Abstract
Children in urban and eastern regions tend to be taller and have higher body mass index (BMI) compared to those in rural and central-western regions, partially due to better family resources. We examined urban‒rural areas, regional differences in growth trajectories, focusing on family influences. Longitudinal data on 8542 children from the China Health and Nutrition Survey (1991–2015) were used. Random effects models assessed the mean height/BMI growth trajectories across different regions, urban–rural areas, and sexes within cohorts born in 1980–1989, 1990–1999, and 2000–2009. In the 1980–1989 cohort, before adjusting for family dietary structure, children from eastern regions were on average 3.3 cm taller than those from central-western regions at age 6. After adjustment, the height difference decreased to 2.44 cm. In the 2000–2009 cohort, the urban–rural BMI difference at age 6 was initially 0.53 kg/m2, which narrowed to 0.40 kg/m2 after adjusting for family socioeconomic factors. After adjusting for family environmental sanitation, the regional difference in the 2000–2009 cohort was attenuated by half before adjustment and was 0.44 kg/m2 after adjustment. Family factors significantly account for the regional and urban–rural disparities in height and BMI. These disparities were driven by the family resource environment, like dietary structure and sanitation. However, with China’s socioeconomic changes, broader socioeconomic factors, including household income and parental education, have become more influential.
Similar content being viewed by others
Introduction
In China, the distinction between urban and rural areas is not only geographical but also significantly driven by socioeconomic status and environmental sanitation. Urban areas typically feature higher household incomes, better educational resources, and superior healthcare services, whereas rural areas face challenges due to poor infrastructure and limited resources. Additionally, the eastern regions of China, being more economically developed and closer to economic centers, generally exhibit better child health and nutrition outcomes compared to the resource-rich but economically lagging central-western regions. These complex urban–rural and regional disparities provide a critical backdrop for our study into children’s growth trajectories1. Growth and development in childhood and adolescence are related to health and well-being throughout the life cycle2. In low-income/middle-income countries, stunting and underweight children (indicators of malnutrition) are associated with excessive disability and mortality3. The rising rates of overweight and obesity among children are now major contributors to cardiovascular risks and mortality later in life4,5,6. James Tanner pointed out in his research that adolescent growth spurt is the most significant nonlinear feature in the growth process, and its onset time and magnitude are significantly influenced by environmental and nutritional conditions7. In addition, Barry Bogin and Robert Malina’s research suggests that children in economically disadvantaged areas typically exhibit delayed onset and slower growth rates during puberty growth spurt8,9. This study combines these theoretical foundations to analyze the differences in adolescent growth spurt between urban and rural children in China and the role of family environmental factors. Additional insights into the urban–rural and regional disparities in the timing and characteristics of childhood growth trajectories would be invaluable for developing targeted policies to reduce health inequalities.
In the context of nutritional health and life processes, some studies have observed SES convergence on nutritional health inequalities, while others have identified persistent disparities between socially and economically advantaged individuals and their disadvantaged counterparts during adolescence. Scholars attribute these inconsistencies to the confounding of age effects (the influence of SES on and nutritional health in an individual’s life) and cohort effect (the influence of SES on and nutritional health in birth cohorts born in different historical periods) in cross-sectional design10. However, these issues are not merely methodological or data-related but also conceptual, as the cohort represents the individual’s historical era. When analyzing the lifelong relationship between SES, nutrition, and health, neglecting the cohort structure means overlooks the impact of societal changes on human life.
Since the 1990s, China has aimed to narrow the urban–rural gap. Considering this historical context is crucial when analyzing urban–rural and regional differences in growth trajectories. There is evidence that with the increase in birth years, both height and body mass index (BMI) have increased, particularly among urban children. However, while an increase in height is generally seen as positive, a higher BMI is not necessarily better, as it may indicate an increased risk of obesity11. Despite the importance of family socioeconomic factors in child growth post-China’s economic reforms, their impact on urban–rural and regional disparities remains underexplored. This area of study is limited by small sample sizes and cross-sectional data when examining regional and urban–rural growth differences12. Many studies fail to distinguish between cohort effect and age effect, thus they cannot simultaneously assess the dynamic impacts of family health initiatives and societal changes on children’s nutritional health, leading to inconsistent results13. There is a lack of multilevel analysis of the impact of objective family factors on children’s health, these family factors like parental education, household income, dietary structure, and environmental sanitation.
To better understand how family factors influence regional and urban–rural differences in growth trajectories across cohorts, we analyzed longitudinal data to investigate the role of family factors in regional and urban‒rural differences in height and BMI across birth cohorts.
Results
Of 22,351 measurements in this study, 10,436 (46.69%) children had more than four repeated measurements (Supplementary Tables S1–S3 and Fig. S1). Table 1 indicates that the median per capita household income increased significantly from 1254.2 to 5100 yuan. The percentage of parents with at least a middle school education rose from 49.46 to 78.2%. The median urbanization index increased from 45 to 60.32. Approximately 33.4% of the children were from the eastern region, while the percentage of ethnic minorities stayed around 14%. More parents lived in rural areas (approximately 72%). Carbohydrate intake decreased, whereas fat and protein intake increased. Family environmental sanitation scores improved across cohorts. Parents’ BMI progressively rose across cohorts, from 22 to 23.11 kg/m2.
Figure 1 illustrates an upward trend in mean height trajectories across cohorts, with children in urban and eastern regions consistently taller than those in rural and central-western regions from ages 0 to 18, for both genders (see red vs. orange bars in Supplementary Tables S5, S6). The urban–rural disparity in mean height, initially widening, diminished with age; the most notable difference occurred at age 13, with boys showing a mean height gap of 4.07 cm (95% CI 0.17, 5.52) in the 1990–1999 cohort. Regional differences in mean height first increased and then decreased with age across all cohorts. Girls at age 10 had the largest differences, which was 7.29 cm (95% CI 5.69, 8.89) in the latest cohorts. We compared the time points of adolescent growth spurt in urban and rural children and found that the growth spurt in urban children occurred on average 1.4 years earlier, which may be related to better nutritional and hygiene conditions (see Supplementary Table S4).
Regional and urban–rural differences in height trajectory by cohorts. Note: (A) Shows mean height (95% CI) trajectories by urban–rural for the earliest and latest cohorts for boys. (B) Shows mean height (95% CI) trajectories by urban–rural for the earliest and latest cohorts for girls. (C) Shows mean height (95% CI) trajectories by regional for the earliest and latest cohorts for boys. (D) Shows mean height (95% CI) trajectories by regional for the earliest and latest cohorts for girls.
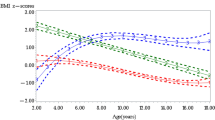
Figure 2 shows that the mean BMI trajectories in the latest cohort were also above those in the earliest cohort and that urban‒rural/regional disparities in BMI growth were much greater in the latest cohort than in the earliest cohort (orange vs. blue bars and corresponding values in Supplementary Tables S7, S8). For urban and rural areas, differences in mean BMI were greatest during adolescence and narrowed slightly thereafter. In the latest cohorts, the largest difference was among 13-year-old boys, which was 0.85 kg/m2 (95% CI 0.09, 1.60). For regional differences, differences in mean BMI were greatest during adolescence and narrowed slightly thereafter. Girls at 10-year-old had the largest difference, 1.45 kg/m2 (95% CI 1.03, 1.88) in the latest cohorts.
Regional and urban–rural differences in BMI trajectory by cohorts. Note: (A) Shows mean BMI (95% CI) trajectories by urban–rural for the earliest and latest cohorts for boys. (B) Shows mean BMI (95% CI) trajectories by urban–rural for the earliest and latest cohorts for girls. (C) Shows mean BMI (95% CI) trajectories by regional for the earliest and latest cohorts for boys. (D) Shows mean BMI (95% CI) trajectories by regional for the earliest and latest cohorts for girls.
Figures 3 and 4 show the role of family socioeconomic and resource environmental factors in mean height/BMI trajectories for both sexes. Regarding regional/urban‒rural differences in mean height, differences in the 1990–1999 and 2000–2009 cohorts were attenuated after adjustment for education and further attenuated after adjustment for household income level (Supplementary Tables S9, S10). Urban‒rural differences decreased after adjustment for family socioeconomic factors (e.g., boy at age 10 years in the 1980–1989 birth cohort, the difference was 2.58 cm (95% CI 1.78, 3.38) before adjustment and 1.87 cm (95% CI 1.06, 2.65) after adjustment). Adjustment for household income level further attenuated urban‒rural and regional differences in mean height. Regarding regions, after adjustment for dietary structure, the urban‒rural/regional differences in mean height in the earliest birth cohort were not significantly reduced, but they were reduced by half in the latest birth cohort. After adjustment for environmental sanitation, the regional differences in mean height were attenuated in the earliest birth cohort (for example, for 6-year-old girls in the 1980–1989 cohort, the differences in mean height were 3.29 cm (95% CI 2.58, 4.01) before adjustment and 2.44 cm (95% CI 1.34, 3.56) after adjustment).
Regional and urban–rural differences in height trajectory by cohorts. Note: (A) Shows the role of family socio-economic factors for boys. (B) Shows the role of family socio-economic factors for girls. (C) Shows the role of family resource environmental factors for boys. (D) Shows the role of family resource environmental factors for girls. A positive value indicates urban/east region are higher than rural/central-west region.
Regional and urban–rural differences in BMI trajectory by cohorts. Note: (A) Shows the role of family socio-economic factors for boys. (B) Shows the role of family socio-economic factors for girls. (C) Shows the role of family resource environmental factors for boys. (D) Shows the role of family resource environmental factors for girls. A positive value indicates urban/east region are higher than rural/central-west region.
Regional/urban‒rural differences in mean BMI in the 1980–1989 and 1990–1999 cohorts were attenuated after adjustment for education and further attenuated after adjustment for household income level (Supplementary Tables S11, S12). In particular, among 6-year-old boys in the latest birth cohort, there was the greatest attenuation in urban‒rural differences in mean BMI, and urban‒rural differences were approximately halved after adjustment for family socioeconomic factors (e.g., at 6 years in the 2000–2009 birth cohort, the urban‒rural differences in mean BMI were 0.53 kg/m2 (95% CI 0.17, 0.88) before adjustment and 0.40 kg/m2 (95% CI − 0.02, 0.82) after adjustment). Adjustment for dietary structure substantially reduced the urban‒rural and regional differences among girls in the earliest birth cohorts. After adjustment for environmental sanitation, the regional differences in the latest birth cohort were attenuated by half (for example, for 6-year-old boys in the 2000–2009 cohort, the regional differences in mean BMI were 1 kg/m2 (95% CI 0.68, 1.33) before adjustment and 0.44 kg/m2 (95% CI − 0.30, 1.17) after adjustment).
Discussion
This study highlights three main findings. Firstly, over nearly 30 years, children in urban and eastern regions exhibited greater height and BMI. Secondly, considering family socioeconomic factors, the differences in BMI and height were reduced in the more recent cohorts. Urban–rural disparities in height decreased in the 1980–1989 and 1990–1999 cohorts, with regional differences halving. Thirdly, across all cohorts and ages, mean height and BMI were consistently higher in urban and eastern regions, even after adjusting for family socioeconomic and resource environmental factors. The height gap typically narrowed between ages 6 and 10, once family factors were considered. Similarly, the BMI gap narrowed during puberty, between ages 10 and 13.
Although this study focuses on China, its findings have broader implications for low- and middle-income countries facing rapid urbanization and regional disparities. Similar socioeconomic transitions in other nations suggest that the impact of urbanization on child growth patterns may be a global phenomenon14. Understanding how family socioeconomic status and resource environmental factors interact offers crucial insights for creating adaptable public health interventions across various cultural contexts. Applying these insights can help other countries more effectively address health inequalities and support child development. Our research results indicate that there is a significant difference in the onset time of adolescent growth spurt among urban and rural children in China, which is consistent with the theory proposed by James Tanner on the impact of environment and nutrition on growth. In addition, this finding contrasts with similar studies on urban and rural children in Guatemalan8, further demonstrating the crucial role of economic development and family resources in growth patterns. This study provides new data support for policy-making through model innovation and large sample analysis.
A strength of this research is the examination of family socioeconomic status and environmental differences in children’s nutritional health throughout their lives. Given the social and economic changes since the late 1970s, understanding how these changes influence children’s life trajectories are crucial. Considering the differences in birth cohorts helps contextualize the life cycle and inequality, thus clarifying the dynamics between social changes and individual lives. Our research highlights significant short-term variations in children’s nutritional health trajectories. Ignoring this source of variation biases the relationship among family SES, age and health. In general, our findings revealed a high family SES group on a healthy track in the cohort and different family SES patterns of nutritional health between cohorts.
The disparities in urban and rural environments, particularly in terms of resources, explain the differences in family resource environmental factors starting from school age13,15. The school-age period is critical for children’s development16. As age increased, the average height differences between regions neither converged nor expanded. Approximately 80% of differences in height is controlled by genes or biology, and the remaining 20% is determined by environmental factors such as nutrition, disease, living conditions and psychological pressure17,18. At the same time, height differences between regional/urban‒rural areas gradually narrowed and improved. Our findings align with previous studies showing that rural children aged 7–18 years have a higher growth rate in height compared to urban children19. This suggests that children in rural areas are reaching their genetic potential for height by benefiting from improved living conditions. Meanwhile, adolescents in rural and western areas are reducing the height gap with their urban counterparts by accessing better nutrition and energy.
Each generation of children has undergone distinct social development. To a large extent, China’s social and economic structure was formed after the beginning of the economic reform in the early 1980s20. Children in the 1990s and 2000s coincided with China’s accession to the World Trade Organization (WTO)21, and rapid urbanization and nutrition changes substantially increased children’s BMI22. Our study noted that with the rapid economic development in rural areas and changes in people’s diets, the overweight and obesity rates among rural children also rose rapidly. National decision-making departments and public health institutions should not ignore this trend. From a regional perspective, the main reason for these higher rates is the unbalanced economic development among regions. The relationship between socioeconomic status and BMI in China reflects the broader phenomenon of the ‘nutrition transition’, where rapid economic development leads to shifts in dietary patterns and physical activity, resulting in increased obesity rates among lower socioeconomic groups23.
Rationalizing diet structures and enhancing family resource environment can mitigate height disparities between urban and rural areas24. Furthermore, the correlation weakened over successive cohorts: early improvements in family environmental health spurred growth in rural and central-western children, whereas the influence of family socioeconomic status became more pronounced in later cohorts. One explanation is that social and economic advancements have reduced resource inequalities between urban and rural areas, significantly improving sanitation. However, social stratification continues to persist. The social identity formed by urban and rural household registration, as well as the “nested” identity formed by a provincial identity, have considerable differences in nutrition and health25. The mechanism behind these differences is access to educational resources and the space for income improvement in socioeconomic status. The reduction of inequality mainly comes from the narrowing of the urban–rural education development gap within the region26. Additionally, recent studies have increasingly validated the long-term health benefits of improved water quality. Chinese scholars have proven that drinking water sanitation and toilet hygiene can effectively improve height27.
Individuals with a lower family socioeconomic status may rely more on local resources because they have less ability to purchase goods and services in other ways28. Our research indicated sex-based differences in the effects of family health promotion. After considering family income, the urban and rural differences in girls’ BMI age trajectories were enhanced, while the differences among boys were reduced. In regions with a traditional preference for sons, boys tend to access more family resources. The above results showed that family health promotion largely explains the differences in the trajectories of children’s BMI between urban and rural areas.
Our findings indicate that urban–rural disparities and the differences between eastern and central-western regions significantly impact children’s growth and development. While urban children display better growth indicators due to access to superior resources, children in rural areas also show potential for growth improvement with gradually enhancing infrastructure and sanitary conditions. Moreover, children in eastern regions generally outperform their central-western counterparts in terms of height and BMI, likely due to higher family incomes and better access to education and healthcare resources in the east. However, as China’s economic development becomes more internally balanced and resource allocation improves, we anticipate enhancements in the health conditions of children in central-western regions. This shift suggests that policymakers need to focus on regional balanced development, especially in the distribution of educational and health resources, to reduce the health inequalities driven by these disparities.
This study had some limitations. First, loss to follow-up occurred over time, with 12–20% for each wave, and we applied random effects models that allowed children with different numbers and timing of measurements. Despite methodological improvements, limitations in sample size and inherent challenges in tracking longitudinal growth across diverse age groups persist. These limitations necessitate larger, more comprehensive datasets in future studies. Second, the observed effects reversing after age 12 may relate to schooling, as children spend significant time at school, potentially confounding family-based measures. However, our database lacked school-related variables, which should be considered in future research. Finally, the small size of the 2000–2009 cohort, particularly among older adolescents, likely explains the broader 95% confidence intervals in our estimates. This reduction in sample size over time may have somewhat compromised the accuracy of our estimations.
Methods
Study participants
Data were taken from the China Health and Nutrition Survey (CHNS). The CHNS is an ongoing open cohort study of the National Institute for Nutrition and Health (Chinese Center for Disease Control and Prevention) in collaboration with the Population Center of the University of North Carolina in the United States. The CHNS is the first longitudinal cohort study on the nutrition and health of Chinese residents since 1989, and it is conducted every 2–4 years. The CHNS employs a multistage random cluster sampling method, sampling over 30,000 individuals across 15 provinces. A multistage random clustering sample design was adopted to ensure adequate representation. In each province, provincial capital cities, low-income cities and four (one high-income, two middle-income and one low-income) counties were selected. Two cities and two suburban communities (each city) or one township and three villages (each county) were selected. Each community contributed twenty selected families. In each wave of surveys, community/family/individual-level surveys were conducted by trained field workers. Previous studies have shown that the characteristics of participants in the CHNS are comparable to those of the national sample29,30. In this study, we used data from nine survey periods of the CHNS (1991, 1993, 1997, 2000, 2004, 2006, 2009, 2011, and 2015). Our analysis included 8542 children born between 1980 and 2015 who underwent physical measurements between the ages of 0 and 18 from 1991 to 2015 (twins made up only 0.2% of the survey population) (Fig. S1). To better describe the role of social changes31, we used three birth cohorts (born in 1980–1989, 1990–1999 and 2000–2009) (Supplementary Tables S1–S3).
The survey procedures were reviewed and approved by the institutional review committees of the University of North Carolina at Chapel Hill, and the National Institute of Nutrition and Food Safety, Chinese Center for Disease Control and Prevention in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all participants and/or their legal guardians (for more information, please refer to https://www.cpc.unc.edu/projects/china)32.
Measures
Height and BMI
Our database uses machine-measured body shape data. For each survey wave, height (to the nearest 0.1 cm) and body weight (to the nearest 0.1 kg) were measured twice, after participants removed their shoes, hats and heavy outer garments. The average of two height measures was recorded, and BMI (kg/m2) was calculated. Height-for-age z scores (HAZs) and BMI-for-age z scores (BAZs) were used to define outliers (sex-/age-specific WHO 2007 growth reference).
Regional/urban‒rural and family factors
The division of regions was based on the geographical locations of the eastern and central-western regions of China. The eastern region included Jiangsu, Shandong, Heilongjiang, Liaoning, Beijing, Shanghai and Zhejiang provinces. The central-western regions included Guangxi, Guizhou, Henan, Hubei, Hunan, Chongqing, Shaanxi and Yunnan provinces. The distinction between urban and rural areas was based on whether the respondents lived in rural or urban areas.
Family socioeconomic status
Parental education (highest educational attainment of parents) was classified into high (≥ middle school) and low (< middle school) education groups. Household income per capita for each wave was calculated as the sum of the self-reported annual income of all adult family members divided by household size and inflated to 2015 Chinese currency (Yuan) by adjusting for the consumer price index ratio15. Then, family income was classified into high (≥ the median) and low (< the median) family income groups.
The family resource environment
This encompassed environmental sanitation and dietary structure. The environmental sanitation scores included drinking water hygiene and toilet hygiene. Drinking water hygiene: “What is the source of your household drinking water?”. In this study, “water plant, bottled water/mineral water or purified water” were defined as “treated water = 2”, and “river water and other water sources” were defined as “nontreated water = 1”33. Toilet hygiene: “What type of toilet is in your home?”. In this study, “indoor toilet” was defined as a “household toilet = 2”, and “outdoor toilet” was defined as a “household non-toilet = 1”. Dietary structure: The CHNS recorded the content and amount of food intake in 24 h for all interviewees for 3 consecutive days. During the investigation, the investigators ensured the accuracy of the recorded meals through food pictures and recorded the food intake per family to determine food consumption. The average intake of carbohydrates, protein and fat (g/day) among children in three days was calculated34. The daily protein proportion among children included in this study was analyzed as an indicator of children’s dietary structure35.
Confounding variables
Confounding variables included age (years), sex (male or female), ethnicity (ethnic minority or Han ethnicity), parents’ BMIs, parents’ heights, urbanization index score, and siblings15,36.
Statistical analysis
In responding to the need for a more nuanced understanding of regional and urban–rural disparities in child growth trajectories, we applied a mixed effects model combined with non-restrictive cubic splines to BMI analysis and a Preece–Baines growth model to height analysis, conducting a detailed analysis of growth patterns in specific age groups. Such methodological enhancements enable a more accurate depiction of growth trajectories.
The Preece–Baines growth model was fitted for each individual using nonlinear least squares and, mostly, longitudinal series of data, separate models were fitted for each individual, and the analytical solution for velocity and acceleration was used to estimate the parameters of height spurt, the Preece–Baines growth model was widely reported to fit the height growth in Asian countries24. The age at peak velocity (APHV) and peak height velocity (PHV) were obtained from the Preece–Baines growth model. The APHV was defined as the age at the maximum height velocity. The PHV was defined as the velocity at the maximum spurt velocity. This nonlinear model has five parameters and is inferred by the following equation:
where t = age in years, h1 = height (cm), h0 = height at peak height velocity (cm), S0 and S1 = prepubertal and pubertal rate constants, h0 = height constant (cm) at age \(\theta\), and \(\theta\) = age (years) constant at peak velocity. In analyzing height trajectories using the PB model, we grouped birth cohort, region, rural and urban, and sex for analysis.
Non-restricted cubic spline growth curve models that included a random intercept and slope with an unstructured covariance matrix were used to account for the clustering of measurements (level 1) within individuals (level 2) (see Supplementary Table S13). For BMI, the initial model included urban‒rural area and region, age, birth cohort, urban‒rural area and region by age, birth cohort by age, region, and time-varying variables. We tested the interactions (age terms * urban‒rural/regional area, cohort * urban‒rural/regional area) to assess whether urban‒rural and regional disparities in growth differed across ages and cohorts. For illustration, we depicted mean (95% confidence interval, CI) height and BMI trajectories for the earliest (1980–1989) and latest (2000–2009) cohorts by urban‒rural and regional area. To demonstrate the cohort trend in urban‒rural and regional disparities, we also estimated the differences in mean (95% CI) height and BMI between urban‒rural and regional groups at 6–13 years for each cohort. Higher-order interactions with age were then examined for each of these variates and retained in the model if shown to be significant based on the Wald test (α = 0.05). The model was then adjusted for socioeconomic (education and income) or family resource environmental (dietary structure and environmental sanitation) factors and higher-order interactions of education with age if significant (Supplementary Appendix A).
We used SAS version 9.4 (SAS Institute, Cary, NC, USA) and R 4.2.0 for all statistical analyses. Statistical significance (p < 0.05) was inferred using a two-tailed test.
Data availability
The data used in this study can be obtained from cpc.unc.edu/projects/china.
Abbreviations
- BMI:
-
Body mass index
- CHNS:
-
China Health and Nutrition Survey
- HAZ:
-
Height-for-age z score
- BAZ:
-
BMI-for-age z score
- LMICs:
-
Low-/middle-income countries
- HICs:
-
High-income countries
References
Paciorek, C. J. et al. Children’s height and weight in rural and urban populations in low-income and middle-income countries: a systematic analysis of population-representative data. Lancet Global Health 1(5), E300–E309 (2013).
Simmonds, M. et al. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes. Rev. 17(2), 95–107 (2016).
Victora, C. G. et al. Revisiting maternal and child undernutrition in low-income and middle-income countries: variable progress towards an unfinished agenda. Lancet 397(10282), 1388–1399 (2021).
Chen, M. N. et al. Decomposing and predicting China’s GDP growth: past, present, and future. Popul. Dev. Rev. 44(1), 143 (2018).
O’Connor, T. M. et al. Cultural adaptation of ‘Healthy Dads, Healthy Kids’ for Hispanic families: applying the ecological validity model. Int. J. Behav. Nutr. Phys. Act. 17(1), 52 (2020).
Rodriguez-Martinez, A. et al. Height and body-mass index trajectories of school-aged children and adolescents from 1985 to 2019 in 200 countries and territories: a pooled analysis of 2181 population-based studies with 65 million participants. Lancet 396(10261), 1511–1524 (2020).
Tanner, J. M. Fetus into Man: Physical Growth from Conception to Maturity (Harvard University Press, 1978).
Johnson, W. et al. Inequalities in adiposity trends between 1979 and 1999 in Guatemalan children. Am. J. Hum. Biol. 36(5), e24031 (2024).
Bartowiak, S. et al. Secular change in heights of rural adults in west-central Poland between 1986 and 2016: The transition from pre- to post-communism. Econ. Hum. Biol. 53, 101377 (2024).
Chen, F. N., Yang, Y. & Liu, G. Y. Socioeconomic disparities in health over the life course in China: a cohort analysis. Am. Sociol. Rev. 75(1), 126–150 (2010).
Dong, Y. H. et al. Economic development and the nutritional status of Chinese school-aged children and adolescents from 1995 to 2014: an analysis of five successive national surveys. Lancet Diabetes Endocrinol. 7(4), 288–299 (2019).
Song, Y. et al. Secular trends of obesity prevalence in Chinese children from 1985 to 2010: urban-rural disparity. Obesity 23(2), 448–453 (2015).
Wang, L. M. et al. Body-mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004–18. Lancet 398(10294), 53–63 (2021).
Ogden, C. L. et al. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013–2016. JAMA-J. Am. Med. Assoc. 319(23), 2410–2418 (2018).
Fong, T. C. T. & Ho, R. T. H. Longitudinal measurement invariance in urbanization index of Chinese communities across 2000 and 2015: a Bayesian approximate measurement invariance approach. BMC Public Health 21(1), 1635 (2021).
Ornelas, I. J. et al. Engaging school and family in Navajo Gardening for Health: Development of the Yeego Intervention to promote healthy eating among Navajo children. Health Behav. Policy Rev. 8(3), 212–222 (2021).
de Fluiter, K. S. et al. Association between fat mass in early life and later fat mass trajectories. JAMA Pediatr. 174(12), 1141–1148 (2020).
Ogden, C. L. et al. Trends in obesity prevalence by race and Hispanic origin-1999-2000 to 2017–2018. JAMA-J. Am. Med. Assoc. 324(12), 1208–1210 (2020).
Perkins, C. & DeSousa, E. Trends in childhood height and weight, and socioeconomic inequalities. Lancet Public Health 3(4), E160–E161 (2018).
Liang, Y. & Qi, Y. Developmental trajectories of adolescent overweight/obesity in China: socio-economic status correlates and health consequences. Public Health 185, 246–253 (2020).
Chen, Z. M. et al. Adiposity and risk of ischaemic and haemorrhagic stroke in 0.5 million Chinese men and women: a prospective cohort study. Lancet Global Health 6(6), E630–E640 (2018).
Tan, Y. T., Xu, H. & Zhang, X. L. Sustainable urbanization in China: A comprehensive literature review. Cities 55, 82–93 (2016).
Ma, L. et al. Parent-child resemblance in BMI and obesity status and its correlates in China. Public Health Nutr. 24(16), 5400–5413 (2021).
Chen, L. et al. Association between height growth patterns in puberty and stature in late adolescence: A longitudinal analysis in Chinese children and adolescents from 2006 to 2016. Front. Endocrinol. 13, 882840 (2022).
Zhang, Y. Q. et al. Stunting, wasting, overweight and their coexistence among children under 7 years in the context of the social rapidly developing: Findings from a population-based survey in nine cities of China in 2016. PLoS One 16(1), e0245455 (2021).
Guo, Y. & Li, X. Regional inequality in China’s educational development: An urban-rural comparison. Heliyon 10(4), e26249 (2024).
Gregory, G. Link women’s drinking in pregnancy to child’s health records at birth. BMJ-Br. Med. J. 377, o1049 (2022).
Xin, J. G. et al. Association between access to convenience stores and childhood obesity: A systematic review. Obes. Rev. 22, e12908 (2021).
Du, S. F. et al. A new stage of the nutrition transition in China. Public Health Nutr. 5(1a), 169–174 (2002).
Liang, J. et al. Community context, birth cohorts and childhood body mass index trajectories: Evidence from the China nutrition and health survey 1991–2011. Health Place 66, 102455 (2020).
Kiyoshige, E. et al. Projections of future coronary heart disease and stroke mortality in Japan until 2040: a Bayesian age-period-cohort analysis. Lancet Region. Health-West. Pac. 31, 100637 (2023).
Popkin, B. M. et al. Cohort profile: The China Health and Nutrition Survey-monitoring and understanding socio-economic and health change in China, 1989–2011. Int. J. Epidemiol. 39(6), 1435–1440 (2010).
Saboga-Nunes, L., Medeiros, M. & Bittlingmayer, U. Health literacy impact on nutrition status and water intake in children. Eur. J. Public Health 30, 1244 (2020).
Garcia-Iborra, M. et al. Optimal protein intake in healthy children and adolescents: evaluating current evidence. Nutrients 15(7), 1683 (2023).
Jeans, M. R. et al. Breakfast consumption in low-income Hispanic elementary school-aged children: associations with anthropometric, metabolic, and dietary parameters. Nutrients 12(7), 2038 (2020).
Feng, J. et al. The built environment and obesity: A systematic review of the epidemiologic evidence. Health Place 16(2), 175–190 (2010).
Acknowledgements
This research uses data from the China Health and Nutrition Survey (CHNS). We sincerely thank the National Institute for Nutrition and Health (Chinese Center for Disease Control and Prevention) and the Carolina Population Center at the University of North Carolina at Chapel Hill for designing and conducting the CHNS, as well as all participants and staff involved in the survey. The CHNS has been a critical resource for understanding health and nutrition changes in China, and we are deeply grateful for their efforts and contributions.
Author information
Authors and Affiliations
Contributions
Fang Tang conceived and designed the study. Fang Tang analyzed the data. Fang Tang interpreted the data. Minghe Zhou and Fang Tang wrote the draft of the manuscript. Bo Li and Fang Tang modified the manuscript, Bo Li and Fang Tang reviewed the manuscript. All authors critically revised the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Data used in this article comes from the China Health and Nutrition Survey (CHNS), which was an open data and own ethics approval and consent to participate.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tang, F., Zhou, M. & Li, B. Regional and urban‒rural differences in childhood growth trajectories and the role of family in China. Sci Rep 14, 31938 (2024). https://doi.org/10.1038/s41598-024-83459-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-83459-4