Abstract
The rapid and early detection of infections and antibiotic resistance markers is a critical challenge in healthcare. Currently, most commercial diagnostic tools for analyzing antimicrobial resistance patterns of pathogens require elaborate culture-based testing. Our study aims to develop a rapid, accurate molecular detection system that can be used directly from culture, thereby introducing molecular testing in conjunction with culture tests to reduce turnaround time and guide therapy. PathCrisp assay, a combination of loop-mediated isothermal amplification and CRISPR-based detection, maintained at a single temperature, was designed and tested on clinical isolates. The specificity and sensitivity of the assay was analyzed, post which the assay was compared with the polymerase chain reaction (PCR) method to detect the New Delhi metallo-beta-lactamase (NDM) gene in carbapenem-resistant enterobacteriaceae clinical samples. Our PathCrisp assay demonstrated the ability to detect as few as 700 copies of the NDM gene from clinical isolates. Our assay demonstrated 100% concordance with the PCR-Sanger sequencing method, more commonly used. Additionally, the lack of the need for a kit-based DNA purification step, rather a crude extraction via heating, enables the direct use of culture samples. The PathCrisp assay is precise, specific and rapid, providing results in approximately 2 h, and operates at a constant temperature, reducing the need for complex equipment handling. In the near future, we hope that this assay can be further optimized and designed as a point-of-care test kit, facilitating its use in various healthcare settings and aiding clinicians in the choice of antibiotics for therapy.
Similar content being viewed by others
Introduction
Antimicrobial resistance (AMR), a silent pandemic, was associated with 4.95 million deaths in 20191. The World Health Organization (WHO) reports that one in every five of these deaths occurred in children below five years, highlighting the acute demand for addressing the crisis1. Antibiotics like Carbapenems serve as the last treatment phase for high-risk patients infected with bacteria resistant to most β-lactamases. Carbapenems, a type of β-lactam antibiotic, possess a broad spectrum of antimicrobial activity against Gram-positive and Gram-negative bacteria and are resistant to most of β-lactamases, acting as a promising last line of antibiotics2. However, the absence of affordable and rapid diagnostic tools increases the risk of antibiotic overuse and contributes to the emergence of resistance3. Regrettably, carbapenems experienced a similar resistance outbreak.
The emergence of carbapenem resistance represents a notable hazard to public health4. WHO reports that carbapenem resistance-related mortality rates range from 26 to 70% globally, and the death rate was significantly higher in carbapenem resistance in comparison to susceptible infection5. Therefore, effective, timely diagnostics are crucial for guiding appropriate antibiotic treatment, particularly in resource-limited settings.
Carbapenemase production is currently reported to be one of the leading causes of carbapenem resistance6. Hence, carbapenemase genes are the best candidates for the detection of carbapenem resistance. Within carbapenemases, New Delhi metallo-β-lactamases (NDM), a Class B metallo-β-lactamase, is known for its resistance to a wide range of β-lactam antibiotics including carbapenems7. Furthermore, NDM has spread globally, with India being its predicted epicentre8, increasing the need for early detection in the subcontinent.
Early screening of resistance patterns is crucial for treating high-risk patients. Conventional antibacterial susceptibility tests typically require 2–5 days. Commercially available tests like VITEK-2 can deliver results in a few hours but are expensive, require heavy equipment and need pure cultures, resulting in a turnaround time of 18–24 h9. MALDI-TOF-based analysis can detect the pathogen and resistance within a few hours but also requires costly equipment10. Meanwhile, molecular tests, which are both rapid and accurate, offer an alternate detection platform. In nucleic acid-based diagnostics, thermal cycler-dependent PCR and qPCR are considered the gold standards. However, the implementation of these robust tests demands sophisticated equipment and techniques, such as qPCR and whole genome sequencing (WGS)11.
Isothermal amplification techniques, particularly Loop-mediated isothermal amplification (LAMP), are frequently suggested as molecular alternatives due to their elimination of the need for a thermal cycler and superior analytical sensitivity compared to gold standard PCR and qPCR methods12. LAMP utilizes the Bst enzyme, a strand-displacing polymerase, and 2–3 primer pairs leading to a concatemer product. However, LAMP’s low specificity often results in a high rate of false-positive outcomes13.
Meanwhile, CRISPR/Cas is a well-known tool in molecular biology, especially for gene editing. It primarily involves the Cas enzyme, a customizable nuclease and an engineered single guide RNA (sgRNA) with an RNA scaffold binding to the Cas enzyme and a customizable target-binding sequence14. Cas12a, a CRISPR/Cas variant, is renowned for activating collateral trans-cleavage of ssDNA15. This property can be exploited for diagnostic purposes16. For instance, when the Cas12a RNP complex encounters the target site, it binds and activates trans-cleavage, which can be utilized for diagnostic readouts using an ssDNA reporter with a fluorophore and quencher. The reporter emits fluorescence only when cleaved, enabling precise detection.
In this study, we introduce the PathCrisp assay, a combination of CRISPR/Cas12a and LAMP, specifically the PathCrisp-NDM variant for detecting carbapenemase NDM. This assay employs Fluorescence-Quencher ssDNA for real-time fluorescence-based detection within 2 h. We compared it with the gold standard molecular detection method, PCR. using 49 CRE isolates sequenced with Sanger sequencing. PathCrisp-NDM demonstrated greater sensitivity than the PCR method and can also directly detect bacterial colonies. Overall, PathCrisp-NDM is a specific, sensitive, and rapid diagnostic assay that can assist in therapy at the point of need.
Materials and methods
sgRNA and LAMP primers designing
NDM variant gene sequences were downloaded from databases such as the Comprehensive Antibiotic Resistance Database (CARD)17 and the National Center for Biotechnology Information (NCBI)18, and aligned using Clustal Omega19. The aligned sequences were then viewed using AliView20. sgRNA was designed in the conserved region, and six LAMP primers were designed around the sgRNA. (see Table 1 for sequences).
Testing the conservation of designed oligos and Ethical statement
This was done using the genomic sequence data from 122 isolates. Briefly, these isolates are part of a multi-centre study mapping the prevalence of AMR, as well as its genetic underpinnings, across India. With this goal, genomic DNA of three pathogenic species, namely Escherichia coli, Klebsiella pneumoniae and Acinetobacter baumanii, from diverse specimens were extracted in two different tertiary healthcare centers using a DNeasy Blood & Tissue Kit (69504, Qiagen).
Library was prepared using Nextera XT DNA Library Preparation Kit -96 samples (CAT No: FC-131-–1096) at the sequencing facility of the National Center for Biological Sciences. Sequencing was done at the same place using the Illumina NovaSeq 6000 platform with 2 × 100 bp sequencing read length. The raw sequence data was filtered and assembled using a GitHub pipeline21.
We used the fasta files of the genomic assemblies to screen for the presence of the NDM gene. For the screening, we first used ResFinder22 to determine the overall antibiotic-resistance genes and their positions in the 122 assembled genomes. Using python (v 3.9.13) and RStudio (R v4.2.1)23, the samples positive for NDM gene variants were screened and the NDM gene sequences (ranging from 793 to 813 base pairs in length) were extracted. Jalview (v 2.11.3.3)24 was used to view and align these sequences and check for the designed oligos conservation. The details of the NDM-positive isolates are given in Table S1.
Institutional ethics committee approval for the multi-centre study was obtained at Ashoka University. Additionally, both clinical partners viz. Max Healthcare and Sahyadri Hospital obtained ethical clearances from their respective ethics committees. Informed consent was obtained from all subjects and/or their legal guardian(s).
Isothermal amplification
Multi-Purpose LAMP Master Mix (DNA) (ABT-025S, Aurabiotech) was used to set up isothermal amplification. Briefly, 1 µl of the sample was added to the LAMP reaction mix containing, 5 µl of 2× reaction buffer, 0.4 µl of Bst1.0 enzyme, 0.2 µM of outer primers, 0.4 µM of loop primers, and 1.6 µM of inner primers. The reaction was incubated at 60 °C for one hour.
Trans-cleavage assay
The detection mix was prepared by pre-incubating 26 nM (final concentration) of the sgRNA, 26 nM (final concentration) of Cas12a (Alt-RTM L.b. Cas12a (Cpf1) Ultra, (10007923, IDT)), 200 nM (final concentration) ssDNA-FQ (/56-FAM/TT ATT /3IABkFQ, IDT) in 1× NEBuffer™ 2 (B7002S, NEB) at room temperature for 10 min to facilitate RNP complex formation. Following incubation, the detection mix was introduced to the template and incubated at 37 °C for both cis and trans-cleavage activity in the Tecan Infinite MPlex with an excitation wavelength of 480 nm. Relative fluorescence units were recorded for every 2.5 min at 520 nm emission wavelength.
PathCrisp assay-isothermal amplification followed by trans-cleavage assay (two-step)
For UDG-free amplification of the target, a Multi-Purpose LAMP Master Mix (DNA) (ABT-025S, Aurabiotech) was used. Briefly, 1 µl of the sample was added to the LAMP reaction mix containing, 5 µl of 2× reaction buffer, 0.4 µl of Bst1.0 enzyme, 0.2 µM of outer primers, 0.4 µM of loop primers and 1.6 µM of inner primers.
For amplification with UDG, WarmStart Multi-Purpose LAMP/RT-LAMP 4× Master Mix (with UDG) (M1718B, NEB) was used. Briefly, 1 µl of the sample was added to the LAMP reaction mix containing, 3.5ul of master mix, 0.2 µM of outer primers, 0.4 µM of loop primers and 1.6 µM of inner primers.
LAMP reaction was carried out at 60 °C for 1 h. No template control (NTC) was used as a negative control for the LAMP reaction in each batch.
For detection, 10 µl of amplified product was treated with the detection Mix for the trans-cleavage assay. The detection Mix was prepared as described previously in trans-cleavage assay using Cas12a (Alt-R™ A.s. Cas12a (Cpf1) Ultra, (10001272, IDT) or Alt-R™ L.b. Cas12a (Cpf1) Ultra, (10007923, IDT)) and incubated at 60 °C for Cis- and Trans-cleavage activity for 30 min. An end-point reading at the 30th minute was recorded in a Tecan Infinite MPlex (Sl. No: 2203009710) with 480 nm wavelength excitation and 520 nm wavelength emission.
Known NDM controls were used to study the specificity of our assay: NDM-1 positive K.pneumoniae (NDM-1) DNA CONTROL (MBC107-R, Vircell) and NDM negative controls: genomic DNA of P.aeruginosa, A.baumannii, K.pneumoniae, E.coli (O157:H7) from Himedia. Further, pJET1.2 backbone plasmid negative for NDM was used as a negative plasmid control, and a human sample’s genomic DNA was also included in the study.
No template control (Detection negative) and 0.3 nM pJET1.2_NDM plasmid (Detection positive) were used in each batch as trans-cleavage controls. This pJET1.2_NDM plasmid details are mentioned in the next segment.
Limit of detection of PathCrisp assay
To analyze the limit of detection of our developed assay, the NDM partial gene was amplified using NDM F4 and NDM B4 primers (sequences available in Table 1), which are located outside of outer LAMP primers, using Q5 High-Fidelity 2X Master Mix (M0492S, NEB). The amplified product was cloned into the pJET1.2/blunt plasmid using CloneJET PCR Cloning Kit (K1231, Thermo Scientific). The sequence-confirmed (sequence available in Supplementary data-1), pJET1.2_NDM plasmid was quantified using NanoDrop One™ (Thermo Scientific, USA). The concentration was 28.6 pg/µl, roughly corresponding to 7.36E+06 copies/µl (calculated through NEBioCalculator25). This plasmid was further tenfold serial diluted to obtain dilutions as low as 7 copies/µl. The diluted plasmid was used to set up the PathCrisp assay. The assay was replicated 5 times: 3 times with Alt-R™ A.s. Cas12a (Cpf1) Ultra, (10001272, IDT) and 2 times with Alt-RTM L.b. Cas12a (Cpf1) Ultra, (10007923, IDT) at Trans-cleavage step of PathCrisp.
Clinical sample preparation and ethical statement
Clinical Samples were collected from patients, from which the pathogens were then isolated post-culture. These pathogens were further cultured, and bacterial cultures with VITEK-2 reports were obtained from Sri Venkateswara Institute of Medical Sciences, Tirupati. The DNeasy Blood & Tissue Kit (69504, Qiagen) was used for DNA extraction.
Institutional Ethics Committee approval was obtained from Sri Sathya Sai Institute of Higher Learning (SSSIHL/IEC/PSN/BS/2014/03) and Sri Venkateswara Institute of Medical Sciences Tirupati (1121 dated 20.03.2021) in accordance with the ethical standards of the Declaration of Helsinki. Further, the Institutional Biosafety Committee of C-CAMP approved the study.
(BT/IBKP/392/2020) and also from the MedStar Speciality Hospital Ethics Committee (Dated 07022024).
Sequencing-based sample validation
Clinical samples were amplified using Thermo 2X PCR master mix (K0171, Thermo Scientific) as described in Mahalingam et al. 201826. Briefly, a 50 µl PCR amplification was carried out using ~ 20 ng template, 25 µl 2X thermo MM, and 1 µM primer mix: NDM_ref_F and NDM_ref_R. Positive samples were further sequenced to analyze the NDM variant using NCBI’s nucleotide Basic Local Alignment Search Tool (BLAST)27. Negative samples were further amplified by using NDM-F3/B3 and NDM-F4/B4 primers (refer to Table 1 for sequences and Table 2 for thermal cycler conditions).
PathCrisp assay from crude extract
To analyze the sensitivity of the PathCrisp assay in detecting NDM from crude extract, pJET1.2_NDM plasmid transformed E. coli DH5-alpha were used. Two types of culture were used: (1) streaked colony and (2) broth culture.
For colony testing: A single bacterial colony was picked up using a 10 µl tip, dissolved in 10 µl of NFW, and boiled at 95 °C for 5 min to prepare the crude extract. One microlitre of crude extract was used to initiate PathCrisp assay-based diagnosis. For the media control, the pipette tip was scratched on a fresh agar plate to represent no colony control. The plasmid transformed E. coli DH5-alpha negative for pJET1.2_NDM was used for the negative control.
For broth testing: two hundred microlitres of overnight cultured broth were spun down at 13,000g for 5 min. Ten microliters of the culture from the bottom of the tube were collected in a fresh tube and boiled at 95 °C for 5 min to prepare crude extract. One microlitre of crude extract was used to initiate PathCrisp assay-based diagnosis. For the broth-only control, 10ul of fresh LB broth was used. For the negative control, Salmonella culture was used. All the work was done in appropriate biosafety cabinets with appropriate controls.
Diagnostic testing accuracy of PathCrisp assay and PCR
Sensitivity and Specificity were calculated according to Shreffler J, Huecker MR, 202428. Briefly, Sequenced confirmed samples were considered True positives and the rest were True negatives. Based on this, the following counts were made for each type of test: True positives (A), False positives (B), False negatives (C) and True negatives (D).
Sensitivity (in percentage) was calculated using the following equation:
Specificity (in percentage) was calculated using the following equation:
Analysis
To determine if the sample is positive or negative, its RFU value was compared with the LAMP_NTC. In the case of multiple repeats, the Sum of 3 times the Standard deviation and average RFU value of LAMP was considered to mark the cutoff.
Results
Conserved regions used to design sgRNA and LAMP primers
Sequences of NDM variants 1 to 43, except for NDM-32, were analyzed for conserved regions (Fig. 1.a). Details of the sequences used are available in Table S.1. The sequence for NDM-32 could not be found in any gene repository, as previously reported and hence not used29. The Cas12a guide was designed to target a region conserved across these variants (Fig. 1.a). LAMP primers were also built around this guide target using NDM-1 as the primary reference (Fig. 1.c). SNPs that may potentially overlap the designed LAMP primers were analyzed (Fig. 1.a). Outer primers: LAMP_F3 had the most SNPs and it was 51% conserved, while LAMP_B3 was 93% conserved. Inner primers: FIP (complementary of LAMP_F1–LAMP_F2) was 97% conserved, while BIP (complementary of LAMP_B1–LAMP_B2) was also 97% conserved. Loop primers: LAMP_LF, were also 97% conserved. LAMP_LB was 100% conserved.
Similarity of NDM-1 variant with different variants: primer and guide design. (a) Conserved regions across deposited NDM variants: partial NDM gene sequences from NCBI and CARD were aligned to study conserved regions across NDM variants (NDM-1 to NDM-43, except NDM-32). The green-coloured histogram at the beginning of the alignment depicts the conserved region. The Cas12a guide target is marked in pink, and is conserved across all variants. SNPs in the sequences are marked with block colours: dATP (red), dGTP (yellow), dCTP (blue), dTTP (green). (b) Conservation analysis in Indian patient samples: The NDM gene sequence of 101 NDM-positive clinical samples from different priority pathogens, such as E. coli, K. pneumoniae, and A. baumannii, from Indian patients, were screened to check for the conservation of the designed oligos. Whole genome sequences of these samples were used to extract the NDM gene sequences (793–813 base pairs in length). The NDM gene regions were screened to detect homology with the designed Cas12a guide and LAMP PCR primer sequences. The Figure shows conservation of the regions used for LAMP primer design (F1, B1, F2,B2, B3, LF and LB regions). Only the F3 region, shown in dark blue, shows SNPs at the 12th bp (A/C). All the other regions, including the Cas12a guide (red) are conserved across the recent Indian patient samples sequenced. Abbreviations: EC—E. coli, KP—K. pneumoniae, AB—A. baumannii, RC—reverse complementary sequence, F-Forward, B-Backward, L-Loop. (c) Map of LAMP primers designed with Cas12a guide: The layout of the designed LAMP primers with the sgRNA.
To further validate the conservation of these designed oligos, we screened the genomic sequence data of 122 isolates from two tertiary healthcare centers in India. 101 isolates showed the presence of NDM gene out of the total isolates screened (Fig. 1b). 36 of E.coli out of 44, 47 of K.pneumoniae out of 64 and 18 A.baumanii out of 29 showed at least one NDM variant. All the isolates showed resistance to at least one carbapenem; while 22 isolates were resistant to all four carbapenems. Apart from LAMP_F3, all other regions were conserved. The F3 primer is conserved only in the NDM-1 variants (28.7% of the samples). The NDM-5 and NDM-4 variants (71.3% of the samples) contain an A to C SNP in this region and thus do not show homology with the F3 primer. Details of the sequences used in the study are available in Table S.1.
Preliminary testing of designed oligos confirms their accuracy for NDM variants
To validate the designed guide and LAMP primers, a known control (genomic DNA of K.pneumoniae positive for NDM-1) was used to set up a 2-step assay, LAMP at 60 °C followed by Transclevage assay at 37 °C (Fig. 2a). The designed guide and primers were able to confirm the NDM-positive test sample. Further, to test the accuracy of our assay, different negative samples were tested in duplicates, using previously used K. pneumoniae (NDM-1) as assay controls (Fig. 2b). In both cases, only positive samples had higher fluorescence readings, more than 20 times of negative control (LAMP_NTC).
Validation of designed oligos for NDM variants: (a) testing with genomic DNA of K. pneumoniae: the genomic DNA of K. pneumoniae, positive for NDM-1 (obtained from Vircell), is being used to test the designed LAMP primers and sgRNA. Our designed guide and primers can detect NDM-1. (b) specificity testing with negative controls: different known negative genomic DNAs are being used to test the specificity of the PathCrisp assay, with previously used K. pneumoniae (NDM-1) as assay control. The assay was repeated twice: once with Bst1.0 (without UDG) depicted as circles in the graph, and a second time with BST2.0 (with UDG) depicted as diamonds in the graph. The average value of each sample is represented as a bar graph, while individual values are marked either as circles or diamonds. Grey dotted lines represent the cutoff to consider if the sample is positive, which is the average of RFU of LAMP-NTC plus 3 times the standard deviation. (c) Testing with carbapenem-resistant E. coli isolates: sixteen carbapenem-resistant E. coli isolates from patient samples were tested with designed LAMP primers and sgRNA. VIR-5, VIR-8 and VIR-9 were negative for NDM, consistent with the previous report. The NDM as per previous sequencing data is mentioned for the samples. In each assay, the negative control for LAMP is no-template control, depicted as LAMP-NTC. For detection controls, negative control, with no LAMP product, is shown as Det. negative in the graph. For positive control, pJET1.2_NDM was used, depicted as Det. positive.
Previously, Mahalingam, Niranjana et al. (2018) had analysed AMR genes in carbapenem-resistant E. coli26. We used sixteen samples from this report to test the ability of the designed primers and sgRNA to detect different NDM-variants (Fig. 2c) and compared them with the previous data (Fig. 2d). Among 16 VIR samples, 13 were positive for NDM variants ranging from NDM-4 to NDM-7 and 3 were negative for NDM. Our assay accurately reproduced the same results as previously published, correctly calling out the NDM positives. As previously described, many NDM variants had SNPs in the LAMP F3 primer region like NDM-4 and NDM-5, yet our assay was able to specifically detect them.
Limit of detection of PathCrisp assay
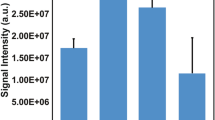
Our PathCrisp assay, integrating LAMP and CRISPR/Cas12a-based trans-cleavage, was developed to operate at a constant temperature of 60 °C. This assay was meticulously analyzed to establish its limit of detection. To achieve this, a serial dilution of the pJET1.2_NDM plasmid was employed. The assay demonstrated high sensitivity, consistently detecting as little as 2.86E-03 picograms of the plasmid DNA, approximately equivalent to 700 copies of the target gene. This low detection limit highlights the assay’s potential for rapid and accurate molecular diagnostics, making it a robust tool for identifying antimicrobial resistance markers (Fig. 3).
Limit of detection of NDM-PathCrisp assay. Purified pJET1.2_NDM plasmid was serially dilated up to 2.86E−05 picogram (which roughly corresponds to 7 copies) and then used as a template for Pathcrisp. The assay can consistently detect up to 2.86E−03 picogram (~ 700 copies). The mean value for each sample is represented as a bar graph while individual values are marked either as circles The Grey dotted line represents the cutoff to consider if the sample is positive, which is the sum of the average LAMP-NTC RFU and 3 times its Standard deviation. The negative control for LAMP is no-template control, depicted as LAMP-NTC. For detection controls, negative control, with no LAMP product, is shown as Det. negative in the graph. For positive control, pJET1.2_NDM was used, depicted as Det. positive.
Validation of PathCrisp assay using unknown CRE samples confirms its precision
Fifty Carbapenem-resistant Enterobacteriaceae (CRE) isolates were collected from patients at Sri Venkateswara Institute of Medical Sciences, Tirupati. Details about samples with VITEK data are available in Table S2. Sample BF-1302 could not be cultured and was therefore excluded from further analysis. We tested 49 samples, using the PathCrisp assay in batches of seven samples each, as shown in Fig. 4. Among 49 samples, only sample CRE-27 was negative for NDM. To validate the assay, samples were also tested using the PCR method with electrophoresis-based detection (Figure S1). Positive bands were given for sequencing to confirm the results. However, few samples had non-specific bands or no band: samples CRE-22, CRE-23, CRE-27, CRE-33, CRE-36, CRE-47, CRE-48. To confirm the presence of the NDM gene, discrepant samples were amplified using three different sets of primers (Figure S2) and confirmed by Sanger sequencing (Table S3). Sequencing results confirmed that, except for CRE-27 all other samples were positive for NDM.
Tested PathCrisp assay on unknown CRE samples 49 carbapenem-resistant enterobacteriaceae (CRE) isolates obtained from patient samples were tested for the presence of NDM using PathCrisp assay. The obtained RFU values are normalized to the detection negative of each batch and plotted here. For a few samples, the assay was repeated twice, once with Bst 1.0 (without UDG) depicted as circles in the graph and a second time with BST 2.0 (with UDG) depicted as diamonds in the graph. The average value of each sample in case of repetition is represented as a bar graph, while individual values are marked either as circles or diamonds. Grey dotted lines represent the cutoff to consider if the sample is positive, which is the average of RFU of LAMP-NTC plus 3 times Std. deviation. The 49 samples obtained were either K. pneumoniae (striped bars) or E. coli (solid coloured bar). In each batch, the negative control for LAMP is no-template control, depicted as LAMP-NTC. For detection controls, negative control, with no LAMP product, is shown as Det. negative in the graph. For positive control, pJET1.2_NDM was used, depicted as Det. positive.
The diagnostic testing accuracy of the PathCrisp assay and the PCR were evaluated against Sanger sequencing results which is considered the gold standard (Table 3). The sensitivity of the PCR test was 85.42% while the PathCrisp assay was 100%. The specificity of both tests was 100%. The Sanger sequencing files have been deposited in NCBI, the GenBank accession numbers for the same are PQ324711-PQ324770.
Testing PathCrisp assay on crude extract
In our study, the PathCrisp assay was validated using pure extracted DNA from clinical bacterial isolates, to reduce cost and further processes, we tested if the assay is compatible with crude extracts of DNA from the culture. For this, we transformed DH5⍺ E. coli cells with pJET1.2_NDM and used two types of samples (1) Colony from agar plate and (2) overnight inoculated broth. In both cases, NDM-positive samples were successfully detected against negative controls, repeatedly (Fig. 5).
PathCrisp test on crude extract pJET1.2_NDM transformed DH5⍺ E. coli cells were used to test the PathCrisp assay, after crude extraction. The assay was repeated twice, once with Bst1.0 (without UDG) depicted as circles in the graph and the second time with BST2.0 (with UDG) depicted as diamond shapes in the graph. The average value of each sample is represented as a bar graph while individual values are marked either as a circle or a diamond. The grey dotted lines represent the cutoff to consider if the sample is positive, which is the average of RFU of LAMP-NTC plus 3 times standard deviation. Negative control for media was also included for each type of culture: LB Agar plate and LB broth, respectively. The negative control for LAMP is no-template control, depicted as LAMP-NTC. For detection controls, negative control, with no LAMP product, is shown as Det. negative in the graph. For positive control, 0.3 nM pJET1.2_NDM was used, depicted as Det. positive.
Discussion
Our PathCrisp-NDM assay, a Cas12a-based detection method, employs a carefully designed guide to target an NDM region conserved across variants. Notably, recently Shin, Jiyong, et al. (2024) published a PCR-amplified Cas12a-based detection method for NDM using a sgRNA similar to our PathCrisp guide30. Additionally, Curti, Lucia Ana et al. (2020), reported that the Cas12a-based NDM-gene detection capacity significantly increased with pre-amplified products compared to target DNA directly31 (summarized in Table S4). Our PathCrisp assay includes LAMP-based amplification, known for its high sensitivity12. While direct LAMP-based methods for NDM detection have also been proposed to improve sensitivity,33, using longer and multiple primers can compromise specificity. Therefore, we reported a combination, a LAMP-amplified CRISPR-Cas12a-based NDM diagnostics, supported by clinical sample testing, that benefits from isothermal amplification of LAMP and the precise secondary validation by CRISPR.
Previously, LAMP-based amplification followed by Cas12a-based detection has been proposed for NDM34. Here, the assay uses two different temperature conditions, LAMP at 65 °C for amplification and trans-cleavage at 37 °C for detection. Fuchs, Ryan T et al. (2022) compared different Cas12a enzymes and found both AsCas12a and LbCas12a, which we used, exhibit both cis and trans activity active at 48oC35, 36. Furthermore, to improve the specificity of LAMP-based detection of Neisseria meningitidis, the LbCas12a-based Trans-cleavage assay was set up at 55 °C by another group36. We advanced these studies by using a constant temperature of 60 °C for both steps of our assay. This resulted in a sequential assay maintained at 60 °C throughout, enabling the use of simple heating instruments like a water or heat block.
When the analytical sensitivity of different types of amplification methods was compared, LAMP was better than the gold standard PCR methods12. Additionally, the combination of Cas12a and LAMP is known for its high sensitivity and specificity34. An indepth review of CRISPR based diagnostics by Kumar et al.35, corroborates the superiority of the dual layer target confirmation that an assay like our PathCrisp uses. Our PathCrisp assay was able to detect as low as 700 copies when tested in a serial dilution of target-carrying plasmid. For AMR markers present in plasmid form, it is challenging to determine the copy number per CFU of bacteria and accurately determine the Limit of detection. Often, these AMR genes exist in multiple copies per plasmid, and each plasmid can be present in multiple copies per bacterium. Given that, the current limit of 700 copies detected using a surrogate plasmid through our PathCrisp assay is indeed promising.
The PCR method, a gold standard molecular method, was used to screen clinical samples for NDM positives. The previously reported PCR method26, when analysed on gel electrophoresis, showed that some of the samples had either no band or a non-specific band. However, many of these discrepant samples were positive for NDM when the PCR was repeated with different sets of primers. Meanwhile, our PathCrisp assay outperformed the gold standard PCR method in sensitivity.
Most of the LAMP-CRISPR/CAS12a-based diagnostics proposed used kit-based DNA extraction for target detection37,38,39. Many others have also proposed methods to extract DNA and increase the concentration of the target gene, such as immunocapture magnetic beads40 or directly boiling the culture34. In the present study, the latter method was used to prepare extracts, demonstrating that both types of culture: from plate and broth samples could be used as the template for the assay. This implies that for rapid diagnosis of NDM, patient samples could be cultured in relevant bacterial media and tested within a few hours of incubation. This could lead to a significant reduction in the time required to grow culture and eliminate the need for morphological analysis of colonies formed after several days of culture, which unfortunately continues to be the current dominant form of diagnosis. Although testing directly from culture is definitely an improvement from current methods, a direct blood test for NDM would be ideal in these conditions. This however currently remains a challenge which hopefully we will be able to address in the near future with the next version of PathCrisp.
In summary, we have developed a LAMP-CRISPR/Cas12a-based isothermal assay, PathCrisp for detecting the most notorious carbapenemase in South Asian countries, NDM. It outperformed the PCR method in detection and can detect low copy numbers. Furthermore, pretreated culture can be directly used for this analysis The PathCrisp assay was developed as a rapid, point-of-care test and is instrument-light and easy to set up. Although in the present study, fluorescence-based validation was used as a primary read-out, we are developing a lateral flow test for easy identification. Furthermore, we continue to develop this assay into a ‘one-pot’ (one tube which carries a combination of LAMP and CRISPR reagents) test to fill the point of need diagnostic requirement more effectively. For now, we will continue to extend this to the detection of other major carbapenemases and hope to build a robust diagnostic test to help clinicians decide on antibiotic therapy soon.
Data availability
Sequence data reported in this manuscript is being submitted to NCBI.
References
WHO. Antibacterial Agents in Clinical and Preclinical Development: An Overview and Analysis (World Health Organization, Geneva, 2024).
Armstrong, T., Fenn, S. J. & Hardie, K. R. JMM Profile: Carbapenems: A broad-spectrum antibiotic. J. Med. Microbiol. 70, 001462 (2021).
Laxminarayan, R. et al. Expanding antibiotic, vaccine, and diagnostics development and access to tackle antimicrobial resistance. Lancet Lond. Engl. 403, 2534–2550 (2024).
Jean, S.-S., Harnod, D. & Hsueh, P.-R. Global threat of carbapenem-resistant gram-negative bacteria. Front. Cell. Infect. Microbiol. 12, 823684 (2022).
WHO. Guidelines for the Prevention and Control of Carbapenem-Resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in Health Care Facilities (World Health Organization, Geneva, 2017).
Tesfa, T., Mitiku, H., Edae, M. & Assefa, N. Prevalence and incidence of carbapenem-resistant K. pneumoniae colonization: systematic review and meta-analysis. Syst. Rev. 11, 240 (2022).
Yong, D. et al. Characterization of a new metallo-β-lactamase gene, blaNDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob. Agents Chemother. 53, 5046–5054 (2009).
Das, S. The crisis of carbapenemase-mediated carbapenem resistance across the human–animal–environmental interface in India. Infect. Dis. Now 53, 104628 (2023).
Barman, P., Chopra, S. & Thukral, T. Direct testing by VITEK® 2: A dependable method to reduce turnaround time in Gram-negative bloodstream infections. J. Lab. Phys. 10, 260–264 (2018).
Yoon, E.-J. & Jeong, S. H. MALDI-TOF mass spectrometry technology as a tool for the rapid diagnosis of antimicrobial resistance in bacteria. Antibiotics 10, 982 (2021).
Vasala, A., Hytönen, V. P. & Laitinen, O. H. Modern tools for rapid diagnostics of antimicrobial resistance. Front. Cell. Infect. Microbiol. 10 (2020). https://doi.org/10.3389/fcimb.2020.00308
Foo, P. C. et al. Loop-mediated isothermal amplification (LAMP) reaction as viable PCR substitute for diagnostic applications: A comparative analysis study of LAMP, conventional PCR, nested PCR (nPCR) and real-time PCR (qPCR) based on Entamoeba histolytica DNA derived from faecal sample. BMC Biotechnol. 20, 34 (2020).
Moehling, T. J., Choi, G., Dugan, L. C., Salit, M. & Meagher, R. J. LAMP diagnostics at the point-of-care: emerging trends and perspectives for the developer community. Expert Rev. Mol. Diagn. 21, 43–61 (2021).
Jinek, M. et al. A programmable dual-RNA-guided DNA endonuclease in adaptive bacterial immunity. Science 337, 816–821 (2012).
Swarts, D. C. & Jinek, M. Mechanistic insights into the cis- and trans-acting DNase activities of Cas12a. Mol. Cell 73, 589-600.e4 (2019).
Chen, J. S. et al. CRISPR-Cas12a target binding unleashes indiscriminate single-stranded DNase activity. Science 360, 436–439 (2018).
Alcock, B. P. et al. CARD 2023: expanded curation, support for machine learning, and resistome prediction at the comprehensive antibiotic resistance database. Nucleic Acids Res. 51, D690–D699 (2023).
Sayers, E. W. et al. Database resources of the national center for biotechnology information. Nucleic Acids Res. 50, D20–D26 (2022).
Madeira, F. et al. Search and sequence analysis tools services from EMBL-EBI in 2022. Nucleic Acids Res. 50, W276–W279 (2022).
Larsson, A. AliView: a fast and lightweight alignment viewer and editor for large datasets. Bioinformatics 30, 3276–3278 (2014).
Karthikeyan, V. Vasundhara-Karthik/IlluminaBacSeq (2023).
Bortolaia, V. et al. ResFinder 4.0 for predictions of phenotypes from genotypes. J. Antimicrob. Chemother. 75, 3491–3500 (2020).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, Vienna, 2022).
Waterhouse, A. M., Procter, J. B., Martin, D. M. A., Clamp, M. & Barton, G. J. Jalview Version 2—a multiple sequence alignment editor and analysis workbench. Bioinformatics 25, 1189–1191 (2009).
NEBioCalculator. https://nebiocalculator.neb.com/#!/dsdnaamt.
Mahalingam, N. et al. Detection of antibiotic resistance determinants and their transmissibility among clinically isolated carbapenem-resistant Escherichia coli from South India. Med. Princ. Pract. 27, 428–435 (2018).
Camacho, C. et al. BLAST+: Architecture and applications. BMC Bioinform. 10, 421 (2009).
Shreffler, J. & Huecker, M. R. Diagnostic testing accuracy: sensitivity, specificity, predictive values and likelihood ratios. In StatPearls (StatPearls Publishing, Treasure Island, FL, 2024).
Ma, W. et al. Genetic and enzymatic characterization of two novel blaNDM-36, -37 variants in Escherichia coli strains. Eur. J. Clin. Microbiol. Infect. Dis. 42, 471–480 (2023).
Shin, J., Kim, S. R., Xie, Z., Jin, Y.-S. & Wang, Y.-C. A CRISPR/Cas12a-based system for sensitive detection of antimicrobial-resistant genes in carbapenem-resistant enterobacterales. Biosensors 14, 194 (2024).
Curti, L. A. et al. CRISPR-based platform for carbapenemases and emerging viruses detection using Cas12a (Cpf1) effector nuclease. Emerg. Microbes Infect. 9, 1140–1148 (2020).
Rathinasabapathi, P., Hiremath, D. S., Arunraj, R. & Parani, M. Molecular detection of New Delhi metallo-beta-lactamase-1 (NDM-1) positive bacteria from environmental and drinking water samples by loop mediated isothermal amplification of blaNDM-1. Indian J. Microbiol. 55, 400–405 (2015).
Feng, W. et al. Design of rapid detection system for five major carbapenemase families (blaKPC, blaNDM, blaVIM, blaIMP and blaOXA-48-Like) by colorimetric loop-mediated isothermal amplification. Infect. Drug Resist. 14, 1865–1874 (2021).
Xu, H. et al. A new method based on LAMP-CRISPR–Cas12a-lateral flow immunochromatographic strip for detection. Infect. Drug Resist. 15, 685–696 (2022).
Kumar, M. et al. Capturing nucleic acid variants with precision using CRISPR diagnostics. Biosens. Bioelectron. 217, 114712 (2022).
Fuchs, R. T. et al. Characterization of Cme and Yme thermostable Cas12a orthologs. Commun. Biol. 5, 1–16 (2022).
Trung, N. T. et al. CRISPR-Cas12a combination to alleviate the false-positive in loop-mediated isothermal amplification-based diagnosis of Neisseria meningitidis. BMC Infect. Dis. 22, 429 (2022).
Shi, Y. et al. Crispr/cas12a-enhanced loop-mediated isothermal amplification for the visual detection of shigella flexneri. Front. Bioeng. Biotechnol. 10 (2022).
Shaizadinova, A., Amanzholova, M., Kirillov, S., Bulashev, A. & Abeldenov, S. Rapid and highly sensitive LAMP-CRISPR/Cas12a-based identification of bovine mastitis milk samples contaminated by Escherichia coli. J. Agric. Food Res. 14, 100721 (2023).
Nguyen, L. T., Rananaware, S. R., Pizzano, B. L. M., Stone, B. T. & Jain, P. K. Clinical validation of engineered CRISPR/Cas12a for rapid SARS-CoV-2 detection. Commun. Med. 2, 1–11 (2022).
Li, C. et al. Immunocapture magnetic beads enhanced the LAMP-CRISPR/Cas12a method for the sensitive, specific, and visual detection of Campylobacter jejuni. Biosensors 12, 154 (2022).
Acknowledgements
We acknowledge Rockefeller Foundation Grant Number 2021 HTH 018 and financial aid by Axis Bank for funding the multi-centre AMR mapping and genomic analysis study at Ashoka University. Technical teams from Max Healthcare and Sahyadri Hospital for maintenance of pathogen culture stocks and DNA extractions. Yuvraj J. and Vasundhara K. for building the genomic assemblies. UGC-SAP-DRS-III, DST-FIST and DBT-BIF, Govt. of India for the infrastructural support to the Department of Biosciences, SSSIHL, Prasanthi Nilayam and ICMR-SRF from Govt. of India. Dr. BEP received extramural Research support from ICMR, Govt. of India. Abbireddy Sairam and Harinath Hemanth Bapat for their support with clinical sample extraction used for assay validation. CRISPRBITS team for their unwavering support, and a special mention to Bhargav CN, Salil Hangekar and Kanikah Mehndiratta for their scientific inputs, constant troubleshooting help and helpful discussions. We would also like to acknowledge ex-team member Bilal Shah for the initiation of this project and Santosh M and Lavanya C for administrative support. Additionally, we also would like to acknowledge the Sequencing facility of the National Center for Biological Sciences and Barcode Biosciences for sequencing DNA samples. RA would like to thank Z, Z and K for their love, strength and support.
Author information
Authors and Affiliations
Contributions
S.P., A.S., R.A., and V.G. contributed to the conceptual design of the study. S.P. conducted the development and validation of the PathCrisp assay with support from D.M., A.S., M.N., K.B.S. and V.H.. N.G., S.K., M.K., and B.T. sequenced and analyzed Indian clinical samples for designed oligos. J.R. and B.E.P provided clinical samples and extracted DNA for validating the PathCrisp. S.P., N.G., S.K. and R.A. performed the analyses and generated figures and tables. S.P. and R.A. wrote the manuscript. V.G., S.A. and V.C. provided input on subsequent drafts. All authors acknowledge full responsibility for the analyses and interpretation of the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Patil, S., Siji, A., Mallur, D. et al. PathCrisp: an innovative molecular diagnostic tool for early detection of NDM-resistant infections. Sci Rep 15, 490 (2025). https://doi.org/10.1038/s41598-024-84832-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-84832-z