Abstract
Myopia is a global pandemic, with significant adverse effects on visual health. It is imperative to establish a more comprehensive and inclusive myopia control that can address the lack of myopia defences due to age, refractive error and astigmatism range. In this study, we evaluated the efficacy of multifocal rigid gas-permeable contact lenses (MF-RGPCL) as a myopia control intervention.The efficacy of MF-RGPCL were assessed by the changes in axial length (AL) and best-corrected visual acuity (BCVA), and the safety was evaluated by monitoring the changes in corneal endothelial cells. Furthermore, an analysis was conducted on subjects’ ocular parameters, genetic characteristics, lens’ fit, growth and development and which may influence AL progression in the MF-RGPCL group. Following a 12-month period, the axial elongationAL of the MF-RGPCL group was significantly slower than that of the single-vision spectacle lenses (SVL) group. Similarly, the BCVA of the MF-RGPCL group was significantly better than that of the SVL group. And the AL progression in the MF-RGPCL group was significantly correlated with onset age of myopia, parental myopia, lens decentration, pupil diameter, and corneal curvature. No significant alterations were observed in the corneal endothelial cells. MF-RGPCL has been demonstrated to provide effective myopia control and good safety, and can be used as an alternative for myopia defence in adolescents. Complementary clinical indications for orthokeratology lenses (OK lenses) and multifocal soft contact lenses (MF-SCL).
Similar content being viewed by others
Introduction
Myopia represents a significant factor affecting visual health1,2, with an estimated prevalence of 30% in the global population3. Epidemiological projections suggest that nearly 50% of the global population will be myopic by 2050.The prevalence of myopia among young adults in East and Southeast Asia is approximately 80–90%4, while the myopia rate among children and adolescents aged 6–18 in China is approximately 53.6%5. In China, the increased prevalence of electronic products and the concomitant rise in academic pressure have resulted in a notable increase in nearwork time6,7 and a marked reduction in outdoor activities8,9. Under the “heavy attack” of these factors, the development of myopia shows a trend of low age, high incidence rate and high diopter. The onset age of myopia is a significant predictor of its subsequent progression10,11 In the absence of timely intervention, myopia will progress at an alarming rate, with the potential for it to develop into high myopia, which represents a significant threat to the health of the fundus. The risk of fundus disease in individuals with high myopia is more than 40 times higher than that of the general population, and is accompanied by complications such as cataract, glaucoma, retinal detachment and macular degeneration12,13,14. Given the current lack of evidence-based strategies to prevent myopia initiation, optimizing interventions to decelerate myopia progression and reduce progression rates to high myopia (-6.00 D or greater) represents the paramount clinical priority for managing this global epidemic. The current effective prevention and control measures for myopia include increasing the time spent in outdoor activities8,15, low-concentration atropine16,17,18, orthokeratology lenses (OK lenses)19,20,21, multifocal soft contact lenses (MF-SCL)22,23,24, and peripheral defocus modifying spectacle lenses25,26,27,28. Among them, OK lenses, as the most established one, although its efficacy and safety have been widely recognised, CFDA has strict limitations on age (< 8 years old) and myopic diopter registration range ( ≦ 6.00 D); MF-SCL, although it can make up for the limitations of OK lenses mentioned above, it does not have a ideal effect on the correction of high astigmatism but have a high cost. Low concentration atropine can not meet the needs of myopia correction. Peripheral defocus modifying spectacle lenses can correct myopia above 6.00 DS. However, this approach is constrained by alterations in spatial perception and visual field parameters due to vertex distance effects, which may further impede children’s engagement in dynamic physical activities. Therefore, for patients with myopic refraction above 6.00 D, age less than 8 years old, with large astigmatism, who need to control myopia and free from glasses, the above modalities are obviously not applicable. In this case, a new type of defocus designed rigid gas permeable contact lens (MF-RGPCL) has a significant benefit for this particular patient group. MF-RGPCL offer a number of advantages over traditional RGP lenses. In addition to high oxygen permeability, moisture content, and high imaging quality, these lenses combine the classic design of peripheral retinal myopia defocus29 with greater inclusivity for the wearer’s age, refractive range, and corneal astigmatism.
It is therefore imperative to conduct further clinical studies on the efficacy of MF-RGPCL in controlling myopia in adolescents and children, in order to expand the range of myopia prevention and control methods currently available. Despite the clinical application of MF-RGPCL having been several years, there is still no clear report on the effect of MF-RGPCL on myopia control in adolescents and children. This paucity of clinical evidence likely stems from the limited adoption of MF-RGPCL in clinical practice. To address this gap, the current study retrospectively enrolled MF-RGPCL wearers to longitudinally monitor AL progression and BCVA over a 12-month period to evaluate the efficacy for myopia control, while the ocular safety through serial assessments of corneal endothelial parameters (CD, CV, HEX). Furthermore, multivariable analyses were conducted to identify determinants influencing treatment outcomes, incorporating ocular biometrics, genetic predisposition, lens fitting characteristics, and auxological indices. This will facilitate the provision of more reliable options for clinical work in myopia prevention and control.
Results
Baseline characteristics of participants in the MF-RGPCL and SVL groups
After screening, 48 MF-RGPCL wearers (12.33 (± 2.1) years old, male 20 (42%), female 28 (58%)), and 21 SVL wearers (13.40 (± 2.40) years old, male 9 (43%), female 12 (57%)) were included in the statistics. The baseline data are shown in Table 1; Fig. 1. There is no significant difference in the baseline date of each parameter between the two groups (all P > 0.05). At the same time, it can be seen from the heatmap that the baseline color changes and color scales of each parameter in the two groups of data are basically consistent, which ensures the principle of unique variables in the control experiment. It can be seen that the ratio of male to female in the two groups was similar, and the age of onset of myopia was earlier (SVL, 6.89(± 0.25) years old; MF-RGPCL, 7.00(7.00 (± 0.17) years old), IOP was high than normal (SVL, 18.10(± 2.61)mm/Hg; MF-RGPCL, 19.21(± 2.56) mm/Hg), spherical equivalent (SVL, −8.71 (± 2.3) D; MF-RGPCL, −8.59(± 2.3)D) and AL (SVL, 26.30(± 1.04) mm; MF-RGPCL, 26.55(± 1.17) mm) reached the high myopia. In addition, the family history survey of myopia in both groups of patients found that one or both parents had a higher proportion of myopia. These results suggest that patients who choose to wear MF-RGPCL are mostly a group with high myopia or high-risk factors for high myopia.
Changes in axial lenth in one year
The mean annual axial elongation was significantly lower in the MF-RGPCL group (0.18 ± 0.015 mm) compared to the SVL group (0.33 ± 0.018 mm; P < 0.0001)., and the remission rate (= ([ (Annual axial elongation in control group − Annual axial elongation in observation group) / Annual axial elongation in control group ] × 100%))was 46%( Control group: SVL group; Observation group: MF-RGPCL group) (Fig. 2a). Although the annual axial elongation of the MF-RGPCL group is widely distributed (-0.2 mm ~ 0.6 mm), most of the participants (64%) have an annual axial elongation ≦ 0.20 mm /year, and nearly half of the participants (42%) have an annual axial elongation within 0.1 mm (Fig. 2b). In the SVL group, the annual axial increase was greater than 0.1 mm, and most of the participants (65%) had axial increase ≧ 0.30 mm /year(Fig. 2c). It can be seen that MF-RGPCL can significantly control the axial progression of myopia patients, regardless of the average annual axial elongation or the distribution range of the axial elongation.
Changes in AL in one year of MF-RGPCL and SVL groups. (a) Comparison of AL changes between MF-RGPCL and SVL groups in one year, ****P < 0.0001; (b) Distribution of the annual range of AL growth in the MF-RGPCL group; (c) Distribution of the annual range of AL growth in the SVL group; (d) Comparison of the AL growth at each follow-up compared with the baseline AL, ***P < 0.001, ****P < 0.0001; (e) Comparison of AL at each follow-up compared with the previous one, 3mo-BL vs. 6mo-3mo, t = 2.81, **P = 0.005.
In addition, we also analyzed the changes in AL at each follow-up visit in the MF-RGPCL group, and the average increase in AL from the baseline at the initial examination to the 3rd, 6th, 9th, and 12th months was 0.060 (± 0.084) mm, 0.089 (± 0.118) mm, 0.0132 (± 0.124) mm, and 0.179 (± 0.144) mm, respectively. The results of the One-Way-ANOVA showed there were significant differences between groups in all pairwise comparisons (Fig. 2d, all P < 0.001). At the same time, we compared the AL at each follow-up visit with the previous one, and found that the AL increased the most at the 3rd month, the first follow-up, at 0.060 (± 0.084) mm; the difference in AL between the first and second follow-ups (i.e., the 6th month) was the smallest, at 0.029 (± 0.063) mm; the AL changes at the 3rd and 4th follow-ups (i.e., the 9th and 12th months) were similar. The One-Way-ANOVA results showed that only the first and second follow-up AL differences had a significant difference (Fig. 2e, P = 0.005).
Changes in BCVA in one year
Both groups of participants had non-normal distribution of BCVA at each follow-up visit, as shown in Fig. 3a; Table 2. After non-parametric test, there was no difference in the baseline BCVA between the SVL group and the MF-RGPCL group (P = 0.18). Following a 12-month period of wearing the lenses, the BCVA of the SVL group was significantly lower than that of the SVL-12mo group (P < 0.0001), while the BCVA of the MF-RGPCL group remained at a good level (MF-RGPCL-12mo vs. MF-RGPCL-BL, P = 0.93). At the same time, the BCVA of the MF-RGPCL group was significantly better than that of the SVL group at one year of wearing (MF-RGPCL-12mo vs. SVL-12mo, P = 0.003). This is because the SVL group absence of myopia control interventions resulting in rapid progression of AL and refractive power. In addition, the BCVA of the MF-RGPCL group at the 3rd, 6th, 9th, and 12th month follow-up visits was also recorded in detail, and no significant difference was found between each visit (all P > 0.05, Fig. 3b). It can be seen that MF-RGPCL not only has good visual correction effect, but also has stable visual maintenance ability.
The decentration of MF-RGPCL
In accordance with the classification of decentration range proposed by Tsai and Lin30, the distance is defined as follows: 0.5 mm or less is classified as mild decentration, 0.5 mm to 1.0 mm is classified as moderate decentration, and 1.0 mm or greater is classified as severe decentration. In the following statistics, any decentration that affects the visual quality or exceeds the patient’s tolerance would be reassessed and the parameters adjusted, until the best fit is achieved. As illustrated in Fig. 4a, the summary of the deviated position with review records reveals that the majority of cases (79%) exhibit mild decentration, while moderate decentration accounts for approximately 16% and severe decentration accounts for the least, only 5% (Fig. 4b). Furthermore, the decentration direction is subdivided into four categories: nasal inferior, nasal superior, temporal inferior, and temporal superior. The majority of decentration cases (40.3%) are classified as temporal inferior deviations, with temporal superior deviations accounting for 26% of cases. The proportion of cases without decentration was 14.6%. The least common types of decentration are nasal inferior and nasal superior, which account for 4.4% and 6.5% of cases, respectively. Furthermore, 8.2% of the deviations are categorised as other directional deviations (Fig. 4c). The aforementioned results indicate that the most prevalent types of decentration for MF-RGPCL are mild decentration distance and temporal inferior deviation.
Multiple regression modeling to analyze the factors affecting AL growth in MF-RGPCL group
Following a year of monitoring the AL changes in the experimental group, a multiple regression model was constructed with the annual change in AL as the dependent variable and other potential factors influencing AL development as independent variables. The adjusted R² was 0.80, indicating that the predictive independent variables could explain 80% of the AL growth. The Durbin-Watson statistic yielded a value of 2.10, indicating that the samples in this model exhibited satisfactory independence between them. The normal distribution of the standardized residuals indicated that the residuals were random and not the result of any artificial influences. Once a reliable regression model had been obtained, the results of the multivariate analysis were presented in Table 3. It was found that the AL growth of the MF-RGPCL group subjects was significantly correlated with older age (Beta = 0.191, P = 0. 025) The results indicated that there was a significant correlation between the onset age of myopia and the AL growth of the subjects (Beta=-0.258, P = 0.010). Additionally, parental myopia (Beta = 0.489, P < 0.0001), decentration distance (Beta=-0.182, P = 0.018), pupil diameter (Beta=-0.233, P = 0.013), and corneal curvature (Beta=-0.269, P = 0.002) were identified as significant predictors. No significant correlation was observed with the remaining factors in the table (all P > 0.05). It is worth mentioning that the correlation analysis was also conducted, and to be consistent with those of the multivariate regression analysis(Supplementary Fig. 1 and Supplementary Table 1).This indicates that the factors affecting the AL changes of the experimental group subjects are multifaceted, suggesting that the MF-RGPCL in this study have withstood numerous objective and subjective factors that affect AL growth. This further proves the effectiveness of the MF-RGPCL in preventing myopia.
Effect of MF-RGPCL on corneal endothelium
It is of paramount importance that any myopia prevention and control product is safe and effective. Consequently, we also examined the alterations in corneal endothelial cell-related variables following the use of glasses for a period of one year. In comparison to the baseline values recorded prior to the commencement of wearing glasses, no statistically significant alterations were observed in the proportion of HEX, CV, CCT, and CD following a one-year period of wearing glasses (Fig. 5a-d, all P > 0.05). This result objectively indicates that daily use of MF-RGPCL in the short to medium term will not have a significant structural impact on the cornea, which provides evidence of the safety of wearing MF-RGPCL.
Changes of corneal endothelial cells after wearing MF-RGPCL in one year. Figure (a–d) is a comparison results of the coefficient of variation, central corneal thickness, percentages of hexagonal corneal endothelial cells, and density of corneal endothelial cells before and one year after wearing MF-RGPCL, respectively.
Discussion
The findings of this study suggest that MF-RGPCL are predominantly utilised by patients with high myopia or significant astigmatism, whose ocular conditions exceed the indications for conventional corneal contact myopia prevention and control products. Additionally, these patients present with an earlier age of onset of myopia, elevated IOP in both eyes, and a clear family history of myopia, which further reinforces their characteristics of high myopia. The subjects’ eye conditions fully comply with the indications range of MF-RGPCL. To ensure the scientific rigour of the experiment, a control group was selected comprising SVL wearers with similar refractive and age characteristics to the MF-RGPCL group. Following a one-year period of wearing glasses, it was observed that MF-RGPCL were capable of significantly decelerate the axial elongation of the subjects. The experimental group exhibited an annual axial elongation of 0.18 mm, while the control group demonstrated an annual axial elongation of 0.33 mm. The wide range in axial elongation is potentially associated with multiple factors, including the age of myopia onset, the degree of parental myopia, pupil diameter, as well as individual visual habits and lifestyle-related factors.
The axial elongation progression in the MF-RGPCL group was reduced by 46%. Furthermore, the distribution range of annual axial elongation was analysed, and the results demonstrated that approximately half (42%) of the MF-RGPCL group exhibited an annual axial elongation of less than 0.1 mm, whereas 65% of the SVL group demonstrated an annual axial elongation of over 0.3 mm. In terms of vision correction, as the majority of participants in this study exhibited high myopia, the improvement of corrected vision is also a significant outcome. It was found that both wearing SVL and MF-RGPCL can achieve optimal corrected vision. However, Following a 12-month period of wearing glasses, the MF-RGPCL group exhibited significantly superior corrected vision compared to the SVL group. This is because the study cohort consisted of adolescents with active axial elongation and high baseline myopia, the SVL group demonstrated faster AL progression compared to the MF-RGPCL group after one year of SVL wear due to the absence of myopia control interventions.Regrettably, the records of refraction results were unavailable during data collection. However, the observed AL increase in the SVL group (0.33 ± 0.018 mm) suggests an estimated spherical equivalent refraction (SER) progression of approximately − 1.00 D, which would explain the clinically observed blurred VA. While VA changes were included as an endpoint to evaluate MF-RGPCL efficacy under the assumption that SVL-related VA decline reflected SER progression, inadequate elaboration on this rationale introduced ambiguity. This not only demonstrates the effective visual maintenance capacity of MF-RGPCL, but also substantiates the efficacy of myopia control. In terms of the effect of AL, the findings of our research indicate that the mean myopia control effic acy of MF-RGPCL is comparable to that of OK lenses31,32,33 and, to a certain extent, superior to that of MF-SCL34,35. However, as this is a retrospective analysis of real-world research (RWR), it is not possible to rigorously control for the influence of various confounding factors in the same way as in a randomised controlled trial (RCT)36. In the context of RWR, the lifestyle and glasses (or lenses)-wearing habits of the subjects are more closely related to their actual condition, and the experimental results have greater practical relevance for clinical application37. In this study, patients in the MF-RGPCL group underwent a comprehensive eye examination and were screened for eligibility for myopia prevention and control measures. This approach is similar to having strict inclusion and exclusion criteria. In addition, follow-up cards are distributed to each individual wearing MF-RGPCL and staff are instructed to provide regular reminders for follow-up examinations. Similarly, the characteristics of the MF-RGPCL group were used as the criterion for selecting SVL wearers as the control group to minimise between-group bias due to differences in baseline values or ocular conditions. However, the follow-up period for patients in the SVL group is not strictly defined, resulting in the SVL group having only a 12-month follow-up record for calculating changes in AL and BCVA. In conclusion, this study controlled for certain confounding factors based on the actual daily life situation of the wearer and suggests that MF-RGPCL may indeed be effective in slowing the rate of axial elongation in adolescents.
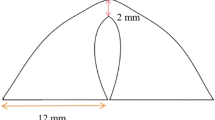
In general, the human eye is in a constant state of development until adulthood, especially 15 years of age, and the younger the age, the faster the axial elongation of the eye, and as the age increases, the development of the eyeball will gradually stabilize38,39,40,41. However, during the normal physiological development of the human eye, it can be affected by many unpredictable factors, such as congenital genetic factors and acquired environmental factors, which lead to the premature and rapid development of the eye, the premature depletion of the hyperopic reserve, and the onset and rapid progression of myopia. In order to combat the attack of such factors, the application of myopia prevention and control products is urgent. Therefore, the final myopia control effect of a product depends on the game between ‘attack’ and ‘prevention’. In this study, MF-RGPCL had a relative AL reduction of 0.15 mm and an absolute AL control of 46%. Because there is a lack of other reports on the effect of MF-RGPCL on myopia control in adolescents, in addition to analysing the AL development, we also performed multiple regression and correlation analyses of various other factors that may affect the efficacy of MF-RGPCL. Most notably, we generalised the decentration in the fitting assessment of MF-RGPCL and found that, consistent with OK lens: (1) the decentration in the fitting of MF-RGPCL were mostly infratemporal, and were predominantly moderate (decentration distances of 0.5 mm to 1.0 mm)42; and (2) the greater the decentration distances were, the more pronounced was the AL retardation42. The defocus design of MF-RGPCL is located on the anterior surface of the lens. The central 2 mm zone is devoid of defocus distribution, thereby correcting refractive errors and ensuring clear central vision. The mid-peripheral 2 mm to 6 mm zone constitutes a progressive defocus zone, capable of forming a myopic defocus with a continuous distribution of the pupil-entry zone. Beyond the diameter of 6 mm, a multitude of stable defocus zones can be observed, collectively termed the ‘bulls-eye zone’. This zone is analogous to the reverse curve observed in OK lenses. It can therefore be surmised that when MF-RGPCL are decentration, the progressive zone with a considerable amount of defocus, or the ‘bull’s-eye ring zone’ with an even larger amount of defocus, enters the pupil. Myopic defocus theory suggests that more peripheral myopic defocus produces a more pronounced myopia control efficacy43,44. On the other hand, an increasing number of studies have demonstrated that the use of OK lenses is associated with an increase in higher-order aberrations, and the greater the higher-order aberrations, the slower the AL growth45,46,47. Similarly, when MF-RGPCL are decentration, an increased defocus area within the pupil may result in a greater induction of higher-order aberrations, thereby enhancing the myopia control efficacy. Consequently, the present study revealed a significant negative correlation between the decentration distance of MF-RGPCL and AL growth. In addition, we also found that the age of myopia onset, parental myopia, corneal curvature and pupil diameter were significant factors influencing the development of the AL. This is basically consistent with the factors that influence OK lense on AL reduction10,11. A number of studies have investigated the effect of pupil diameter on the retardation axial elongation of the OK lenses47,48,49, In this study, when the optic zone diameter of MF-RGPCL is unchanged, the larger the pupil diameter, the more the treatment area and the peripheral positive defocusing ring can enter the pupil, resulting in a larger relative myopic peripheral defocusing area of the retina, thus slowing down the growth of the AL48. The reverse is also true. The mean AL of the group included in this paper was 26.55 mm and the diopter was − 8.59 DS. It has been shown that there is a correlation between the AL and the corneal curvature in high myopic populations50, with the longer of AL, the steeper of the corneal curvature. Following correlation analyses at various levels, it was determined that the AL progression of the MF-RGPCL group was significantly associated with their individual ocular characteristics, the genetic predisposition to myopia in the subjects, and the lenses’ fitting. It should be noted that the analysis did not include the other important factors affecting the myopia control effect of MF-RGPCL, such as the nearwork time and outdoor activities. This was mainly due to the following reasons: (1) The average age of the subjects in the present study was 12–13 years old, and they were already junior high school students, with higher academic pressure and a heavier burden of nearwork time in general; (2) The observation phase of the experiment coincided with the time of stricter control by the COVID-19, with more online teaching, and outdoor activities were restricted to a certain extent. In conclusion, the factors affecting myopia are multi-level and multi-angle. Therefore, when analysing the efficacy of any myopia prevention and control product, it is essential to consider the overall situation of the patients in order to ensure that the experimental results are true and reliable.
This study provides preliminary confirmation of the efficacy of MF-RGPCL in controlling myopia progression and focuses on their safety as an additional key evaluation index. All patients with contact lenses in our hospital will undergo comprehensive ocular surface health and lens cleaning examinations during regular follow-up visits. Additionally, hygienic habits will be instructed to address safety concerns due to adherence at the source, thereby addressing the issue at the earliest possible stage. The corneal endothelium plays a pivotal role in maintaining the corneal transparency, moisture content stability, and normal thickness of the cornea. Consequently, corneal endothelial health is frequently employed as a crucial indicator for evaluating corneal safety. General RGP has a long history of clinical use, and its safety has been the subject of continuous investigation. A related study demonstrated that following a six-month period of RGP wear, there was a notable decline in corneal epithelial cell density, whereas corneal endothelial cell density remained relatively stable51 Another study demonstrated that wearing RGP lenses for 30 consecutive days did not result in any notable alterations to corneal endothelial cell morphology52 Additionally, a series of long-term cross-sectional studies revealed that the CV and the HEX exhibited a correlation with the duration of RGP wear. However, the CCT and the CD did not undergo any significant changes53. The aforementioned studies indicate that short-term RGP wear does not negatively impact the corneal endothelium. However, long-term wear may potentially influence CV and HEX to a certain degree. In the present study, the use of MF-RGPCL (PROTONG of iBright, DK 125) as an intervention was observed over a one-year period. No significant changes were noted in the corneal endothelial HEX, CV, CCT or CD. Concerning safety evaluation, we agree that corneal endothelial parameters alone cannot comprehensively assess ocular safety. However, as a retrospective study, our analysis was inherently limited to systematically documented metrics, with endothelial count being the only standardized parameters available in the institutional database. To mitigate this limitation, we conducted a thorough review of all participants’ medical records, which included detailed documentation of slit-lamp examinations, subjective complaints and lens hygiene assessments at each follow-up visit. These qualitative records were integral to our safety evaluation framework. All MF-RGPCL wearers in our institution undergo standardized protocols during follow-up visits, including slit-lamp evaluations of ocular surface integrity, lens deposition analysis, and patient-reported symptom assessments. Additionally, strict hygiene education is reinforced to minimize compliance-related risks. Our thorough review of medical records revealed no clinically significant ocular surface complications except transient foreign body sensation during the initial adaptation period (resolving within one week in all cases). Furthermore, the maintained BCVA throughout the study period further supports the relative safety profile of MF-RGPCL wear.“. The aforementioned evidence indicates that the use of MF-RGPCL for a period of one year does not present a threat to the wearer’s ocular surface health. Nevertheless, further observation is required to ascertain the long-term safety of lens wear.
In summary, the present study demonstrated that MF-RGPCL have good efficacy in myopia control and a greater safety profile, based on the most rigorous efforts to control confounding factors. Compared with OK lenses, MF-RGPCL can be worn during the daytime and the oxygen permeability of the material is higher, which is safer for the cornea. The oxygen permeability of MF-RGPCL is also higher than that of soft contact lenses. Hydrogel soft lenses have poor mobility, poor tear circulation, easy to form deposits, and are not as safe as MF-RGPCL. In addition to the fact that the price of MF-SCL is more expensive, MF-RGPCL is a more ideal choice for many ordinary families. But For the myopic group with low to medium refractive error, MF-RGPCL is not the only choice. Compared with OK lenses, MF-RGPCL will have disadvantages such as lens detachment, loss, and stronger foreign body sensation when worn during daytime. Compared with MF-SCL, MF-RGPCL has the disadvantages of strong foreign body sensation, easier detachment and fragmentation with small diameter. In addition to the inherent limitations of the lenses themselves, the design of this study merits discussion. As this study was retrospective in nature, it was not feasible to comprehensively document the participants’ ocular parameters, including refractive error at follow-up. Consequently, when assessing the myopia control efficacy of MF-RGPCL, we solely employed the AL as a reference point, which could potentially introduce a degree of evaluation index bias. Furthermore, all the baseline assessments of the participants in this study were conducted on the day of the procedure, during which a waiting period of approximately one month was observed. During this interval, the subjects did not engage in any additional myopia prevention or control measures. It should be noted that the AL found at the third-month follow-up were, in fact, four months after the initial examination. Furthermore, a comparison of the AL of each follow-up visit with the previous one revealed that the fastest growth of the AL was 0.060 mm in the third month, with the smallest AL difference between the sixth and the third month being 0.029 mm. The difference between the ninth month and the sixth month was 0.043 mm, while the difference between the twelfth month and the ninth month was 0.047 mm. Notably, the change of AL of the first two follow-up visits was the only one that exhibited a statistically significant difference. It is possible that this discrepancy could have been avoided if the AL on the first day of lens wear is used as a reference. Furthermore, it can be observed that with the prolongation of wearing time, the AL control effect of MF-RGPCL gradually tends to stabilise. However, the long-lasting efficacy requires further observation. Furthermore, given that the AL of MF-RGPCL wearers in this study was 26.55 mm and the diopter was − 8.59 DS, if the study participants were randomly selected as the control group among patients wearing SVL as in a general retrospective study, it would be challenging to select individuals whose myopia degree can match that of the MF-RGPCL group. This is because children with severe myopia will choose myopia prevention and control lenses. On the other hand, if the diopter of the randomly selected SVL group deviates significantly from that of the MF-RGPCL group, the scientific comparison may be compromised, as the axial elongation of children with high myopia and those with moderate and low myopia differs considerably, resulting in additional variables influencing the observed measures beyond the intervention. Therefore, when selecting the control group, we deliberately chose individuals with AL and diopter similar to those of the observation group. However, due to the need for myopia prevention in children with high myopia, the number of SVL wearers who fulfilled the inclusion criteria was obviously sparse, and this, together with the seriousness of the missed visits, greatly affected the size of the sample of the control group.Therefore, to increase the sample size, we had to include both eyes in the statistics.
In light of these unavoidable shortcomings, we have initiated a new randomised controlled trial to investigate the long-term efficacy of MF-RGPCL in controlling myopia in adolescents. The trial will observe and evaluate the effects of these lenses on several key parameters, including AL, refractive error, and choroidal thickness, over a period of at least three years. Although the AL is recognized as one of the criteria that can reflect the progression of myopia, due to the difference in corneal curvature between individuals, the AL and diopter are not necessarily one-to-one corresponding. Therefore, the inclusion of diopter in the evaluation index can more comprehensively analyze the myopia control effect of MF-RGPCL. Another closely related to the length of the AL is the peripheral retinal refraction, the inclusion of choroid thickness is necessary and important, beacuse choroid thickness may be predictive biomarkers of long-term changes in the AL54,55,56,57. The study also assessed BCVA, visual function, BCVA is the basic requirement of any refractive error correction lens, and the visual function is to ensure comfortable and lasting vision on the basis of clear vision. Therefore in order to evaluate the safety and efficacy comprehensively of myopia control with MF-RGPCL with a more extensive data collection and a broader range of evaluation criteria. It is anticipated that the results will be available in a more complete form in the near future.
Methods
This study is a retrospective study in the real world, which complies with the principles of the Declaration of Helsinki, informed consent was obtained from all participants and/or their legal guardians. All research was performed in accordance with relevant guidelines/regulations and has been approved by the Ethics Committee of Shanxi Aier Eye Hospital (Approval number: EYESX-20220303-02).
Study subjects
The data set comprises myopic adolescents and children who wore MF-RGPCL (PROTONG of iBright, DK 125, Defocus design, Beijing, China. The optical and defocus design are illustrated in Fig. 6) from January 2020 to December 2021 at Aier Eye Hospital in Shanxi and Taiyuan. Inclusion criteria: (1) aged between 6 and 18 years old; (2) spherical equivalent (SE) range after cycloplegia: -1.00 D to -20.00 DS, astigmatism ≦ |-4.00 | DC; (3) corneal curvature (Kf): 39.00 D to 46.00 D; (4) best-corrected visual acuity (BCVA) ≦ 0.22 logMAR (Snellen 0.6 or 12/20); (5) no concurrent use of other myopia control products. Exclusion criteria: (1) poor compliance and failure to follow up regularly; (2) discontinuation of wear for more than one week consecutively during follow-up; (3) those with ocular or systemic diseases that do not meet the indications for rigid gas permeable contact lenses. At the same time, single-vision spectacle (SVL) wearers with similar diopter and axial characteristics as the subjects in the MF-RGPCL group were screened as a control group, and the rest of the criteria including inclusion and exclusion for the control group were the same as those for the experimental group.
Clinical pathway
The initial (pre-wearing) examination items for two groups of subjects include: AL, cycloplegic refraction distance and near eye position, uncorrected VA, BCVA, positive/negative relative adjustment (PRA/NRA), accommodative response (BCC method), intraocular pressure (IOP), body mass index (BMI). In addition, the MF-RGPCL group also measures corneal topography, tear break-up time (BUT), corneal central thickness(CCT), corneal endothelial cell density(CD), coefficient of variation (CV), and the percentage of hexagonal shape cells (HEX) The MF-RGPCL group was followed up at 3, 6, 9, and 12 months after wearing lenses, and the AL, BCVA, and corneal topography were checked at each follow-up, CCT/CD/CV/HEX were only recorded at the 12 month follow-up. The SVL group only had AL and BCVA reviewed in the 12th month. Follow up time and examination items are shown in Fig. 7.
Data source
MF-RGPCL group: A total of 165 patients who wore MF-RGPCL from January 2020 to December 2021 were screened by the rigid corneal contact lens sharing system in Shanxi and Taiyuan Aier Eye Hospitals. All the wearers established a case file of rigid corneal contact lenses, and the examination data were kept in both electronic and paper versions. Following a review of the cases, 23 cases were excluded due to the use of combined atropine therapy or other means of myopia control, a history of discontinuation of wear for greater than one week, failure to attend at least one follow-up during the observation period, or the presence of large strabismus, which affects fusion function. This resulted in 48 subjects (96 eyes) meeting the enrolment criteria (see Fig. 8).
SVL group: After preliminary screening, it was found that most of the individuals wearing MF-RGPCL were highly myopic. In order to maintain consistency between the baseline values of the two groups as much as possible, stricter requirements were placed on the refractive range when selecting subjects with SVL. After screening, within the observation time range of this study, a total of 124 SVL wearers who met the conditions for equivalent spherical lens and AL recorded by optometrists from both hospitals were included. Among them, 42 were replaced with defocus lenses (including orthokeratology lenses, peripheral myopic defocus design spectacle lenses, and others) less than one year after wearing single vision spectacle lenses, and 61 were not found to have any follow-up records. Finally, a total of 21 SVL subjects (42 eyes) were included in the study.
Measurement of ocular parameters and characteristics
All objective examinations involved in this study were performed in the multi-functional examination rooms of the Department of Optometry at the Shanxi Aier Eye Hospital and Taiyuan Aier Eye Hospital, and a dedicated person was responsible for all examinations. Objective examinations included: autorefraction, (TOPCON, KR-800, JAP); intraocular pressure, non-contact tonometer (NIDEK, NT-510, JAP); AL, ophthalmic optic correlation biometry (TOMEY, OPTICAL BIOMETEROA-2000, JAP); corneal thickness and corneal endothelium, corneal endothelial cell microscope (TOMEY, EM-400, JAP); corneal topography, corneal topographer (TOMRY, TMS-5, JAP) For the above objective examinations, the eyes were asked to be opened as wide as possible while ensuring that the patient was in the correct position, and the final result was the average of the three measurements or optimal result (topography). Subjective examinations included: visual acuity, standard logarithmic visual acuity chart (GB11533-2011); evaluation of the anterior eye segment and fit assessment of MF-RGPCL, digital slit lamp (Topcon, AJ6000823, JAP); preliminary examination of the eye position, corneal reflectance and masking test; subjective refraction, NRA, PRA, BCC, distance and near eye positions (Von Graefe method), comprehensive optometry (TOPCON, CV-5000, JAP). Subjective refraction followed MPMVA principles. All of the above examinations were performed under an illumination intensity of about 350 lx.
Measurement of the treatment zone decentration for corneal topography
The axial power corneal topography of the naked eye was measured before fitting the MF-RGPCL (Fig. 9a), and the instantaneous power corneal topography was measured after the fitting (Fig. 9b). The examiner and the environment were as described in “Measurement of ocular parameters and characteristics” above.The eccentricity distance of the MF-RGPCL was defined as the distance from the center of the pupil to the center of the treatment area 52, 53. The treatment area: In the TOMEY system, the mode was set to instantaneous, take the pupil centre as the reference, and the refractive error and curvature values were automatically displayed when the mouse was clicked at any point (Fig. 9b), and the range of corneal curvature that varied within 1.00 D and had fewer than two colour variations was selected54, which is the treatment area of the MF-RGPCL (Fig. 9c, blue circle). Open the downloaded topography in Adobe Illustrator CC 2019 and make the horizontal and vertical bisectors of the treatment area respectively, and the two line segments intersect at the point S at the centre of the treatment area (Fig. 9c, purple star). The distance between the pupil center point O (Fig. 9c, red point) and the point S is the eccentricity distance of MF-RGPCL. In TOMEY’s system, the parameters of the corneal topography can be set. Here, we only show the pupil diameter and coordinate axis, and each small box in the coordinate is 0.02 mm. Take the center O of the pupil as the origin, and the directions 0° and 90° as the X and Y axes, respectively. In Adobe Illustrator CC 2019, draw a line segment from the origin O to the center S of the treatment area, and the Angle α between OS and the X axis can be automatically displayed. The vertical line of the X-axis through the point S is at the point H, and OH can be read through the axes (Fig. 9c, red box in the upper right corner). Then OS = OH/ | cosα |. In this case, the angle is 135.6° and OH = 0.15 mm, then OS= | cos135.6° | /0.15 = 0.17 mm.
Evaluation and measurement of decentration of MF-RGPCL. (a) Axial power corneal topography; (b) Instantaneous power corneal topography; (c) The measurement of the treatment area, with blue circles indicating the size of the treatment area, purple stars indicating the center of the treatment area, and the red dot indicating the center of the pupil. OS is the eccentricity distance. The red box in the upper right corner of Figure c represents a partially enlarged image, and also indicates that SH is perpendicular to the X-axis and the angle between the OS and the X-axis.
Statistical analysis
All the data were entered into the Data editor system of IBM SPSS Statistics 26 for the normal distribution test. For the comparison between two groups of variables, if they were normally distributed, the independent samples t-test was used, and the result was expressed as mean±SD (standard deviation); if they were non-normally distributed, the non-parametric Wilcoxon rank test was used, and the result was expressed as the median (25% percentile, 75% percentile). For the comparison of ≧ 3 groups of variables, the homogeneity of variance test is first performed on the variables. If the variance was not homogeneous, but the variance ratio between the group with the highest variance and the group with the lowest variance is less than 3, the default analysis of variance results will not be affected. Therefore, this study only used One Way ANOVA (F-test) for the comparison of multiple groups of variables. In analysing the factors influencing the axial elongation in the MF-RGPCL group, in addition to multiple regression analysis, Pearson (between continuous numerical variables) and Spearman (between rank variables) correlation analyses were used. All statistical analyses of data involved above were used IBM SPSS Statistics 26 and statistical graphs were produced using GraphPad Prism. Auxiliary lines or labels in heatmaps and other plots were drawn using Adobe Illustrator CC 2019 or Adobe Photoshop CC 2015. In this study, the sample size (n) was 96 for all parameters pertaining to the eyes and 48 for parameters pertaining to individuals in the MF-RGPCL group. Similarly, the sample size (n) was 42 for all parameters pertaining to the eyes and 21 for parameters pertaining to individuals in the SVL group. In the expression of significant differences, * means P < 0.05, ** means P < 0.01, *** means P < 0.001, and **** means P < 0.0001.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Dandona, R. & Dandona, L. Refractive error blindness. Bull. World Health Organ. 79(3), 237–243 (2001).
Santodomingo-Rubido, J. et al. Long-term efficacy of orthokeratology contact Lens wear in controlling the progression of childhood Myopia. Curr. Eye Res. 42(5), 713–720 (2017).
Holden, B. A. et al. Global prevalence of myopia and high myopia and Temporal trends from 2000 through 2050. Ophthalmology 123(5), 1036–1042 (2016).
Morgan, I. G. et al. The epidemics of myopia: Aetiology and prevention. Prog Retin Eye Res. 62, 134–149 (2018).
Xu, L. et al. Design, methodology, and baseline of whole city-million scale children and adolescents myopia survey (CAMS) in Wenzhou, China. Eye Vis. (Lond). 8(1), 31 (2021).
Mutti, D. O. & Zadnik, K. The utility of three predictors of childhood myopia: A bayesian analysis. Vis. Res. 35(9), 1345–1352 (1995).
Quek, T. P. et al. Prevalence of refractive errors in teenage high school students in Singapore. Ophthalmic Physiol. Opt. 24(1), 47–55 (2004).
Rose, K. A. et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 115(8), 1279–1285 (2008).
Mutti, D. O. et al. Parental myopia, near work, school achievement, and children’s refractive error. Invest. Ophthalmol. Vis. Sci. 43(12), 3633–3640 (2002).
Cheng, H. C. et al. Risk factors and behaviours of schoolchildren with myopia in Taiwan. Int. J. Environ. Res. Public. Health 17(6) (2020).
Pärssinen, O. & Kauppinen, M. Risk factors for high myopia: A 22-year follow-up study from childhood to adulthood. Acta Ophthalmol. 97(5), 510–518 (2019).
Flitcroft, D. I. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog. Retin Eye Res. 31(6), 622–660 (2012).
Tsai, A. S. H. et al. Clinical characteristics, surgical outcomes, and prognostic Factors. Retina 39(9), 1751–1760 (2019).
Hu, Y. et al. Association of age at myopia onset with risk of high myopia in adulthood in a 12-year follow-up of a Chinese Cohort. JAMA Ophthalmol. 138(11), 1129–1134 (2020).
Wu, P. C. et al. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 120(5), 1080–1085 (2013).
Ha, A. et al. Efficacy and safety of 8 Atropine concentrations for myopia control in children: A network meta-analysis. Ophthalmology 129(3), 322–333 (2022).
Yam, J. C. et al. Low-Concentration Atropine for myopia progression (LAMP) study: A randomized, Double-Blinded, Placebo-Controlled trial of 0.05%, 0.025%, and 0.01% Atropine eye drops in myopia Control. Ophthalmology 126(1), 113–124 (2019).
Gong, Q. et al. Efficacy and adverse effects of Atropine in childhood myopia: A meta-analysis. JAMA Ophthalmol. 135(6), 624–630 (2017).
Hiraoka, T. et al. Safety and efficacy following 10-years of overnight orthokeratology for myopia control. Ophthalmic Physiol. Opt. 38(3), 281–289 (2018).
Yang, G. et al. The effect of orthokeratology Lens on the axial length of Globe in children with myopia in Asia. J. Coll. Physicians Surg. Pak. 32(11), 1459–1464 (2022).
Queirós, A. et al. Assessment of the clinical effectiveness of DRL orthokeratology lenses vs. Single-Vision spectacles in controlling the progression of myopia in children and teenagers: 2 year retrospective Study. (2023). Children (Basel), 10(2)
Garcia-Del Valle, A. M. et al. Efficacy and safety of a soft contact lens to control myopia progression. Clin. Exp. Optom. 104(1), 14–21 (2021).
Zhu, Q. et al. Retardation of myopia progression by multifocal soft contact Lenses. Int. J. Med. Sci. 16(2), 198–202 (2019).
Chamberlain, P. et al. A 3-year randomized clinical trial of misight lenses for myopia Control. Optom. Vis. Sci. 96(8), 556–567 (2019).
Lam, C. S. Y. et al. Defocus incorporated multiple segments (DIMS) spectacle lenses slow myopia progression: A 2-year randomised clinical trial. Br. J. Ophthalmol. 104(3), 363–368 (2020).
Fengchao, Z. et al. Effect of spectacle lenses with highly aspherical lenslets on binocular vision and accommodation in myopic children with and without intermittent exotropia. J. Ophthalmol. 2022, 9306848. (2022).
Bao, J. et al. Spectacle lenses with aspherical lenslets for myopia control vs Single-Vision spectacle lenses: A randomized clinical Trial. JAMA Ophthalmol. 140(5), 472–478 (2022).
Bao, J. et al. One-year myopia control efficacy of spectacle lenses with aspherical lenslets. Br. J. Ophthalmol. 106(8), 1171–1176 (2022).
Pauné, J. et al. Peripheral myopization and visual performance with experimental rigid gas permeable and soft contact lens design. Cont. Lens Anterior Eye 37(6), 455–460 (2014).
Tsai, Y. Y. & Lin, J. M. Ablation centration after active eye-tracker-assisted photorefractive keratectomy and laser in situ keratomileusis. J. Cataract Refract. Surg. 26(1), 28–34 (2000).
Gifford, K. L. et al. Stability of peripheral refraction changes in orthokeratology for myopia. Cont. Lens Anterior Eye 43(1), 44–53 (2020).
Guo, B. et al. Manual and software-based measurements of treatment zone parameters and characteristics in children with slow and fast axial elongation in orthokeratology. Ophthalmic Physiol. Opt. 42(4), 773–785 (2022).
Vincent, S. J. et al. CLEAR. - Orthokeratology Cont. Lens Anterior Eye 44(2), 240–269. (2021).
Ribeiro Reis, A. P., Palmowski-Wolfe, A. & Beuschel, R. Correction: Slowing down Myopia Progression with Contact Lenses - Everyday Cases from the Clinic (Klin Monbl Augenheilkd, 2023).
Huang, J. et al. Efficacy comparison of 16 interventions for myopia control in children: A network meta-analysis. Ophthalmology 123(4), 697–708 (2016).
Liu, J. et al. The efficacy of defocus incorporated multiple segments lenses in slowing myopia progression: Results from diverse clinical Circumstances. Ophthalmology 130(5), 542–550 (2023).
Grapow, M. T. et al. Randomized controlled trials do not reflect reality: real-world analyses are critical for treatment guidelines!. J. Thorac. Cardiovasc. Surg. 132(1), 5–7 (2006).
Donovan, L. et al. Myopia progression rates in urban children wearing single-vision spectacles. Optom. Vis. Sci. 89(1), 27–32 (2012).
Chua, S. Y. et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol. Opt. 36(4), 388–394 (2016).
Li, S. M. et al. Distribution of ocular biometry in 7- and 14-year-old Chinese children. Optom. Vis. Sci. 92(5), 566–572 (2015).
Chen, J. H. et al. Lens thickness and associated factors in Chinese children: The Shandong children eye Study. Acta Ophthalmol. 95(6), e521–e522 (2017).
Zhang, S. et al. Effect of treatment zone decentration on axial length growth after orthokeratology. Front. Neurosci. 16, 986364 (2022).
Koomson, N. Y. et al. Relationship between peripheral refraction, axial lengths and parental myopia of young adult myopes. J. Optom. 15(2), 122–128 (2022).
Zhong, Y. et al. Central and peripheral corneal power change in myopic orthokeratology and its relationship with 2-Year axial length change. Invest. Ophthalmol. Vis. Sci. 56(8), 4514–4519 (2015).
Lau, J. K. et al. Higher-Order aberrations and axial elongation in myopic children treated with Orthokeratology. Invest. Ophthalmol. Vis. Sci. 61(2), 22 (2020).
Huang, Y. et al. Comparison of peripheral refraction and higher-order aberrations between orthokeratology and multifocal soft contact lens designed with highly addition. Graefes Arch. Clin. Exp. Ophthalmol. 260(5), 1755–1762 (2022).
Nti, A. N. & Berntsen, D. A. Optical changes and visual performance with orthokeratology. Clin. Exp. Optom. 103(1), 44–54 (2020).
Pauné, J. et al. The role of back optic zone diameter in myopia control with orthokeratology Lenses. J. Clin. Med. 10(2) (2021).
González-Méijome, J. M. et al. Changes in peripheral refractive profile after orthokeratology for different degrees of Myopia. Curr. Eye Res. 41(2), 199–207 (2016).
Jin, G. et al. Corneal biometric features and their association with axial length in high Myopia. Am. J. Ophthalmol. 238, 45–51 (2022).
Alipour, F. et al. Effects of soft Toric, rigid Gas-Permeable, and Mini-Scleral lenses on corneal microstructure using confocal Microscopy. Eye Contact Lens 46(2), 74–81 (2020).
Barr, J. T. et al. Corneal endothelial morphology results in the Menicon Z 30-day continuous-wear contact lens clinical trial. Eye Contact Lens 29(1), 14–16 (2003).
Doughty, M. J. An observational cross-sectional study on the corneal endothelium of medium-term rigid gas permeable contact lens wearers. Cont. Lens Anterior Eye 40(2), 109–115 (2017).
Liu, Y. et al. The influence of the choroid on the onset and development of myopia: from perspectives of choroidal thickness and blood flow. Acta Ophthalmol. 99(7), 730–738 (2021).
Hanyuda, A. et al. Relationship of choroidal thickness and axial length with posterior vitreous detachment in patients with high myopia. Sci. Rep. 12(1), 4093 (2022).
Wang, Y. et al. Choroidal circulation in 8- to 30-Year-Old Chinese, measured by SS-OCT/OCTA: Relations to age, axial length, and choroidal Thickness. Invest. Ophthalmol. Vis. Sci. 64(7), 7 (2023).
Nickla, D. L. & Wallman, J. The multifunctional choroid. Prog Retin Eye Res. 29(2), 144–168 (2010).
Author information
Authors and Affiliations
Contributions
Ding Jia designed the study. Yanming Kang, Xiaobo Yu, Yali Hao, Qi Zhang, Weiwei Hao and Yuru Wang tracking and recording follow-up visits and collecting data. Lina Zhang analyzed and interpreted the data, drafted the manuscript, prepared figures. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study complies with the principles of the Declaration of Helsinki, informed consent was obtained from all participants and/or their legal guardians. All research was performed in accordance with relevant guidelines/regulations and has been approved by the Ethics Committee of Shanxi Aier Eye Hospital (Approval number: EYESX-20220303-02).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, L., Kang, Y., Yu, X. et al. Efficacy of multifocal rigid gas permeable contact lenses to control myopia progression. Sci Rep 15, 17261 (2025). https://doi.org/10.1038/s41598-025-01058-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01058-3