Abstract
This study aims to assess the effectiveness of digital multidisciplinary conferences (MDCs) in preventing imaging-related quality management (QM) events during the coronavirus-disease-19 (COVID-19) pandemic. COVID-19 challenged interdisciplinary exchange and QM measures for patient safety. Regular MDCs between radiologists and intensive care unit (ICU) physicians, introduced in our hospital in 2018, enable re-evaluation of imaging examinations and bilateral feedback. MDC protocols from 2020 to 2021 were analysed regarding imaging-related QM events. Epidemiological data on COVID-19 were matched with MDCs. 333 MDCs including 1324 radiological examinations in 857 patients (median age = 64 (IQR = 55–73) years, 66.7% male) were analysed. MDCs were held within a median of 1 day after imaging (IQR = 1–3). QM events were identified in 2.7% (n = 36/1324) of examinations. This represented a significant decrease compared to a control group from 2018/2019 (QM events identified in 14.0%, p < 0.001). QM incidence remained consistent in the pandemic cohort (regression coefficient estimate = -0.01, 95% confidence interval = [0.000, 0.000], p = 0.68). 81% (n = 29/36) of QM events were report-related, 19% process-related (n = 6/36), and 2.8% indication-related (n = 1/36). In 7.3% (n = 97/1324) of examinations, the patient was affected by COVID-19. With MDCs as an effective feedback mechanism in place, the challenges of the COVID-19 pandemic led to no increase in QM incidence. Notably, COVID status did not impact QM event occurrence.
Similar content being viewed by others
Introduction
Imaging is central in the diagnostic workup but remains prone to error1,2,3. Imaging-related medical error, i.e. quality management (QM) events, may affect the indication for an imaging examination, the procedure of image gaining, and image interpretation4. Multidisciplinary conferences (MDCs) between radiologists and intensive care physicians held in our institution are associated with a reduction of medical error over time4.
The emergence of Severe acute respiratory syndrome 2 (SARS-CoV-2) and coronavirus-disease-19 (COVID-19) led to an enormous burden on healthcare systems around the world5,6. Even years after the onset of the pandemic, the variability in the clinical manifestation of COVID-19 still poses diagnostic and therapeutic challenges7,8. The radiology department has been central in the diagnostic workup: Imaging plays an important role in the evaluation of COVID-19 lung affection, the differentiation to additional bacterial superinfection and the detection of additional infectious foci9,10,11,12,13. Interpretation of COVID-19 chest scans is prone to perception bias and varies inter-individually14,15. Thus, multidisciplinary exchange is important in order to benefit from the experience each specialty has been gaining and to reduce the likelihood of medical error.
Interprofessional consultation between radiologists and clinicians has been shown to improve patient care4,16. However, the pandemic has fundamentally changed the ways of communication. Severe measures, especially the reduction of face-to-face interaction, were taken by governments to reduce viral transmission17. Consequently, direct multidisciplinary exchange has become increasingly difficult when trying to avoid in-person contact. In-person contact was replaced with online meetings, which drastically changes our perception of audio and visual input18,19,20,21. Thus, an analysis of error detection and prevention in times of digitalised interpersonal exchange is essential.
In hospitals, COVID-positive patients are isolated from non-infected patients22 while radiology departments are required to examine both COVID-positive and -negative patients. This side-by-side treatment of infected and non-infected patients is especially resource intensive. Time-consuming protective measures are necessary, e.g., the application of protective gear and special cleaning measures23. Intensive care patients, regardless of their COVID status, require special handling when undergoing imaging, e.g., mobile ventilation. Such measures are personnel-intensive, which may further aggravate existing staff shortages24,25. Severe stress and exhaustive working conditions in healthcare have aggravated during the COVID-19 pandemic and thus potentially increase the likelihood of error26,27,28.
Thus, measures for error prevention and improvement of multidisciplinary communication became ever more important in the situation of the rising COVID-19 pandemic. In our department MDCs had been established as a quality management (QM) initiative previously. Intensive care physicians and radiologists meet regularly to discuss recent radiological examinations and their first written interpretation. As a main alteration in the context of the COVID-19 pandemic, MDCs were held in an online video format in order to comply with social distancing. This study aims at assessing the effectiveness of MDCs in preventing imaging-related QM events during the COVID-19 pandemic.
Methods
QM initiative
MDCs were introduced along with the opening of one medical and one surgical ICU at our hospital in 2018. A detailed description of said MDCs has been published previously4. Prior to the pandemic, MDCs were held in person, but were temporarily switched to an online video format with the introduction of social distancing measures. Radiologists and ICU physicians meet in biweekly conferences, separately for each ICU, to discuss imaging examinations of patients under intensive care treatment. MDCs are not scheduled for public holidays. MDCs follow the principles of common diagnostic demonstrations: recent examinations are enrolled in advance by the treating physicians to allow for adequate preparation. The cases selected require clarification for various reasons including inconclusive clinical presentation, complexity of cases, and open questions regarding imaging. Additionally, examinations of newly admitted patients are usually registered. MDCs are chaired by one of two senior radiologists. Patients are introduced by the treating physicians including clinical presentation, suspected diagnosis, current treatment regime, and clinical question regarding the imaging examination(s). Imaging examinations are demonstrated to all participants in the conference and are re-interpreted by the chairing radiologist. Readings and their implications for further diagnostic tests and treatment are then discussed in a multidisciplinary fashion. To our knowledge, MDCs at our hospital differ from many common radiological demonstrations in that standardised protocols are employed for documentation. QM events, i.e., imaging-related errors, are identified and recorded. QM events are defined as not complying with hospital guidelines in the following categories: indication, procedure and reporting. The classification of an incident as a relevant QM event is left to the case-specific interpretation of the chairing radiologists in consultation with all attendees (examples of QM events are given in supplementary Table 1). Both, oral, and written feedback is provided.
Study population
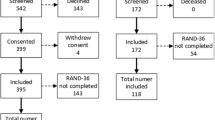
We included all ICU patients who were enrolled in an MDC during the period from 1st of January 2020 through 31st of December 2021 (Fig. 1). All scheduled MDCs were included for analysis (n = 333). Cancelled MDCs, for which no protocol was created, were excluded. One patient may be enrolled in multiple MDCs with different imaging examinations. Exclusion criteria were external and outpatient imaging examinations. We further categorised all examinations by imaging modality including CT, magnetic resonance imaging (MRI), and X-ray. Other imaging modalities, like sonography or positron emission tomography scans (PET-CTs), and interventions were excluded. Examinations were further categorised by body region examined, i.e., head, chest, abdomen, and other. One examination may be included in several body region categories, if more than one body region was examined in one session (e.g. a combined CT of chest and abdomen was included, both in the chest and abdomen category). Approval of the local ethics committee was gathered under the number EA1/024/21 (Ethikkommission Charité – Universitätsmedizin Berlin). Informed consent has been waived by Ethikkommission Charité – Universitätsmedizin Berlin. The declaration of Helsinki was respected.
Patient flow chart. Multidisciplinary conferences (MDCs) were introduced for two intensive care units (ICUs) of a university hospital in 2018. These were adapted to an online format with the emergence of the coronavirus-disease-19 (COVID-19) pandemic. Radiologists and ICU physicians meet in biweekly conferences to discuss imaging examinations of mutual patients, identify quality management (QM) events (any imaging-related error), and provide bilateral feedback. A detailed report of such MDCs has been published earlier. Structured protocols of these MDCs were collected over a 2-year period and were analysed with for QM events and COVID status. MDCs were routinely held biweekly, except for public holidays.
Data collection
This study has a retrospective observational analytic design. Protocols from all consecutive MDCs held during the study period were digitalised using Microsoft® Excel 2016. Data protection was assured. Further clinical information on all examinations affected by QM events was retrieved from the patient administration system (SAP ® Software 2021 SAP SE or an SAP affiliate company) and radiological information system (CentricityTM RIS-I 6 2018 General Electric Company). Data were collected by a doctoral candidate.
COVID status
While most COVID-19 patients were treated in separate COVID ICUs newly established in our hospital, the two ICUs included in this study regularly treated both COVID-positive and -negative patients side by side. Relevant COVID affection (i.e., relevant to this specific imaging examination as defined by the ICU physicians) was documented in the MDC protocols and included suspected, confirmed, and recent COVID-19 infection or pneumonia. Relevant COVID affection is referred to as COVID status for the purpose of this manuscript. Proof of a positive COVID status was collected based on positive SARS-CoV-2 PCR and/or typical imaging features on chest CT. Official epidemic data on COVID-19 were gathered from the Robert Koch Institute (RKI) website29,30. The RKI definition of epidemic COVID-19 phases used for this study relies on the following parameters: positivity rate of SARS-CoV-2 PCR testing, PCR tests per 100,000 inhabitants, 7-day-incidence, 7-day-reproduction value, rate of infected individuals with relation to outbreaks, hospitalisation rate, rate of infected individuals with COVID exposure abroad, syndromic surveillance of acute respiratory diseases, COVID-19 rate in ICUs, and current national governmental restrictions.
Statistical analysis
All statistical analyses were conducted using Excel® or SPSS®. Descriptive statistics are provided as mean and standard deviation (SD) or median and interquartile range (IQR). The QM incidence and time to MDC (i.e., the interval between the imaging examinations itself and the MDC during which it was presented) were compared to a patient population from the same ICUs investigated in 2018–2019 employing Pearson’s Chi-Squared test and Mann-Whitney-U test respectively4. Imaging examinations were only discussed once i.e. patients enrolled in multiple MDCs were enrolled with different imaging examinations. Thus, statistical independence was assumed. Due to the low sample size with positive COVID status, no statistical testing was performed to evaluate the difference in QM incidence according to COVID status. The effect of time on the incidence of QM events was calculated using simple linear regression analysis. Epidemic data on COVID-19 and baseline characteristics of MDCs were cross-matched: different epidemic COVID-19 phases were analysed regarding differences in MDC cancellation rate and QM comments using Pearson’s Chi-Squared tests and number of examinations per MDC using ANOVA. The MDC cancellation rate is defined as the percentage of cancelled MDCs, for which no protocol was created, out of all potentially scheduled MDCs. The limit for statistical significance was set at a p-value of 0.05. P-values and confidence intervals were not adjusted for multiplicity due to the explorative study design. Due to the low incidence in the study cohort, no statistical testing was performed for comparison of COVID status and QM incidence between different epidemic COVID-19 phases.
Results
Baseline characteristics
A total of 333 MDCs held in an online format were included in this analysis. Of those, 165 were held in a surgical ICU (49.5%) and 168 in a medical ICU (50.5%). During the study period of two years, 1324 radiological examinations of 857 patients were discussed (Fig. 1; Table 1). A median of four (IQR = 3-4.75) examinations was presented per MDC. The median time to MDC was one day (IQR = 1–3). This was shorter compared to a previously published study cohort of the same ICUs (median = 2, IQR = 1–3, p = 0.174 4). The most frequently discussed imaging modality was CT (64.0%, n = 847/1324), followed by MRI (2.3%, n = 30/1324), and X-ray (1.7%, n = 22/1324). Body regions examined included the chest (53.9%, n = 714/1324), abdomen (28.8%, n = 381/1324), head (12.8%, n = 169/1324), and pelvis (4.7%, n = 62/1324). Imaging was most commonly requested for identification of an infectious focus (34.7%, n = 459/1324) including 7.1%, (n = 94/1324) examinations with already known or suspected infectious foci, e.g., in patients with pneumonia or pancreatitis. This indication was followed by evaluation of bleeding (8.2%, n = 108/1324) and imaging because of acute respiratory distress syndrome (ARDS) (7.2%, n = 95/1324).
QM events
A total of 36 QM events were recorded during the study period. Of those, one examination was affected by two QM events. In total, QM incidence was 2.6% (n = 35/1324). No repeat errors (i.e., multiple QM events of the same category affecting imaging examinations of the same patient) occurred in this patient population. Twenty-nine QM events affected the radiological report (80.6%), six affected the imaging procedure itself (16.7%), and one the indication for imaging (2.8%). A total of 720 (54.4%) feedback comments were provided in the study protocols, among them 685 for examinations without QM events. For all examinations affected by QM events, written feedback regarding the respective QM event was provided in the standardised MDC protocol. Here, additional aspects of findings or clinical implications were noted, i.e., general feedback was provided to requesting ICU physicians or radiologists involved in the procedure or reporting.
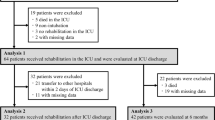
COVID status and QM events
COVID status was positive in 7.3% (n = 97/1324) of examinations and in 8.6% (n = 3/35) of patients who experienced QM events (Fig. 2). All examinations with positive COVID status discussed in MDCs were CTs. In 44.3% of examinations with positive COVID status, written feedback was provided in the MDC protocol (n = 43/97).
QM events by COVID status. COVID status was noted as documented in the protocol. Relevance of COVID-19 affection is specific to an individual examination and was defined by the experienced ICU physicians involved in MDCs. This included suspected/confirmed/recent COVID-19 infection based on polymerase chain reaction (PCR) testing or computed tomography (CT) imaging. The two ICUs included in this study are specialised in the treatment of medical and surgical conditions respectively. Both ICUs also treated patients with COVID-19 when required for other reasons.
MDCs over time
In a previous study conducted in the same ICUs prior to the COVID-19 pandemic, a QM incidence of 14.0% (n = 136/973) was calculated4. The QM incidence in the present analysis was significantly lower (2.7%, n = 36/1324, p < 0.001). The first COVID-19 case in Berlin was confirmed on the 1st of March 2020. The QM incidence remained consistent during the course of the COVID-19 pandemic (Fig. 4). A simple regression analysis yielded no significant change over time (regression coefficient estimate = -0.01, 95% confidence interval = [0.000, 0.000], p = 0.68, supplementary Table 2).
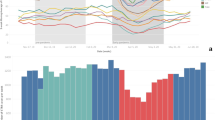
Impact of COVID-19 waves on MDCs
Epidemic COVID-19 phases were defined by the RKI incorporating various aspects such as COVID incidence, the rate of positive PCR tests and hospitalisation rates amongst others: first wave, summer plateau 2020 (2a and 2b), second wave, third wave (Variant of concern (VOC) alpha), summer plateau 2021, fourth wave (VOC delta summer and VOC delta autumn/winter) and fifth wave (VOC Omicron BA.1) (Fig. 3)29,30. MDC cancellation rate was higher during COVID-19 waves (21.5%, n = 58/270) than during low incidence phases (11.0%, n = 15/136) (p = 0.01). More examinations with positive COVID status were discussed during COVID-19 waves (10.2%, n = 87/854) than during low incidence phases (2.1%, n = 10/450). The rate of examinations discussed during MDCs for which written feedback comments were provided did not differ between different epidemic COVID-19 phases (p = 0.23). The number of examinations discussed per MDC did not differ between epidemic COVID-19 phases (p = 0.22). QM incidence remained steady throughout different epidemic COVID-19 phases (Fig. 4).
Course of MDCs during the COVID-19 pandemic. MDCs in our hospital were adapted to pandemic requirements with the rise of the COVID-19 pandemic. Radiologist and intensive care physicians met in biweekly QM video calls to discuss mutual patients. The x-axis shows the calendar weeks of 2020 and 2021 separated into different COVID-19 phases as defined by the Robert Koch Institute (RKI) taking various factors such as incidence, rates of positive PCR-tests, and hospitalisation rate into account29,30. COVID-19 waves are highlighted. The left y-axis shows the MDC cancellation rate (out of n = 406 potentially scheduled MDCs during the study period) (black), the rate of examinations with relevant COVID affection (as defined by experienced ICU physicians involved in MDCs) (dark gray), and the percentage of examinations discussed in MDCs for which written feedback was provided, i.e., comments/exam (light gray). The right y-axis shows the mean number of examinations that was presented during an MDC for each epidemic COVID-19 phase (supplementary Table 3).
QM incidence over time. The rate of examinations affected by QM events (QM incidence) (y-axis) per MDC is shown for all calendar week (x-axis) of the study period. No decrease in QM incidence was found by simple regression analysis (regression coefficient estimate = -0.01, 95% confidence interval = [0.000, 0.000], p = 0.68, supplementary Table 2). Epidemic COVID-19 phases according to the RKI are shown29,30 and COVID-19 waves are highlighted.
Discussion
Summary
MDCs between ICU physicians and radiologists for identification of imaging-related QM events were introduced in our university hospital in 2018 and initially analysed in an earlier study (2018/2019)4. The present study provides follow-up data during the COVID-19 pandemic from 2020 to 2021. MDCs were switched to an online format after the onset of the pandemic. Our results suggest that the rising COVID-19 pandemic had no impact on the incidence of QM events: QM incidence in the present study population remained steady at a consistently lower level compared to our pre-pandemic study population4. COVID-positive and -negative patients were equally affected by QM events. The interval between an imaging examination and its discussion during an MDC was shorter in the present study compared to the interval observed in the pre-pandemic study, which started directly after the implementation of MDCs in 2018 4. COVID-19 waves differed from low incidence COVID-19 phases in terms of a higher MDC cancellation rate. Other comparing factors were congruent across different epidemic COVID-19 phases.
Interpretation
Having established a structured multidisciplinary feedback mechanism between radiologists and ICU physicians in our hospital in 2018, we could rapidly adapt the format to continue early error identification during the COVID-19 pandemic. This was essential for all physicians to gain expertise in coping with the emergence of a new disease. After two years with regular MDCs providing immediate feedback between radiologists and clinicians, the incidence of QM events did not rise despite the tremendous challenges of COVID-19. This may be explained by constant interdisciplinary exchange and a growing feedback culture. During the initial phase of the COVID-19 pandemic, no new radiologists were hired in our department. Thus, the decrease in QM incidence compared to a pre-pandemic study population may be explained by the radiologists’ individual learning curve on the grounds of MDC based feedback. The innovation and implementation of new communication channels during the pandemic facilitated ongoing interpersonal exchange, which appears to be critical for the identification and prevention of medical error. Despite more frequent cancellations of MDCs during COVID-19 waves than during low incidence phases, time to MDC, number of imaging examinations discussed and QM comments provided did not vary. This suggests that the quality of MDCs remained consistent. Such a format seems to provide an effective approach to quality management which may be implemented in other hospitals. Its successful implementation into clinical routine allows for quick adaptation to new situtations, including another rising pandemic. Digitalisation of the format shows to be possible and equally effective.
Comparison with the literature
The incidence of QM events observed in the present study decreased compared to the incidence we found immediately after the implementation of MDCs in our hospital4. This development indicates that MDCs as a QM initiative may be an effective tool for the long-term prevention of imaging-related QM events even in times of a global pandemic. Our data thus suggest that an online format may sufficiently replace in-person meetings when required. To the best of our knowledge, there are no studies analysing the effectiveness of previously established QM interventions during the COVID-19 pandemic. The time to MDC has decreased marginally compared to our initial study4. In other words, QM events thus could be identified earlier in the current study, which may have averted potential adverse events. Further characteristics of MDCs have not changed either compared to this initial patient cohort4 or during epidemic COVID-19 phases. This indicates a consistently high-quality standard of MDCs, in-person and online, confirming their successful establishment in clinical routine and their effectiveness even during a pandemic. All patients with a positive COVID status in the current study underwent chest CT. Published results show CT to be superior to X-rays in terms of both sensitivity and specificity10. This is in line with recommendations of the European Society of Radiology recommending CT as the best imaging modality in the diagnosis of COVID-19 22. Existing studies reported only moderate inter-reader agreement concerning CTs of PCR-positive COVID patients7. MDCs aim at reducing the consequences of discrepant reports when imaging studies are interpreted by different readers by contributing to inter-reader consensus through multidisciplinary discussion. Relevant COVID affection reported in this study population was lower compared to the COVID-19 incidence of hospitalised patients31. This is owed to the establishment of special COVID ICUs in our institution. Hence, only few COVID patients were treated in the two ICUs included in our analysis.
Clinical impact
Errors in diagnostic workup may have serious consequences for patients. Early QM identification is therefore of utmost importance. Multidisciplinary exchange is imperative in times of a pandemic but may be especially difficult to realise when all face-to-face interactions must be minimised. Remote multidisciplinary QM conferences may be a suitable approach to keep up a previously established feedback culture. Steps to set up an online format were undertaken immediately and effectively. MDCs were evaluated in a medical and a surgical ICU i.e. they were validated for a wide range of diseases. Thus, the here established format of MDCs may be effectively adjusted to varying challenges in the future. It may also be adopted by other institutions allowing for their adaptation to local requirements. This may continue to improve radiological workup, multidisciplinary cooperation, and ultimately patient safety.
Limitations
Our retrospective analysis has several limitations. Importantly, causality cannot be established as several confounding factors remain unknown. This study only focussed on imaging-related quality management, an analysis of further modalities and their influence on quality management was beyond the scope of this manuscript and should be the focus of further research. The incidence of both COVID-19 and QM events in the present study is low, limiting the power of the statistical analysis. The retrospective, single-centre design does not guarantee the generalisability of the results to a larger population. However, it ensures consistency in the format of MDCs and the data collection resulting in fewer discrepancies in data quality. As an explorative study, this study merely provides a suitable approach to combat imaging-related error and may be adapted to the hospital-specific circumstances elsewhere. Two senior radiologists led all MDCs, thereby limiting conclusions regarding a larger community of radiologists. Still, the high continuity of the conference format keeps the assessment of QM events constant, allowing further evaluation and identification of relevant factors. The ICUs analysed in the present study did not reflect the level of QM events on primary COVID ICUs that were established in our hospital during the pandemic. This was not within the scope of this manuscript and is the focus of an ongoing study. Our data thus primarily reflect the impact of the COVID-19 pandemic on the management of all patients with common medical and surgical conditions requiring intensive care.
Conclusion
To conclude, a previously established format of MCDs was adapted to an online format. MDCs continued to identify imaging-related QM events in ICU patients during the COVID-19 pandemic. There was no rise in QM incidence in the face of COVID-related challenges. This format has been shown to be effective, both in a pre-pandemic setting, and during the COVID-19 pandemic. It might be adapted to further epidemic or pandemic challenges that may arise in the future. Further research should focus on digitalised communication channels in quality management.
Data availability
Data are available from the corresponding author upon reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- COVID-19:
-
Coronavirus-disease-19
- CT:
-
Computed tomography
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- MDCs:
-
Multidisciplinary conferences
- MRI:
-
Magnetic resonance imaging
- PCR:
-
Polymerase chain reaction
- PET CT:
-
Positron emission tomography scan
- QM:
-
Quality management
- RKI:
-
Robert Koch Institute
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SD:
-
Standard deviation
References
Garland, L. H. On the scientific evaluation of diagnostic procedures. Radiology 52, 309–328. https://doi.org/10.1148/52.3.309 (1949).
Bassiouni, M., Bauknecht, H. C., Muench, G., Olze, H. & Pohlan, J. Missed radiological diagnosis of otosclerosis in high-resolution computed tomography of the Temporal Bone-Retrospective Analysis of Imaging, Radiological Reports, and request forms. J. Clin. Med. 12 https://doi.org/10.3390/jcm12020630 (2023).
Lauritzen, P. M. et al. Radiologist-initiated double reading of abdominal CT: Retrospective analysis of the clinical importance of changes to radiology reports. BMJ Qual. Saf. 25, 595–603. https://doi.org/10.1136/bmjqs-2015-004536 (2016).
Muench, G. et al. Imaging intensive care patients: multidisciplinary conferences as a quality improvement initiative to reduce medical error. Insights Imaging 13, 175 (2022). https://doi.org/10.1186/s13244-022-01313-5
Di Fusco, M. et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J. Med. Econ. 24, 308–317. https://doi.org/10.1080/13696998.2021.1886109 (2021).
Bartsch, S. M. et al. The potential Health Care costs and Resource Use Associated with COVID-19 in the United States. Health Aff (Millwood). 39, 927–935. https://doi.org/10.1377/hlthaff.2020.00426 (2020).
Bellini, D. et al. Diagnostic accuracy and interobserver variability of CO-RADS in patients with suspected coronavirus disease-2019: A multireader validation study. Eur. Radiol. 31, 1932–1940. https://doi.org/10.1007/s00330-020-07273-y (2021).
Grasselli, G. et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 323, 1574–1581. https://doi.org/10.1001/jama.2020.5394 (2020).
Fang, Y. et al. Sensitivity of chest CT for COVID-19: Comparison to RT-PCR. Radiology 296, E115–E117. https://doi.org/10.1148/radiol.2020200432 (2020).
Borakati, A., Perera, A., Johnson, J. & Sood, T. Diagnostic accuracy of X-ray versus CT in COVID-19: A propensity-matched database study. BMJ Open. 10, e042946. https://doi.org/10.1136/bmjopen-2020-042946 (2020).
Shi, H. et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. Lancet Infect. Dis. 20, 425–434. https://doi.org/10.1016/S1473-3099(20)30086-4 (2020).
Pohlan, J. et al. Relevance of CT for the detection of septic foci: Siagnostic performance in a retrospective cohort of medical intensive care patients. Clin. Radiol. 77, 203–209. https://doi.org/10.1016/j.crad.2021.10.020 (2022).
Rubin, G. D. et al. The role of chest imaging in Patient Management during the COVID-19 pandemic: A multinational Consensus Statement from the Fleischner Society. Chest 158, 106–116. https://doi.org/10.1016/j.chest.2020.04.003 (2020).
Bercean, B. A. et al. Evidence of a cognitive bias in the quantification of COVID-19 with CT: An artificial intelligence randomised clinical trial. Sci. Rep. 13, 4887. https://doi.org/10.1038/s41598-023-31910-3 (2023).
Hadied, M. O. et al. Interobserver and intraobserver variability in the CT assessment of COVID-19 based on RSNA consensus classification categories. Acad. Radiol. 27, 1499–1506. https://doi.org/10.1016/j.acra.2020.08.038 (2020).
Won, E. & Rosenkrantz, A. B. JOURNAL CLUB: Informal consultations between radiologists and referring physicians, as identified through an Electronic Medical Record Search. AJR Am. J. Roentgenol. 209, 965–969. https://doi.org/10.2214/AJR.17.18050 (2017).
Institut, R. K. Ergänzung zum Nationalen Pandemieplan – COVID-19 – neuartige Coronaviruserkrankung (2020). https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Ergaenzung_Pandemieplan_Covid.pdf?__blob=publicationFile
Min, X., Zhai, G., Zhou, J., Farias, M. C. Q. & Bovik, A. C. Study of subjective and Objective Quality Assessment of Audio-Visual signals. IEEE Trans. Image Process. https://doi.org/10.1109/TIP.2020.2988148 (2020).
Min, X. et al. A multimodal saliency model for videos with high audio-visual correspondence. IEEE Trans. Image Process. https://doi.org/10.1109/TIP.2020.2966082 (2020).
Zhai, G. Perceptual image quality assessment: A survey. Sci. China Inform. Sci. 63 (2020).
Xiongkuo Min, H. D., Sun, W. & Zhu, Y. Guangtao Zhai. Perceptual video quality assessment: A survey. Sci. CHINA (2024).
Revel, M. P. et al. COVID-19 patients and the radiology department - advice from the European Society of Radiology (ESR) and the European Society of Thoracic Imaging (ESTI). Eur. Radiol. 30, 4903–4909. https://doi.org/10.1007/s00330-020-06865-y (2020).
ECDC, E. C. f. D. P. a. C. Guidance for wearing and removing personal protective equipment in healthcare settings for the care of patients with suspected or confirmed COVID-19 (2020). https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-guidance-wearing-and-removing-personal-protective-equipment-healthcare-settings-updated.pdf
Foley, S. J., O’Loughlin, A. & Creedon, J. Early experiences of radiographers in Ireland during the COVID-19 crisis. Insights Imaging. 11, 104. https://doi.org/10.1186/s13244-020-00910-6 (2020).
Blum, D. K. Personalsituation in der Intensivpflege und Intensivmedizin: Gutachten des Deutschen Krankenhausinstituts im Auftrag der Deutschen Krankenhausgesellschaft (2017). https://www.dki.de/sites/default/files/2019-01/2017_07_personalsituation_intensivpflege_und_intensivmedizin_-_endbericht.pdf
Sinsky, C. A., Brown, R. L., Stillman, M. J. & Linzer, M. COVID-Related stress and work intentions in a sample of US Health Care Workers. Mayo Clin. Proc. Innov. Qual. Outcomes. 5, 1165–1173. https://doi.org/10.1016/j.mayocpiqo.2021.08.007 (2021).
Lai, J. et al. Factors Associated with Mental Health Outcomes among Health Care workers exposed to Coronavirus Disease 2019. JAMA Netw. Open. 3, e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 (2020).
Coppola, F., Faggioni, L., Neri, E., Grassi, R. & Miele, V. Impact of the COVID-19 outbreak on the profession and psychological wellbeing of radiologists: A nationwide online survey. Insights Imaging. 12, 23. https://doi.org/10.1186/s13244-021-00962-2 (2021).
Institut, R. K. Epidemiologisches Bulletin, (2021). https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2021/Ausgaben/15_21.pdf?__blob=publicationFile
Institut, R. K. Epidemiologisches Bulletin, (2022). https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2022/Ausgaben/38_22.pdf?__blob=publicationFile
Robert-Koch-Institut. 7-Tage-Inzidenz der COVID-19-Fälle nach Kreisen sowie der hospitalisierten COVID-19-Fälle nach Bundesländern, https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Daten/Inzidenz-Tabellen.html (2020–2023).
Acknowledgements
Bettina Herwig provided professional language editing.
Funding
Open Access funding enabled and organized by Projekt DEAL.
This study received no third party funding.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the conception of this manuscript. G.M. collected, analysed and interpreted the data, wrote the manuscript and created all figures. D.W., S.M., D.P., V.W. and J.N. co-wrote the manuscript. KR provided statistical expertise and co-wrote the manuscript. E.Z. and M.D. implemented the quality management (QM) initiative, chaired the multidisciplinary conferences (MDCs), provided the MDC protocols and co-wrote the manuscript. J.P. provided assistance in data collection, analysation and interpretation and co-wrote the manuscript. J.P. and M.D. supervised the project with senior advice and infrastructure. All authors reviewed the manuscript and approved of its submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethics approval was granted by the local ethics committee under EA1/024/21. Written consent from patients was waived. The Declaration of Helsinki was respected.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Muench, G., Witham, D., Rubarth, K. et al. Digitalised multidisciplinary conferences effectively identify and prevent imaging-related medical error in intensive care patients during the COVID-19 pandemic. Sci Rep 15, 1197 (2025). https://doi.org/10.1038/s41598-024-83978-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-83978-0