Abstract
C2 pars interarticularis length (C2PIL) required for pars screws has not been thoroughly studied in subjects with high-riding vertebral artery (HRVA). We aimed to measure C2PIL specifically on the sides with HRVA, define short pars, optimal pars screw length, and incorporate C2PIL into HRVA clusters using machine learning algorithms. A clinical anatomical study based on cervical CT was conducted with STROBE-compliant case–control design. HRVA was defined as accepted. Interobserver, intraobserver, and inter-software agreement coefficients for HRVA were adopted from our previous study. Sample size was estimated with pwr package and C2PIL was measured. Cut-off value and predictive statistics of C2PIL for HRVA were computed with cutpointr package. Unsupervised machine learning clustering was applied with all three pars parameters. 345 potential screw insertion sites (PSIS) were grouped as HRVA (143 PSIS in 110 subjects) or controls (202 PSIS in 101 subjects). 68% participants were females. The median C2PIL in HRVA group was 13.7 mm with interquartile range (IQR) of 1.7, whereas in controls it was 19.8 mm (IQR = 2.7). The optimal cut-off value of C2PIL discriminating HRVA was 16.06 mm with sensitivity of 96.5% and specificity of 99.3%. Therefore, clinically important short pars was defined as ≤ 16 mm rounding to the nearest screw length. Two clusters were created incorportating three parameters of pars interarticularis. In preoperative planning, the identified C2PIL cut-off of ≤ 16 mm may assist surgeons in early recognition of HRVA. The average screw lengths of 14 mm for bicortical and 12 mm for safer unicortical purchase in HRVA cases may serve as practical intraoperative reference points, particularly in situations requiring rapid decision-making or when navigation systems are unavailable. Moreover, C2PIL complements the classic HRVA parameters within the dichotomized clustering framework.
Similar content being viewed by others
Introduction
A high-riding vertebral artery (HRVA) is an anomalous course of vertebral artery exiting the C2 transverse foramen. It has been defined as a C2 isthmus height (C2IsH) of ≤ 5 mm and/or an internal height (C2InH) of C2 superior articular facet ≤ 2 mm measured 3 mm lateral to the border of the spinal canal1. The HRVA poses a risk of injuring the vessel during C2 instrumentation, especially with transpedicular or transarticular screws and its overall pooled prevalence is estimated at 25.3% (95% CI, 19.6% to 31.5%)2 but is notably more prevalent in rheumatoid arthritis3. The VA groove violation might follow 63% of fixation procedures with application of transarticular and 49% of transpedicular screws4. A safer alternative is a pars screw placed entirely within the pars interarticularis, especially in type 2 (internal) HRVA according to our recent HRVA classification5. This is due to the fact that pars screw is shorter and does not reach the C2 pedicle obviating the risk of the medial or lateral breach6. Importantly, it has been shown that bicortical short C2 pars screw provide adequate biomechanical pullout strength to promote fusion and are a viable option on the sides of HRVA. Despite its importance, C2 pars interarticularis length (C2PIL) required for pars screws has not been thoroughly studied in subjects with HRVA.
While preoperative analysis of the two cardinal parameters of HRVA (C2IsH and C2InH) provides valuable information whether transpedicular or transarticular screws should be discouraged in favor of other techniques5, it adds no value when ultimately settling for pars screws. For this purpose, pars length is the optimal parameter as it incorporates the trajectory of the pars screw.
In this study, we aimed to measure C2PIL specifically on the sides with HRVA, compare them with individuals without HRVA on either side, and define short C2 pars that could complement the established C2IsH and C2InH parameters in the clustering analysis. As a secondary goal, we wanted to determine which pars screw lengths would, on average, provide bicortical and unicortical purchases in case of HRVA.
Methodology
Study design
A clinical anatomical study based on cervical computed tomography (CT) scans was conducted with observational case–control design. Due to the applied pseudonymization and retrospective radiologic nature of the study, ethical approval was waived by the local Bioethics Committee (KB-0012/24/04/2020/Z). The authors confirm that all methods were performed in accordance with the Declaration of Helsinki. Study and manuscript preparation were conducted in accordance with STROBE statement (see Supplementary Material 1).
Sample size estimation
Pwr package in RStudio was used for the sample size calculation with “pwr.t.test” function. Based on the background information from our previous studies2,5,7, the effect size was set at 0.225. With the common probability of type I error at 5% (α = 0.05) and type II error at 20% (β = 0.2) with theoretical power of the study set at usual 80%, no dropout rate due to retrospective radiologic design, and plus 10% accounting for non-parametric testing, we estimated a minimum total sample size at 311.04 + 31.10 = 342.14 (rounded up to 343) potential screw insertion sites (PSIS) for significance of the two-sample non-parametric testing.
Eligibility
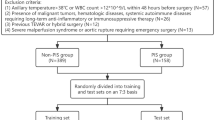
Inclusion criteria were as follows: (1) adults, (2) CT scan of the cervical spine with adequate visualization of the atlas and axis, and (3) correct reformatting of the scans into the sagittal section. On the other hand, patients were excluded from the study in case of (1) instrumentation of the upper cervical spine, (2) any fracture of the C2 vertebra, (3) age less than 18 years, (4) inadequate quality of the study due to excessive motion or other technical issues, and (5) diagnosed rheumatoid arthritis. Cases were subjects with unilateral or bilateral HRVA. Controls were defined as patients with both non-HRVA sides.
Software and measurements
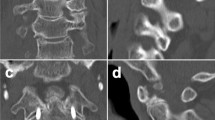
Somatom Sensation 64 (Siemens Healthineers, Erlangen, Germany) was used to acquire CT scans. The standard imaging protocol included a tube voltage of 120 kVp with automatic tube current modulation. Axial images were reconstructed using a slice thickness of 0.6 mm, applying a high-resolution bone kernel (B60f.). The matrix size was 512 × 512, and the field of view was adapted individually to cover the cervical spine. Scans were performed with the patient in the supine position, head-first, with the scan range extending from the base of the skull to the upper thoracic spine. HRVA was defined as uniformly accepted: C2 isthmus height (C2IsH) of ≤ 5 mm and/or C2 internal height (C2InH) of ≤ 2 mm measured 3 mm lateral to the lateral border of the spinal canal1,2,7. Measurements of pars length were taken using the method described by Kothari et al.8—see Fig. 1. We used Horos—an open-source code software distributed under the LGPL license at Horosproject.org and sponsored by Nimble Co LLC d/b/a Purview (Annapolis, MD, USA). The measurements took place from October till December 2024. As calculated by us in our previous study7, the interobserver, intraobserver, and intersoftware coefficients for HRVA measurements are all either good or excellent, therefore a second observer was not invited to replicate the results this time.
(A) The schematic presentation of C2 parameters measured in the study: *internal height, **isthmus height, ***pars interarticularis length. VA—vertebral artery. (B) The unaltered sagittal computed tomography (CT) slice showing the raw “in situ” anatomy. (C) the sagittal CT slice with the simulated pars screw trajectory, roughly paralleling C2/C3 zygapophyseal joint. Created with assistance of Biorender.com.
Biostatistics
Statistical analysis was performed by means of RStudio. The level of significance for the P value of the comparative tests was arbitrarily set to < 5% (P < 0.05). To check for normality, the Anderson–Darling test was used. The Fisher’s exact test was applied for comparison of categorical variables, whereas for continuous variables of non-normal distribution the Wilcoxon–Mann–Whitney test was used. To determine a definition of short pars length, cutpointr package was employed utilizing Youden’s J statistic and maximizing the balance between sensitivity and specificity. Other packages in use were pwr, ggplot2, ggstatsplot, nortest, dplyr, ggpubr, factoextra, data.table, writexl, scatterplot3d. Unsupervised machine learning K-means clustering was applied with all three pars parameters: C2 isthmus height, C2 internal height, C2 pars interarticularis length.
Results
Subject characteristics
211 subjects met eligibility criteria. There were 144 females (68%) and 67 males (32%). The median age of the entire cohort was 50 years with an interquartile range (IQR) of 30. 110 patients (52%) had at least one HRVA with a total of 143 sides with HRVA (77 had unilateral, 33 had bilateral HRVA). Sides with normal pars in the subjects with unilateral HRVA were not included in the analysis. There were also 101 controls with 202 PSIS appreciated as bilaterally normal pars interarticularis. In total, 345 potential screw insertions sites were analyzed meeting the estimated sample size. See Table 1 for detailed participant characteristics.
Measurements
In HRVA group, the mean C2IsH was 4.2 mm (IQR = 1.5), whereas in controls it was 7.8 mm (IQR = 2.5). C2InH was 3.5 mm (IQR = 1.7) and 7.2 mm (IQR = 2.8) for HRVA and controls, respectively. C2PIL was 13.7 mm (IQR = 1.7) and 19.8 mm (IQR = 2.7) for HRVA and controls, respectively. For detailed measurements including sides (left or right), see Table 2. The results of Mann–Whitney tests are presented as box plots in Fig. 2.
Boxplots illustrating the results of Mann–Whitney tests between sides with high-riding vertebral artery (light blue) and controls (light peach) for (A) internal height, (B) pars interarticularis length, and (C) isthmus height. HRVA – high-riding vertebral artery. All tests were statistically significant (p value < 0.05). Created in RStudio.
Defining short C2 pars interarticularis
The cut-off of 16.06 mm was calculated to provide the optimal discriminatory power with sensitivity of 96.5% and specificity of 99.3% for HRVA, with overall accuracy of 97.7% (see Supplementary Material 2). Therefore, rounding to the nearest size of pars screws, we defined a short C2 pars as ≤ 16 mm. The cut-off point was visualized on the ROC curve with AUC = 0.993 (see Figs. 3).
(A) A histogram showing distributions of C2 pars interarticularis length in subjects with (light blue) and without (light peach) high-riding vertebral artery (HRVA). The black dashed line indicates an optimal cut-off point of 16.06 mm above which the HRVA is unlikely. (B) A receiver operating characteristic (ROC) curve evaluating the discriminative performance of the C2 pars length measurement for HRVA detection. The selected cut-off of 16.06 mm achieves sensitivity and specificity of 96.5% and 99.3%, respectively. Created in RStudio.
Clustering
Machine-learning unsupervised K-means clustering revealed two clusters with selection of all three features of C2 pars interarticularis: pars length, isthmus height, and internal height. Cluster 1 was characterized by universely larger dimensions of all three parameters, whereas cluster 2 with small dimensions, in accordance with manual HRVA measurements (see Fig. 4). Detailed clustering statistics are presented as Supplementary Material 3.
(A) A two-dimensional plot visualizing the results of the K-means clustering analysis capturing 81.6% (Dim1) and 12% (Dim2) of the variance. Two distinct clusters have been identified: cluster 1 (red circular points) and cluster 2 (teal triangular points). Convex hulls outline the distribution of each cluster in the dimensional‐reduction space. (B) A three‐dimensional plot illustrating the separation of the two clusters within the original measurement space of pars length, isthmus height, and internal height. Created in RStudio.
Discussion
Pars screw insertion is considered a salvage technique in case of HRVA, especially in type 2 (internal) HRVA when C2InH is critically reduced precluding safe transpedicular, subfacetal, or transarticular techniques5. If fixation with a pars screw is chosen, special attention should be paid to pars length as this parameter incorporates the trajectory. Hereby, we have provided the first measurements of C2PIL in European subjects of Caucasian ethnicity. On average, 14 mm screws would provide bicortical purchase, whereas shorter 12 mm screws would grant a safer unicortical grip. To date, only Kothari et al.8 have conducted a similar study amongst the South Asian population. In their study, subjects with concomitant HRVA and ponticulus posticus had pars length of 13.69 mm with standard deviation (SD) of 2.13 mm, which is very similar to our results. Their control group had C2PIL of 20.65 mm (SD = 2.79), slightly larger when compared to C2PIL in our study (median = 19.8, IQR = 2.7), which might stem from the known ethnic differences in C22,9.
Short C2 pars
Furthermore, our study indicates that C2PIL of 16.06 mm serves as an optimal statistical cutoff for predicting the presence of HRVA with a notable sensitivity of 96.5% and specificity of 99.3%. The nearest screw size is 16 mm, which allows for translation into clinical practice during surgical planning, as shorter pars length suggests a higher risk of encountering HRVA. In daily practice, a cut-point of 16 mm provides a robust and useful guideline—neurosurgeons and craniocervical orthopedics can quickly assess preoperative imaging and anticipate the need for modified trajectories such as medial window technique10, pars screw11, laminar screw12, subfacetal screw13, or to consider anterior submandibular retropharyngeal approach to C1-C2 joint14 when the measured pars is critically reduced. The strong diagnostic performance of this measurement underscores its potential role in enhancing patient safety and reducing vertebral artery injury, yet further multicenter validation studies would help confirm the generalizability and refine its utility in diverse patient populations. Importantly, our findings do not diminish the critical role of individualized preoperative assessment. As C2 morphology varies between patients, and even bilaterally within the same individual, precise evaluation of axial and sagittal CT images is essential for safely determining the pars screw trajectory and optimal screw length. The cut-off of 16 mm may serve as a valuable reference, but final surgical decisions should be based on patient-specific measurements obtained from high-resolution imaging in multiple planes. Surgeons are therefore strongly encouraged to incorporate multiplanar CT evaluation into routine preoperative planning for every case.
Clusters
Pars interarticularis is a three dimensional structure, which cannot be fully appreciated with a single measurement. Utilizing unsupervised machine-learning K-means clustering, we have identified two clusters based on a combination of C2 radioanatomical features including C2 pars interarticularis length, internal height, and isthmus height. This comprehensively highlights groups of patients with specific risk profiles that can be encountered during C2 instrumentation. Cluster 1 (larger dimensions) indicates adequate bone stock and anatomical space for classic transpedicular screw placement, which provides the highest pullout strength. On the other hand, if any of the three cardinal parameters falls within the cluster 2, the screw trajectory options are limited and the isthmus should be thoroughly regarding salvage techniques such as C2 pars or C2/C3 transfacetal screw11,15,16.
Limitations and generalizability
As for limitations, our data did not have normal distribution, therefore non-parametric tests were used for comparison of medians. Although there was a predominance of females within the HRVA group as compared to controls, this is concordant with the known higher prevalence of HRVA in women as indicated in our meta-analysis2. Another limitation is that subjects with HRVA were significantly older than controls. The classic HRVA parameters (C2IsH and C2InH) are characterized by high reproducibility and can be easily memorized with the “Hand as Foot” teaching method17, into which C2PIL can be incorporated. However, generalizability of the results is limited as only subjects of Caucasian ethnicty were included. Although our measurements were similar to South Asian population, validation in other ethnicities should be done.
Conclusions
We have presented a detailed radiological anatomy of C2PIL, which is significantly reduced on the sides with HRVA as compared to controls. Although screw selection should always be tailored to each patient’s anatomy, the clinical utility of our findings lies in offering a practical and quantifiable threshold to flag high-risk cases. The identified C2PIL cut-off of ≤ 16 mm may assist surgeons in early recognition of HRVA probability and facilitate preoperative risk stratification, especially in settings with limited image post-processing capabilities. Moreover, the average lengths of 14 mm (bicortical) and 12 mm (unicortical) screws in HRVA cases can serve as useful intraoperative benchmarks when a decision must be made rapidly, or when navigation is not available.
Data availability
The data that support the findings of this study are provided as Supplementary Materials. Additional data are available from the corresponding author, TK, upon reasonable request.
References
Neo, M. et al. Atlantoaxial transarticular screw fixation for a high-riding vertebral artery. Spine (Phila Pa 1976) 28, 666–670. https://doi.org/10.1097/01.BRS.0000051919.14927.57 (2003).
Klepinowski, T., Pala, B., Cembik, J. & Sagan, L. Prevalence of high-riding vertebral artery: A meta-analysis of the anatomical variant affecting choice of craniocervical fusion method and its outcome. World Neurosurg 143, e474–e481. https://doi.org/10.1016/j.wneu.2020.07.182 (2020).
Klepinowski, T., Cembik, J. & Sagan, L. Risk of the high-riding variant of vertebral arteries at C2 is increased over twofold in rheumatoid arthritis: a meta-analysis. Neurosurg Rev 44, 2041–2046. https://doi.org/10.1007/s10143-020-01425-w (2021).
Yeom, J. S. et al. Risk of vertebral artery injury: comparison between C1–C2 transarticular and C2 pedicle screws. Spine J 13, 775–785. https://doi.org/10.1016/j.spinee.2013.04.005 (2013).
Klepinowski, T. et al. Types of high-riding vertebral artery: a classification system for preoperative planning of C2 instrumentation based on 908 potential screw insertion sites. Spine J 25, 59–68. https://doi.org/10.1016/j.spinee.2024.08.021 (2025).
Singh, D. K. et al. C2 screw fixation techniques in atlantoaxial instability: A technical review. J Craniovertebr Junction Spine 13, 368–377. https://doi.org/10.4103/jcvjs.jcvjs_128_22 (2022).
Klepinowski, T. et al. Prevalence of high-riding vertebral arteries and narrow C2 pedicles among Central-European population: A computed tomography-based study. Neurosurg Rev 44, 3277–3282. https://doi.org/10.1007/s10143-021-01493-6 (2021).
Kothari MK, Dalvie SS, Gupta S, et al (2019) The C2 pedicle width, pars length, and laminar thickness in concurrent ipsilateral ponticulus posticus and high-riding vertebral artery: A radiological computed tomography scan-based study. Asian Spine J 13:290–295. https://doi.org/10.31616/asj.2018.0057
Chazono, M. et al. Ethnic differences in pedicle and bony spinal canal dimensions calculated from computed tomography of the cervical spine: a review of the English-language literature. Eur Spine J 21, 1451–1458. https://doi.org/10.1007/s00586-012-2295-y (2012).
Lee, D.-H. et al. The medial window technique as a salvage method to insert C2 pedicle screw in the case of a high-riding vertebral artery or narrow pedicle: A technical note and case series. Eur Spine J 31, 1251–1259. https://doi.org/10.1007/s00586-022-07146-6 (2022).
Buchmann, N. et al. C1–C2 posterior screw fixation in atlantoaxial fractures revisited: technical update based on 127 cases. Eur Spine J 29, 1036–1042. https://doi.org/10.1007/s00586-019-06244-2 (2020).
Ma, W. et al. Clinical application of C2 laminar screw technique. Eur Spine J 19, 1312–1317. https://doi.org/10.1007/s00586-010-1447-1 (2010).
Patkar, S. V. New entry point for C2 screw, in posterior C1–C2 fixation (Goel-Harm’s technique) significantly reducing the possibility of vertebral artery injury. Neurol Res 38, 93–97. https://doi.org/10.1080/01616412.2015.1105582 (2016).
Patkar, S. Anterior retropharyngeal cage distraction with atlantoaxial plate-screw fixation for basilar invagination with atlantoaxial dislocation. Neurosurg Focus Video 3, V11. https://doi.org/10.3171/2020.4.FocusVid.20157 (2020).
De Iure, F., Donthineni, R. & Boriani, S. Outcomes of C1 and C2 posterior screw fixation for upper cervical spine fusion. Eur Spine J 18(Suppl 1), 2–6. https://doi.org/10.1007/s00586-009-0981-1 (2009).
Rusconi, A. et al. Bicortical facet screws as a new option for posterior C2 fixation: anatomical study and clinical experience. Eur Spine J 26, 1082–1089. https://doi.org/10.1007/s00586-017-4997-7 (2017).
Klepinowski, T., Hanaya, J., Pettersson, S. D. & Sagan, L. The “Hand as Foot” teaching method in the high-riding vertebral artery. Asian J Surg https://doi.org/10.1016/j.asjsur.2024.07.073 (2024).
Acknowledgements
We sincerely thank the China National Cancer Center and the Migrant Population Service Center for the publicly accessible data of cancer registration and migration population in 2016. We greatly appreciate Epi Info, the R software, and its extensive open-source packages for data management and statistical modeling, as well as ChatGPT by OpenAI for partial grammar checking.
Funding
Open access funding provided by Pomeranian Medical University in Szczecin.
Author information
Authors and Affiliations
Contributions
T.K. and L.S. conceptualized the study design. T.K. and M.C. wrote the main manuscript text. L.S. revised the manuscript. B.P., N.Ż. prepared computed tomography reconstruction. N.Ż., M.C. and M.K. took the measurements. T.K. and D.T. did statistical analysis. T.K. prepared figures and tables. W.P. and L.S supervised the project. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
As this was a retrospective analysis of the studies that had been published in the past, no consent to participate was necessary.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Klepinowski, T., Kałachurska, M., Chylewski, M. et al. C2 pars interarticularis length on the side of high-riding vertebral artery with implications for pars screw insertion. Sci Rep 15, 18639 (2025). https://doi.org/10.1038/s41598-025-02174-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02174-w