Abstract
Dental checkups are integral to maintaining oral function in older adults and are a critical determinant of overall health and quality of life. However, their impact on oral function parameters remains understudied. This study investigated the association between dental checkup attendance and oral function in older adults. This cross-sectional study recruited a convenience sample of 235 older adults (75.1 ± 5.6 years, 125 males). Participants were categorized based on biannual dental checkup attendance. Seven oral parameters were assessed: oral cleanliness, oral dryness, occlusal support, oral motor function, tongue pressure, masticatory performance, and swallowing function. Statistical analyses included the Mann‒Whitney U test, chi-squared test, and linear regression analysis. Significant differences between attendees and non-attendees were found in sex, body mass index, and oral hygiene practices. Oral cleanliness (p = 0.005), masticatory performance (p < 0.001), and swallowing function (p = 0.001) were significantly better in checkup attendees. Non-attendance at dental checkups was consistently associated with the extent of declined oral function in crude (B:0.45; 95%CI:0.12,0.77) and fully adjusted models (B:0.56; 95%CI:0.16,0.97). Given the positive association between dental checkup non-adherence and declined oral function, encouraging community-based awareness campaigns with accessible dental care could promote checkup attendance. Consequently, it contributes to maintaining oral function in the older adult population.
Similar content being viewed by others
Introduction
Oral health is critical to general health, particularly in an aging society. Oral functions are particularly vulnerable to age-related changes, with significant implications for daily life and social interaction1. Aging, systemic, and oral diseases can significantly impact oral function, potentially leading to reduced nutritional intake and malnutrition2. Poor oral health with decreased function is reported to have detrimental effects on physical and general well-being, including mortality3. Age-related changes, such as reduced saliva production, muscle weakness, diminished taste, and increased disease risk, compromised oral function. It often occurs alongside other age-related health issues, necessitating a comprehensive healthcare approach.
Japan is experiencing rapid population aging. Roughly 40% of older adults exhibit some degree of oral hypofunction (OHF), characterized by reduced tongue pressure, difficulty speaking, and decreased masticatory efficiency4. Preventive health strategies, including government-funded dental checkups and home visits for older adults, have increased tooth retention in this population5. Japanese researchers have also developed protocols to check for oral health challenges. Even with advancements, many older Japanese adults struggle with functional challenges. After age 60, masticatory function declines by approximately 5% per decade6. According to a 2016 survey, 25% of Japanese people aged 75 and above report difficulty chewing hard foods, rising to nearly 40% in those over 857. A significant number of older adults experience swallowing difficulties: 13.8% of those living independently and 41.7% of those in nursing homes6. This contributes to a high rate of aspiration pneumonia, representing approximately 70% of pneumonia cases in Japanese nursing facilities8.
The timely implementation of early intervention is crucial to alleviate the progression of OHF to progress to oral dysfunction4. Despite the significance of early intervention, the uptake of preventive dental care services among older adults remains limited. It was previously reported that preventive dental care utilization was low (18.6%) and tends to decline with age9,10. This declined dental checkup attendance could often be due to financial constraints11, lack of motivation or encouragement, and various barriers to healthcare access that disproportionately affect older adult populations.
Dental checkups are important for the early detection and prevention of decline in oral function. They enable the timely identification of reduced oral function, helping to prevent further disability12 and tooth loss13. Non-adherence to dental visits has negatively impacted oral health outcomes14, underscoring the importance of encouraging older adults to attend dental checkups. There were many studies about the association between dental checkups and oral health outcomes, such as dental caries and periodontal status. Only a few studies have directly examined the association between dental checkups and oral function components. This gap highlights a need to raise awareness and promote dental checkup services, particularly among older adults. Public health initiatives, like oral health education, can encourage preventive dental visits and improve overall oral health15 by raising awareness and promoting proactive oral health care16. Given the integral role of oral function in overall oral health and healthy life expectancy16, promoting dental checkups adherence is crucial for preserving oral function as individuals age.
Research indicates that 37.8% of older Japanese outpatients have OHF, with prevalence increasing with age and correlating with reduced oral health-related quality of life17. Community-dwelling older adults exhibit higher rates of OHF compared to those receiving dental care18. To address these concerns, Japan has implemented several dental checkup programs targeting older adults under National Health Insurance, including subsidized annual checkups and Community-Based Prevention Programs. However, these often prioritize disease detection over comprehensive functional assessment5.
Despite Japan’s aging population, oral health promotion strategies have shown limited effectiveness in addressing oral function concerns among older adults19,20,21. Iwasaki et al. reported that current dental checkup systems rarely incorporate the sophisticated oral function components developed by Japanese researchers22. This discrepancy highlights the necessity for future research to bridge this gap by incorporating advanced oral function components into routine dental checkups. Although Japan possesses robust infrastructure for both oral function assessment and dental checkups, a significant research gap persists regarding the direct impact of regular dental examinations on oral functional outcomes in the aging population.
This study seeks to address the identified research gaps by examining the relationship between dental checkup attendance and oral function in older Japanese adults. Also, it could provide evidence-based insights into the importance of dental checkup attendance by evaluating all seven proposed parameters of oral function. Therefore, this study aims to raise public awareness, encourage dental visit habits for older adults, and advocate for the integration of oral function assessments into broader oral and general health frameworks for aging populations. We hypothesize that dental checkup attendance positively contributes to the preservation of oral function in older individuals.
Materials and methods
Approval statement
All experimental protocols were reviewed and approved by the Niigata University Ethics Committee (Reg no. 2021/0172) reviewed and approved all experimental protocols.
Accordance statement
All procedures were conducted in accordance with the guidelines and regulations outlined in the Declaration of Helsinki (1964). Written informed consent was obtained from all participants prior to their inclusion in the study.
Data collection
Participants were divided into two groups based on their dental checkup history. Each group underwent a data collection process that involved three specialized teams, each consisting of a professionally trained senior dentist and an assistant dentist. All team members underwent comprehensive training before the study to ensure systematic and consistent data collection.
The data were collected through a structured questionnaire and a clinical oral examination. The data collection protocol consisted of three main components. Team 1 conducted face-to-face interviews using the Mini-Mental State Examination (MMSE) and assisted participants with self-administered questionnaires covering demographics and general information. Team 2 performed oral examinations and measurements, including height and weight for Body Mass Index (BMI) calculations. Team 3 conducted detailed oral function assessments, evaluating seven key criteria: oral cleanliness, oral dryness, occlusal support, oral motor function, tongue pressure, masticatory performance, and swallowing function. All procedures followed standardized protocols to maintain data quality and reliability throughout the study.
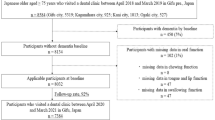
Cognitive function was assessed using the validated Japanese version of MMSE23. The healthy participants were included with no cognitive impairment or prolonged medication history. Individuals with potential cognitive impairment (MMSE score of less than 20), severe systemic diseases, or those taking medications affecting salivary secretion or oral function were excluded. The feasibility of the study protocol was confirmed through a pilot study from the same resource. A detailed participant selection process is illustrated in the flowchart diagram (see Additional Fig. 1). We collected data from May 2022 to December 2023 at the Preventive Dental Clinic at Niigata University Medical and Dental Hospital, using a convenience sampling method, and registered data in the evening on that day of collecting data from participants.
Study design and participants
A convenience sample of 235 older Japanese adults aged 65 and older was divided into two groups based on their dental checkup history. The first group, “dental checkup attendees” (n = 127), consisted of individuals who had attended checkups at least every six months at the Preventive Dental Clinic at Niigata University Medical and Dental Hospital. A standardized dental checkup involves several routine examinations and procedures. These include an oral examination, periodontal examination, optional X-rays, teeth cleaning (scaling and polishing if needed), oral hygiene and dietary advice, and treatment recommendations. The second group, “dental checkup non-attendees” (n = 108), comprised individuals from a local community center near the university hospital who reported no dental checkups within the past year.
Demographic information
Subjective questionnaires
A dentist from team 1 asked participants to complete self-administered questionnaires related to socioeconomic status (SES), general health status, and dental factors. The self-administered questionnaires are modified from the previous large-scale cohort study in Japan24. The participants were evaluated for the following characteristics: age, sex (male, female), education (high school or higher, junior high school or lower), marital status (married, unmarried), living status (with accompaniment, alone), current medication (yes, no), past medical history (yes, no), BMI (normal (18.5–24.9), underweight (< 18.5), overweight (≥ 25.0)) and dental factors; toothbrushing frequency (times/day) (≥ 2, ≤ 1), interdental brush usage (yes, no), and dental checkup (yes, no).
Assessment of oral function status
The participants were seated in reclinable chairs and underwent oral examinations under well-lit conditions. Team 2 conducted an oral examination and evaluated factors such as the number of remaining teeth, and occlusal support. Team 3 conducted oral function assessments as described in a previous study4. Oral function assessments were performed using seven diagnostic criteria (oral cleanliness, oral dryness, oral motor function (tongue-lip), tongue pressure, masticatory performance, swallowing function, and occlusal support). Oral function was assessed for functional decline, with scores ranging from 0 to 7. The score was 0 if all functions were normal.
Oral cleanliness
We utilized Bacteria Counter® from Panasonic Healthcare Co., Tokyo, Japan25, to measure oral cleanliness through dielectrophoretic impedance measurements by rubbing the dorsum of the tongue five times with a standardized cotton swab. Bacterial counts are expressed in colony-forming units per millilitre (CFU/ml) and are categorized from 1 to 7. Poor oral hygiene was indicated when the concentration exceeded 1 × 106.5 CFU/ml (score 4)4.
Oral dryness
Oral dryness was measured by collecting unstimulated saliva samples from participants seated comfortably in a private environment. Participants were asked to spit as much saliva as possible into a disposable paper cup within five minutes. The flow rate was calculated by weighing the saliva volume, and a value less than 0.1 ml/min indicated a diagnosis of oral dryness26.
Occlusal support
The remaining teeth (excluding third molars) were evaluated, and occlusal support was determined. Diminished occlusal support was identified if there were fewer than 20 remaining natural teeth4.
Oral motor function
Tongue-lip motor function was assessed using oral diadochokinetic (ODK) tests. A digital measuring device (KENKOU-KUN®; Takei Scientific Instruments Co., Ltd., Niigata, Japan) was used to measure the number of syllables pronounced per second. Participants were asked to repeatedly articulate the pa/, ta/, and ka/ syllables as quickly as possible for 5 s, and the number of articulations was counted. ODK scores were calculated separately for each syllable and recorded as the mean number of articulations per second. A decrease in function was determined if the count was less than six times per second for any syllable3.
Tongue pressure
A tongue pressure measuring device (TPM-01) (JMS, Hiroshima, Japan) was used to measure tongue pressure at the midline of the dorsum of the tongue27. Results of less than 30 kPa were considered to indicate reduced tongue pressure.
Masticatory performance
Masticatory performance was evaluated using gummy jelly (UHA Mikakuto Co., Ltd., Osaka, Japan) and a visual scoring method, with poor performance indicated by a score ≤ 2 points. Participants were instructed to chew a gummy jelly freely 30 times, and after chewing, to expectorate all the chewed fragments onto a piece of gauze spread over a paper cup covered with gauze. Participants with dentures were instructed to wear them while chewing28. The pieces of gummy jelly were spread out and the investigators subjectively evaluated them by the visual scoring method, which categorizes the pieces into ten levels (ranging from 0 to 9). To assess masticatory performance, we adopted a scoring method (ranging from 0 to 9).
Swallowing function
The repetitive saliva-swallowing test (RSST) was used to evaluate swallowing function. Participants were instructed to swallow saliva as many times as possible within 30 seconds, while the degree of deglutition was determined through palpation of the larynx. Dysphagia was noted if the participants met the criterion of occurring less than three times per 30 seconds4,29.
Statistical analysis
The data were collected through a structured questionnaire and a clinical oral examination. The Kolmogorov‒Smirnov test was used to analyze the normality of the data. The results are reported as the means and standard deviations or as frequencies and proportions. For non-parametric data, the Mann‒Whitney U test was performed to investigate differences in age and mean oral function scores. The chi-square test was used to evaluate relationships between covariate factors and outcomes. Linear regression analysis used the number of declined oral functions as the dependent variable because the normality assumption was met. For data analysis, IBM SPSS Statistics 25 (IBM, New York, USA) was used with a significance level of less than 5%. EndNote (Clarivate Analytics, New York, United States) was used for reference management.
Results
Characteristics of participants
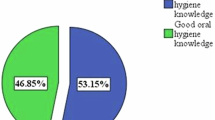
The current study included 235 participants with a participation rate of 95.9%. The mean age of the participant is 75.1 ± 5.6 years and 53.2% males. A total of 127 individuals had dental checkup experience, while 108 had no dental checkup experience. Male participants were less likely to attend dental checkups (31.5% attendance). Table 1 shows the general characteristics of the participants. Several factors were significantly associated with dental checkup attendance (Table 1). A significantly lower proportion of males (31.5%) attended checkups compared to females (78.7%) (p < 0.001). Differences in BMI values were also significantly associated with attendance (p = 0.024). Attendees reported better oral self-care practices, including more frequent tooth brushing (p < 0.001) and interdental brush use (p < 0.001).
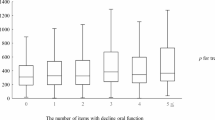
Characteristics of oral function and hypofunction status concerning dental checkups
Table 2 shows the characteristics of the oral function distribution of the participants. Most oral functions were within normal limits, except for poor oral cleanliness (5.1 ± 1.2) and decreased tongue pressure (29.6 ± 9.1). On average, participants had 23.3 ± 6.2 remaining natural teeth, with those who had dental checkups averaging 24.0 ± 4.9 and those without averaging 22.6 ± 7.4 remaining natural teeth. Those with dental checkup visits had better oral function than those without, except for tongue pressure. There was a significant difference between those with or without dental checkup visits in terms of oral cleanliness (p = 0.005), masticatory performance (p < 0.001), and swallowing function (p = 0.001). Table 3 presents the distribution of declined oral function across seven distinct parameters, comparing participants based on dental checkup attendance. Statistical analysis revealed significant differences between the groups for oral uncleanliness (p = 0.005), declined masticatory performance (p < 0.001), and declined swallowing function (p = 0.001).
Relationship between dental checkups and declined oral function
Linear regression analysis revealed that declined oral function was associated with age (B: 0.07; 95% CI: 0.04, 0.09) and sex (B: -0.46; 95% CI: -0.79, -0.14). Non-attendance at dental checkups showed a significant positive association with oral function decline in the crude analysis (B: 0.45; 95% CI: 0.12, 0.77). This association persisted after adjusting for socioeconomic factors (Model I: B: 0.45; 95% CI: 0.09, 0.80) and general health factors (Model II: B: 0.45; 95% CI: 0.08, 0.81). The final multiple regression model, adjusting for all potential confounders, confirmed this relationship (B: 0.56; 95% CI: 0.16, 0.97). Table 4 shows the adjusted linear regression models between dental checkups and declined oral function. (Details of crude linear regression analysis were shown in Additional Table 1.)
Discussion
The current study demonstrated that dental checkup attendance was significantly associated with better oral function in Japanese older adults. These associations remained significant even after adjusting for possible confounders including socioeconomic factors and general and dental healthcare variables. While previous studies have explored the potential impact of dental visits on oral health15,30, and physical health-related problems31,32,33, our study specifically addresses the previously unexplored relationship between dental checkups and oral function in the aging population.
Our study revealed that dental checkups were significantly associated with better oral cleanliness, a key determinant in preserving oral function4. Regular checkups facilitate early detection of oral health problems and enable personalized oral health education and appropriate hygiene measures, ultimately contributing to improved oral health34. Thus, these findings underscore the importance of dental visits in maintaining oral function over time.
We found that checkup attendees significantly demonstrated better masticatory performance than non-attendees, aligning with previous research34. This association can be explained through several mechanisms: checkups enable early detection of oral diseases like dental caries and periodontal problems, thereby reducing the risk of tooth loss30 and preserving chewing efficiency. Moreover, when tooth loss does occur, timely restorative treatments such as dentures can restore oral function. Our observation that checkup attendees showed better swallowing function aligns with previous findings35. The improvement in swallowing function may be attributed to dental checkups indirectly ensuring proper food breakdown, potentially mitigating dietary restrictions associated with chewing difficulties.
These findings collectively emphasize the importance of preserving natural teeth for optimal masticatory performance and overall well-being in older adults. However, impaired oral function, which may arise from tooth loss, can hinder chewing and processing food and negatively impact nutritional intake, potentially influence BMI in older adults, possibly resulting in underweight or obesity36. It is also important to acknowledge that BMI itself can be a confounding variable, potentially influencing both oral function and nutritional status. Our study confirms a relationship between dental checkup attendance and BMI in older adults, highlighting the importance of an integrated healthcare approach. Dental professionals should be aware of this potential link and collaborate with other healthcare providers to ensure comprehensive care.
While dental checkup attendees showed lower average tongue pressure than non-attendees, this difference may be influenced by age and sex, as tongue pressure varies across age decades and between sexes37. Our study observed a higher proportion of female participants in the checkup group, and conversely, a lower proportion in the non-checkup group. However, the intergroup comparison revealed no significant variation in tongue and lip motor function, suggesting a potential positive impact of oral health education on functional preservation. It is important to note that tongue and lip motor function is influenced by a range of factors beyond age and sex, including other oral functions and psychosocial factors38,39.
Even though the relationship between remaining teeth and dental checkup attendees shows no significant variation, an average of more than 20 remaining teeth was observed in both groups. This suggested sufficient occlusal support for the mastication40. While attendees and non-attendees showed a similar average number of remaining teeth, attendees demonstrated better oral cleanliness. This may be due to dental checkup attendees likely benefit from oral health education and preventive treatments to preserve natural teeth and maintain oral health.
There is no significant association was found between dental checkups and oral dryness in this study. This may be due to the diverse aetiologies of oral dryness, which include systemic diseases and medications that may overshadow any potential impacts of dental checkups. Future research is needed to investigate the complex relationship of these factors in oral health outcomes.
We found that dental checkup attendees had better oral hygiene care, masticatory performance, and swallowing functions. Our findings demonstrated that older adults who do not attend dental checkups experienced a notable decline in oral function. This might be explained by non-adherence to dental checkups, which may overlook the declining oral function until a significant problem arises, necessitating further emergency oral healthcare. Specifically, in our initial analysis, those without dental checkup attendance had a 0.45 unit decrease in oral function compared to those who attended dental checkups. This highlights the fundamental impact of dental care on oral function. This association remains significant across all models, even after adjusting for various factors. Upon adjusting socioeconomic factors including age, sex, education, marital status, and living status, the association remains significant. This consistency suggests that the beneficial effects of dental checkups are directly related to dental care itself, not just a byproduct of socioeconomic status. This aligns with the prior research indicating that routine dental attendees had better overall oral health15.
Further adjustment for general health status, such as current medications, past medical history, and BMI, does not change the significance of the findings. This indicates that the positive impact of dental checkups on oral function is independent of overall health. Besides, when we consider all potential influencing factors, including oral hygiene practices like toothbrushing frequency and interdental dental brush usage, the association between lack of dental checkups and reduced oral function becomes even more pronounced. This emphasizes the importance of comprehensive dental care, including regular checkups and consistent oral hygiene practices. The consistent significance of these findings across all models highlights the necessity of promoting regular dental checkups among older adults.
The observed decline in oral function among those who do not attend dental checkups calls for public health interventions. These interventions should focus on improving accessibility to dental care, particularly for older adults who may encounter barriers such as financial constraints and physical limitations. This might be explained by non-adherence to dental checkups may overlook the declining oral function until a significant problem arises, necessitating further emergency oral healthcare.
Study limitations
There are several limitations in our study. The cross-sectional nature of the study prevents the establishment of a causal direction. Potential selection bias and convenience sampling constrain the generalizability of the results to the entire population. While we acknowledge that lifestyle behaviors and financial considerations were not accounted for in this study, it is crucial to emphasize that health literacy was also not considered in the present study. Future research should prioritize investigations into the influence of health literacy to enhance our understanding of dental checkup adherence. Longitudinal studies incorporating interventions focused on the impact of lifestyle and financial behaviors are warranted to address the limitations of the present study. Furthermore, it is recommended to explore the psychological and social gradients and disparities in oral function to identify factors affecting older adults’ utilization of preventive oral health measures, including policies and practices.
Measuring oral dryness during a typical checkup usually only involves a quick observation, without usually including in-depth investigations into the causes of reduced salivary flow. Thus, another limitation of this study was that it relies on unstimulated salivary flow (USF) as a measurement. However, since USF measures saliva production at rest, a routine checkup is unlikely to significantly change it, making the results potentially unreliable.
Clinical implications
This study investigates the impact of dental checkup attendance on oral function in older adults, an area of focus given the globally aging populations. The robust association between dental checkup attendance and oral function across all analytical models underscores the reliability of our findings and adds to the existing body of knowledge. Our comprehensive approach, adjusting for socioeconomic status, general health, and oral hygiene practices, provides a better understanding of this relationship.
The increased associations observed in model III highlight the synergistic role of both dental visits and daily oral hygiene practices in maintaining oral function. Our findings suggest integrating comprehensive oral function assessments into routine dental examinations. While most participants maintained adequate tooth count, their oral function declined, particularly in hygiene, mastication, and swallowing. This indicates that dental care should focus on both tooth preservation and functional quality. These results have significant implications for public health initiatives clinically.
Healthcare providers should implement preventive strategies with early detection of functional decline, particularly for vulnerable populations (older adults, low socioeconomic status, poor oral hygiene, compromised dentition). Healthcare policy should address financial and physical barriers to dental care access to ensure equitable preventive care delivery. Encouraging both professional dental care and consistent home hygiene practices is crucial for preserving oral function and overall well-being in later life.
Future research recommendations
Future studies should focus on conducting robust longitudinal research to establish causal relationships between dental checkups and oral function decline in older adults. Researchers should investigate socioeconomic, cultural, and geographical barriers to dental care access through mixed-method approaches, combining quantitative and qualitative research. The development of standardized oral health surveillance systems is essential to monitor and evaluate intervention effectiveness across different populations.
To better understand the relationship between dental checkups and oral dryness, future research should consider multiple methods of measuring oral dryness, the impact of underlying medical conditions, the role of medications, and a more comprehensive study design to account for confounding variables. It is also advisable to explore the impact of dental checkup frequency and oral health literacy on older adults.
Additionally, research should evaluate the impact of various public health policies on dental care accessibility, particularly focusing on insurance coverage protocols for underserved populations. Studies examining the effectiveness of different dental education programs and their influence on regular checkup attendance would provide valuable insights for healthcare policy development. These could strengthen evidence-based preventive dental healthcare frameworks that optimize oral function and enhance the quality of life for older adults.
Conclusion
Dental checkup non-adherence correlates with oral functional decline in older adults, highlighting the importance of dental checkups as a preventive measure for maintaining optimal oral function, particularly in the older adult population. Healthcare providers should prioritize and develop accessible preventive dental services and implement comprehensive oral health surveillance systems for the overall quality of life of aging populations.
Data availability
The dataset utilized in this investigation is available upon formal request to the corresponding author. Public accessibility is restricted following privacy protocols, as the data contains information that could potentially compromise research participant confidentiality.
References
Dibello, V. et al. Oral frailty and its determinants in older age: a systematic review. Lancet Healthy Longev. 2 (8), e507–e520 (2021).
Nowjack-Raymer, R. E. & Sheiham, A. Numbers of natural teeth, diet, and nutritional status in US adults. J. Dent. Res. 86 (12), 1171–1175 (2007).
Tanaka, T. et al. Oral frailty as a risk factor for physical frailty and mortality in Community-Dwelling elderly. J. Gerontol. Biol. Sci. Med. Sci. 73 (12), 1661–1667 (2018).
Minakuchi, S. et al. Oral hypofunction in the older population: position paper of the Japanese society of gerodontology in 2016. Gerodontology 35 (4), 317–324 (2018).
Takehara, S. et al. The 8020 campaign in Japan: A policy analysis. Asia Pac. J. Public. Health. 37 (1), 116–125 (2025).
Ikebe, K. et al. Association of masticatory performance with age, gender, number of teeth, occlusal force and salivary flow in Japanese older adults: is ageing a risk factor for masticatory dysfunction? Arch. Oral Biol. 56 (10), 991–996 (2011).
Aida, J. et al. Burden of oral diseases and access to oral care in an ageing society. Int. Dent. J. 72 (4), S5–S11 (2022).
Teramoto, S. et al. High incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: a multicenter, prospective study in Japan. J. Am. Geriatr. Soc. 56 (3), 577–579 (2008).
Astrom, A. N. et al. Long-term routine dental attendance: influence on tooth loss and oral health-related quality of life in Swedish older adults. Community Dent. Oral Epidemiol. 42 (5), 460–469 (2014).
Ishimaru, M. et al. Dental utilization stratified by the purpose of visit: A Population-Based study in Japan. Int. Dent. J. 73 (6), 896–903 (2023).
Zaitsu, T., Saito, T. & Kawaguchi, Y. The oral healthcare system in Japan. Healthc. (Basel) 6(3), 79 (2018).
Maille, G. et al. Use of care and the oral health status of people aged 60 years and older in France: results from the National health and disability survey. Clin. Interv Aging. 12, 1159–1166 (2017).
Thomson, W. M. et al. Long-term dental visiting patterns and adult oral health. J. Dent. Res. 89 (3), 307–311 (2010).
Lertpimonchai, A. et al. The association between oral hygiene and periodontitis: a systematic review and meta-analysis. Int. Dent. J. 67 (6), 332–343 (2017).
Murakami, K. et al. Associations of health literacy with dental care use and oral health status in Japan. BMC Public. Health. 23 (1), 1074 (2023).
Irie, K. et al. Relationship between risk of oral frailty and awareness of oral frailty among community-dwelling adults: a cross-sectional study. Sci. Rep. 14 (1), 433 (2024).
Morinaga, D. et al. Relationships between test results for oral hypofunction, subjective frailty symptoms and oral Health-Related quality of life of Japanese dental outpatients: A multicentre, Cross-Sectional study. J. Oral Rehabil. 51 (12), 2634–2642 (2024).
Izutsu, M. et al. Risk factors for oral frailty among community-dwelling pre-frail older adults in Japan: A cross-sectional analysis. Community Dent. Health. 40 (4), 221–226 (2023).
World Health Organization. Oral Health. ; (2021). Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA74/A74_R5-en.pdf
Tsuji, I. Current status and issues concerning health Japan 21 (second term). Nutr. Rev. 78 (12 Suppl 2), 14–17 (2020).
Cabinet Office of Government of Japan. The Aging Society: Current Situation and Implementation Measures FY 2017. ; (2018). Available from: https://www8.cao.go.jp/kourei/english/annualreport/2018/pdf/c1-1.pdf
Iwasaki, M. et al. Correlation between number of teeth and mortality: the significance of retaining 28 teeth during later life. J. Dent. Health. 69 (3), 131–138 (2019).
Ideno, Y. et al. Evaluation of a Japanese version of the Mini-Mental state examination in elderly persons. Geriatr. Gerontol. Int. 12 (2), 310–316 (2012).
Fujiwara, N. et al. Exploratory research on determinants of place of death in a Large-scale cohort study: the JPHC study. J. Epidemiol. 33 (3), 120–126 (2023).
Hirota, K. et al. Evaluation of a rapid oral bacteria quantification system using dielectrophoresis and the impedance measurement. Biocontrol Sci. 19 (1), 45–49 (2014).
Wiener, R. C. et al. Hyposalivation and Xerostomia in dentate older adults. J. Am. Dent. Assoc. 141 (3), 279–284 (2010).
Yoshikawa, M. et al. Comparison of three types of tongue pressure measurement devices. Dysphagia 26 (3), 232–237 (2011).
Igarashi, K. et al. Validity of a visual scoring method using gummy jelly for evaluating chewing efficiency in a large-scale epidemiological survey. J. Oral Rehabil. 46 (5), 409–416 (2019).
Persson, E., Wårdh, I. & Östberg, P. Repetitive saliva swallowing test: norms, clinical relevance and the impact of saliva secretion. Dysphagia 34 (2), 271–278 (2019).
Eguchi, T. et al. Factors associated with undergoing regular dental Check-ups in healthy elderly individuals. Bull. Tokyo Dent. Coll. 59 (4), 229–236 (2018).
Tomioka, K., Kurumatani, N. & Saeki, K. Regular dental visits May prevent severe functional disability: A community-based prospective study. Arch. Gerontol. Geriatr. 88, 104019 (2020).
Kubota, C. et al. Gender differences in the relationship between personality, cognitive function and regular dental visits in Japanese community-dwelling older adults. Int. J. Dent. Hyg. 20 (3), 553–563 (2022).
Shirahase, R. et al. A Cross-Sectional study on the relationship between oral function and sarcopenia in Japanese patients with regular dental maintenance. Int. J. Environ. Res. Public. Health 19(9), 5178 (2022).
Janto, M. et al. The importance of periodic dental control in the oral health status of elderly patients. Clin. Pract. 13 (2), 537–552 (2023).
Okamoto, N. et al. Relationship between swallowing problems and tooth loss in community-dwelling independent elderly adults: the Fujiwara-kyo study. J. Am. Geriatr. Soc. 60 (5), 849–853 (2012).
Issrani, R. et al. Exploring an association between body mass index and oral Health-A scoping review. Diagnostics (Basel) 13(5), 902 (2023).
Iwasaki, M. et al. Population-based reference values for tongue pressure in Japanese older adults: A pooled analysis of over 5,000 participants. J. Prosthodont. Res. 67 (1), 62–69 (2023).
Hatanaka, Y. et al. Impact of oral health guidance on the tongue-lip motor function of outpatients at a dental hospital. Gerodontology 39 (1), 83–89 (2022).
Tun, T. Z. et al. Oral diadochokinesis and potential associated factors in Japanese older adult outpatients. Oral Health Prev. Dent. 22 (1), 601–608 (2024).
Ueno, M. et al. Category of functional tooth units in relation to the number of teeth and masticatory ability in Japanese adults. Clin. Oral Investig. 14 (1), 113–119 (2010).
Acknowledgements
We would like to express our heartfelt gratitude to all participants from the preventive dental clinics of the university hospital clinics and the community center. We extend our heartfelt appreciation to Teru Watanabe, Aulia Ramadhani, Fania Chairunisa, Chit Su Khaing, and all the other colleagues and staff who contributed their utmost effort.
Funding
This study was partially supported by the Futoku Foundation (Grant for overseas) and by the JSPS KAKENHI Grant-in-Aid for Scientific Research (C), JP19K10439. The funder has no role in the study design, data collection, analysis, or interpretation of the data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
T.Z.T. wrote the manuscript as the first author, while S.T. conceived and designed the study as the corresponding author. K.M.T., S.T., T.Z.T., N.K., and K.M. contributed to the data collection, and K.M.T. and T.Z.T. interpreted the data. After T.Z.T. finished writing the manuscript, K.M.T. closely supervised it, and S.T., N.K., and K.M. supervised it. S.T. and H.O. revised the final manuscript, which has been read and approved by all the authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that there are no competing interests. The study design, data collection, analysis, interpretation, preparation of the manuscript, and choice to publish the findings were all made independently of the funders.
Ethical approval
All study procedures involving study participants were approved by the Niigata University Ethics Committee of the 1964 Declaration of Helsinki (2021/11/10) (Reg no. 2021/0172), and all participants provided written informed consent before the study procedure. The participants were free to revoke their consent at any time. All data and information were stored in a secure location and assigned a coded ID number to ensure confidentiality, and all procedures were conducted according to the relevant guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tun, T.Z., Thwin, K.M., Takehara, S. et al. Impacts of dental checkups on oral function among Japanese older adults. Sci Rep 15, 17622 (2025). https://doi.org/10.1038/s41598-025-02206-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02206-5