Abstract
The Japanese government suspended its proactive recommendation for routine HPV vaccination for nine years, from June 2013 to May 2022, due to concerns about unconfirmed reports of adverse events. This study represents the fifth in our ongoing series of surveys assessing Japanese obstetricians’ and gynecologists’ attitudes toward HPV vaccination, and the first survey conducted since the recommendation was reinstated. In January 2024, we distributed a questionnaire to 632 obstetricians and gynecologists affiliated with Osaka University Hospital. The survey evaluated their attitudes toward HPV vaccination for both daughters and sons. A total of 348 specialists (55.1%) responded. After the government resumed its proactive recommendation, approximately 90% of their daughters had received or planned to receive the HPV vaccine. Among daughters eligible for catch-up vaccination, 71.4% had been vaccinated. Over 70% of respondents agreed that boys should also routinely receive HPV vaccination. Among those with sons aged 12 to 16 at the time of approval for boys, 12.5% had vaccinated them. Most respondents ensured HPV vaccination for their daughters, and some for their sons. Encouraging physicians from other specialties to do the same may help promote widespread HPV vaccine uptake in Japan.
Similar content being viewed by others
Introduction
The pro-cancerous impact of human papillomavirus (HPV) infections on cervical cancer and the protective effect of HPV vaccination are equally well known1,2. However, in June 2013, the Japanese government suspended its recommendation for its national program of routine HPV vaccination for girls. That suspension dragged on for nine years, finally ending in March 2022. The initial health concern was reports of adverse symptoms in some girls after HPV vaccination, even though numerous reports in other countries indicated that the HPV vaccine was well tolerated and highly effective3,4. Following the suspension, Japan’s vaccination rate plunged from 70% to near zero and remained under 1% during those nine years5.
In November 2021, the government announced the resumption of its recommendation for HPV vaccination, with a full proactive recommendation for the routine vaccination program officially resuming in April 2022. To compensate for nine years of negligible HPV vaccination, a catch-up vaccination program was introduced, targeting girls born between the fiscal years (FY) of 1997–2007.
In 2020, the World Health Organization (WHO) launched an ambitious strategy for cervical cancer elimination, aiming for all countries to achieve 90% HPV vaccination coverage by 20306. Although the HPV vaccination rate in Japan has slightly recovered after the government resumed its vaccine program, the rate is still far below the WHO target7. Women born in Japan in or after FY 2000, most of whom missed their vaccinations during the suspension period, face the same cervical cancer risk that women had before the HPV vaccine was introduced5. It is clear that, among developed countries, Japan is at risk of falling further behind its peers regarding the prevention of cervical cancer.
During previous surveys in this series, we found that the vaccine-eligible daughters of obstetricians and gynecologists were not receiving the vaccination as much as might be expected8,9,10,11. Since obstetricians and gynecologists are the professionals most familiar with the effectiveness of the HPV vaccine, their medical opinions should significantly influence the decisions of their patients and their mothers regarding whether their daughters should receive the vaccine. Increasing the number of vaccinated individuals might be facilitated if obstetricians and gynecologists, who are highly knowledgeable about the HPV vaccine, share their positive experiences and opinions with their patients and their families.
We conducted four HPV vaccination awareness surveys among our extended medical group’s obstetricians and gynecologists between 2014 and 2021. Our surveys revealed that our obstetricians and gynecologists have been uncharacteristically hesitant to vaccinate their daughters against HPV. We conducted our fifth and latest survey in January 2024. This is the first survey conducted after the government had fully resumed its proactive recommendation for HPV vaccination in 2022. The aim was to evaluate, as a snapshot in time, changes in the attitudes of obstetricians and gynecologists toward the HPV vaccination before and after the resumption of a proactive recommendation for HPV vaccination.
Patients and methods
Study design
We mailed our survey in January 2024 to 632 obstetricians and gynecologists affiliated with our Osaka University Hospital, with a response deadline set for March 2024. A total of 348 specialists responded. The questionnaire used was similar to those in our previous surveys conducted in 2014, 2017, 2019, and 2021, and included both closed- and open-ended questions. The target population was also the same groups as in previous surveys. We designated it as the FY 2023 Survey. All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects involved in the study. This study was approved by the ethics committee of the Osaka University Hospital.
Our survey series has been used to analyze changes in the respondent’s attitudes toward HPV vaccination, first, during the nine years the proactive recommendation was suspended, and now in the two years since it was reinstituted. We used a questionnaire similar to those used in our previous four studies, including closed and open-ended questions. Throughout, we have asked about their attitudes toward vaccination of their daughters, and we have now added questions about vaccination of their sons. As in our previous four surveys, we investigated the characteristics of the respondents and their opinions about HPV vaccination.
We have added several new questions, such as: “Did your daughter receive the catch-up vaccination, if she hadn’t received the vaccine by the age of 16?”, “Why?”, and, “Do you agree that an HPV test should be included in cervical cancer screening?”
In Japan, girls aged 12 to 16 years are eligible for HPV vaccination. Although the governmental recommendation was suspended, HPV vaccination remained part of the routine immunization program, and eligible girls were still able to receive the vaccine on a voluntary basis. The respondents’ daughters were classified into five generational groups, (1) The Preintroduction generation of women born before FY 1993, who were never eligible for subsidized vaccination; (2) The Vaccination generation of girls born between FY 1994 and FY 1999 who became eligible for subsidized routine vaccination before the government suspended its proactive recommendation of HPV vaccination; (3) The Vaccine-suspension generation, girls born between FY 2000 and FY 2005, who became age-eligible for routine HPV vaccination but did so during the period of suspended recommendation; (4) The Partial-reintroduction generation of girls born between FY 2006 and FY 2009 who became eligible for routine vaccination before or after the resumption of a proactive recommendation of HPV vaccination; and (5) The Reintroduction generation of girls born after FY 2010 who became eligible for once-again subsidized routine HPV vaccination after the resumption of the government’s proactive recommendation of HPV vaccination.
Statistical analysis
Total response counts to survey questions were determined based on the number of responses received, with incomplete answers excluded from the results for each question. In this study, we compared the characteristics of the responders and their opinions regarding HPV vaccination for boys with responses in the fourth survey using the Chi-square and Fisher’s exact probability tests. The rates of their vaccinated daughters among daughters who became eligible for vaccination after the proactive recommendation was suspended were calculated in each survey; we evaluated the trends using the Jonckheere–Terpstra trend test. The statistical significance level was set at p < 0.05. We used R software (version 4.3.3; R Core Team, 2024).
Results
Characteristics of the responders
Of the physicians mailed the survey, 348 (55.1%) responded by the March 2024 deadline. In Table 1, we summarize and compare the characteristics of the respondents of our fourth and fifth surveys. There were no significant differences in the characteristics of the respondents between these two most recent surveys.
Of the respondents, 98.3% (337/343) agreed that the government should officially recommend HPV vaccination, and 98.2% (336/342) recommended HPV vaccination for teenagers. Additionally, 74.4% (258/347) agreed that an HPV test should be included in cervical cancer screening (data not shown in the Table).
Comparison of behaviors toward the HPV vaccination
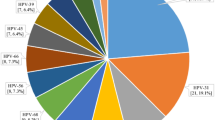
Table 2 shows the HPV vaccination status of respondents’ daughters by fiscal year of birth in the fifth survey. This table reflects the current situation of HPV vaccination as of 2024 and demonstrates generational differences in vaccination status. The vaccinations were categorized as self-paid, routine, catch-up, planned, none, or unknown. Among the respondents’ daughters born before FY 1993, who were never eligible for subsidized vaccination, 56.9% (29/51) had at some point received the vaccine through self-payment. Regarding subsidized routine vaccination, 83.3% (25/30) of girls born between FY 1994 and FY 1999, 65.6% (21/32) of those born between FY 2000 and FY 2005, and 65.2% (15/23) of those born between FY 2006 and FY 2009, were vaccinated. Among daughters born after FY 2010 - eligible following the government’s resumption of the proactive recommendation for HPV vaccination − 6.9% (8/116) have already been vaccinated, while 89.7% (104/116) said they intend to have their daughter receive the vaccination. In short, approximately 90% of the physician’s daughters had already received the HPV vaccine or were planning to receive it.
Figure 1 summarizes the HPV vaccination rate of daughters aged 12–16 years who were eligible for vaccination at each survey during the suspension-of-recommendation period, which lasted from June 2013 to May 2022. Our latest survey showed that 35 out of 55 eligible daughters (63.6%) were vaccinated during the suspension of proactive recommendations. That rate has increased statistically significantly over previous surveys (p = 0.017).
Catch-up vaccination data
Regarding catch-up vaccination, 3.3% (1/30) of girls born between FY 1994 and FY 1999, 21.9% (7/32) of those born between FY 2000 and FY 2005, and 8.7% (2/23) of those born between FY 2006 and FY 2009 were vaccinated (Table 2).
Although not shown in the table, in the fifth survey, there were 14 daughters of respondents who were eligible for catch-up vaccination, defined as those born between 1997 and 2007 who had not received routine vaccination. Of these 14 daughters, 71.4% received catch-up vaccination. The respondent’s opinions regarding catch-up vaccination are shown in Supplemental Table 1. We examined the reasons why the physicians chose to have their daughters receive or not receive the catch-up vaccination. Three respondents indicated they left the decision to their daughters, who chose not to participate (Supplemental Table 1).
The catch-up vaccination program was provided free of charge; however, after the program ended, those who wish to receive the HPV vaccine at their own expense are required to pay approximately 50,000 to 100,000 yen (about 330 to 660 USD).
Opinions on the HPV vaccination of boys
We summarized in Table 3 the changes in physicians’ opinions between the fourth and fifth surveys regarding the routine HPV vaccination of boys. The percentage of respondents who believed that boys should be vaccinated was significantly higher in the fifth survey compared to the fourth (p < 0.001). However, there was no significant difference in the percentage of respondents whose sons had been vaccinated or planned to be vaccinated, between the fourth and fifth surveys.
Although the data is not presented, in the current survey, 12.5% (4/32) of the respondents with sons aged 12 to 16 since the HPV vaccine for boys was approved had already vaccinated them. Among respondents with sons over 12, 5.9% (7/119) had completed their vaccination. Furthermore, 56.0% (56/100) of the respondents with sons under 16 indicated plans to vaccinate them.
Discussion
Over the 10 years of our follow-up survey series, including this latest one, we have gained insight into Japan’s obstetricians’ and gynecologists’ opinions on HPV vaccination. We have compared the rates of routine vaccination among the daughters of obstetricians and gynecologists across different vaccination generations, examined their opinions on catch-up vaccination, and assessed their perspectives on HPV vaccinations for boys. Most obstetricians and gynecologists now agree that HPV vaccination should be recommended for both girls and boys.
Regarding vaccination status by fiscal year of birth, the daughters of obstetricians and gynecologists have consistently had a high vaccination rate across the vaccine generations we specified. Over the oldest generation, those that were never eligible for subsidized vaccination, more than 50% of them received the vaccine through self-payment. The vaccination rate in our first survey, which was conducted just after the government suspended its proactive recommendation of the HPV vaccine, was remarkably low even among the daughters of obstetricians and gynecologists. The vaccination rate has gradually increased over the years as the effectiveness of HPV vaccination was considered to outweigh the risks of adverse events, which had been frequently reported in Japan and caused the temporary suspension of proactive recommendations.
In our fifth survey, the first to be conducted after the resumption of active recommendation, approximately 90% of daughters who were eligible for routine HPV vaccination during the period when the proactive recommendation for HPV vaccination was suspended had already received the HPV vaccine or planned to receive it (Table 2). These changes in the HPV vaccination rate among obstetricians’ and gynecologists’ daughters may indicate that both the accumulation of evidence regarding the safety and efficacy of the HPV vaccine and the government policies may influence obstetricians’ and gynecologists’ attitudes toward the HPV vaccine.
Recommendations for those eligible for catch-up vaccinations need to be further strengthened. According to this current survey, approximately 70% of the daughters received the catch-up HPV vaccination. Even in the birth cohort with the highest catch-up vaccination rate, the rate was only 35.9%12. This rate appears to be higher than that reported in the general population in Japan. However, even among the daughters of obstetricians and gynecologists who should best recognize the efficacy of the HPV vaccine, it is clear that the rate does not reach 100%.
We and others have shown that parental attitudes toward HPV vaccination greatly affected the vaccination uptake rate13,14; however, this questionnaire revealed that some daughters had opted not to receive the vaccine based on their own opinions. This indicates that it is crucial, in this new culture of increasing teen independence, to provide education about the HPV vaccine not only to parents but also to daughters. It has been reported that while social media can serve as a major source of information and a platform for discussion about HPV vaccination, the information shared is not always accurate. In addition, social media has been suggested to be a useful platform for delivering information about HPV vaccination to young people15.
In Japan, the low HPV vaccination rate among women eligible for catch-up vaccination may have allowed their HPV 16/18 infection rates to rise16. In other countries, the efficacy of catch-up vaccination in preventing HPV infection has been demonstrated17,18. Although the vaccination rate in Japan has steadily increased year by year after the resumption of proactive recommendations for the HPV vaccine, we need to accelerate this trend. The catch-up vaccination program in Japan was initially set to end in March 2025. However, there is now a growing concern that the many young women who have yet to accept the full HPV vaccine series may not do so before the March deadline, both leaving them at risk for cervical and other HPV-related cancers and acting as a reservoir for the virus. In November 2024, the government decided to extend the deadline until the end of FY 2025, provided that the first vaccination shot is administered by FY 2024. The catch-up vaccination program was provided free of charge; however, after the program ended, those who wish to receive the HPV vaccine at their own expense are required to pay approximately 50,000 to 100,000 yen (about 330 to 660 USD). To promote the catch-up program, we need to enhance public awareness and education efforts not only to parents but also to the daughters.
Most of the surveyed obstetricians and gynecologists support HPV vaccination for boys; however, the actual vaccination rate of boys and men remains considerably low. HPV-related cancers account for 8.6% of all cancer cases in women and 0.8% of all cancer cases in men19. Recently, the demand for the HPV vaccination of boys has been increasing, as early intervention in men helps prevent the transmission of HPV infection, which reduces the incidence of cervical, vaginal, and vulvar cancer in their female partners, but also reduces the incidences of HPV-linked penile cancer in men and anal and oropharyngeal cancers in both men and women20. The WHO reported that by late November 2022, 125 countries (64%) had introduced the HPV vaccine into their national immunization programs for girls; 47 countries (24%) had already included boys, and the good news is that the number is rapidly catching up to that for girls21,22.
In Japan, HPV vaccination for boys was approved in December 2020, but it is not yet a part of the national recommended and subsidized routine vaccination program. Many of our obstetricians and gynecologists recognize the importance of HPV vaccination for boys, and some of their sons, although not many, have been vaccinated. When a nationally subsidized HPV vaccination program for boys is eventually adopted by Japan, our survey finds that the sons of our obstetricians and gynecologists can be expected to be among the first to receive the vaccine. This will lead by example the way for others’ sons.
The strength of our study is that we have investigated the opinions and behaviors of obstetricians and gynecologists, leading medical specialists in fields most affected by HPV-caused diseases, regarding the HPV vaccine. This survey analysis series has covered an extended (nine-year) period during which the Japanese government suspended its proactive recommendation of the HPV vaccine and then recently (two years ago) resumed it. The respondents were the same groups who responded all along, allowing us to track changes in their opinions. To the best of our knowledge, there were no other surveys like this tracking this cohort of specialists. Each survey has had a relatively high response rate.
This study has its limitations; the targets of this survey were limited to doctors affiliated with our main Osaka University Hospital and its affiliated hospitals. We did not include doctors from unassociated specialties or a broader sample of all similar specialists elsewhere in Japan. We have been surveying this group of doctors all along on this subject, and that interaction may have affected their opinions and influenced their actions. In addition, the survey responses were entirely voluntary and so reached only 55% of those mailed the survey. The respondents may have been biased toward those more likely to have agreed with vaccination. For some questions, it remains to be determined whether the reason daughters were not vaccinated was because they did not want to be vaccinated or because they have not yet been vaccinated but plan to do so. All five surveys were anonymous, so it was not possible to identify changes in HPV vaccination intentions for each respondent.
In conclusion, most of the responding obstetricians and gynecologists agreed that HPV vaccination should be recommended, and that now includes boys and men. The rate of HPV vaccination among their daughters and sons was higher than that of the general population. Furthermore, the vaccination rate for their daughters has been accelerating since the resumption of Japan’s proactive recommendations for HPV vaccination. Because of the good examples they set for their patients, recommendations for vaccination from these obstetricians and gynecologists are highly desirable. Now that Japan has resumed its national HPV vaccination program, and with the help of these specialists, we fervently hope that we can soon match the HPV vaccine uptake rate of other developed countries.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Lei, J. et al. HPV vaccination and the risk of invasive cervical cancer. N Engl. J. Med. 383, 1340–1348 (2020).
Yoshikawa, H., Ebihara, K., Tanaka, Y. & Noda, K. Efficacy of quadrivalent human papillomavirus (types 6, 11, 16 and 18) vaccine (GARDASIL) in Japanese women aged 18–26 years. Cancer Sci. 104 (4), 465–472 (2013).
Skinner, S. R. et al. Efficacy, safety, and immunogenicity of the human papillomavirus 16/18 AS04-adjuvanted vaccine in women older than 25 years: 4-year interim follow-up of the phase 3, double-blind, randomised controlled VIVIANE study. Lancet 384, 2213–2222 (2014).
WHO. Statement on safety of HPV vaccines: Global Advisory Committee on Vaccine Safety. (2015). https://cdn.who.int/media/docs/default-source/pvg/vaccine-safety/gacvs/gacvs_hpv_statement_17dec2015.pdf?sfvrsn=6bd04fd6_1.
Nakagawa, S. et al. Corrected human papillomavirus vaccination rates for each birth fiscal year in Japan. Cancer Sci. 111(6), 2156–2162 (2020).
Gultekin, M., Ramirez, P. T., Broutet, N. & Hutubessy, R. World health organization call for action to eliminate cervical cancer globally. Int. J. Gynecol. Cancer 30, 426–427 (2020).
Yagi, A., Ueda, Y., Oka, E., Nakagawa, S. & Kimura, T. Human papillomavirus vaccination by birth fiscal year in Japan. JAMA Netw. Open. 7(7), e2422513. https://doi.org/10.1001/jamanetworkopen.2024.22513 (2024).
Egawa-Tanaka, T. et al. Human papillomavirus vaccination of the daughters of obstetricians and gynecologists in Japan. Int. Clin. Oncol. 21, 53–58 (2016).
Sawada, M. et al. HPV vaccination in Japan: Results of a 3-year follow-up survey of obstetricians and gynecologists regarding their opinions toward the vaccine. Int Clin. Oncol. 23, 121–125 (2018).
Nagase, Y. et al. Changing attitudes in Japan toward HPV vaccination: A 5-year follow-up survey of obstetricians and gynecologists regarding their current opinions about the HPV vaccine. Hum. Vaccin Immunother. 16(8), 1808–1813 (2020).
Oka, E. et al. Attitudes and behaviors of obstetricians and gynecologists toward HPV vaccination: A 7-year follow-up survey in Japan. Int. Clin. Oncol. 27, 1356–1363 (2022).
Ministry of Health. Labor and Welfare [Catch-up HPV vaccination] (in Japanese). (2024). https://www.mhlw.go.jp/content/10900000/001366510.pdf
Berenson, A. B., Laz, T. H., Hirth, J. M., McGrath, C. J. & Rahman, M. Effect of the decision-making process in the family on HPV vaccination rates among adolescents 9–17 years of age. Hum. Vaccin. Immunother. 10(7), 1807–1811 (2014).
VanWormer, J. J. et al. Association between parent attitudes and receipt of human papillomavirus vaccine in adolescents. BMC Public. Health 17(1), 766. https://doi.org/10.1186/s12889-017-4787-5 (2017).
Rebecca, R. O., Andrea, S. & Tamera, C-B. A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum. Vaccin. Immunother. 15(7–8), 1465–1475 (2019).
Sekine, M. et al. Suspension of proactive recommendations for HPV vaccination has led to a significant increase in HPV infection rates in young Japanese women: Real-world data. Lancet Reg. Health West. Pac. 16, 100300 (2021).
Silverberg, M. J. et al. Effectiveness of catch-up human papillomavirus vaccination on incident cervical neoplasia in a US health-care setting: a population-based case-control study. Lancet Child. Adolesc. Health 2(10), 707–714 (2018).
Robelj, M. et al. The impact of catch-up bivalent human papillomavirus vaccination on cervical screening outcomes: an observational study from the english HPV primary screening pilot. Br. J. Cancer 127(2), 278–287. https://doi.org/10.1038/s41416-022-01791-w (2022).
Serrano, B., Brotons, M., Bosch, F. X. & Bruni, L. Epidemiology and burden of HPV-related disease. Best Pract. Res. Clin. Obstet. Gynaecol. 47, 14–26 (2018).
Zou, K., Huang, Y. & Li, Z. Prevention and treatment of human papillomavirus in men benefits both men and women. Front. Cell. Infect. Microbiol. 12, 1077651. https://doi.org/10.3389/fcimb.2022.1077651 (2022).
WHO. Human papillomavirus vaccines: WHO position paper, December 2022. Wkly Epidemiol. Rec. 97(50), 645–672 (2022). https://www.who.int/publications/i/item/who-wer9750-645-672
Bruni, L. et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev. Med. 144, 106399 (2021).
Acknowledgements
We thank Dr. GS Buzard for his constructive critique and editing of our manuscript and the Ministry of Health, Labour, and Welfare for funding this research.
Author information
Authors and Affiliations
Contributions
M.N., E.O., A.Y., and Y. U. designed the study. M.N. wrote the initial manuscript draft and E.O. and Y.U. critically reviewed it. M.N., E.O., A.Y., and Y.U. contributed to the analysis and interpretation of the data and otherwise assisted in the preparation of the manuscript. All authors contributed to the writing and approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nakai, M., Oka, E., Ueda, Y. et al. A ninth-year follow-up survey of attitudes and behaviors of obstetricians and gynecologists toward HPV vaccination in Japan. Sci Rep 15, 18898 (2025). https://doi.org/10.1038/s41598-025-02980-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02980-2