Abstract
This retrospective study aimed to evaluate the incidence of medication-related osteonecrosis of the jaw (MRONJ) and associated antiresorptive drugs in the Finnish population. All adult patients (aged 18 years and older) who were prescribed with antiresorptive drugs (AR) during 2013–2015 were included in this study. A total of n = 58,367 patients met the inclusion criteria and were followed up until 2020. The outcome variable was the diagnosis of MRONJ during the study period. Patients’ age, gender, type of AR prescribed, reason for using AR drugs, use of corticosteroids, use of vascular endothelial growth factor (VEGF) inhibitors were used as covariates. The incidence of MRONJ was 0.3% in low-dose and 9.0% in high-dose AR recipients in this study population. The risk of developing MRONJ among denosumab users was 5 times higher in both low-dose and high-dose AR recipients compared to bisphosphonates users. Simultaneous use of corticosteroids in addition to AR drug increased the risk of developing MRONJ by 2 times in high-dose recipients and 6 times in low-dose recipients. In conclusion, male, denosumab, any type of cancer diagnosis, high dose of AR drug and simultaneous use of corticosteroids were the most noteworthy risk factors for MRONJ.
Similar content being viewed by others
Introduction
Antiresorptive drugs are mainly used in the management of osteoporosis and secondary malignant neoplasms. They are also used in treatment of multiple myeloma, osteitis deformans (a.k.a. Paget’s disease) and giant cell granuloma1,2,3. The most common antiresorptive drugs are denosumab and bisphosphonates (BP), which can be administered orally (BP), intravenously (BP) or subcutaneously (denosumab). The use of antiresorptive drugs has been linked with the medication-related osteonecrosis of the jaw (MRONJ). The most widely accepted definition of MRONJ was established by The American Association of Oral and Maxillofacial Surgeons (AAOMS). According to this definition, MRONJ is the exposed bone or bone that can be probed through an intraoral or extraoral fistula in the maxillofacial region that has persisted for longer than eight weeks. The patient typically has been exposed to current or previous treatment with antiresorptive (AR) or antiangiogenic agents and has no history of radiation therapy to the jaws or obvious metastatic disease to the jaws4.
The first case of MRONJ was diagnosed in 2003, and since then the number of diagnosed MRONJ cases has been reported frequently5. In cancer patients, a mean incidence of MRONJ of 6.1% was reported previously in 20106. Most recently a systematic review and meta-analysis concluded a varied range of prevalence (1–19%) of MRONJ in both cancer and osteoporosis patients depending upon the choice of antiresorptive therapy, dose, and administration route7. A previous Nordic study consisted of MRONJ cases reported specifically to national Medical Agencies of Denmark, Finland, Norway and Sweden. The cumulative incidence was found to be 0.7, 0.8, 1.1 and 1.3 per 100,000, respectively. However, those unreported MRONJ cases to the Medical Agencies may have been missed out8.
Bisphosphonates (BP) were initially used as antiresorptive drugs. However, since the introduction of denosumab, its use has grown exponentially, globally4,9 as well as in Finland10. In 2016, there were approximately 44 000 antiresorptive drug users in Finland, 28 000 of them using bisphosphonates and 16 000 denosumab10. Several previous studies have also reported that the MRONJ is more common among denosumab users compared to bisphosphonates7,9,11. For instance, incidence of MRONJ was found to be 4.1–13.0% among breast cancer patients with bone metastases treated with antiresorptive drugs, and most common among denosumab-treated patient12. A previous case series study that included 254 men diagnosed with prostate cancer and bone metastases from Helsinki University Hospital concluded that 11.4% of them developed ONJ and 86% of the ONJ cases were detected during denosumab therapy13. Additionally, those using multiple antiresorptive drugs in sequence, such as pamidronate-zoledronate therapy or bisphosphonate-denosumab therapy have higher incidence of MRONJ when compared to single antiresorptive drug7,14. Furthermore, the incidence is also higher among high dose users compared to low-dose users and among intravenous administration compared to peroral route. For instance, in a Swedish prospective cohort study (55 patients followed, in a population of 1.3 million, over 4 years), the incidence rates were 0.043% for low-dose oral BP, 1.03% for high-dose intravenous BP, and 3.64% for high-dose denosumab15.
However, to our knowledge, despite a centralised data registration system in Finland, a large population-based cohort study among the antiresorptive drugs user has not been done before. Therefore, it is important to evaluate the incidence of MRONJ and use of associated antiresorptive drugs in the Finnish population.
Results
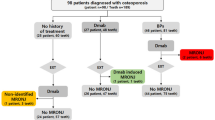
The mean (SD) age of the patient was 72.4 (11.6) years, and more than four-fifths of the patients (82%) were female. More than half of the patients (63.2%) were receiving bisphosphonate therapy, almost one-fourth (22.1%) were receiving denosumab therapy, and about 15% (14.6%) were receiving sequential therapy. Osteoporosis was the most common reason (86.7%) for using antiresorptive drugs. The incidence of MRONJ varied between 0.14% and 11.41% depending on the purpose of use and dosage during the follow-up period (2013/2015 to 2020) and the majority of them were denosumab users (315/432) (Tables 1 and 2).
Figure 1 illustrates the yearly incidence of MRONJ in high dose and low dose recipients, and peaked during the fifth year for both high-dose (n = 85) and low dose (n = 25) recipients.
Figures 1 and 2 illustrate the yearly incidence of MRONJ. The incidence increased rapidly after around 40 months of use and keeps on increasing especially in denosumab users.
The risk of developing MRONJ among denosumab users was 5 times higher in both low-dose (HR: 5.03, 95% CI: 3.23–7.82) and high-dose (HR: 5.07, 95% CI: 2.94–8.72) AR recipients compared to bisphosphonates only users. Similarly, risk of developing MRONJ among both AR drug (bisphosphonates followed by denosumab) was 2.4 times higher in low-dose AR recipients (HR: 2.37, 95% CI: 1.42–3.96) as well as in high-dose AR recipients (HR: 2.39, 95% CI: 1.43–4.00) compared to bisphosphonates only users. Additionally, the low-dose AR recipients diagnosed with cancer had 99-fold risk (HR: 99.21, 95% CI: 51.69–190.43) of developing MRONJ compared to those diagnosed with only osteoporosis. Likewise, simultaneous use of corticosteroids in addition to AR drug increased the risk of developing MRONJ by 6.3 times in low-dose AR recipients (HR: 6.35, 95% CI: 3.71–10.87) and by 2 times in high-dose AR recipients (HR: 2.01, 95%CI: 1.52–2.64). Simultaneous VEGF use moderately increased the risk only in high-dose AR recipients (HR = 1.77, 95% CI 1.23–2.54). Among the high-dose recipient, female had significantly lower risk of developing MRONJ compared to male (HR 0.33, 95% CI 0.22–0.48) (Table 3).
Discussion
This study aimed to evaluate the incidence of MRONJ and associated antiresorptive drugs in the Finnish population. The incidence of MRONJ differed from 0.14 to 11.41 during the follow-up period (2013/2015 to 2020) depending on the purpose of use and dosage. The risk of MRONJ was 0.3% in low-dose recipients and 9.0% in high-dose recipients. The risk of developing MRONJ among denosumab users was consistently higher in all patient groups compared to only bisphosphonates users. Additionally, the patients diagnosed with cancer receiving low-dose ARs had almost 100-fold risk of developing MRONJ compared to those diagnosed with only osteoporosis. Likewise, simultaneous use of corticosteroids in addition to ARs increased the risk of developing MRONJ by 6 times in low-dose AR recipients and by 2 times in high-dose AR recipients. Simultaneous VEGF use moderately increased the risk only in high-dose AR recipients. Among the high-dose recipient, female had significantly lower risk of developing MRONJ compared to male.
To our knowledge, this is the first population-based cohort study among the antiresorptive drug users in Finland. Another strength of the present study was large sample (n = 58367) that were followed up for a period of 5 to 7 years. Merging of the observations in steps in Kaplan-Meier survival analyses can be considered as limitation of the present study. However, in order to maintain the anonymity of the patient as required by the secondary use of social and health data act in Finland16, it was necessary. Another limitation was the use of M87.1 that may have included cases of medication related to ear canal osteonecrosis (MRECO). However, it may not have impacted the result from this study as MRECO is very rare and only 30 cases have been reported globally during 2005-202217. Furthermore, this is a registry-based study with pseudonymized data making this study more explorative than definitive.
In the present study, the incidence of MRONJ was found to be 0.8% after 5–7 years of antiresorptive therapy in total population. An earlier case-report study conducted in four Nordic countries (Denmark, Finland, Norway, and Sweden) reported incidence of 0.7–1.3 during the period of 2003–2010 in their study population8. However, Krüger and colleagues (2013) studied the incidence of bisphosphonate-related osteonecrosis of jaw (BRONJ) and they studied only the cases reported to National Medicine Agencies, which doesn’t make the reported incidence fully comparable with the present study. Additionally, denosumab might have been excluded from the study by Krüger and colleagues because of the late introduction of denosumab in Europe in June 2010. Since then, the use of denosumab has grown rapidly in Finland and presumably in other Nordic countries too, and it has partly replaced the use of bisphosphonates10. In the present study, denosumab-related osteonecrosis of the jaw (DRONJ) was 0.6% in low-dose patients and 11% in high-dose cancer patients, which indicates significantly higher risk of MRONJ across all patient groups compared to bisphosphonate users (0.1% and 2.6%, respectively). In patients using sequential therapy the incidence of MRONJ was 0.3% and 7.6%, respectively. The incidence of BRONJ in this present study is relatively low compared to the study by Krüger and colleagues (2013) and on similar level on high-dose patients compared to the systematic review by Limones et al. in 20149 Similarly, the incidence of BRONJ in total population in the present study corroborates with a registry-based study from Hungary18. Furthermore, when patients are stratified by the diagnosis, incidence of MRONJ was similar to a South Korean study conducted in osteoporotic patient as well as Swedish study conducted in breast cancer patient with malignancy12,19.
Furthermore, the risk of MRONJ has been shown to rise yearly if the medication is continued9. In the present study, similar trends were noted particularly among the high-dose recipients. The risk started to increase more rapidly after five years of antiresorptive use. Previously, the risk of MRONJ has been shown to increase after three years of use and it might increase even after 10 years of use in low dose recipients. In comparison, high dose denosumab and zoledronic acid receivers are exposed to risk of MRONJ immediately20. Considering that our follow-up period was limited between 5 and 7 years, it is expectable that some MRONJ cases have been missed, especially in low-dose bisphosphonate users.
Notably, the risk of developing MRONJ was higher among denosumab users as well as among bisphosphonate combined with denosumab users compared to bisphosphonate only users in this study. There is robust evidence related to higher risk of denosumab users compared to bisphosphonate users1,7,9,11,12. The possible pathophysiology could be due to the effect of tissue’s TRAP (tartrate-resistant acid phosphatase) level, which indicates the number of osteoclasts in the tissue as explained by Williams and colleagues21. Denosumab therapy reduces the TRAP level close to zero whereas TRAP level is high during bisphosphonate therapy and so is the number of osteoclasts. If the development of MRONJ is largely related to inhibiting the direct activity of osteoclasts, then one could assume that denosumab is a more likely drug to induce the development of MRONJ lesions21. In addition, denosumab and bisphosphonates have not necessarily been compared equally, as it has been observed that bisphosphonate-induced ONJ lesions develop slower than those of denosumab. Unlike bisphosphonates, denosumab does not accumulate in the bones and it has a circulatory half-life of 26 days, compared to bisphosphonates half-life of 10 years22,23. Hereby, denosumab is not necessarily any more likely to cause MRONJ than bisphosphonates, but the onset of the disease and thus the diagnosis is probably made earlier in patients with denosumab medication24. Longer follow-up periods, even up to 10 to 15 years, would be needed to exclude these questions more definitely. However, as the mean age of antiresorptive users is relatively high, as long onset periods as 10–15 years might not be meaningful in terms of life span or quality.
In the present study, higher doses of ARs had a significant risk for development of MRONJ. This is probable to be related to the fact that high-dose recipients are more often immuno-compromised. Intravenous and subcutaneous administration also increases the absorption of the drug compared to oral administration route, which might play a role. In clinical practice, dosage of ARs can be broadly categorized into two main groups (high-dose and low-dose). The first group includes antiresorptive to treat cancer-related conditions e.g. bone metastases. These ARs are administered in higher doses and always intravenously or subcutaneously (e.g. 5 mg intravenous zoledronic acid every 4 weeks and 120 mg denosumab subcutaneous every 4 weeks)9. The second category includes ARs to treat patients with osteoporosis and these ARs are more often orally administered but can additionally be administered intravenously or subcutaneously depending on the choice of medication (e.g. 70 mg peroral alendronate weekly, 5 mg intravenous zoledronic acid once a year and subcutaneous 60 mg denosumab every six months)25,26,27. Similar to the present study, intravenously administered zoledronic acid and subcutaneously administered denosumab have been proven in previous literature to be the most potent AR drugs to induce MRONJ1,4,28. The incidence of MRONJ in cancer patients treated with subcutaneous denosumab ranged from 0.5 to 3.2% and with intravenous zoledronic acid treated patients from 0.4–2.3%25. In a meta-analysis, the difference in risk of MRONJ was not significant between denosumab and zoledronic acid patients4,29, which indicates that higher doses are more potent to cause MRONJ apart from medication used.
As mentioned earlier, it is also to be noted that cancer patients are immuno-compromised and thereby have a higher risk of developing MRONJ. Furthermore, chemotherapy induces xerostomia, which is exposed to increased risk of caries and tooth extractions. In a Brazilian prospective cohort study, prevalence of xerostomia was 48% in breast cancer patients30 and in another American cross-sectional study 39% of the oropharyngeal cancer patients reported severe symptoms of xerostomia31. Poor oral hygiene has also been linked to a lower survival in head and neck cancers, which might similarly play a role in overall occurrence rate of MRONJ32. It is well known that poor oral hygiene is one of the leading causes for dental caries, periodontitis and if left untreated leads to periapical periodontitis and fistulas. Additionally, it has recently been suggested that MRONJ lesion requires inflammatory stimulus to occur, and the trauma caused by tooth extraction itself would play a smaller role than previously assumed33. Oral cavity offers ideal conditions for infections in terms of potent microbes (for example Aggregatibacter actinomycetemcomitans and Porphyromonas gingivalis), plaque and oral traumas. Low pH levels, which are present in infection sites, are shown to induce osteonecrosis development by releasing bisphosphonate from bone tissue. Besides, bone regeneration becomes disturbed by reduced osteoclast activity due to antiresorptive therapy increasing risk for MRONJ33. The presence of inflammatory conditions is naturally higher in poor oral conditions, which suggests that poor oral hygiene increases the risk of MRONJ.
Use of corticosteroids increased the risk of developing MRONJ in the present study as well as VEGF inhibitor use in high-dose recipients. These findings are similar to a recent position paper by the American Association of Oral and Maxillofacial Surgeons4. Furthermore, authors reported that when corticosteroids and antiresorptive are used together the risk multiplies. However, Hallmer and colleagues (2020) reported that use of corticosteroids decreases the risk of MRONJ. It can be presumed that the VEGF inhibitor medication affects bone remodeling by inhibiting vascular endothelial growth factors (VEGFs) thereby inhibiting the growth of new blood vessels, bone regeneration and differentiation of osteoblasts34. Simultaneous antiresorptive use, which by virtue, inhibits osteoclast activity and cell apoptosis is thought to accumulate the development process of MRONJ4,35. Corticosteroids on the other hand are theorized to induce osteocyte apoptosis, which results in similar consequences as VEGF inhibition36,37. While corticosteroids are commonly prescribed in cancer patients, the incidence should be studied between corticosteroid-medicated cancer patients and non-corticosteroid-medicated cancer patients to deduce the definite differences in risk of corticosteroid use.
Female had lower risk of MRONJ compared to male. This might be related to a higher risk of developing MRONJ due to prostate cancer than to breast cancer. Hata et al., 2022 studied the difference in MRONJ incidence between different cancer diagnosis patients. Prostate cancer was similarly found to be a risk factor in MRONJ development. Although, in their study other types of cancers and especially lung cancer diagnosis balanced the differences in cumulative incidence between genders as male-dominated lung cancer patients rarely developed MRONJ38. It can be speculated that the difference is more likely to be found in dental hygiene practices, comorbidities, and other qualitative habits of living. For instance, Finnish men brush teeth less frequently, have more plaque on tooth surfaces, use more often prosthesis and drink and smoke more often than females39. Therefore, future studies should incorporate oral health-related factors and comorbidities among MRONJ patients.
It is to be noted that the risk of MRONJ should be evaluated by the purpose of use and dosage rather than the choice of drug. Given the risk of bisphosphonate being low, evasion of denosumab treatment should be seriously considered if bisphosphonate treatment is a respectable alternative. Additionally, health care practitioners should be encouraged for comprehensive proactive dental treatment for each patient before the initiation of antiresorptive medications.
In conclusion, denosumab or sequential use of both denosumab and bisphosphonate, any type of cancer diagnosis, high dose of AR drug and simultaneous corticosteroid treatment were the most noteworthy risk factors for MRONJ in our study. Therefore, choice of antiresorptive drugs must be cautiously considered before its use.
Methods
Study design and participants
This retrospective study utilized the data obtained from national registries of Finland, the Finnish Institute for Health and Welfare (THL) database and the Social Insurance Institution of Finland (Kela). The THL database comprises national patient registers known as Avohilmo and Hilmo. The registers cover both primary healthcare (Avohilmo) and specialized health care (Hilmo) patient data collected in Finland to be utilized in decision-making, planning and research. All the adult patients (aged 18 years and older) who were prescribed with antiresorptive drugs (AR) during 2013–2015 were included in this study. The Anatomical Therapeutic Chemical (ATC) codes (M05BA01-08, M05BB01-09 and M05BX04) were used for listing the AR drugs use. All patients (n = 58367) who met inclusion criteria were included in this study and were followed up until 2020.
Ethical issues
This study utilizes secondary data from national registries therefore a separate ethical approval was not required. Due to the retrospective nature of the study, the Finnish Institute for Health and Welfare (THL) database and the Social Insurance Institution of Finland (Kela) waived the need of obtaining informed consent. However, as per the legislation on secondary use of social and health data16, a separate permit from the Finnish Social and Health Data Permit Authority (Findata) was obtained (Permission number: THL/3317/14.02.00/2021). Anonymous data was requested and received from Findata. The act on the secondary use of health and social data obliges Findata to provide specifying regulations on matters such as secure operating environments, data descriptions and data permit applications and data utilization plans. All the methods in this study were performed in accordance with the relevant guidelines and regulations.
Outcome variable
The outcome variable for this study was the diagnosis of MRONJ among the antiresorptive drugs users during the study period. The diagnosis of MRONJ (M87.1) was confirmed using the International Classification of Diseases 10 th Revision ICD-10 code40. In Finland, M87.1# is used for the diagnosis of osteonecrosis due to drugs in jaw.
Covariates
Data on age and gender of patients who received AR drugs, type of AR prescribed, reason for using AR drugs, dosage of AR drugs, use of corticosteroids, and use of vascular endothelial growth factors were used as covariates. The International Classification of Diseases 10 th Revision ICD-10 codes were used to define the underlying cause for using AR drugs (M80, M81, M82 for osteoporosis; C50 for breast cancer; C61 for prostate cancer; C90 for multiple myeloma; and C76-C80 for malignant neoplasm from other sites). Additionally, the ATC codes were used to define the use of corticosteroids (H02) and vascular endothelial growth factor inhibitors (L01)41.
Statistical methods
All statistical analyses were performed using IBM-SPSS Statistics (version 26, SPSS, Inc., Chicago, Ill., USA) and R software version 4.2.2 (R Core Team 2022). For statistical analyses, covariates were categorized as age (≤ 64 years and ≥ 65 years), gender (male and female), type of AR prescribed (bisphosphonates, denosumab, and sequential therapy), purpose of using AR drugs (osteoporosis, breast cancer, prostate cancer, multiple myeloma, and malignant neoplasm from other sites), use of corticosteroids, use of vascular endothelial growth factor inhibitors and dosage of AR drugs (high dose that included patient diagnosed with breast or prostate cancer with bone metastases, patient diagnosed with malignant neoplasm, patient diagnosed with multiple myeloma and low dose that included patient diagnosed with breast or prostate cancer without bone metastases, patient diagnosed with osteoporosis).
Proportions were calculated and the difference in proportion between groups were evaluated using chi-square test. To study the association between the outcome variable and co-variates, Cox regression analyses were performed. Hazard Ratios (HR) and 95% confidence intervals (95% CI) were computed. For analyses, reason for using AR drugs were recategorized as osteoporosis, and any type of cancer (breast cancer, prostate cancer, multiple myeloma, and malignant neoplasm from other sites). The Kaplan-Meier survival curves were drawn to study the time-event occurrence of the MRONJ, and the Log-rank tests were performed to determine the difference in occurrence of MRONJ for different groups. However, to maintain the anonymity of patient as required by the legislation16, any steps that corresponded with less than sufficient number of observations (< 5 counts in this study) in Kaplan-Meier survival curves were merged with the adjacent higher time (in months). The p-value was set at < 0.05 for statistical significance.
Data availability
The data that support the findings of this study can be requested from the Finnish Social and Health Data Permit Authority (Findata; THL/3317/14.02.00/2021). Corresponding author can be contacted for help with the data request from Findata.
References
Ruggiero, S. L. et al. American association of oral and maxillofacial surgeons position paper on Medication-Related osteonecrosis of the Jaw—2014 update. J. Oral Maxillofac. Surg. 72, 1938–1956 (2014).
Poubel, V. L. et al. C. The risk of osteonecrosis on alveolar healing after tooth extraction and systemic administration of antiresorptive drugs in rodents: a systematic review. J. Cranio-Maxillofacial Surg. 46, 245–256 (2018).
Basu Mallick, A. & Chawla, S. P. Giant cell tumor of bone: an update. Curr. Oncol. Rep. 23, 51 (2021).
Ruggiero, S. L. et al. American association of oral and maxillofacial surgeons’ position paper on Medication-Related osteonecrosis of the Jaws—2022 update. J. Oral Maxillofac. Surg. 80, 920–943 (2022).
Marx, R. E. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J. Oral Maxillofac. Surg. 61, 1115–1117 (2003).
Migliorati, C. A. et al. A systematic review of bisphosphonate osteonecrosis (BON) in cancer. Support. Care Cancer. 18, 1099–1106 (2010).
Srivastava, A. et al. Prevalence of medication related osteonecrosis of the jaw in patients treated with sequential antiresorptive drugs: systematic review and meta-analysis. Support. Care Cancer. 29, 2305–2317 (2021).
Krüger, T. B., Sharikabad, M. N. & Herlofson, B. B. Bisphosphonate-related osteonecrosis of the jaw in four nordic countries and an indication of under-reporting. Acta Odontol. Scand. 71, 1386–1390 (2013).
Limones, A. et al. Medication-related osteonecrosis of the jaws (MRONJ) in cancer patients treated with denosumab VS. zoledronic acid: A systematic review and meta-analysis. Med. Oral Patol. Oral Cir. Bucal. e326–e336. https://doi.org/10.4317/medoral.23324 (2020).
Social Insurance Institution. Finnish statistics on medicines. (2016). https://www.julkari.fi/handle/10024/135599
Saad, F. et al. Incidence, risk factors, and outcomes of osteonecrosis of the jaw: integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann. Oncol. 23, 1341–1347 (2012).
Hallmer, F., Bjarnadottir, O., Götrick, B., Malmström, P. & Andersson, G. Incidence of and risk factors for medication-related osteonecrosis of the jaw in women with breast cancer with bone metastasis: a population-based study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 130, 252–257 (2020).
Vehmanen, L., Suojanen, J., Kontio, R., Utriainen, T. & Blomqvist, C. High frequency of osteonecrosis of the jaw among denosumab-treated prostate cancer patients. Acta Oncol. (Madr). 56, 104–106 (2017).
Coello-Suanzes, J. et al. Preventive dental management of osteonecrosis of the jaws related to Zoledronic acid treatment. Oral Dis. 24, 1029–1036 (2018).
Hallmer, F. et al. Prevalence, initiating factor, and treatment outcome of medication-related osteonecrosis of the jaw—a 4-year prospective study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 126, 477–485 (2018).
Finlex Act on the Secondary Use of Health and Social Data, Finland. (2019). https://www.finlex.fi/en/legislation/2019/552#Text%20of%20statute
Khan, I. Medication-related osteonecrosis of the external auditory canal – A rapid review of the literature and relevance to special care dentists. Spec. Care Dentist. 44, 314–327 (2024).
Veszelyné Kotán, E. et al. Database analysis of the risk factors of bisphosphonate-related osteonecrosis of the jaw in Hungarian patients. BMJ Open. 9, e025600 (2019).
Ko, S. Y., Hwang, T. Y., Baek, K. & Park, C. Incidence and severity of medication-related osteonecrosis of the jaw in patients with osteoporosis using data from a Korean nationwide sample cohort in 2002 to 2019: a retrospective study. J. Yeungnam Med. Sci. 41, 39–44 (2024).
Nicolatou-Galitis, O. et al. Medication-related osteonecrosis of the jaw: definition and best practice for prevention, diagnosis, and treatment. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 127, 117–135 (2019).
Williams, D. W. et al. Impaired bone resorption and woven bone formation are associated with development of osteonecrosis of the Jaw-Like lesions by bisphosphonate and Anti–Receptor activator of NF-κB ligand antibody in mice. Am. J. Pathol. 184, 3084–3093 (2014).
Owosho, A. A. et al. Medication-related osteonecrosis of the jaw: an update on the memorial sloan kettering cancer center experience and the role of premedication dental evaluation in prevention. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 125, 440–445 (2018).
Papapoulos, S. E. & Cremers, S. C. L. M. Prolonged bisphosphonate release after treatment in children. N. Engl. J. Med. 356, 1075–1076 (2007).
Williams, W. B. & O’Ryan, F. Management of Medication-Related osteonecrosis of the jaw. Oral Maxillofac. Surg. Clin. North. Am. 27, 517–525 (2015).
Beth-Tasdogan, N. H., Mayer, B., Hussein, H., Zolk, O. & Peter, J. U. Interventions for managing medication-related osteonecrosis of the jaw. Cochrane Database of Systematic Reviews (2022). (2022).
Mastrantoni, L. et al. Adjuvant denosumab in early breast cancer: a systematic review and meta-analysis of randomized controlled clinical trials. Ther. Adv. Med. Oncol. 15, 175883592311731 (2023).
Wang, Q., Yu, Q., Zeng, P. & Ai, W. Efficacy and safety of annual infusion of Zoledronic acid and weekly oral alendronate in the treatment of primary osteoporosis: A Meta-Analysis. J. Clin. Pharmacol. 63, 455–465 (2023).
McGowan, K., McGowan, T. & Ivanovski, S. Risk factors for medication-related osteonecrosis of the jaws: A systematic review. Oral Dis. 24, 527–536 (2018).
Chen, F. & Pu, F. Safety of denosumab versus Zoledronic acid in patients with bone metastases: A Meta-Analysis of randomized controlled trials. Oncol. Res. Treat. 39, 453–459 (2016).
Pinto, V. L., Fustinoni, S. M., Nazário, A. C. P., Facina, G. & Elias, S. Prevalence of Xerostomia in women during breast cancer chemotherapy. Rev. Bras. Enferm 73, (2020).
Aggarwal, P. et al. Determinants of patient-reported Xerostomia among long-term oropharyngeal cancer survivors. Cancer 127, 4470–4480 (2021).
Chang, C. et al. Oral hygiene and the overall survival of head and neck cancer patients. Cancer Med. 8, 1854–1864 (2019).
Bassan, M., Maciel, G., Marinho Maciel, R. & Linhares Ferrazzo, K. Cademartori Danesi, C. Etiopathogenesis of medication-related osteonecrosis of the jaws: a review. J. Mol. Med. 102, 353–364 (2024).
Duan, Y. et al. VEGF mitigates bisphosphonateinduced apoptosis and differentiation Inhibition of MC3T3E1 cells. Exp. Ther. Med. 23, 130 (2021).
Christodoulou, C. et al. Combination of bisphosphonates and antiangiogenic factors induces osteonecrosis of the jaw more frequently than bisphosphonates alone. Oncology 76, 209–211 (2009).
Vermeer, J. A. F., Renders, G. A. P. & Everts, V. Osteonecrosis of the Jaw—a bone Site-Specific effect of bisphosphonates. Curr. Osteoporos. Rep. 14, 219–225 (2016).
Weinstein, R. S. Glucocorticoid-induced osteonecrosis. Endocrine 41, 183–190 (2012).
Hata, H. et al. Prognosis by cancer type and incidence of Zoledronic acid–related osteonecrosis of the jaw: a single-center retrospective study. Support. Care Cancer. 30, 4505–4514 (2022).
Tiisanoja, A., Syrjälä, A. M., Anttonen, V. & Ylöstalo, P. Anticholinergic burden, oral hygiene practices, and oral hygiene status—cross-sectional findings from the Northern Finland birth cohort 1966. Clin. Oral Investig. 25, 1829–1837 (2021).
World Health Organisation (n.d.a). International Statistical Classification of Diseases and Related Health Problems (ICD). https://www.who.int/standards/classifications/classification-of-diseases
World Health Organization (n.d.b). Anatomical Therapeutic Chemical (ATC) Classification.
Acknowledgements
SK received a research grant from the Finnish Dental Society Apollonia to conduct this research.
Author information
Authors and Affiliations
Contributions
MK: Conceptualization, study design, formal analyses, interpretation and writing- original manuscript; VV: formal analyses, interpretation and writing- reviewing and editing; AT: writing- reviewing and editing; MLL: writing- reviewing and editing; GS: Conceptualization, study design, writing- reviewing and editing; SK: Conceptualization, study design, formal analyses, interpretation, writing- review and editing, and supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kujanpää, M., Vuollo, V., Tiisanoja, A. et al. Incidence of medication-related osteonecrosis of the jaw and associated antiresorptive drugs in adult Finnish population. Sci Rep 15, 17377 (2025). https://doi.org/10.1038/s41598-025-02225-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02225-2