Abstract
Appendicitis is the most common acute abdominal condition affecting general surgical practice. Recently, conservative treatment with antibiotics has been considered as an alternative. Therefore, this study was conducted to evaluate if antibiotics could be cost-effective compared to laparoscopic appendectomy or open appendectomy. A prospective study was undertaken to estimate health-related quality of life for antibiotic and operative treatment, and to ascertain costs in a cohort. A societal perspective incremental cost-effectiveness ratio (ICER) at 1 year after surgery was estimated. A probabilistic sensitivity analyses was performed. ICERs were estimated comparisons between individual antibiotics, laparoscopic appendectomy, and open appendectomy in uncomplicated acute appendicitis. Antibiotics showed improved cost savings compared to operative treatments with an ICER of -113,973.09 USD per quality adjusted life year at 1 year. Based on one year findings, antibiotics represent a lower cost treatment option with better cost-utility compared to operative treatment options in uncomplicated acute appendicitis patients. As such, antibiotic treatment can be initially considered as an alternative option where resources are limited to minimize complication rates associated with operative treatments.
Similar content being viewed by others
Introduction
Appendicitis is the most common acute abdominal condition in general surgical practice with an approximate incidence of 1 in 1000 person years1,2. Standard treatment is either open appendectomy or laparoscopic appendectomy, which can result in intra- and post-operative complications ranging from 2–23%3,4,5, with more than 3% of patients commonly readmitted with intestinal obstructions and post-operative adhesions6,7,8.
Recently, conservative treatment with antibiotics has been considered an alternative treatment option for uncomplicated appendicitis, including third generation cephalosporin, metronidazole/tinidazole, beta-lactam antibiotics, penicillin, and combinations thereof. The results from a recent network meta-analysis9 suggest the use of antibiotics for treating uncomplicated appendicitis would result in about 12–32% lower treatment success at 1 year than appendectomy but about 23–86% fewer complications, which corresponded with findings from a previous meta-analysis10. In addition, this network meta-analysis also suggested that beta-lactam with/without penicillin was ranked first for treatment success and had the least complications compared to other antibiotic regimens. Furthermore, the most recent randomized control trial (RCT)11 also found that the treatment success rate after 1 year was 65% or higher for both oral monotherapy of antibiotics and intravenous antibiotics followed by oral antibiotics.
Treatment of uncomplicated appendicitis should also consider clinical outcomes in combination with health-related quality of life (HRQoL) to inform a cost-utility analysis (CUA). The majority of previous studies in adults have highlighted improved HRQoL associated with antibiotic treatments compared to laparoscopic appendectomy12,13,14,15 in developed countries. Of them, only one16 considered a CUA with a hospital perspective reporting antibiotic treatment to be more cost effective than laparoscopic appendectomy with cost reductions of 1,865 USD and 0.04 quality adjusted life years gained. Only a single RCT17 in adults included a cost analysis with a societal perspective, reporting overall costs 1.6 times higher in laparoscopic appendectomy compared to antibiotics. This study was continued to 7 year follow up13 reporting no difference in long term HRQoL but lower satisfaction in patients who received antibiotics and later underwent appendectomy compared to patients with successful antibiotics or appendectomy outcomes. Most economic evidence has been generated from developed countries, evidence from developing countries is still lacking, particularly using CUA from a societal perspective. As such, this study used real practice data to assess HRQoL and CUA comparing individual antibiotics with appendectomy. This evidence will inform practitioners in treatment management for uncomplicated acute appendicitis.
Materials and methods
This prospective cohort study was conducted between November 2018 and October 2019 in the Department of Surgery, Faculty of Medicine, Ramathibodi Hospital, Bangkok, Thailand. This study had been approved by the ethical committee of Ramathibodi Hospital (#COA. MURA2019/1212). The study was confirmed that all participants were signed informed consent according to the Declaration of Helsinki. All adult patients were included based on the criteria of diagnosed with uncomplicated appendicitis and without ruptured or gangrenous symptom (proven by ultrasonography or computer tomography) were eligible if they received either antibiotics or appendectomy. Patients were later diagnosed as complicated appendicitis by operation were excluded. Clinical outcome (i.e., complication/recurrence) and utilities were assessed during follow up for 1 month and 1 year post treatment, if patients were willing to participate following written informed consent.
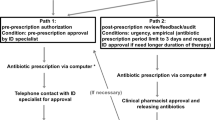
CUA was performed to compare, cost, and quality adjusted life year between two interventions (antibiotic and appendectomy) using a decision tree model with 1 year time horizon in societal perspective, see Fig. 1.
Interventions of interest included three antibiotics (beta-lactam, quinolone, and cephalosporin + metronidazole) and two operative modalities (open appendectomy and laparoscopic appendectomy). Laparoscopic appendectomy was performed by single to three port incision and open appendectomy was performed using McBurney’s point muscle-splitting incision immediately at the area of appendectomy. However, the treatment allocation was not manipulated because of the nature of study design with depended on the condition of the patients and the surgeon or patients preferences.
Cost and utility score measurements
Three main categories of direct medical cost data for medical services/resources and treatments for appendicitis patients between 2013 and 2017 were retrieved. All costs were adjusted to 2021 rates using an inflation rate from the national bank of Thailand18. Costs were converted to USD (33.223 Baht/USD) and classified into three categories: drug, equipment, and staff. The costs associated with complications for operative and antibiotic treatments were also included within the model. Direct non-medical and indirect costs were collected by patient interview at the following time points: before receiving intervention, discharge, 1 week, 1 month and 1 year post discharge. HRQoL was measured by a European Quality of Life-5 Dimensions questionnaire at the time points indicated for each treatment with conversion to a Thai utility score reflecting perception of HRQoL. Scores ranged from 0 to 1, with 0 meaning worse/death and 1 meaning better health status19. Quality adjusted life years were calculated by multiplying 1 month and 1 year utility scores by 365 days. Patient’s electronic medical records were reviewed for any complication or recurrence that occurred within 1 year after discharge.
Transition probability
The transition probability of a decision tree model demonstrates the effect size for each outcome of interest and the corresponding confidence intervals (95% CI). For antibiotic treatments, probabilities of transition to success (complete response without recurrence), failure (did not complete response during admission), and recurrence (repeated occurrence of appendicitis within one month) were applied based on the network meta-analysis effect size and 95% CI(9). For operative treatments, transition probabilities of success (complete operation and confirmed pathology as acute appendicitis), complication-free (success of the initial operation with no postoperative complications, adverse events, or operative failure occurring) and complications (major complications of operative treatment including: wound infection, wound hematoma, wound dehiscence, intra-abdominal abscess and other complications within one month)10 were applied according to the effect size and 95% CI from an umbrella review20.
Statistical analysis
Data were described using mean (± standard deviation) or median (interquartile range) for continuous variables and frequency (%) for categorical variables, respectively. The utility scores following treatment were compared between interventions using a treatment effect model with inverse-probability-weighted regression adjustment (IPWRA)21. Two equations were constructed. Firstly, a treatment model was constructed based on regressing interventions on co-variables (i.e., age, body mass index (BMI), nausea, neutrophil/lymphocyte ratio, utility score at baseline, and time) using a multi-logit link function. A propensity score was estimated as a weight in step 2. Secondly, the outcome model constructed was based on regressing the utility score for interventions with IPWRA with adjustment for co-variables (i.e., age, BMI, nausea, neutrophil/lymphocyte ratio, and utility score at baseline). Potential outcome mean (POM) and average treatment effect (ATE) were estimated for each intervention.
For CUA, all costs and quality adjusted life years for each treatment represented roll back transition probabilities from the decision tree model, then an incremental cost-effectiveness ratio (ICER) was calculated by dividing the incremental total admission cost by the incremental quality adjusted life year of any treatment comparison19. The treatment of interest was cost-effectiveness if the ICER was less than a willingness to pay threshold. A probabilistic sensitivity analysis to account for the uncertainty in the CUA model considered 1,000 simulations by Monte-Carlo methods based on beta and gamma distributions for incremental utilities and costs, respectively. As a result, the model presentation was estimated in the cost-effectiveness scatter plot and was evaluated against the ceiling ratio or willingness to pay in a cost-effectiveness acceptability curve. Data were analyzed in STATA version 16, and all simulations were performed by TreeAge® Pro version 202122.
Results
A total of 226 patients with uncomplicated acute appendicitis were included in the study. Among them, 138 (61%), 8 (3.5%), 18 (7.9%), 13 (5.7%), and 49 (21.6%) patients received open appendectomy, laparoscopic appendectomy, beta-lactam, quinolone, and cephalosporin + metronidazole, respectively. Mean (± standard deviation) utility scores at baseline between the five groups were not significantly different, see Table 1. The mean age and BMI were also not significantly different between groups, although diabetes mellitus, nausea, vomiting, and median neutrophil/lymphocyte ratio were statistically different (P-value: 0.016, 0.011, 0.007, and < 0.001 respectively).
Comparison of utility scores
All patients were available for interview at 1 month and 1 year follow-up. A counterfactual approach was applied to assess the effects of the five treatments on utility scores. The treatment model was constructed to balance factors associated with treatment allocations, see supplementary document. Three factors (i.e., nausea, neutrophil/lymphocyte ratio, and baseline utility score) were significantly associated with treatment allocation between intervention groups.
The outcome model was generated from the IPWRA estimated from the treatment model. The POMs for the utility scores following treatment during hospitalization were 0.91, 0.89, 0.91, 0.30 and 0.03 for beta-lactam, quinolone, cephalosporin + metronidazole, laparoscopic appendectomy, and open appendectomy respectively. As a result, the ATEs were significantly higher for the three antibiotics and laparoscopic appendectomy relative to open appendectomy, see Table 2.
The utility scores at 1 month follow-up were much improved for all interventions, i.e., 1.00, 1.00, 0.99, 0.93, and 0.98 for beta-lactam, quinolone, cephalosporin + metronidazole, laparoscopic appendectomy, and open appendectomy, respectively, see Table 2. The ATEs (95% CI) were not significant for the interventions with the exception of beta-lactam. At 1 year follow up, the utility scores were return to normal for all interventions, i.e., 0.99, 1.00, 0.99, 1.00, and 0.99 for beta-lactam, quinolone, cephalosporin + metronidazole, laparoscopic appendectomy, and open appendectomy, respectively; only ATEs of quinolone and laparoscopic appendectomy were significant.
CUA
The CUA compared cost and utility of antibiotic and operative treatments for uncomplicated acute appendicitis with a societal perspective. Direct medical costs associated with appendectomy drugs and equipment were higher than with antibiotic treatments. Furthermore, direct non-medical and indirect costs associated with operative treatments were also higher compared to antibiotics, see Table 3.
Overall means for utility scores and transition probabilities for 1 month post antibiotic and operative treatments were estimated and stratified by complication/recurrence, see Table 4. For open appendectomy and laparoscopic appendectomy at 1 month, the utility scores ranged between 0.50 and 0.71 and 0.66–0.94 with and without wound complications. Taking into account recurrence of appendicitis, the utility scores for antibiotics were 0.60, 0.74, and 0.66 for beta-lactam, cephalosporin + metronidazole, and quinolone. Utility scores for all interventions were higher in the absence of complications or recurrence of appendicitis, i.e., 0.58, 0.66, 0.96, 0.97, and 0.98, respectively for beta-lactam, quinolone, cephalosporin + metronidazole, laparoscopic appendectomy and open appendectomy. Occurrence of complications in open appendectomy and laparoscopic appendectomy ranged from 17 to 56% and 20–44%, respectively. At 1 year, utility scores for all modalities were improved to 0.98 to 1.00.
Results of the decision tree model are described in Table 5. Comparisons between overall antibiotic and appendectomy resulted in cost-savings with an ICER of -113,973.09 USD per quality adjusted life year, i.e., we could save money if patients were treated with antibiotics instead of appendectomy.
Among the antibiotics investigated, the ICERs for beta-lactam and quinolone relative to cephalosporin + metronidazole were 853,235.00 and − 156,406.67 USD respectively per quality adjusted life year, which could be interpreted that patients treated with beta-lactam would pay less but receive less benefit, or alternatively if patients changed to cephalosporin + metronidazole, they would pay 853,235 USD more for each quality adjusted life year gained. With negative ICER, patients using quinolone represented a cost-saving as there was more benefit to be gained with less cost paid. The ICER for laparoscopic appendectomy relative to open appendectomy was 24,626.07 USD per quality adjusted life year, highlighting the benefits of the former compared to the later with its higher costs. Overall, at 1 year post treatment, beta-lactam was most cost-effective in comparison to the other antibiotics and open appendectomy was more cost-effective compared to laparoscopic appendectomy.
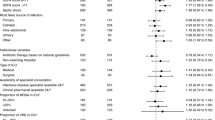
Incremental cost and effectiveness scatter plots were based on 1,000 Monte-Carlo simulations, see Fig. 2. Each plot was divided into 4 areas, i.e., the southeast quadrant (cost-saving, i.e., more effectiveness at less cost), northwest quadrant (i.e., more cost and less effectiveness), northeast quadrant (i.e., more cost and more effectiveness) and southwest (i.e., less cost and less effectiveness); the last two quadrants are required for the comparison of willingness to pay thresholds. Antibiotics offered greater cost-savings in comparison to appendectomy, see Fig. 2A. For the 2 different types of appendectomy, the values were scattered in all quadrants but most of them were in the southeast quadrant, i.e. laparoscopic appendectomy might be more effective than open appendectomy, see Fig. 2B. Among antibiotic treatments, most values were centrally scattered for all comparisons (see Fig. 2C,E), suggesting the cost-effectiveness of antibiotics as a treatment option might be dependent on willingness to pay.
Cost-effectiveness acceptability curves illustrate the percentage cost-effectiveness (y-axis) in relation to a given willingness to pay (x-axis), see Fig. 3. Antibiotics were more cost-effective for all willingness to pay levels compared to overall appendectomy, see Fig. 3A. Likewise, beta-lactam was more cost-effective in comparison to other antibiotics for all willingness to pay thresholds (Fig. 3C). For operative comparisons, laparoscopic appendectomy was more cost-effective at willingness to pay thresholds in excess of 4,816 USD per quality adjusted life year.
Discussion
This cohort study compared utility scores and CUA of three antibiotics (beta-lactam, quinolone, and cephalosporin + metronidazole) and two appendectomy modalities (laparoscopic appendectomy and open appendectomy) in uncomplicated acute appendicitis. The ATEs for antibiotics (beta-lactam, quinolone, and cephalosporin + metronidazole) and appendectomy (open appendectomy and laparoscopic appendectomy) during hospitalization and 1 month after discharge were considered for each outcome of interest (success, complications and recurrence). The ICER identified beta-lactam with the lowest cost at 4,086.56 USD, followed by quinolone (4,845.91), cephalosporin + metronidazole (5,831.42), open appendectomy (7,877.05), and laparoscopic appendectomy (8,358.42), for a quality adjusted life year gain at 1 year after treatment. cost-effectiveness ratios with a time horizon of 1 year, estimated that operative treatment cost at almost twice those compared to any antibiotic use. A one-year follow-up period should be sufficient for assessing recurrence, as previous RCT have concluded that the median time to recurrence of appendicitis is approximately 102 days2.
HRQoL utility scores were significantly higher for beta-lactam, quinolone, and cephalosporin + metronidazole compared to either laparoscopic appendectomy or open appendectomy following treatment during hospitalization. However, overall utility scores at one month post treatment were much improved for all interventions, with only beta-lactam demonstrating a significantly higher utility score approximating 0.03 (0.01, 0.05) compared to open appendectomy. This difference might not be clinically significant as the previous study also found antibiotics were non-inferior to appendectomy with the difference of 30-day utility score of 0.01 (-0.001, 0.03)23. Moreover, the overall utility scores at 1 year post treatment were improved and returned to normal for all interventions. However, previous comparisons of antibiotics with laparoscopic appendectomy reported higher HRQoL values associated with antibiotic treatments compared to laparoscopic appendectomy at 1 year (0.872 versus 0.802 in adults)16. In addition, a recent RCT13 showed similar HRQoL at 7 year long term follow-up for antibiotic and operative treatments with a median health index value (95% CI) of 1.0 (0.86, 1.0), with patient satisfaction indicating those who received operative treatments were more satisfied than patients who had received antibiotic treatment (68% versus 53%, respectively). Previous HRQoL evidence over equivalent timeframes have shown similar findings between antibiotics and appendectomy and as such, the level of variation in the utility scores may be time dependent.
Our CUA showed that antibiotic treatment options presented cost-savings compared to operative treatment options with ICER of -113,973.09 USD per quality adjusted life year at 1 year. These findings support previously reported cost effectiveness of antibiotic use over operative treatment with ICER ranging between 1,865 and 4,271 USD per quality adjusted life year for antibiotics treatment compared to 172,600 − 427,100 USD per quality adjusted life year for operative treatments12,16 and the most recent study reported antibiotic treatment savings approximating − 30,759.65 USD for each quality adjusted life year gained compared to appendectomy15. The cost-effectiveness ratio for operative treatments in our study was higher compared to that for antibiotic treatments, similar to previous RCT, although the latter had not also been considered utility17.
Our previous network meta-analysis9 suggested that all antibiotics were about 12–32% lower in success rates when compared with appendectomy, which corresponded with a previous meta-analysis10. laparoscopic appendectomy and open appendectomy comparisons from our umbrella review of 10 systematic reviews and meta-analyses suggested that laparoscopic appendectomy had significantly lower infection risk ranging from 0.47 to 0.67 but showed a higher intra-abdominal abscess risk approximately 1.2 times greater than open appendectomy20. Although, the benefit of laparoscopic appendectomy appear beneficial compared to the risks, a recent study also showed that a per-oral antibiotic treated in out-patients might be sufficient relative to intravenous followed by oral antibiotics treated in-patients with acute uncomplicated appendicitis11.
The issue of antibiotic resistance should also be considered regarding Clostridium difficile growth in intestinal flora among antibiotic users24. Use of broad-spectrum antibiotics are more likely to lead to the development of flora infections when compare to penicillin regimen combinations25. Long term antibiotic resistance among different pharmacological types warrant further investigation.
Our study had several strengths. We investigated an adult cohort of acute uncomplicated appendicitis for CUA to compare utility scores using a counter-factual approach by treatment effect model. Our data was representative of real clinical practice to emulate a randomized-controlled trial26, using the IPWRA method. All costs, including direct medical and non-medical costs, and indirect costs with societal perspectives, were appropriately considered. Standard direct costs from the Ramathibodi Hospital were used which are generalizable to similar healthcare settings and economic models.
Our study also had some limitations. The sample size for each antibiotic and laparoscopic appendectomy/open appendectomy against individual outcomes (i.e., recurrence, wound complication) was small, therefore, analysis of individual antibiotic and operation approach could not be undertaken, limiting the certainty associated with the HRQoL outcomes for each branch of the decision tree. Furthermore, laparoscopic appendectomy was more commonly used in developed countries, while it was still very much less applied relative to open appendectomy in our and other settings in developing countries, due largely to the cost of implementation and maintenance, and a lack of trained surgeons27,28. Therefore, our findings may have been less precise, particularly for laparoscopic appendectomy, and may be less generalizable to countries where laparoscopic appendectomy is commonly performed.
In summary, our findings suggest that antibiotic treatments may represent a higher utility score and cost effective than appendectomy. Costs associated with antibiotic treatments may be as much as half that of appendectomy. Therefore, antibiotics should be considered as a treatment option for patients if surgery is contraindicated, or patients prefer a non-surgical alternative. However, the potential post treatment consequences particularly for appendicitis recurrence and post-operative complications, should be carefully considered in a balanced risk benefit assessment.
Conclusions
Antibiotics represent a more cost effective treatment option for the management of acute uncomplicated adult appendicitis in both short and long term. Therefore, antibiotic treatment may be offered as an initial or alternative option for patients with contraindications for surgery and uncomplicated acute appendicitis, to those who prefer not to undergo surgery or to patients who are more likely to develop post-surgical complications.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Di Saverio, S. et al. The NOTA study (Non operative treatment for acute Appendicitis): prospective study on the efficacy and safety of antibiotics (amoxicillin and clavulanic acid) for treating patients with right lower quadrant abdominal pain and long-term follow-up of conservatively treated suspected appendicitis. Ann. Surg. 260 (1), 109–117 (2014).
Salminen, P. et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. Jama 313 (23), 2340–2348 (2015).
Emil, S. & Duong, S. Antibiotic therapy and interval appendectomy for perforated appendicitis in children: a selective approach. Am. Surg. 73 (9), 917–922 (2007).
Malik, A. A. & Bari, S. U. Conservative management of acute appendicitis. J. Gastrointest. Surgery: Official J. Soc. Surg. Aliment. Tract. 13 (5), 966–970 (2009).
Omundsen, M. & Dennett, E. Delay to appendicectomy and associated morbidity: a retrospective review. ANZ J. Surg. 76 (3), 153–155 (2006).
Leung, T. T., Dixon, E. & Gill, M. Bowel obstruction following appendectomy what is the true incidence? Ann. Surg. 250, 51–53 (2009).
Parker, M. C., Ellis, H. & Moran, B. J. Postoperative adhesions: ten-year follow-up of 12,584 patients undergoing lower abdominal surgery. Dis. Colon Rectum. 44, 822–829 (2001).
Vons, C. et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet 377 (9777), 1573–1579 (2011).
Poprom, N. et al. The efficacy of antibiotic treatment versus surgical treatment of uncomplicated acute appendicitis: systematic review and network meta-analysis of randomized controlled trial. Am. J. Surg. 218 (1), 192–200 (2019).
Harnoss, J. C. et al. Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and Meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann. Surg. (2016).
Sippola, S. et al. Effect of oral Moxifloxacin vs intravenous ertapenem plus oral Levofloxacin for treatment of uncomplicated acute appendicitis: the APPAC II randomized clinical trial. Jama 325 (4), 353–362 (2021).
Sceats, L. A. et al. Operative versus nonoperative management of appendicitis: A Long-Term cost effectiveness analysis. MDM Policy Pract. 4 (2), 2381468319866448 (2019).
Sippola, S. et al. Quality of life and patient satisfaction at 7-year follow-up of antibiotic therapy vs appendectomy for uncomplicated acute appendicitis: A secondary analysis of a randomized clinical trial. JAMA Surg. (2020).
Turhan, A. N. et al. Comparison of operative and Non operative management of acute appendicitis. Ulusal Travma Ve Acil Cerrahi Dergisi. 15 (5), 459–462 (2009).
Ali, A. et al. Cost-utility analysis of antibiotic therapy versus appendicectomy for acute uncomplicated appendicitis. Int. J. Environ. Res. Public Health 18 (16). (2021).
Wu, J. X., Dawes, A. J., Sacks, G. D., Brunicardi, F. C. & Keeler, E. B. Cost effectiveness of nonoperative management versus laparoscopic appendectomy for acute uncomplicated appendicitis. Surgery 158 (3), 712–721 (2015).
Sippola, S. et al. Economic evaluation of antibiotic therapy versus appendicectomy for the treatment of uncomplicated acute appendicitis from the APPAC randomized clinical trial. Br. J. Surg. 104 (10), 1355–1361 (2017).
Bank of Thailand. Foreign Exchange Rates. Bangkok: Bank of Thailand. (2020).
Pattanaphesaj, J. et al. The EQ-5D-5L valuation study in Thailand. Expert Rev. Pharmacoecon Outcomes Res. 18 (5), 551–558 (2018).
Poprom, N. et al. Comparison of postoperative complications between open and laparoscopic appendectomy: an umbrella review of systematic reviews and meta-analyses. J. Trauma. Acute Care Surg. 89 (4), 813–820 (2020).
Stata Statistical Software: Release 16 [computer program]. College Station, TX: StataCorp LLC; (2019).
TreeAge Software [computer program]. Williamstown, MA: TreeAge Software, Inc; (2021).
Flum, D. R. et al. A randomized trial comparing antibiotics with appendectomy for appendicitis. N. Engl. J. Med. 383 (20), 1907–1919 (2020).
Huston, J. M. et al. Antibiotics vs. Appendectomy for acute uncomplicated appendicitis in adults: review of the evidence and future directions. Surg. Infect. (Larchmt). 18 (5), 527–535 (2017).
Slimings, C. & Riley, T. V. Antibiotics and hospital-acquired Clostridium difficile infection: update of systematic review and meta-analysis. J. Antimicrob. Chemother. 69 (4), 881–891 (2014).
Desai, R. J. & Franklin, J. M. Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners. Bmj 367, l5657 (2019).
Pizzol, D. et al. Laparoscopy in low-Income countries: 10-year experience and systematic literature review. Int. J. Environ. Res. Public Health 18 (11). (2021).
Alfa-Wali, M. & Osaghae, S. Practice, training and safety of laparoscopic surgery in low and middle-income countries. World J. Gastrointest. Surg. 9 (1), 13–18 (2017).
Author information
Authors and Affiliations
Contributions
NP: Study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, and critical revision of the manuscript. OP: Study concept and design, analysis and interpretation of data, and critical revision of the manuscript. CW: Technical and material support, and critical revision of the manuscript. SR: Acquisition of data, analysis and interpretation of data. GJM: Critical revision of the manuscript. JA: Critical revision of the manuscript. AT: Concept and design, analysis and interpretation of data, drafting of the manuscript, and critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study had been approved and consent by the ethical committee of Ramathibodi Hospital (#COA. MURA2019/1212).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Poprom, N., Pattanaprateep, O., Wilasrusmee, C. et al. Cost utility analysis of antibiotics compared with operative treatment in uncomplicated acute appendicitis. Sci Rep 15, 14963 (2025). https://doi.org/10.1038/s41598-025-00111-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-00111-5