supply and demand, positioning themselves as the future of hospital innovation15,16,17. However, clinical studies on this model are scant, prompting this investigation into the effectiveness of mobile internet management in the postoperative care of radical prostatectomy patients.
Materials and methods
General information
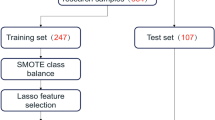
Between September 2020 and September 2021, we retrospectively selected prostate cancer patients who were admitted to the Department of Urology at our hospital and underwent radical surgery as participants for our study. Participants were allocated based on clinical eligibility criteria rather than random assignment, ensuring comparable demographic and clinical characteristics, such as age and education level, across both groups. The eligibility criteria for participation included: (1) being diagnosed with prostate cancer through prostate biopsy and disease stage evaluation and having undergone laparoscopic radical prostatectomy; (2) patients and their accompanying family members being in a stable mental state; (3) having the ability to understand normally, without communication obstacles, and being capable of using internet-enabled devices such as smartphones; and (4) giving informed consent by both patients and their families. Conversely, we excluded individuals from the study based on the following conditions: (1) having severe concurrent diseases in other systems; (2) suffering from psychiatric or consciousness disorders or cognitive impairments; (3) experiencing a worsening of their condition or other diseases; and (4) inability of patients and caregivers to participate cooperatively in the study or deciding to withdraw for any reason. There were no dropouts during the study period, allowing for complete data collection and analysis. The study was approved by the Ethics Committee of The Second Xiangya Hospital of Central South University (K20201203). All methods were performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients whose data were included in this study.
Method
In this retrospective study, both patient groups received standard perioperative care during their hospital stay. Upon discharge, each patient was provided with comprehensive discharge instructions, a specialized health guide for postoperative prostate cancer management, and enrolled in a structured 6-month follow-up program.
The control group continued with a traditional care model, receiving discharge instructions and a departmental contact number for any further questions. They were also provided educational materials on prostate cancer, guidance on managing their health at home, and information on rehabilitation options. For those requiring additional information, department-specific health education was available. Patients in this group were encouraged to follow their prescribed medication plans and attend regular outpatient follow-up visits. Additionally, supportive measures, including patient associations and seminars organized as a platform for shared experiences and learning, were provided to both the control and intervention groups, ensuring equal access to these opportunities. Follow-up calls at 1, 3, and 6 months post-discharge aimed to assess surgical healing progress, monitor physical activity, dietary habits, sleep quality, medication adherence, and mental well-being. These interactions also provided an opportunity for personalized advice. Surveys and questionnaires were distributed to facilitate follow-up processes, ensuring timely feedback and effective monitoring of outcomes.
The intervention group, in contrast, was supported by an enhanced digital care model using mobile internet technology to augment the follow-up process. This approach consisted of the following elements:
(a) Digital nursing management team
A team of 14 specialized members was formed to coordinate this digital intervention. This team included a head nurse who managed the project, two urology nurses who gathered patient queries via WeChat, six nurse practitioners responsible for responding to these inquiries, and two practitioners who uploaded responses to the group. Additionally, a chief urology surgeon, a resident, and an attending surgeon addressed surgical-related questions, with two surgeons providing online answers.
(b) Group management workflow
Upon enrollment, intervention group patients were incorporated into a digital management system, setting up profiles, completing daily check-ins, and engaging with questionnaires to provide feedback. Queries from telephone consultations, organized each morning, were vetted by the head nurse and addressed promptly. Team members proficiently managed these processes using internet tools.
(c) Health promotion via mobile internet
Informational content was shared weekly on WeChat, covering topics like oral medication management, surgical care, nutrition, and recent prostate cancer treatment advancements. Patients and their families were able to ask questions, with responses guaranteed within 12 h. This forum also welcomed relatives, offering a broader support network. Questions outside urology were directed to appropriate specialists for comprehensive answers.
This digital model prioritized privacy and personalized communication, allowing intervention group patients to discuss sensitive matters directly with team members on WeChat. The team analyzed feedback from the intervention group to tailor educational support to meet individual needs, covering aspects such as tube care (e.g., drainage bag replacement, infection management), wound care, venous access maintenance, and lifestyle advice for those undergoing endocrine therapy. Additionally, the initiative included health consultations, home care instructions, and standardizing pelvic floor muscle exercises guidance provided exclusively to the intervention group, supporting recovery and adjustment post-surgery.
Each intervention group patient’s information was meticulously documented in personal profiles, capturing details such as name, address, contact details, prognosis, endocrine therapy status, and past follow-up records. A specially designed follow-up questionnaire assessed patients’ and families’ understanding of discharge instructions. Our team ensured thorough questionnaire collection, frequently communicated the importance of these follow-up activities for optimal recovery, and carried out follow-ups rigorously.
After a 6-month period, both groups attended an outpatient follow-up appointment. This session allowed for a comparative assessment of outcomes between the groups, yielding insights into the effectiveness of the internet-based follow-up in supporting post-discharge patient recovery.
Observation outcomes
Mastery of disease knowledge
A questionnaire, developed from literature reviews and urologist consultations, assessed knowledge across five areas: disease specifics, treatment options, follow-up care, complication prevention, and daily management. Comprising 100 questions, scores were categorized as follows: above 80 (good knowledge), 60–80 (basic understanding), and below 60 (poor knowledge). The questionnaire demonstrated high reliability and validity, with a Cronbach’s alpha of 0.840.
Psychological well-being
Psychological well-being was assessed using self-rating anxiety and depression scales (SAS/SDS)18, each containing 20 questions, with higher scores indicating greater anxiety or depression.
Self-care capability
The Evaluation Scale of Self-care Ability (ESCA)19, with a total score of 172, was used to measure self-care skills. Lower scores indicated reduced self-care ability.
Quality of life
The Chinese version of the SF-3620 survey, a recognized quality-of-life measure covering eight domains (social functioning, mental health, vitality, role-emotional, role-physical, bodily pain, physical functioning, and general health), was employed, with higher scores indicating better quality of life.
Statistical analysis
we utilized SPSS version 22.0 (IBM, Armonk, NY, USA) to meticulously analyze the collected data. Categorical data were presented as counts and percentages (n, %) and analyzed using the chi-square (χ2) test for between-group comparisons. Continuous data were represented as mean and standard deviation (mean ± SD), with the independent samples t-test applied for comparisons between groups. Within-group comparisons over time were assessed using the paired samples t-test. For evaluating changes in continuous variables across multiple time points, we employed repeated measures analysis of variance (ANOVA). A p-value of less than 0.05 was deemed indicative of statistical significance.
Results
Understanding of disease
A total of 112 patients were retrospectively included in the study and divided into two groups: a control group and a study group, with 56 patients in each group. We evaluated patients’ understanding of their condition before the intervention, as well as 3- and 6-months post-intervention and no significant differences between the two groups were obtained, including age, education level, marital status and disease stages (p > 0.05, Table 1). The analysis of variance (ANOVA) showed notable differences over time, between groups, and in their interaction regarding knowledge about the disease (p < 0.05). Notably, both groups saw an increase in disease knowledge scores 3- and 6-months post-intervention compared to before the intervention (p < 0.05). Moreover, the study group demonstrated greater mastery of disease knowledge than the control group at both these time points, with 3 months (79.00 ± 2.90 vs. 70.87 ± 3.36) and 6 months (82.73 ± 3.77 vs.75.72 ± 3.56) (Table 2; Fig. 1).
Psychological well-being
Following the intervention, there was a significant decrease in the self-rating depression (SDS) and anxiety scores (SAS) in both groups (p < 0.05) (Table 3). Importantly, reductions in both SDS (23.47 ± 6.38 vs.16.78 ± 5.29) and SAS (28.51 ± 6.61 vs.22.66 ± 6.47) scores were more pronounced in the study group than in the control group post-intervention (p < 0.05).
Capability in self-care
Post-intervention, both groups exhibited significant improvements in scores for self-care concepts, nursing responsibility, self-care skills, and health knowledge, as well as overall scores on the ESCA scale (p < 0.05) (Table 4). The study group, in particular, scored higher than the control group in these aspects after the intervention, with self-care concepts (69.93 ± 10.49 vs. 64.46 ± 10.25), nursing responsibility (64.42 ± 10.22 vs. 57.74 ± 10.37), self-care skills (72.48 ± 8.40 vs. 68.84 ± 8.33), and health knowledge (86.69 ± 11.46 vs. 78.6 ± 9.67), as well as overall scores (293.55 ± 32.69 vs. 269.70 ± 32.76) on the ESCA scale (p < 0.05).
Quality of life
There was a significant improvement in the quality of life dimensions, including social functioning (SF), mental health (MH), vitality (VT), role emotional (RE), bodily pain (BP), role physical (RP), physical function (PF), and general health (GH) following the intervention (Table 5) (p < 0.05). The study group outperformed the control group in all these quality of life aspects after the intervention, with SF (81.84 ± 11.21 vs. 74.34 ± 9.77), MH (75.73 ± 8.23 vs. 63.18 ± 7.23), VT (78.87 ± 11.31 vs. 71.22 ± 9.19), RE (86.28 ± 11.18 vs. 78.37 ± 9.64), BP (69.79 ± 10.32 vs. 64.39 ± 10.48), RP (64.21 ± 10.47 vs. 58.42 ± 10.13), PF (72.5 ± 8.35 vs.68.64 ± 8.27), and GH (529.30 ± 56.20 vs. 478.59 ± 49.99) (p < 0.05).
Discussion
As minimally invasive extracorporeal endovascular surgeries, including radical prostatectomy, continue to evolve, postoperative care, particularly after patient discharge, remains a significant challenge21. In the era of digital information, mobile online learning has gained traction in managing health outside the hospital for cancer patients, earning widespread patient endorsement22,23. Despite the abundance of disease-related information available online, filtering and identifying relevant content remains a challenge24. Addressing this issue, our study leveraged mobile internet management to deliver information-rich continuing care to post-surgical prostate cancer patients. This approach transcended the traditional limitations of time and space associated with out-of-hospital care, facilitating accurate comprehension of prostate cancer-related information among patients and their families.
Contrasting with a previous study25, which focuses on the global incidence of prostate cancer and underscores the negative impact of postoperative complications like urinary incontinence and sexual dysfunction on life quality, our research introduces an innovative mobile internet management model. While they explores the potential of an eHealth intervention, electronic Patient Activation in Treatment at Home (ePATH), to alleviate symptom burden and enhance quality of life through improved self-care management25, our study seeks to expand on these findings by assessing the utility of mobile internet management in continuous patient care post-surgery. The mentioned study adopts a pragmatic multicenter, block-randomized controlled trial to evaluate the effectiveness of combining standard care with ePATH against standard care alone, with an emphasis on patient activation, motivation, well-being, and health literacy over time25. Our research aims to build upon this foundation by exploring the broader applications of mobile internet in postoperative patient management, potentially offering a more versatile and accessible solution for ongoing care in the evolving digital health landscape.
Our study demonstrated that after 3 and 6 months of intervention, patients’ understanding of their disease significantly improved, especially in the group receiving mobile internet management. This method allowed patients easy access to timely, relevant information through platforms like WeChat, with responses guaranteed within 12 h. Regular updates with the latest disease-related knowledge via a mobile health education system had effectively enhanced patients’ awareness and understanding of their condition post-radical prostatectomy. Given the invasive nature of radical prostatectomy and the psychological stress it often induced, affecting patients’ postoperative mental and emotional wellbeing, it’s common for patients to undergo adverse emotional states during and after surgery26,27. Our results and previously reports confirmed that the mobile internet management approach addresses these challenges by providing timely, accessible information and support, significantly impacting patients’ recovery and overall mental health28,29.
After the intervention, both the self-rating depression scale (SDS) and the self-rating anxiety scale (SAS) scores were significantly lower in the study group compared to the control group. This indicates that mobile internet management positively impacts the emotional wellbeing of patients following radical prostatectomy. The improvement is attributed to two main factors. Firstly, the management team’s detailed analysis of feedback from patients and their families allowed for a deeper understanding of patients’ psychological states, knowledge levels, and social support, enabling personalized guidance to enhance their medical experience and mental health. Secondly, involving family members in the care process and providing them with proper caregiving guidance fostered a supportive family care environment, helping alleviate patients’ negative emotions. Patient-led sharing sessions further boosted confidence and promoted a positive outlook30.
Additionally, post-intervention, both groups showed increased Evaluation Scale of Self-Care Agency (ESCA) scores, with the study group exhibiting more significant improvements in self-directed care, responsibility, skills, and health knowledge. This suggests that mobile internet management effectively boosts patients’ self-care capabilities31. Through a structured guidance model, dedicated follow-up, and an organized internet management team, the program ensured comprehensive postoperative care, aiding patients in transitioning smoothly from hospital to home care.
Moreover, quality of life, as measured by the SF-36 scores, improved more in the study group post-intervention, indicating that mobile internet management enhances life quality for post-radical prostatectomy patients. Considering the majority of prostate cancer patients are elderly, factors such as diminished physical function and the complex, lengthy treatment process significantly impact their quality of life32. This study tailored the intervention process to individual patient needs and management of complications, standardizing pelvic floor muscle exercises to improve urinary control post-surgery, thereby facilitating continuity of care akin to hospital-level care at home. This approach not only reduced rehabilitation costs and hospital visits but also minimized the logistical challenges posed by external factors like weather and transportation. Overall, mobile internet management proved effective in enhancing disease understanding, self-care capabilities, and emotional wellbeing among postoperative prostate cancer patients.
Our study presented several limitations. Our retrospective study provided preliminary but promising insights into the application of mobile internet management for the continuing care of patients following radical prostatectomy. For our research methodology, we utilized mobile-based chat tools. While this approach may not be groundbreaking in the research landscape, its convenience and effectiveness had been validated across numerous studies, making it an undeniably practical choice. Although our sample size was modest, the preliminary results appeared to support the hypothesis, indicating positive effects of mobile internet management on aspects such as patient knowledge, emotional well-being, and self-care capabilities. Looking ahead, prospective randomized controlled trials are essential to further substantiate these findings. It was also worth noting that the assessment tools employed in this study, including the Self-Rating Depression Scale, Self-Rating Anxiety Scale, and the Self-Care Ability Evaluation Scale, while not novel or prostate cancer-specific, are nevertheless classic and widely used instruments. Their extensive application in various studies provides a robust basis for our research outcomes. Despite their broad utility, the exploration of their specificity and sensitivity within the specific context of prostate cancer patients remains an area for future research. In a short, although this study navigates certain limitations, including the use of non-novel and non-disease-specific scales, its findings offer valuable insights into the role of mobile internet management in the postoperative care domain, paving the way for future research directions.
Conclusions
In conclusion, our study demonstrated that utilizing mobile internet management for the ongoing care of patients who have undergone radical prostatectomy yields significant benefits. It notably enhanced patients’ understanding of their condition, reduces negative emotional states, and bolsters both self-care competencies and overall quality of life. However, it’s important to acknowledge that this investigation primarily focused on the short to medium-term effects of such interventions. The long-term impacts remain unexplored and present a critical avenue for future research. To fully understand the scope and durability of the benefits observed, further studies with larger sample sizes and potentially more targeted assessment tools are warranted.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding authors on reasonable request.
Abbreviations
- BP:
-
Bodily pain
- COVID-19:
-
Coronavirus disease 2019
- ESCA:
-
Evaluation of self-care ability
- GH:
-
General health
- MH:
-
Mental health
- PF:
-
Physical function
- RE:
-
Role emotional
- RP:
-
Role physical
- SAS:
-
Self-rating anxiety scale
- SDS:
-
Self-rating depression scale
- SF:
-
Social function
- VT:
-
Vitality
References
Daniyal, M. et al. Epidemiology, etiology, diagnosis and treatment of prostate cancer. Asian Pac. J. Cancer Prev. 15, 9575–9578 (2014).
Grozescu, T. & Popa, F. Prostate cancer between prognosis and adequate/proper therapy. J. Med. Life. 10, 5–12 (2017).
Sebesta, E. M. & Anderson, C. B. The surgical management of prostate cancer. Semin Oncol. 44, 347–357 (2017).
Azal, W. N. et al. Incontinence after laparoscopic radical prostatectomy: a reverse systematic review. Int. Braz J. Urol. 48, 389–396 (2022).
Checcucci, E. et al. Retzius-sparing robot-assisted radical prostatectomy vs the standard approach: a systematic review and analysis of comparative outcomes. Bju Int. 125, 8–16 (2020).
Mottet, N. et al. Eau-eanm-estro-esur-siog guidelines on prostate cancer-2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. Eur. Urol. 79, 243–262 (2021).
Patel, H. D. et al. Effect of pharmacologic prophylaxis on venous thromboembolism after radical prostatectomy: the preventer randomized clinical trial. Eur. Urol. 78, 360–368 (2020).
Kawaguchi, K. et al. Effect of general self-efficacy on promoting health-related quality of life during recovery from radical prostatectomy: a 1-year prospective study. Int. J. Clin. Oncol. 25, 2122–2129 (2020).
Chen, P. Y. et al. Body image in patients with prostate cancer undergoing treatment with hormone therapy: observational study using both a cross-sectional and longitudinal design. J. Health Psychol. : 1409780614. (2024).
Fischer, V. J., Andersson, G., Billieux, J. & Vogele, C. The relationship between emotion regulation and sexual function and satisfaction: a scoping review. Sex. Med. Rev. 10, 195–208 (2022).
Ding, K., Tang, R. & Yu, J. Recommendations for the management of patients with benign prostatic hyperplasia in the context of the covid-19 pandemic: a retrospective study of 314 cases. Biomed. Res. Int. 2022, 5739574 (2022).
Zhang, X. et al. Symptoms and health outcomes among survivors of covid-19 infection 1 year after discharge from hospitals in wuhan, china. Jama Netw. Open. 4, e2127403 (2021).
Bousquet, J. et al. Mobile technology in allergic rhinitis: evolution in management or revolution in health and care? J. Allergy Clin. Immunol. Pract. 7, 2511–2523 (2019).
Sharma, S. et al. Mobile technology: a tool for healthcare and a boon in pandemic. J. Family Med. Prim. Care. 11, 37–43 (2022).
Zhao, B. et al. Barriers to accessing internet-based home care for older patients: a qualitative study. Bmc Geriatr. 21, 565 (2021).
Wilmink, G. et al. Real-time digital contact tracing: development of a system to control covid-19 outbreaks in nursing homes and long-term care facilities. Jmir Public. Health Surveill. 6, e20828 (2020).
Yan, W. et al. Study on the application of the internet + nursing service in family rehabilitation of common bone and joint diseases in the elderly. Eur. Rev. Med. Pharmacol. Sci. 26, 6444–6450 (2022).
Yue, T. et al. Comparison of hospital anxiety and depression scale (hads) and zung self-rating anxiety/depression scale (sas/sds) in evaluating anxiety and depression in patients with psoriatic arthritis. Dermatology 236, 170–178 (2020).
Guo, L. et al. Testing and comparing two self-care-related instruments among older chinese adults. Plos One. 12, e0182792 (2017).
Li, L. 1, Wang, H. M. & Shen, Y. Chinese SF-36 Health Survey: translation, cultural adaptation, validation, and normalisation. J. Epidemiol. Community Health. 57 (4), 259–263 (2003).
Pan, L. H., Lin, M. H., Pang, S. T., Wang, J. & Shih, W. M. Improvement of urinary incontinence, life impact, and depression and anxiety with modified pelvic floor muscle training after radical prostatectomy. Am. J. Mens Health. 13, 1818129506 (2019).
Paterson, C. et al. The role of telehealth during the covid-19 pandemic across the interdisciplinary cancer team: implications for practice. Semin Oncol. Nurs. 36, 151090 (2020).
Elkefi, S., Trapani, D. & Ryan, S. The role of digital health in supporting cancer patients’ mental health and psychological well-being for a better quality of life: a systematic literature review. Int. J. Med. Inf. 176, 105065 (2023).
Jang, B., Kim, M., Kim, I. & Kim, J. W. Eagleeye: a worldwide disease-related topic extraction system using a deep learning based ranking algorithm and internet-sourced data. Sens. (Basel) ; 21. (2021).
Ekstedt, M. et al. Enhanced patient activation in cancer care transitions: protocol for a randomized controlled trial of a tailored electronic health intervention for men with prostate cancer. Jmir Res. Protoc. 8, e11625 (2019).
Vitous, C. A., Byrnes, M. E., De Roo, A., Jafri, S. M. & Suwanabol, P. A. Exploring emotional responses after postoperative complications: a qualitative study of practicing surgeons. Ann. Surg. 275, e124–e131 (2022).
Pompe, R. S. et al. The impact of anxiety and depression on surgical and functional outcomes in patients who underwent radical prostatectomy. Eur. Urol. Focus. 6, 1199–1204 (2020).
Fleddermann, K. et al. Patient preferences for mobile health applications to support recovery. J. Addict. Med. 17, 394–400 (2023).
Wu, Y. et al. Mobile nutrition and health management platform for perioperative recovery: an interdisciplinary research achievement using wechat applet. Front. Med. (Lausanne). 10, 1201866 (2023).
Farr, M. et al. Experiences of patient-led chronic pain peer support groups after pain management programs: a qualitative study. Pain Med. 22, 2884–2895 (2021).
Aminuddin, H. B., Jiao, N., Jiang, Y., Hong, J. & Wang, W. Effectiveness of smartphone-based self-management interventions on self-efficacy, self-care activities, health-related quality of life and clinical outcomes in patients with type 2 diabetes: a systematic review and meta-analysis. Int. J. Nurs. Stud. 116, 103286 (2021).
Droz, J. P. et al. Management of prostate cancer in elderly patients: recommendations of a task force of the international society of geriatric oncology. Eur. Urol. 72, 521–531 (2017).
Acknowledgements
We acknowledge the medical and nursing staff and all patients who participated in the study.
Funding
This study was supported by a grant from the Hunan Province Science and Technology Department’s Innovative Province Construction Special Project - Popular Science Special Project (2022 ZK4079). The funder had no role in the study design, data analysis, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
SP, XJ and LH designed the study, collected data, conducted the statistical analysis, and wrote the manuscript. LY and YW revised the paper. All authors reviewed and approved the final version for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of The Second Xiangya Hospital of Central South University (K20201203). All methods were performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients whose data were included in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Peng, S., Wei, Y., Ye, L. et al. Application of mobile internet management in the continuing care of patients after radical prostatectomy. Sci Rep 14, 31520 (2024). https://doi.org/10.1038/s41598-024-83303-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-83303-9