Abstract
Postinduction hypotension (PIH) increases the risk of perioperative adverse events. This study aimed to test if low-dose esketamine could significantly decrease the incidence of PIH in elderly patients undergoing elective noncardiac surgery. This was a post hoc analysis of a randomized clinical trial in university-affiliated academic tertiary hospital. Patients (65 to 85 years, ASA physical status classification II or III) randomly received esketamine (0.2 mg/kg) or normal saline intravenous injection before general anesthesia induction. The primary outcome was the incidence of PIH. The secondary outcomes were the profiles of induction and adverse events during postinduction period. Several different definitions of hypotension and postinduction period were prespecified as the sensitivity analysis. The baseline characteristics were comparable between esketamine group (n = 211) and normal saline group (n = 213). The incidence of PIH was significantly lower in esketamine group than that in normal saline group (44.1 vs. 64.8%, P < 0.01). Esketamine pretreatment significantly decreased the consumption of propofol (P < 0.01) and the rate of vasoconstrictor utilization (P = 0.02). There were no significant differences in the incidence of postinduction adverse events between two groups (all P > 0.05). And, no other severe adverse events were observed. The sensitivity analysis displayed the robustness of the conclusion, though the effect size was lower than 0.2 under certain definition of PIH. A low dose of esketamine treatment before general anesthesia induction for elderly patients undergoing noncardiac surgery could significantly reduce the risk of PIH.
Trial registration: www.chictr.org.cn (ChiCTR2100051179); registered 15 September 2021. Date of enrolment of the first participant to the trial: 24 February 2022.
Similar content being viewed by others
Introduction
Postinduction hypotension (PIH) increases the risk of perioperative adverse events, such as myocardial injury, ischemic stroke, kidney injury, even mortality1,2,3,4. Even with the reduced doses of induction agents given with the bispectral index (BIS)-guided or age-adjusted protocol, the incidence of PIH remains worrisome in elderly patients5,6. There is a serious concern over the prevention of PIH in elderly patients.
It has been well demonstrated that anesthetics-related vasodilation and cardiac suppression, as well as hypovolaemia caused by preoperative disease, dietary abstinence and bowel preparation, contribute to the occurrence of PIH7. In clinical practices, vasoconstrictor and fluid administration have found favor in correcting or preventing PIH8. However, studies argued that vasoconstrictor might fail to prevent PIH9 and increased the risk of cerebral hypoperfusion10 and postoperative acute kidney injury11. Vasoconstrictor also exacerbated hypertension and tachycardia resulted from sympathetic activation induced by tracheal intubation12. Besides, goal-directed fluid therapy before general anesthesia (GA) induction failed to significantly decline the occurrence or degree of PIH when compared with standard fluid therapy in adult patients13. And, there were no significant differences in the incidence of PIH, cardiac arrest and death between critically ill adults with a 500 ml intravenous fluid preload or without14. These findings denote a limitation for vasopressors and fluid treatment in geriatric patients undergoing GA induction. Hence, new pharmacological strategies are still warranted.
As reported, esketamine, an S ( +) enantiomer of ketamine with approximately four times higher affinity for N-methyl-D-aspartate (NMDA) receptors than ketamine, can provide anesthesia, analgesia and sympathetic activation. There is a limited number of studies that have evaluated the clinical effects and safety of esketamine for GA induction and maintaining in adult patients15,16,17,18,19. Notably, low-dose esketamine intervention could improve intraoperative hemodynamics without severe side effects in elderly patients undergoing gastrointestinal operation20,21 or total knee arthroplasty22. Above evidences supported that esketamine might be an alternative adjuvant in GA agent regimen. While, these studies have limited external validity because of the diversity in the definition of PIH and the methodology, as well as the small sample size. Here, we conducted a secondary analysis of a randomized clinical trial to test if low-dose esketamine could significantly decrease the incidence of PIH in elderly patients undergoing elective noncardiac surgery.
Materials and methods
Design
Present study was a post hoc secondary analysis of a randomized clinical trial which was aimed to determine the diurnal variation of postoperative delirium in elderly patients undergoing esketamine anesthesia for elective noncardiac surgery. The trial was registered prior to patient enrollment at www.chictr.org.cn (No. ChiCTR2100051179, Principal investigator: Qingtao Meng, Date of registration: 15 September 2021). This manuscript adheres to the applicable CONSORT guidelines.
Ethics
Ethical approval for this study (No. WDRY2021-K124) was provided by the Institutional Review Board at Renmin Hospital of Wuhan University, Wuhan, China (Chairperson Prof Hong Chen) on 18 August 2021. All methods were carried out in accordance with relevant guidelines and regulations. Written informed consent was obtained from all subjects participating in the trial.
Patients and intervention
The primary study had been published previously23 and a complete description of the trial was presented in the supplement 1. Briefly, patients (aged 65 to 85 years, American Society of Anesthesiologists (ASA) physical status classification II or III) undergoing GA for scheduled operation were enrolled between January 4th, 2022, and March 7th, 2023. Patients were stratified with age and ASA classification, then randomly assigned in a 1:1 ratio to esketamine (0.2 mg/kg) or normal saline administration before GA induction.
GA procedures
Diuretic and angiotensin receptor blockers (ARB)/angiotensin-converting enzyme inhibitors (ACEI) were withheld on the day of surgery, and the physiological liquid requirement were given in ward as it would affect the incidence of PIH. After arriving operation room, vital signs were monitored continuously with PHILIPS medicine system (IntelliVue, 866064). Radial artery blood pressure (ABP) was monitored from either continuous noninvasive blood pressure management device (TL-400 Tensysmeter, Shanshi Medical Co Ltd.) or invasive pressure monitoring set (Pressure Transducer Kit #PX260, Edwards Lifesciences).
Before induction, a single dose of esketamine (5 mg/ml, 0.2 mg/kg, Jiangsu Hengrui Pharmaceutical Co Ltd.) or normal saline was injected intravenously according to the grouping information. Immediately, propofol (10 mg/ml) was delivered via an infusion pump at a rate of 240 ml/h to minimize the influence of injection rate. When BIS value dropped to 60 or lower, the pump was stopped immediately. Then, sufentanil (5 mcg/ml, 0.3–0.6 mcg/kg) and cisatracurium (1 mg/ml, 0.2 mg/kg) were injected sequentially as appropriate. Subsequently, patients were given oxygen by controlled mechanical ventilation or face mask. GA was maintained with inhaled sevoflurane (0.6–1.2 vol % of the expired fraction), propofol (2–4 mg/kg/h), remifentanil (4–8 mcg/kg/h) and cisatracurium (0.05 mg/kg/h).
Routinely, hypotension was treated immediately with intravenous vasoconstrictor with or without fluid therapy. Hypertension was treated with propofol or remifentanil injection. Bradycardia (heart rate (HR) ≤ 50 bpm) was treated with atropine 0.2 mg. Tachycardia (HR ≥ 110 bpm) was treated with esmolol 10 mg.
Outcomes
The primary outcome was the incidence of PIH. The secondary outcomes were defined as postinduction complications, including: hypertension, hypoxemia (SpO2 < 95%), low BIS value (< 40), arrhythmia, injection pain, and cough. The profiles of induction (type of anesthesia, type of blood pressure monitoring, anesthetics, vasoactive drugs, and airway equipment) were also recorded.
The period of postinduction was defined as 15 min after propofol initiation. Hypotension or hypertension was defined as the fluctuation of mean arterial pressure (MAP) over 20% of the baseline value (the mean of MAP measurements over 5 min before induction), respectively.
There is no unified definition for hypotension, as well as postinduction period. In practices, GA induction, mechanical ventilation and surgical incision were conducted sequentially within about 5, 10 and 15 min, respectively. We prespecified several different typical definitions of hypotension (MAP < 65 mmHg or 70% of baseline, systolic blood pressure (SBP) < 100 mmHg, 90 mmHg, 80% or 70% of baseline) and postinduction period (5 or 10 min after propofol initiation) as a sensitivity analysis to value the robustness of the conclusion.
Statistical analysis
All analyses were performed following the modified intention-to-treat (ITT) approach. Missing data would not be imputed.
Continuous variables were provided as mean (stand difference, SD) or median (inter-quartile range, IQR). Categorical variables were expressed as number (proportion). Normality of data was assessed using Shapiro–Wilk’s test. The student’s t test, nonparametric tests, χ2 test or Fisher’s exact test were employed as appropriate. A two-tailed p value less than 0.05 was judged to be statistically significant. All statistical analyses were done using SPSS version 26 (IBM, Armonk, NY, USA).
Results
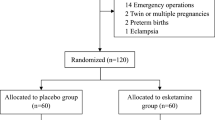
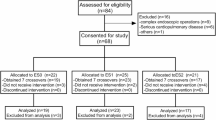
The flowchart of this study was shown in (Fig. 1). A total of 432 cases were randomized in original trail and then allocated to esketamine or normal saline group in a ratio of 1:1. Only 8 cases were excluded from analyses due to canceled operation (6 cases) or withdrew informed consent before operation (2 cases), respectively. Six cases refused to receive the study agents and 1 case received the study drug after GA induction. Finally, 211 cases in esketamine group and 213 cases in normal saline group were included in ITT analysis.
In present study, these participants were comparable with similar baseline characteristics (Table 1). The median age of the participants was 71 years. About 60% of them were male. The most common comorbidity was hypertension (66%) and calcium channel blockers (51%) were overwhelmingly used. There were no significant differences in baseline vital signs, ASA physical status, surgery type and working years of anesthesiologist.
As shown in Table 2, the incidence of PIH was significantly lower in esketamine group than that in normal saline group (44.1 vs. 64.8%, P < 0.001). The incidence risk ratio for PIH was 0.68 (95% CI 0.517, 0.891). At the 0.05 significance level, the Cramér's V-value was 0.208. There were no significant differences in the type of anesthesia and mechanical ventilation (Table 3). Esketamine pretreatment failed to significantly impact the utilization rate of 5-HT3 receptor antagonist and dexamethasone, as well as the dose of sufentanil, compared with normal saline (all P > 0.05). However, esketamine significantly decreased the consumption of propofol (P < 0.001) and the rate of vasoconstrictor utilization (P = 0.016). Besides, the incidence of postinduction adverse events, including injection pain, cough, hypertension, hypoxia, low BIS value, tachycardia and bradycardia, were similar between two groups (Table 4, all P > 0.05). We did not observe any other severe adverse events.
The sensitivity analysis based on the different definitions of PIH displayed that there was a significantly lower PIH incidence in esketamine group than that in normal saline group (Table 5, all P < 0.05). Importantly, the Cramér's V values were 0.246, 0.229, 0.261, 0.237 when defining PIH as SBP lower than 80% of baseline value during the first 15 or 10 min after propofol initiation, MAP lower than 80% of baseline value during the first 10 or 5 min after propofol initiation, respectively.
Discussion
Present study found the incidence of PIH was 54.5% in elderly patients undergoing elective noncardiac surgery. And a low dose of esketamine pretreatment effectively decreased the incidence of PIH and the risk of postinduction complications.
As reported in adult patients with treatment-resistant depression, blood pressure increase began shortly after eskeatmine administration, peaked at around 40 min with 1.1 to 1.5 times of baseline and resolved at approximately 2 h24,25. Although, the potential mechanism is rudimentary, available data suggest that subanesthetic ketamine predominantly stimulates central sympathetic nervous system, as well as directly relaxes vascular smooth muscle, resulting in the increase in heart rate, cardiac output and a relatively stable net effect on systemic vascular resistance26. Present study demonstrated that a low dose of esketamine treatment before GA induction for elderly patients undergoing noncardiac surgery significantly reduced the incidence of PIH. The sensitivity analysis based on the different definitions of PIH displayed the robustness of the conclusion, though the effect size was less than 0.2 under certain definition of PIH. Hence, current evidences support that esketamine maybe alternative in order to maintain hemodynamic stability in elderly surgical patients.
Propofol is widely adopted in GA induction due to rapid action and reliability. However, overdose utilization of propofol is common, which is positively associated with odds of PIH among elderly surgical patients8,27. Previous meta-analysis indicated that BIS-guided anesthetic delivery of total intravenous induction reduced propofol requirements when compared with manually controlled administration28. And, a lower infusion rate is associated with a lower dose requirement and a lower incidence of hypotension in elderly patients suffering propofol induction at different rates29. In present study, we employed an infusion pump to delivery induction agent under BIS monitoring to avoid excessive speed and dose. And the data showed that the induction dose of propofol in patients with or without esketamine pretreatment were consistent with the typical induction dose defined by FDA for elderly patients (1.5 mg/kg). Given that it is difficult to determine a threshold for a safe induction dose to avoid hypotension, a relatively slow delivery rate of propofol combined with BIS monitoring should be suggested to apply in aging patients.
Previous study indicated that the rate of vasopressors administration was 52% in patients aged 60 to 90 years scheduled for major noncardiac thoracic or abdominal surgeries30. In high cardiovascular risk elderly patients undergoing lumbar spine surgery with GA, 57% of them received intraoperative vasopressors intervention and more volume supplementation31. As for adult patients undergoing cerebral endovascular procedures under GA with propofol induction and maintain, the rate of vasopressors utilization was 62.0% during surgery32. Vasopressors seem have the priority in elderly patients suffering with PIH in view of the potential risk of fluid overload. In present study the rate of vasopressors administration was about 33.5%. Importantly, esketamine pretreatment significantly decreased the rate of vasopressors utilization during postinduction period, which might alleviate the risk of vasopressors-related postoperative acute kidney injury.
Usually, 5-HT3 receptor antagonists with or without dexamethasone were used to prevent and treat postoperative nausea and vomiting. However, several meta-analyses revealed that 5-HT3 receptor antagonists could prevent hypotension and bradycardia when analysing obstetric trials alone or combining obstetric and non-obstetric trials33,34, as well as reduce vasoconstrictors administration35. Besides, dexamethasone can decrease the nitric oxide (NO) production, and increase the sympathetic activity and the sensitivity of vascular endothelium to vasoconstrictors36. The role of 5-HT3 receptor antagonists and dexamethasone may be prominent in geriatric patients with high risk of PIH, which would confuse the explain of the results. Hence, present study assessed the administration of 5-HT3 receptor antagonists and dexamethasone.
In clinical practices, the decreased risk of intraoperative hypotension is associated with an anesthesiologist who has more experience. Previous studies found that the risk of hypotension after spinal anesthesia during cesarean section was increased as the working years of anesthesiologist decreased37. The working years of anesthesiologist may be a potential associated factor for PIH. Hence, we evaluated the effects of working years of anesthesiologist on PIH in present study.
Previous study found that compared with standard intermittent oscillometric upper-arm cuff monitoring, continuous invasive arterial blood pressure monitoring significantly reduced the incidence of PIH in adult patients undergoing elective noncardiac surgery with GA38. And, continuous noninvasive monitoring nearly halved the amount of intraoperative hypotension in patients older than 45 years with moderate-to-high-risk noncardiac surgery with GA39. Intriguingly, another study claimed that continuous invasive blood pressure monitoring with intra-arterial catheter detected nearly twice as much intraoperative hypotension as oscillometric brachial cuffs in adult patients undergoing elective noncardiac surgery with GA40. A reasonable explanation is that intermittent noninvasive measurements may miss acute changes in blood pressure. In present study, continuous monitoring was employed and a relatively lower PIH incidence was found in aging patients. Continuous monitoring allows timely intervention with vasopressors or fluid via tracking rapid changes in arterial blood pressure, which would presumably avoid further decline of blood pressure and hypotension occurrence. Hence, continuous monitoring of blood pressure is desirable for elderly individuals who are characterized by an inherent susceptibility and lower resilience to PIH.
We did not focus on a specific type of operation, and patients subjected to various surgical procedures carried distinct type of ventilation and incision, which might potentially skew the study findings. The other limitation was that a post hoc secondary analysis did not allow us to assess the volume supplementation during postinduction period. Besides, researches focused on the intraoperative and postoperative influences of esketamine on geriatric surgical patients were limited. Consequently, esketamine administration should be cautiously evaluated for each aging patient before validating in a multicenter study with large sample size.
Conclusion
A low dose of esketamine treatment before general anesthesia induction for elderly patients undergoing noncardiac surgery could significantly reduce the risk of PIH.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Vernooij, L. M. et al. Different methods of modelling intraoperative hypotension and their association with postoperative complications in patients undergoing non-cardiac surgery. Br. J. Anaesth. 120, 1080–1089. https://doi.org/10.1016/j.bja.2018.01.033 (2018).
Salmasi, V. et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: A retrospective cohort analysis. Anesthesiology 126, 47–65. https://doi.org/10.1097/ALN.0000000000001432 (2017).
Wickham, A. J. et al. Treatment threshold for intra-operative hypotension in clinical practice-a prospective cohort study in older patients in the UK. Anaesthesia 77, 153–163. https://doi.org/10.1111/anae.15535 (2022).
Maheshwari, K. et al. The association of hypotension during non-cardiac surgery, before and after skin incision, with postoperative acute kidney injury: a retrospective cohort analysis. Anaesthesia 73, 1223–1228. https://doi.org/10.1111/anae.14416 (2018).
Moller Petrun, A. & Kamenik, M. Bispectral index-guided induction of general anaesthesia in patients undergoing major abdominal surgery using propofol or etomidate: a double-blind, randomized, clinical trial. Br. J. Anaesth. 110, 388–396. https://doi.org/10.1093/bja/aes416 (2013).
Akhtar, S. et al. Does intravenous induction dosing among patients undergoing gastrointestinal surgical procedures follow current recommendations: a study of contemporary practice. J. Clin. Anesth. 33, 208–215. https://doi.org/10.1016/j.jclinane.2016.02.001 (2016).
de Wit, F. et al. The effect of propofol on haemodynamics: cardiac output, venous return, mean systemic filling pressure, and vascular resistances. Br. J. Anaesth. 116, 784–789. https://doi.org/10.1093/bja/aew126 (2016).
Akhtar, S., Heng, J., Dai, F., Schonberger, R. B. & Burg, M. M. A Retrospective observational study of anesthetic induction dosing practices in female elderly surgical patients: Are we overdosing older patients?. Drugs Aging 33, 737–746. https://doi.org/10.1007/s40266-016-0394-x (2016).
Gopalakrishna, M. D., Krishna, H. M. & Shenoy, U. K. The effect of ephedrine on intubating conditions and haemodynamics during rapid tracheal intubation using propofol and rocuronium. Br. J. Anaesth. 99, 191–194. https://doi.org/10.1093/bja/aem125 (2007).
Koch, K. U. et al. Cerebral macro- and microcirculation during ephedrine versus phenylephrine treatment in anesthetized brain tumor patients: A randomized clinical trial using magnetic resonance imaging. Anesthesiology 135, 788–803. https://doi.org/10.1097/ALN.0000000000003877 (2021).
Ariyarathna, D. et al. Intraoperative vasopressor use and early postoperative acute kidney injury in elderly patients undergoing elective noncardiac surgery. Ren. Fail. 44, 648–659. https://doi.org/10.1080/0886022X.2022.2061997 (2022).
Ho, A. M. & Mizubuti, G. B. Co-induction with a vasopressor “chaser” to mitigate propofol-induced hypotension when intubating critically ill/frail patients—A questionable practice. J. Crit. Care 54, 256–260. https://doi.org/10.1016/j.jcrc.2019.09.015 (2019).
Khan, A. I. et al. The impact of fluid optimisation before induction of anaesthesia on hypotension after induction. Anaesthesia 75, 634–641. https://doi.org/10.1111/anae.14984 (2020).
Russell, D. W. et al. Effect of fluid bolus administration on cardiovascular collapse among critically Ill patients undergoing tracheal intubation: A randomized clinical trial. JAMA 328, 270–279. https://doi.org/10.1001/jama.2022.9792 (2022).
Xu, C. et al. Esketamine prevents propofol-induced injection pain: Randomized controlled trial. Front. Pharmacol. 13, 991559. https://doi.org/10.3389/fphar.2022.991559 (2022).
Zhu, T. et al. Opioid-reduced anesthesia based on esketamine in gynecological day surgery: a randomized double-blind controlled study. BMC Anesthesiol. 22, 354. https://doi.org/10.1186/s12871-022-01889-x (2022).
Zhou, N. et al. S-ketamine used during anesthesia induction increases the perfusion index and mean arterial pressure after induction: A randomized, double-blind, placebo-controlled trial. Eur. J. Pharm. Sci. 179, 106312. https://doi.org/10.1016/j.ejps.2022.106312 (2022).
Fu, D., Wang, D., Li, W., Han, Y. & Jia, J. Pretreatment with low-dose esketamine for reduction of propofol injection pain: A randomized controlled trial. Pain Res. Manag. 2022, 4289905. https://doi.org/10.1155/2022/4289905 (2022).
Veith, S. B. et al. Hemodynamics and cutaneous microcirculation during induction of general anesthesia with and without esketamine. Clin. Hemorheol. Microcirc. 84, 385–398. https://doi.org/10.3233/CH-231711 (2023).
Han, C. et al. Effect of subanesthetic dose of esketamine on perioperative neurocognitive disorders in elderly undergoing gastrointestinal surgery: A randomized controlled trial. Drug Des. Dev. Ther. 17, 863–873. https://doi.org/10.2147/DDDT.S401161 (2023).
Ma, J. et al. The effect of low-dose esketamine on postoperative neurocognitive dysfunction in elderly patients undergoing general anesthesia for gastrointestinal tumors: A randomized controlled trial. Drug Des. Dev. Ther. 17, 1945–1957. https://doi.org/10.2147/DDDT.S406568 (2023).
Li, J., Wang, Z., Wang, A. & Wang, Z. Clinical effects of low-dose esketamine for anaesthesia induction in the elderly: A randomized controlled trial. J. Clin. Pharm. Ther. 47, 759–766. https://doi.org/10.1111/jcpt.13604 (2022).
Zhang, Y. et al. Diurnal variation of postoperative delirium in elderly patients undergoing esketamine anesthesia for elective noncardiac surgery: a randomized clinical trial. Int. J. Surg. 110, 5496–5504. https://doi.org/10.1097/JS9.0000000000001642 (2024).
Popova, V. et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: A randomized double-blind active-controlled study. Am. J. Psychiatr. 176, 428–438. https://doi.org/10.1176/appi.ajp.2019.19020172 (2019).
Daly, E. J. et al. Efficacy of esketamine nasal spray plus oral antidepressant treatment for relapse prevention in patients with treatment-resistant depression: A randomized clinical trial. JAMA Psychiatr. 76, 893–903. https://doi.org/10.1001/jamapsychiatry.2019.1189 (2019).
Li, L. & Vlisides, P. E. Ketamine: 50 years of modulating the mind. Front. Hum. Neurosci. 10, 612. https://doi.org/10.3389/fnhum.2016.00612 (2016).
Schonberger, R. B. et al. Association of propofol induction dose and severe pre-incision hypotension among surgical patients over age 65. J. Clin. Anesth. 80, 110846. https://doi.org/10.1016/j.jclinane.2022.110846 (2022).
Pasin, L. et al. Closed-loop delivery systems versus manually controlled administration of total IV anesthesia: A meta-analysis of randomized clinical trials. Anesth. Analg. 124, 456–464. https://doi.org/10.1213/ANE.0000000000001394 (2017).
Peacock, J. E., Lewis, R. P., Reilly, C. S. & Nimmo, W. S. Effect of different rates of infusion of propofol for induction of anaesthesia in elderly patients. Br. J. Anaesth. 65, 346–352. https://doi.org/10.1093/bja/65.3.346 (1990).
Li, Y. W. et al. Delirium in older patients after combined epidural-general anesthesia or general anesthesia for major surgery: A randomized trial. Anesthesiology 135, 218–232. https://doi.org/10.1097/ALN.0000000000003834 (2021).
Finsterwald, M. et al. Spinal versus general anesthesia for lumbar spine surgery in high risk patients: Perioperative hemodynamic stability, complications and costs. J. Clin. Anesth. 46, 3–7. https://doi.org/10.1016/j.jclinane.2018.01.004 (2018).
Zhang, J. et al. Effect of remimazolam vs propofol on emergence from general anesthesia in patients undergoing cerebral endovascular procedures: A randomized controlled, non-inferiority trial. J. Clin. Anesth. 93, 111356. https://doi.org/10.1016/j.jclinane.2023.111356 (2024).
Gao, L., Zheng, G., Han, J., Wang, Y. & Zheng, J. Effects of prophylactic ondansetron on spinal anesthesia-induced hypotension: a meta-analysis. Int. J. Obstet. Anesth. 24, 335–343. https://doi.org/10.1016/j.ijoa.2015.08.012 (2015).
Heesen, M., Klimek, M., Hoeks, S. E. & Rossaint, R. Prevention of spinal anesthesia-induced hypotension during cesarean delivery by 5-hydroxytryptamine-3 receptor antagonists: A systematic review and meta-analysis and meta-regression. Anesth. Analg. 123, 977–988. https://doi.org/10.1213/ANE.0000000000001511 (2016).
Hou, X. M., Chen, Y. J., Lai, L., Liu, K. & Shen, Q. H. Ondansetron reduces the incidence of hypotension after spinal anaesthesia: A systematic review and meta-analysis. Pharmaceuticals (Basel) https://doi.org/10.3390/ph15121588 (2022).
Sharon, L. H. O., Yi, Z. & Judith, A. W. Mechanisms of dexamethasone-induced hypertension. Curr. Hypertens. Rev. 5, 61–74. https://doi.org/10.2174/157340209787314315 (2009).
Shitemaw, T., Jemal, B., Mamo, T. & Akalu, L. Incidence and associated factors for hypotension after spinal anesthesia during cesarean section at Gandhi Memorial Hospital Addis Ababa, Ethiopia. PLoS ONE 15, e0236755. https://doi.org/10.1371/journal.pone.0236755 (2020).
Kouz, K. et al. Continuous intra-arterial versus intermittent oscillometric arterial pressure monitoring and hypotension during induction of anaesthesia: the AWAKE randomised trial. Br. J. Anaesth. 129, 478–486. https://doi.org/10.1016/j.bja.2022.06.027 (2022).
Maheshwari, K. et al. A randomized trial of continuous noninvasive blood pressure monitoring during noncardiac surgery. Anesth. Analg. 127, 424–431. https://doi.org/10.1213/ANE.0000000000003482 (2018).
Naylor, A. J. et al. Arterial catheters for early detection and treatment of hypotension during major noncardiac surgery: A randomized trial. Anesth. Analg. 131, 1540–1550. https://doi.org/10.1213/ANE.0000000000004370 (2020).
Acknowledgements
We would like to thank Dr Zhen Qiu for his assistance with the study.
Funding
National Natural Science Foundation of China, 81801085, Chen Xiao-Ping Foundation for the Development for Science and Technology of Hubei Province, CXPJJH12000005-07-28.
Author information
Authors and Affiliations
Contributions
Qingtao Meng and Zhongyuan Xia have contributed equally to this work and share senior authorship. Yuan Zhang and Qin Zhou are co-first authors and contributed equally to this work. All authors contributed to the manuscript and approved the final version. Concept and design: Zhongyuan Xia Obtained funding: Qingtao Meng and Yuan Zhang Drafting manuscript and statistical analysis: Yuan Zhang and Qin Zhou Acquisition, analysis, or interpretation of data: Rong Chen, Yuanmei Guo and Lili Chen Critical revision of the manuscript for important intellectual content: Qingtao Meng.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Y., Zhou, Q., Chen, R. et al. Effect of esketamine on postinduction hypotension in elderly patients undergoing elective noncardiac surgery: a secondary analysis of a randomized clinical trial. Sci Rep 15, 18843 (2025). https://doi.org/10.1038/s41598-025-03297-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-03297-w