Abstract
A multicenter, prospective consecutive case series study was conducted in 5 physiotherapy clinics in the UAE from January 2021 to March 2023 to assess rotations and translations of head posture parameters as potential predictors of conservative therapy outcomes in patients with chronic non-specific neck pain (CNSNP). Eighty-six patients (mean age 35 yrs., 65% male) with CNSNP underwent conservative therapy. All participants received a detailed examination including a computerized cervical spine posture analysis and demographic data was collected. Interventions included specific exercises, diathermy, longitudinal traction, education, a detailed exercise program, ergonomic advice, and medications. Interventions were applied 3 times per week for 8 weeks. Follow-up was 6-months after final treatment. A successful outcome was based on a minimum improvement of the following four outcomes using the patient centered outcome questionnaire (PCOQ): (1) reduction of pain by 17.5 points (0–100 NRS); (2) fatigue reduction by 7.5 points; (3) distress reduction by 5 points; and (4) interference reduction by 9.5 points. At 6-month follow-up it was found that success rates for pain, fatigue, distress, and interference were above 60% for the total participants. The logistic regression for predicting overall success in combined outcomes based on age, gender, smoking status, marital status, and sagittal head translation was: (1) Age: the odds ratio (0.69) suggests that as age increases, the likelihood of overall success decreases (p = 0.001); (2) Sex: females have higher odds of overall success compared to males (OR = 2.71, p < 0.001); (3) Smoking status and marital status: neither of these factors were statistically significant predictors of overall success; (4) Sagittal head translation: each unit increase (more anterior) in this abnormal posture reduced the odds of success by 13%, showing a strong and significant effect (OR = 0.13, p < 0.001). Overall, our findings indicate that younger age, female sex, and less sagittal head translation all had a statistically significant impact on the likelihood of success of 6-month outcomes in patients suffering CNSNP.
Similar content being viewed by others
Introduction
Chronic non-specific neck pain (CNSNP) is a prevalent clinical problem1,2 that significantly impacts an individual’s quality of life,3,4,5,6 leading to delayed recovery, persistent disability,1 and increased healthcare costs2,6 With a reported prevalence varying widely, CNSNP imposes a substantial financial burden on the healthcare system2,6 Although the occurrence of CNSNP increases with age, there is world-wide greater standardized prevalence rate in women (2.89%) vs. men (2%) per 100,000 cases7 Despite its high prevalence, the conservative treatment of CNSNP remains challenging8 Many patients continue to experience symptoms for extended periods, often a year or longer. Recent systematic reviews have highlighted the lack of clearly effective conservative treatments for CNSNP,8 particularly for long-term management9.
Identifying specific outcomes that predict the success of conservative treatment for CNSNP is crucial. Predictors can help tailor treatment options to individual patients, enhancing clinical care and improve long-term prognosis10 Various predictors, such as the perception of treatment outcome success,10 pain intensity,10,11 duration of complaints,12 and response to specific physical tests, have been reported previously. Importantly, the role of mechanical alignment of the cervical spine as a predictor of management outcomes has often been overlooked in clinical practice and research13 According to Harrison et al.,13 the recent focus on the bio-psycho-social model has led to an underemphasis on the ‘bio’ component, particularly biomechanics, in the treatment of spinal disorders. It is relevant that several studies indicate that the sagittal plane posture alignment and overall biomechanics of the cervical spine significantly impact patient outcomes, including pain, disability, and functional mobility14 For example, randomized controlled trials have demonstrated that interventions aimed at correcting cervical sagittal alignment, such as cervical extension traction (CET), results in better long-term health outcomes as compared to conventional treatments that do not address spinal alignment13,15,16,17,18 This evidence underscores the importance of considering biomechanical factors in developing treatment plans for spinal disorders; thus, advocating for a more balanced approach that integrates mechanical alignment with psycho-social factors to enhance patient care and outcomes.
In addition to biomechanical factors, demographic variables such as age, sex, smoking status, marital status, and body mass index (BMI) may also influence rehabilitation outcomes in individuals with CNSNP. However, these factors have received limited attention in conjunction with biomechanical predictors. Recognizing how these demographic characteristics interact with biomechanical displacements could provide a more comprehensive understanding of treatment responses and support the development of personalized rehabilitation strategies.
Recent technological advancements have enabled precise measurement and quantification of head posture in terms of translational and rotational displacements19,20 Studies have demonstrated that postural displacements, both head translations and rotations, are linked to physical fitness and cardiopulmonary functions21,22 These findings highlight the importance in evaluating and addressing postural displacements to enhance clinical outcomes. However, often, rehabilitation programs for CNSNP do not typically consider the rotations and translations of head posture displacements and thus do not include specific interventions and outcomes designed to improve these as part of a multi-modal program of care.
Accordingly, our study aims to investigate the rotations and translations of head posture displacements as predictors of conservative treatment outcomes in patients with CNSNP. Additionally, several patient demographic variables were collected as possible predictors for a complete analysis. This multicenter prospective cohort study used a 6-month follow-up to determine if the magnitude of these displacements predicts success or failure of conservative care outcomes in this patient population. We hypothesized that the magnitude of rotations and translations of head posture displacements would be predictors of the outcomes of conservative care in patients with CNSNP.
Results
Patient demographics and outcome variables
The demographic characteristics of the study participants are shown in Table 1. This was a young adult population with an average age of 35.22 years (SD = 5.93). The body mass index (BMI) distribution shows that 50% of participants had a normal BMI, 33.3% were overweight, and 16.7% were obese, highlighting a substantial portion falling into higher BMI categories. Table 2 shows the differences between males and females for each of the study variables. The sex distribution was skewed towards males (65.2%) compared to females (34.8%). Additionally, 79% of participants were non-smokers, and 67.5% were married. Posture parameters, including craniovertebral angle (CVA), sagittal head translation (SHT), coronal head translation (left and right), and lateral head angulation (left and right tilt), displayed variability among participants as depicted in the boxplot across all participants within males and females in Fig. 1. Pain, fatigue, distress, and interference were assessed at pre-treatment, post-treatment, and 6-months, showing general improvement post-treatment but variable long-term outcomes. Success rates for pain, fatigue, distress, and interference were above 60%, indicating substantial but not universal improvement. Tables 1 and 2.
When comparing demographic characteristics across sex, there was no significant difference in age, BMI, smoking status, or marital status (Table 2). Posture parameters showed no significant sex differences except for lateral head tilt, being greater in males (p = 0.03). Figure 1 shows the boxplot for the distribution of the 4 postural variables between males and females. Pain at 6-months was significantly higher in females (p = 0.04). Fatigue and distress scores did not significantly differ between sexes across any time point. Similarly, interference scores and success and failure rates for pain, fatigue, distress, and interference did not differ significantly between sexes. Table 2 presents this detailed data between males and females.
Multicollinearity among postural variables
Examining multicollinearity in regression models is important. The correlation matrix indicates high correlations among posture variables, suggesting multicollinearity as shown in Table 3. We further computed the variance inflation factor (VIF) for each of the four postural variables to quantify the extent of multicollinearity. These results revealed VIF values exceeding the standard threshold of 5 for these postural variables, confirming high multicollinearity among the postural predictors. Table 4; Fig. 2 present this VIF data. Additionally, we explored principal component analysis (PCA) to address multicollinearity by reducing dimensionality. The PCA revealed that the first principal component explained 85% of the variance, mainly influenced by SHT and CVA. However, interpreting combined components proved less clinically meaningful compared to individual variables.
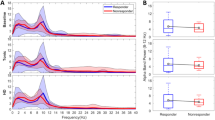
Justification for selecting sagittal head translation (SHT)
The choice of SHT as the most important postural predictor was based on both the statistical results and clinical relevance. From a statistical point of view, stepwise logistic regression continuously selected SHT as the most powerful predictor of the outcome in conservative therapy. As a result, only the SHT is used in logistic regression models to avoid multicollinearity issues. This ensures more reliable and interpretable results in the subsequent analyses. The box plots of the SHT distance in inches measured for all patients, in successful outcome patients, and in those with lack of success or failure to respond to conservative care for the combined outcome is shown in Fig. 3. This figure clearly identifies that increased SHT, measured in inches, is strongly related to those patients who failed to respond at 6-month follow-up.
Logistic regression analysis
The logistic regression result for predicting overall success is shown in Table 5. (1) Age: the odds ratio (0.69) suggests that as age increases, the likelihood of overall success decreases (p = 0.001). (2) BMI: for BMI, the odds ratio is 0.85, indicating that an increase in BMI slightly decreases the likelihood of overall success, but this effect is not statistically significant (p = 0.23). (3) Sagittal head translation: more anterior displacement of the head in the sagittal plane significantly lowers the chances of success. Each unit increase in this displacement reduces the odds of success to about 13%, showing a strong and significant effect (p < 0.001). (4) Sex: females have higher odds of overall success compared to males (OR = 2.7, p < 0.001). (5) Smoking status and marital status: neither of these factors are statistically significant predictors of overall success. See Table 5.
The logistic regression result for predicting pain success is shown in Table 6. (1) Age: the odds ratio of 0.97 suggests no significant impact of age on pain success (p = 0.53). (2) BMI: the odds ratio of 0.77 indicates no significant impact of BMI on pain success (p = 0.53). (3) Sex: shows that females have significantly higher odds of pain success compared to males, with an odds ratio of 0.27 (p = 0.03). This indicates that being female increases the likelihood of pain success. (4) Smoking and marital status: neither smoking or marital status are significant predictors of pain success (p = 0.68 and p = 0.53, respectively). (5) Sagittal head translation: greater SHT significantly reduces the odds of pain success (OR = 0.11, 95% CI: 0.04–0.31, p < 0.001).
The logistic regression result for predicting fatigue success is shown in Table 7. (1) Age: The odds ratio of 1.06 indicates that age does not have a significant impact on fatigue success (p = 0.89). (2) BMI: The negative coefficient suggests a potential inverse relationship, where an increase in BMI might be associated with lower odds of fatigue success. However, this relationship is not statistically significant (p = 0.57). (3) Sex: Sex does not have a statistically significant impact on fatigue success. Although females have 2.46 times the odds of fatigue success compared to males, this finding is not statistically significant (p = 0.24). (4) Smoking Status: Smoking status is a significant predictor of fatigue success. Smokers have 6.62 times the odds of achieving fatigue success compared to non-smokers, and this relationship is statistically significant (p = 0.037). 5. Marital Status: Based on the logistic regression results, there is no strong evidence to suggest that marital status is significantly related to fatigue success. Although the odds ratio indicates that being married might be associated with higher odds of pain success. 6) Sagittal Head Translation: Increased SHT significantly decreases the likelihood of achieving fatigue success. The odds ratio of 0.057 indicates a strong inverse relationship, and this finding is statistically significant (p < 0.001).
The logistic regression result for predicting distress is shown in Table 8. (1) Age: older participants are significantly more likely to succeed in managing distress (OR = 1.16, 95% CI: 1.031–1.324, p = 0.015). (2) BMI: higher BMI is not a significant predictor of distress success (OR = 2.87, 95% CI: 0.838–9.669, p = 0.093). (3) Sex: gender is not a significant predictor of distress success (OR = 0.33, 95% CI: 0.078–1.463, p = 0.147). (4) Smoking status: smoking status is not a significant predictor of distress success (OR = 1.35, 95% CI: 0.602–3.038, p = 0.464). (5) Marital status is not a significant predictor of distress success (OR = 0.77, 95% CI: 0.29–2.05, p = 0.60). (6) Sagittal head translation: greater SHT significantly reduces the odds of distress success (OR = 0.16, 95% CI: 0.038–0.718, p = 0.016).
The logistic regression result for predicting interference success is shown in Table 9. (1) Age: the odds ratio of 0.96 suggests no significant impact of age on interference success (p = 0.433). (2) BMI: the odds ratio of 0.66 indicates no significant impact of BMI on interference success (p = 0.321). (3) Sex: gender is marginally significant, with males less likely to succeed in managing interference compared to females (OR = 0.33, 95% CI: 0.110–1.026, p = 0.055). (4) Smoking status: smoking status is not a significant predictor of interference success (OR = 1.04, 95% CI: 0.574–1.887, p = 0.897). (5) 5) Marital status: Marital status is not a significant predictor of interference success (p = 0.67). The odds ratio of 1.16 suggests a non-significant increase in the odds of interference success for married individuals. (6) Sagittal head translation: greater SHT significantly reduces the odds of interference success (OR = 0.13, 95% CI: 0.048–0.349, p < 0.001).
Generalized estimating equation (GEE) analysis
The generalized estimating equation (GEE) result for assessing the effect of time and other predictors, including marital status, on pain scores is shown in Table 10. Consistent with previous findings, only time and SHT remain statistically significant predictors of pain scores (p < 0.001). Marital status, along with age, BMI, sex, and smoking status, does not significantly predict pain scores.
The GEE result for assessing the effect of time and other predictors, including marital status, on fatigue scores is shown in Table 11. Time and SHT remain statistically significant predictors (p < 0.001), while marital status and other variables remain non-significant.
The GEE result for distress scores, including marital status, is shown in Table 12. As with other outcomes, time and SHT remain significant predictors (p < 0.001), while marital status is not significant.
The GEE result for interference scores with the addition of marital status is shown in Table 13. Time and SHT remain significant predictors (p < 0.001), while marital status does not show a significant effect.
Discussion
The current prospective, multi-center, consecutive case series was conducted to investigate if postural displacements of the cervical spine and demographic variables might predict the successful outcome of physiotherapeutic interventions in clinical practice in patients suffering from a primary complaint of CNSNP. Our study’s primary hypothesis was that cervical spine posture displacements would be predictors of success or failure of conservative care outcomes in patients suffering from CNSNP. One of our primary findings was that the magnitude of SHT (a measure of forward head posture) significantly affected the odds of a successful outcome of conservative care. In fact, considering all four domains on the patient centered outcome questionnaire (PCOQ)23,24 simultaneously, for each unit increase in SHT distance, the odds of a successful outcome decreased by 13%. Thus, our study’s main hypothesis is confirmed by our results. Additionally, we found that younger age and female sex had substantial impacts on the likelihood of a successful outcome when considering all four domains on the PCOQ.
Negative predictors: marital status, smoking and obesity
Several demographic and socio-economic variables have been shown to predict chronicity and outcomes in CNSNP3,6,7,10,25 In the current project, we looked at several demographic variables as they relate to the odds of improving CNSNP using the four parts of the patient centered outcome questionnaire (PCOQ)23,24: pain intensity, fatigue, distress, and interference following a multi-modal conservative care program. Interestingly, we found no relationship with marital status, smoking status, and BMI and the odds of overall recovery; there is conflicting evidence on this in the chronic cervical spine pain literature. For example, studies have provided evidence supporting the notion that higher levels of perceived social support and justice correlate with decreased pain-related disability among individuals dealing with chronic pain-related psychosocial conditions but that age, sex, marital status, and pain duration were not related26 In the current project we did not account for social support (other than marital status) nor did we account for injustice and it is difficult to compare our findings of conservative care for CNSNP to those outcome investigatons that did not specifically look at CNSNP exclusively26.
In the current project, we did have a significant sample of high BMI patients (BMI > 30): where 16.7% of our sample were classified as obese (BMI > 35) and 33%, were classifed as overweight (35 > BMI > 30). The logistic regression result for predicting fatigue success on the PCOQ indicated that BMI had a negative coefficient implying a potential inverse relationship (increased BMI might be associated with lower odds of fatigue success), but this relationship was not statistically significant. In a recent systematic review of risk factors for chronic neck pain, strong evidence for high BMI in women and conflicting evidence for high BMI in men was found; however, this was not a treatment outcomes investigation so it is difficult to compare these findings with ours27 Similarly, smoking status was not a significant predictor of overall success on the total PCOQ score. However, smoking status was found to be a significant predictor of fatigue success; where smokers had 6.62 times the odds of achieving fatigue success compared to non-smokers, and this relationship is statistically significant (p = 0.037). The fatigue success increase with smokers is difficult to explain and it may be unique to our population of younger individuals. In general, though our overall finding of lack of a non-significant smoking effect on outcomes is in general agreement with systematic literature reviews where smoking is not necessarily a contributor to specific chronic neck pain but is more of a risk for low back pain and wide spread pain28,29 Based on the logistic regression results, for marital status there was no strong evidence to suggest that marital status was significantly related to pain success and this is consistent with recent investigations on CNSNP sufferers in general26.
Positive predictors: age and gender
Our logistic regression result for predicting overall success on the four parts of the PCOQ identified that participant age was a statistically significant predictor for the odds of success (OR = 0.69, p = 0.001) suggesting that older age reduced the overall success. This finding that younger age is a significant predictor of treatment success is consistent with previous investigations on chronic neck pain25,30,31 For example, the prevalence of CNSNP peaks between the ages of 45–49 years in men and 50–54 in women31.
Regarding sex differences, the results of our logistic regression analysis for predicting overall success on the four parts of the PCOQ identified that females have a higher odd of overall success compared to males for treatment improvement results when suffering CNSNP (OR = 2.7, p < 0.001). There are general conflicting findings regarding sex and the development and treatment outcomes for CNSNP25 For example, McLean et al.30 and Cote and colleagues32 have identified that women are at greater risk for the development of neck pain. Whereas Kazeminasab et al.25 reviewed the recent epidemiological studies and found no meaningful sex differences between male and females across age groups in populations with chronic neck pain. Specific to treatment outcomes for CNSNP, Chen and colleagues33 presented a systematic review and meta-analysis of RCTs analyzing the effect of scapular treatment on improving chronic neck pain incidence and found that females seemed to be better treated with scapular exercise training. The finding from Chen et al.33 is comparable with our results with women experiencing an overall greater benefit than men although we did not specifically incorporate scapular retraining exercises into our treatment regimen.
Postural predictors
Our primary finding of interest, herein, is that we identified that the sagittal head translation (SHT) significantly affected the odds of success of overall and individual outcomes on the PCOQ. Specifically, displacement of the head in the sagittal plane significantly lowers the chances of success, where each unit increase in SHT displacement reduced the odds of success by 13% (p < 0.001). Importantly, we found multicollinearity between the four potential postural displacements, i.e. that the potential postural predictors were interrelated. A statistical consequence of this is that a multivariate regression model may give non-significant results even if several of the factors are important and significant in bivariate analyses. For instance, all the postural displacements assessed herein (CVA, SHT, coronal head translation (CHT), and lateral head angulation (LHA)) are likely important predictors, but since these variables are correlated a regression model may give non-significant results for these predictors. As a matter of fact, the SHT postural predictor is directly related to the CVA postural variable as they are both attempting to measure the same postural phenomenon of forward head posture (FHP). The choice of SHT as the most important postural predictor was based on both the statistical results of VIF and PCA addressing multicollinearity and clinical relevance. From a statistical point of view, stepwise logistic regression continuously selected SHT as the most powerful predictor of the outcome in conservative therapy. Clinically, SHT directly represents FHP, which is a very common postural displacement studied in association with chronic nonspecific neck pain. The ease of SHT measurement and being a direct derivative of FHP also makes it clinically applicable. The fact that other postural predictors were not selected does not mean that they are unimportant, but they can be omitted, herein, because part of the information they contain is accounted for by the SHT displacement already included in the model.
Recent investigations have identified that imbalance of cervical spine postural alignment in both the coronal and sagittal planes negatively affects patient outcomes and is associated with increased pain, disability, altered neurophysiology, and altered cardio-pulmonary performance13,14,15,16,17,18,21,22 Specific to our regression modelling results, SHT is a very common posture abnormality and multiple recent systematic reviews and meta-analyses have been published on this postural abnormality33,34,35,36,37 From these reviews, it is clear that SHT is a significant postural abnormality related to pain, disability, and function and interventional strategies are recommended to improve identified abnormalities in patients to within normal values as found in asymptomatic populations33,34,35,36,37 Thus, our primary finding that SHT magnitude is a predictor of poor outcomes in patients undergoing treatment for CNSNP is strongly consistent with the current literature on the topic of sagittal plane head posture in varying populations.
Our investigation is the first to look at each of the four scales on the PCOQ in patients with altered posture undergoing treatment for CNSNP which adds value to the evolving literature on the topic of SHT and related outcomes. In contrast, our specific finding that SHT magnitude predicts those patients who fail a conservative care program incorporating a considerable cervical spine exercise regimen is in conflict with a recent meta-analysis review on the topic of exercise types for chronic neck pain38 Rasmussen-Barr and colleagues38 identified that there is low to high certainty of evidence for positive effects of a variety of cervical spine exercises on pain and disability used in chronic neck pain compared to no-exercise interventions. However, they found no evidence of a superior type of cervical spine exercise program, but rather all of them appear to have some beneficial effect. Our results suggest that exercise or other interventions that specifically target al.tered postural displacements, such as SHT, and specifically document their correction should show superiority in treatment outcomes of CNSNP. Preliminarily there appears to be support for this in the recent literature16,17,39 though continued investigation in the form of high-quality randomized trials is needed to further validate this finding.
Limitations and future investigations
As with all investigations, our study has limitations. Primarily, this was not a randomized controlled trial looking at the success or failure of specific treatment interventions. Thus, it is not known whether the exact type of treatment provided was optimum as it was a compilation of interventions known to aid patients suffering from CNSNP. Furthermore, because we did not specifically look at interventions that are known to improve cervical spine posture displacements, we cannot say whether improving these cervical spine postural specific variables would result in better success for patients with this suffering from CNSNP. Additionally, our investigation lacked a cervical spine motion and kinematic assessment so it is unknown how these might have influenced our outcomes. Future randomized trials are needed to investigate these limitations to determine more effective clinical intervention strategies for patients with altered cervical spine posture and CNSNP. Additionally, we recognize the importance of conducting exploratory, associative analyses to investigate how factors such as education, employment status, economic resources, health behaviors, and physical and mental health conditions may influence the association between patient education, patient expectations and management parameters.
Another source of potential bias in this study was the lack of standardization protocols among different hospitals. While our study did not aim to standardize treatment programs across multiple centers, we meticulously selected centers from a similar demographic area with similar treatment approaches to mitigate potential biases. Additionally, we have provided detailed descriptions of our rehabilitation program, thereby enhancing the credibility and reproducibility of our findings. Lastly, although SHT was determined to be the single most influential postural variable, a research effort looking beyond univariate statistics may, using higher-order multivariate analyses or machine learning, uncover interactions incorporating other posture variables. Prospective intervention studies of sagittal as well as coronal and rotational displacements are in a better position to explain further optimization in the treatment strategy for CNSNP patients.
Conclusions
In this multicenter, prospective consecutive case series conducted across 5 physiotherapy clinics in the UAE and Egypt, our findings indicate that younger age, female sex, and better cervical spine posture alignment all had a statistically significant impact on the likelihood of success of 6-month outcomes in patients suffering from chronic nonspecific neck pain (CNSNP). Non-significant (no association) predictors of patient outcomes included marital status, BMI, and smoking perhaps (except where smokers had an increase success on the fatigue scale) due to our unique sample and categorization of these patients. Importantly, a potential primary biomechanical driver of poor outcomes at 6-month follow-up after a 2-month multi-modal treatment program for CNSNP is altered sagittal head translation. Thus, future rehabilitation programs incorporating specific postural corrective approaches need to be tested for short and long-term patient relevant outcomes in patients suffering from CNSNP. Future randomized trials are needed to evaluate treatment outcomes based on correcting cervical spine posture displacements.
Materials and methods
Study design and population
This is a multicenter, prospective cohort study conducted across five physiotherapy clinics in the UAE and Egypt from January 2021 to March 2023 to assess the rotations and translations of head posture parameters as potential predictors of conservative therapy outcomes in patients with CNSNP. The protocol of the study was approved by the Ethical Review Board of the University of Sharjah (REC-21-03-11-03-S). Written informed consent was obtained from all participants and all experimental protocols were carried out following the guidelines of the World Medical Association Declaration of Helsinki. Patients with CNSNP who underwent conservative therapy as the first line of treatment were included in this prospective study. Conservative therapy included rest, physical therapy (neck exercises, diathermy therapy, and distraction (longitudinal) traction), education with instructions for home-based exercise, and medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics, muscle relaxants, or oral narcotics.
Sample size estimation
The sample size was calculated based on logistic regression analysis, considering the primary outcome of predicting conservative therapy success in patients with chronic non-specific neck pain (CNSNP). A priori power analysis was conducted using G*Power 3.1 software to detect a medium effect size (odds ratio = 1.5) with a statistical power of 80% and a significance level (α) of 0.05. Considering up to six predictor variables (age, sex, smoking status, marital status, BMI, and sagittal head translation), the minimum required sample size was calculated to be 82 participants. To account for potential dropouts or incomplete data, we recruited 86 participants, which aligns with the recommended sample size for maintaining statistical power.
Conservative therapy
Although our study, being multi-center in nature, did not intend to standardize the treatment program, we selected centers that predominantly align with a similar treatment approach. The therapeutic approach involved a comprehensive yet personalized treatment strategy. This multifaceted regimen comprises various components to alleviate pain and enhance functionality. This comprehensive conservative therapy aimed to manage CNSNP by addressing pain, functional limitations, and enhancing overall quality of life of the patients. The 8-week conservative therapy protocol for treatment of CNSNP involves a comprehensive treatment approach administered three times per week for the 8-weeks. The protocol begins with a 2-week education phase focusing on patient education, self-management, and activity modification to promote ergonomic practices and proper posture. Simultaneously, therapeutic exercises are introduced from week 1, starting with stabilization and isometric exercises. These exercises progress in intensity and complexity every two weeks, evolving into strengthening exercises targeting deep neck flexors and incorporating motor control principles. From week 3 onwards, manual therapy, including grade III posteroanterior mobilizations, is integrated and continues through week 8. Throughout the entire treatment period, modalities such as heat therapy and TENS are applied to alleviate pain and enhance treatment efficacy. Ergonomic advice emphasized from the beginning and continuously reinforced to support a neutral spine position and improve overall functionality. Each treatment session, conducted three times per week for 8 weeks, is tailored to ensure patient comfort and progress, with modifications made as needed based on individual responses.
Conservative treatment modalities
Education and self-management
-
Patient Education: Informing patients about the nature of their condition, the importance of maintaining good posture, and ergonomic adjustments can empower them to manage their symptoms better.
-
Activity Modification: Advising on modifying daily activities to avoid exacerbating movements and encourage the adoption of ergonomic practices at work and home.
Therapeutic exercises
-
Stabilization Exercises: These exercises aim to improve the control and endurance of the deep cervical flexors and extensors, which can help in reducing pain and preventing recurrence. The protocol for stabilization exercises was adapted from Shin et al.40 It consisted of a 30-minute exercise session, preceded by a 5-minute warm up, and followed by a 5-minute cool down. The warmup and cool down phases included general stretching of the upper extremity and neck. The main exercise session included:
-
Supine isometrics of deep neck flexors.
-
1.
Patient instructions: in supine, the patient is instructed to tuck their chin as if nodding, without lifting their head and holding the position.
-
1.
-
-
Sitting cervical multidirectional isometrics (flexion, extension, lateral flexion, rotation).
-
1.
Patient instructions: while sitting, the therapist applies gentle resistance on the front, back, and side of the head. The patient is then instructed to push against the resistance without moving their neck and hold the position.
-
1.
-
Sitting upper extremity movement exercises.
-
1.
Patient instructions: while sitting, the patient is instructed to preform shoulder shrugs (bring shoulder towards ears), arm flexion (keep your elbow straight and raise your arm straight ahead), and arm abduction (keep your elbow straight and raise your arm out to the side).
-
1.
-
Sitting cervical resistive exercises with Thera-band.
-
1.
Patient instructions: the therapist places the Thera-band around the patients head in different direction to allow resistance to flexion, extension, side flexion, and rotation. The patient is instructed to push against the band and move in the intended direction in a controlled manner.
-
1.
-
Strengthening Exercises: Progressive resistance exercises for the neck and shoulder muscles can enhance overall muscular support for the cervical spine. Therefore, strengthening exercises were incorporated in this intervention program mainly targeting deep neck flexor muscles. The exercises were based on principles of motor control as described by Domingues et al.41 in their randomized controlled trial. The program consisted of three phases:
-
Phase one: This phase targeted activation of deep flexors in the upper cervical region, specifically the longus capitis and colli. Patients were instructed to perform cranio-cervical flexion (chin tuck- bring chin in, as if nodding) in supine position, with a pressure cuff placed behind their neck. This position was held for 10 s and repeated 10 times. Successfully completing 10 repetitions at 26 mmHg permits the transfer to the second phase.
-
Phase two: This phase continues the previous exercises in loading positions such as sitting and quadruped / 4-point kneeling, while maintaining a neutral cervical spine. Additionally, the pressure level was increased to 28 and 30 mmHg.
-
Phase three: This phase begins with the chin tucks and is progressed with a higher load by adding 15 repetitions of shoulder flexion and head lifts in supine position.
-
Exercise prescription.
-
The previously mentioned volumes and intensity were the foundation of exercise prescription for all patients. However, individual modifications were made when required to ensure prescription was suitable for each patient and they remained pain-free.
-
-
Stretching Exercises: Regular stretching of the cervical muscles, especially the upper trapezius, levator scapulae, scalenes, and sternocleidomastoid, can help alleviate tightness and improve range of motion (ROM). Therefore, stretches were incorporated in this intervention plan where participants performed 3 sets of stretches with a 15 s hold42.
-
Manual therapy
-
Mobilization Techniques: Gentle, repetitive movements were applied to the cervical spine to enhance joint mobility and reduce pain.
-
Protocol: The manual therapy protocol used in this study was adopted from a randomized controlled trial by Lopez-Lopez et al.43 Initially, the patient is instructed to lie prone with hands under their forehead. The therapist stands at the patient’s head and places their thumbs over the spinous process of the targeted vertebra. The vertebra that is selected for mobilization is the one that is identified as symptomatic and hypomobile. Then, the therapist applies a grade III posteroanterior (PA) oscillatory force at the frequency of 2 Hz. This is carried on for 3 sets, each lasting 2 min, with a 1-minute rest interval between sets.
Modalities
-
Heat Therapy: Application of heat can relax tight muscles and improve blood flow.
-
Electrotherapy: Techniques such as transcutaneous electrical nerve stimulation (TENS) provide pain relief by modulating the pain signals sent to the brain. This method was added to the intervention plan for pain relief as it is effective in the treatment of CNSNP. All participants in this study received TENS therapy as a standard component of the 8-week multimodal conservative treatment program, regardless of their baseline pain levels. TENS was administered using four electrodes placed over painful areas on the neck and shoulder region. A standardized “cross pattern” electrode configuration was utilized for all participants. This technique was consistently applied over the upper trapezius and cervical paraspinal regions bilaterally, ensuring coverage of the largest possible area involved in pain perception and muscle tension. Moreover, although electrode placement was adapted to individual anatomical landmarks to ensure precision and comfort, the standardized cross configuration minimizes variability and allows for reproducibility across sessions and participants. The stimulation was delivered at a frequency of 80 Hz and an intensity of 10 mA to 30 mA, for 25 min44.
Ergonomic adjustments
Recommendations for workplace adjustments, such as chair height, monitor position, and keyboard placement, can help maintain a neutral spine position.
Outcome variables
Several patient demographic variables were collected and evaluated as possible predictors of overall outcomes of treatment and included: age, body mass index (BMI categorized as normal (18.5–24.9), overweight (25–29), and obese (30–35)), sex, smoking status, and marital status. The primary outcome variable used in this study was the conservative treatment outcome after a 6-month follow-up after completion of active interventions (defined as success or failure). In this study, the success criteria were defined from the spine pain patient’s perspective across multiple relevant domains using the patient centered outcome questionnaire (PCOQ)23 This questionnaire instructs the patient to rate their current level of pain, fatigue, distress, and interference of daily activities on a numerical rating scale (NRS), ranging from 0 to 100 (see appendix 1 in Zeppieri and George23. The patient then repeats the rating in the second section of the questionnaire, but instead of rating current levels, they rate levels of the four domains they expect to achieve following the physical therapy intervention. This allows for the assessment of the patients’ presentation, expectation, and goals, and quantifies the impact these four domains have on the patient’s health, as well as how the intervention will affect them.
The following four endpoints were considered because previous research has shown them to be clinically relevant with good reliability and concurrent validity: reduction of pain, reduction of fatigue, reduction of distress, and reduction of interference24 The rehabilitation program was considered successful if the 4 domain outcomes were decreased at discharge time by the optimal cutoff points according to Brown et al.,24 and this improvement was maintained or further improved at the 6-month follow up, otherwise it was considered as a failure. The optimal cutoff points were: (1) reduction of pain of 17.5 points or more (0–100 numerical rating scale); (2) fatigue reduction of 7.5 points or more; (3) reduction for distress by 5 points or more; and (4) reduction of interference by 9.5 points or more. The criteria for the 6-month follow-up failure were singularly defined as improvement in the 4 components of the PCOQ by less than the optimal cutoff points expressed above24.
In addition to singular successful outcomes on each of the 4 PCOQ components, we used a combined treatment outcome that was classified as successful only if the participant achieved the predefined threshold for improvement in all four domains measured by the PCOQ: a reduction of ≥ 17.5 points in pain, ≥ 7.5 points in fatigue, ≥ 5 points in distress, and ≥ 9.5 points in interference. Failure to meet the threshold in any one of these domains was considered a failure for the combined outcome. This strict criterion ensures that treatment success reflects a comprehensive improvement in the patient’s overall condition rather than isolated progress in a single domain.
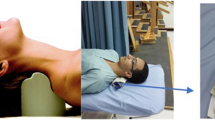
Rotations and translations of head posture parameters
The rotations and translations of head posture displacements were measured using a standardized protocol. The patient was instructed to stand with feet shoulder width apart in their natural posture and look straight ahead. Posture measurement was achieved by the PostureScreen® Mobile app (PSM) which is a digital posturographic assessment tool used to perform 3D postural examinations. The PSM has been established in research as a reliable and valid method for evaluating static posture. For example, investigations have identified that PSM has an intra-rater reliability that ranges from 0.71 to 0.99, and an inter-rater reliability which is good to excellent for all translations (ICC’s between 0.85 and 0.98)19,20 PSM captures images of the participant from four directions: anterior and posterior (coronal plane) and the left and right sides (sagittal plane). After the photograph is captured, specific anatomical reference points are digitized by the user such as the pelvic iliac spines, the greater trochanter, the femoral condyle, and the tragus. To ensure maximum accuracy of the manual digitization of landmarks, participants were instructed to undress/wear clothing that exposes the landmarks required so that they could be identified and labelled prior to digitization. Moreover, the landmarks were digitized by the same research team member and then cross-checked by the same 2 members to ensure accuracy for all participants’ data. The PSM then calculates specific body angles and distances based on the anatomical digitization and creates an output file containing values of posture displacements and images of the participant that can be used to compare and analyze the postural displacements from neutral among participants.
The following postural displacements were assessed using the PSM app:
-
(1)
The cranio-vertebral angle (CVA (°)) is the acute angle that is formed between a straight line that connects the spinous process of C7 to the tragus of the ear, and the horizontal line that passes through the spinous process of C7. The angle is identified by the intersection of those two lines45 See Fig. 4.
-
(2)
Sagittal head translation, which is the displacement of the head (tragus of the ear) anteriorly relative to the center of the glenohumeral joint. See Fig. 4.
-
(3)
Coronal head translation (CHT) or left and right head translation, is the displacement of the cervical spine and head laterally to either side. Figure 5 depicts this measurement.
-
(4)
Lateral head angulation (LHA) or coronal plane side bending displacement of the head towards either side. The PSM app allows LHA to be assessed in either the anterior or posterior view. Figure 6 depicts this measurement.
Two measurements of forward head posture. (1) The craniovertebral angle (CVA°) is measured using two landmarks: the tragus of the ear and the C7 spinous process (marked in yellow). A line (marked in red) is then extended horizontally from the C7 spinous process, and another connects the C7 to the tragus; this intersection creates the CVA. (2) Sagittal head translation (SHT) in inches. A vertical line is constructed at the center of the glenohumeral joint and the horizontal offset of the tragus of the ear is measured as the SHT in inches. Image created using DAZ3d studio version 4.22.0.16 (https://www.daz3d.com/introducing-genesis-9).
Coronal head translation (CHT) left and right measured in inches. CHT can be assessed in anterior and posterior views in the PSM app. The figure above shows the CHT (marked in red) of the head from the true vertical plumbline (marked in black). Image created using DAZ3d studio version 4.22.0.16 (https://www.daz3d.com/introducing-genesis-9).
Lateral head angulation (LHA°) to the left and right (coronal plane bending) can be assessed in either the anterior and posterior views. The figure above shows the LHA (marked in red) of the head from the true vertical plumbline. Image created using DAZ3d studio version 4.22.0.16 (https://www.daz3d.com/introducing-genesis-9).
Data analysis
The descriptive statistics utilized in our investigation included count and percentages to describe categorical data. The Shapiro-Wilk test was used to test the normality of the numerical variables. Based on this, we report the median and interquartile ranges (IQR) to describe numerical data since all the numerical data, such as age, head posture parameters, and the scores of the four study outcomes, were not normally distributed. Multiple logistic regression models were used to assess the predictors of the success of each of the four domains of the PCOQ outcomes as well as the four outcomes combined into one variable. In case of multicollinearity of the four postural variables we analyzed the variance inflation factor (VIF) and we explored principal component analysis (PCA) to address multicollinearity by reducing dimensionality. Generalized estimation equations (GEE) were developed to assess the effect of time on pain, fatigue, distress, and interference scores, as well as the effect of other potential predictors.
While logistic regression addressed the dichotomous classification of success or failure, it could not capture how continuous outcome measures (pain, fatigue, distress, and interference scores) changed over time throughout the study. To address this, we employed GEE for the following reasons: (1) Since the participants’ outcome scores were collected at multiple time points (pre-treatment, post-treatment, and at a 6-month follow-up) GEE accounts for the within-participant correlations inherent in longitudinal data, providing accurate and reliable parameter estimates. (2) Logistic regression only provides a snapshot of predictors related to the final binary outcome of success or failure. In contrast, GEE offers a more granular analysis by illustrating how predictors affected continuous outcomes across the entire study duration. This dual approach enriches our understanding of the treatment effects. SPSS version 25.0 for Windows (IBM, Armonk, NY, USA) was used for data analysis.
Data availability
Data is available upon reasonable request from the corresponding author.
References
Price, J., Rushton, A., Tyros, V. & Heneghan, N. R. Expert consensus on the importance of chronic Non-Specific neck pain motor control and segmental exercise and dosage variables: an international e-Delphi study. PLoS One. 16, e0253523. https://doi.org/10.1371/journal.pone.0253523 (2021).
Raizah, A. et al. A Cross-Sectional study on mediating effect of chronic pain on the relationship between cervical proprioception and functional balance in elderly individuals with chronic neck pain: mediation analysis study. J. Clin. Med. 12, 3140. https://doi.org/10.3390/jcm12093140 (2023).
Chen, Z., Falla, D., Elgueta Cancino, E. & Deane, A. Can baseline features predict a reduction in pain and disability following neck-Specific exercise in people with chronic Non-Specific neck pain? A systematic review and Meta-Analysis protocol. BMJ Open. 13, e074494. https://doi.org/10.1136/bmjopen-2023-074494 (2023).
Côté, P. et al. Management of neck pain and associated disorders: A clinical practice guideline from the Ontario protocol for traffic injury management (OPTIMa) collaboration. Eur. Spine J. 25, 2000–2022. https://doi.org/10.1007/s00586-016-4467-7 (2016).
Cerezo-Téllez, E. et al. Health related quality of life improvement in chronic Non-Specific neck pain: secondary analysis from a single blinded, randomized clinical trial. Health Qual. Life Outcomes. 16, 207. https://doi.org/10.1186/s12955-018-1032-6 (2018).
Park, S. J. et al. Factors associated with increased risk for pain catastrophizing in patients with chronic neck pain. Medicine 95, e4698. https://doi.org/10.1097/MD.0000000000004698 (2016).
GBD 2021 Neck Pain Collaborators. Global, regional, and National burden of neck pain, 1990–2020, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. Mar;6 (3), e142–e155. https://doi.org/10.1016/S2665-9913(23)00321-1 (2024).
de Zoete, R. M. J. Exercise therapy for chronic neck pain: tailoring Person-Centered approaches within contemporary management. J. Clin. Med. 12, 7108. https://doi.org/10.3390/jcm12227108 (2023).
Cheng, C. H., Su, H. T., Yen, L. W., Liu, W. Y. & Cheng, H. Y. K. Long-Term effects of therapeutic exercise on nonspecific chronic neck pain: A literature review. J. Phys. Ther. Sci. 27, 1271–1276. https://doi.org/10.1589/jpts.27.1271 (2015).
Groeneweg, R. et al. J.G. Treatment success in neck pain: the added predictive value of psychosocial variables in addition to clinical variables. Scand. J. Pain. 14, 44–52. https://doi.org/10.1016/j.sjpain.2016.10.003 (2017).
Fernández-Carnero, J. et al. Prediction of patient satisfaction after treatment of chronic neck pain with Mulligan’s mobilization. Life 13, 48. https://doi.org/10.3390/life13010048 (2022).
Guillén, D. et al. Limited prognostic value of pain duration in Non-specific neck pain patients seeking chiropractic care. Eur. J. Pain. 26, 1333–1342. https://doi.org/10.1002/ejp.1954 (2022).
Harrison, D. E., Oakley, P. A. & Moustafa, I. M. Don’t throw the ‘bio’ out of the Bio-Psycho-Social model: editorial for spine rehabilitation in 2022 and beyond. J. Clin. Med. 12, 5602. https://doi.org/10.3390/jcm12175602 (2023).
Abdalatef, N. & Diab, A. A. Cervical sagittal balance as a predictor for the outcome of multimodal treatment program for Non specific neck pain. Med. J. Cairo Univ. 87, 4651–4659. https://doi.org/10.21608/mjcu.2019.80827 (2019).
Moustafa, I. M., Diab, A. A., Hegazy, F. & Harrison, D. E. Demonstration of central conduction time and neuroplastic changes after cervical lordosis rehabilitation in asymptomatic subjects: A randomized, Placebo-Controlled trial. Sci. Rep. 11, 15379. https://doi.org/10.1038/s41598-021-94548-z (2021).
Moustafa, I. M., Diab, A. A., Hegazy, F. & Harrison, D. E. Does improvement towards a normal cervical sagittal configuration aid in the management of cervical myofascial pain syndrome: a 1- year randomized controlled trial. BMC Musculoskelet. Disord. 19 (1), 396. https://doi.org/10.1186/s12891-018-2317-y (2018).
Suwaidi, A. S. A., Moustafa, I. M., Kim, M., Oakley, P. A. & Harrison, D. E. A comparison of two forward head posture corrective approaches in elderly with chronic Non-Specific neck pain: A randomized controlled study. J. Clin. Med. 12 (2), 542. https://doi.org/10.3390/jcm12020542 (2023).
Moustafa, I. M. et al. Utilizing machine learning to predict post-treatment outcomes in chronic non-specific neck pain patients undergoing cervical extension traction. Sci. Rep. 14 (1), 11781. https://doi.org/10.1038/s41598-024-62812-7 (2024).
Boland, D. M., Neufeld, E. V., Ruddell, J., Dolezal, B. A. & Cooper, C. B. Inter- and Intra-Rater agreement of static posture analysis using a mobile application. J. Phys. Ther. Sci. 28, 3398–3402. https://doi.org/10.1589/jpts.28.3398 (2016).
Szucs, K. A. & Brown, E. V. D. Rater reliability and construct validity of a mobile application for posture analysis. J. Phys. Ther. Sci. 30, 31–36. https://doi.org/10.1589/jpts.30.31 (2018).
Tamim, M., Moustafa, I. M., Alaparthi, G. K., Oakley, P. A. & Harrison, D. E. Translational and rotational postural aberrations are related to pulmonary functions and Skill-Related physical fitness components in collegiate athletes. J. Clin. Med. 12, 4618. https://doi.org/10.3390/jcm12144618 (2023).
Moustafa, I., Kim, M. & Harrison, D. E. Comparison of sensorimotor integration and Skill-Related physical fitness components between college athletes with and without forward head posture. J. Sport Rehabil. 32, 53–62. https://doi.org/10.1123/jsr.2022-0094 (2023).
Zeppieri, G., George, S. Z., Patient-Defined Desired & Outcome Success criteria, and expectation in outpatient physical therapy: A longitudinal assessment. Health Qual. Life Outcomes 15 https://doi.org/10.1186/s12955-017-0604-1 (2017).
Brown, J. L. et al. Defining Patient-Centered, multidimensional success criteria for treatment of chronic spine pain. Pain Med. 9, 851–862. https://doi.org/10.1111/j.1526-4637.2007.00357.x (2008).
Kazeminasab, S. et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet. Disord. 23 (1), 26. https://doi.org/10.1186/s12891-021-04957-4 (2022).
Martínez-Borba, V., Ripoll-Server, P., Yakobov, E. & Suso-Ribera, C. Predicting the physical and mental health status of individuals with chronic musculoskeletal pain from a biopsychosocial perspective: A multivariate approach. Clin. J. Pain. 37 (3), 211–218. https://doi.org/10.1097/AJP.0000000000000913 (2021).
Manderlier, A., de Fooz, M., Patris, S. & Berquin, A. Modifiable lifestyle-related prognostic factors for the onset of chronic spinal pain: A systematic review of longitudinal studies. Ann. Phys. Rehabil Med. 65 (6), 101660. https://doi.org/10.1016/j.rehab.2022.101660 (2022).
Mansfield, M., Thacker, M., Spahr, N. & Smith, T. Factors associated with physical activity participation in adults with chronic cervical spine pain: a systematic review. Physiotherapy 104 (1), 54–60. https://doi.org/10.1016/j.physio.2017.01.004 (2018).
Dai, Y. et al. Association of cigarette smoking with risk of chronic musculoskeletal pain: A Meta-Analysis. Pain Physician. 24 (8), 495–506 (2021). PMID: 34793634.
McLean, S. M., May, S., Klaber-Moffett, J., Sharp, D. M. & Gardiner, E. Risk factors for the onset of non-specific neck pain: a systematic review. J. Epidemiol. Community Health. 64 (7), 565–572. https://doi.org/10.1136/jech.2009.090720 (2010).
Safiri, S. et al. Global, regional, and National burden of neck pain in the general population, 1990–2017: systematic analysis of the global burden of disease study 2017. BMJ 368, m791. https://doi.org/10.1136/bmj.m791 (2020).
Côté, P., Cassidy, D. J., Carroll, L. J. & Kristman, V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain 112 (3), 267–273. https://doi.org/10.1016/j.pain.2004.09.004 (2004).
Chen, Y. et al. Effects of scapular treatment on chronic neck pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet. Disord. 25 (1), 252. https://doi.org/10.1186/s12891-024-07220-8 (2024).
Yang, S., Boudier-Revéret, M., Yi, Y. G., Hong, K. Y. & Chang, M. C. Treatment of chronic neck pain in patients with forward head posture: A systematic narrative review. Healthc. (Basel). 11 (19), 2604. https://doi.org/10.3390/healthcare11192604 (2023).
Chaudhuri, S., Chawla, J. K. & Phadke, V. Physiotherapeutic interventions for upper cross syndrome: A systematic review and Meta-Analysis. Cureus 15 (9), e45471. https://doi.org/10.7759/cureus (2023).
Rani, B., Paul, A., Chauhan, A., Pradhan, P. & Dhillon, M. S. Is neck pain related to sagittal head and neck posture?? A systematic review and Meta-analysis. Indian J. Orthop. 57 (3), 371–403. https://doi.org/10.1007/s43465-023-00820-x (2023).
Mahmoud, N. F., Hassan, K. A., Abdelmajeed, S. F., Moustafa, I. M. & Silva, A. G. The relationship between forward head posture and neck pain: a systematic review and Meta-Analysis. Curr. Rev. Musculoskelet. Med. 12 (4), 562–577. https://doi.org/10.1007/s12178-019-09594-y (2019).
Rasmussen-Barr, E. et al. Summarizing the effects of different exercise types in chronic neck pain - a systematic review and meta-analysis of systematic reviews. BMC Musculoskelet. Disord. 24 (1), 806. https://doi.org/10.1186/s12891-023-06930-9 (2023).
Comparison of pressure biofeedback unit and mirror imaging technique in craniovertebral angle, pain, and strength of deep cervical flexors among collegiate students with forward head posture. Yugato 76 (1), 1-16. (2024).
Shin, H. J., Kim, S. H., Hahm, S. C. & Cho, H. Y. Thermotherapy plus neck stabilization exercise for chronic nonspecific neck pain in elderly: A single-blinded randomized controlled trial. Int. J. Environ. Res. Public Health 17 https://doi.org/10.3390/ijerph17155572 (2020).
Domingues, L. et al. Is a combined programme of manual therapy and exercise more effective than usual care in patients with Non-Specific chronic neck pain?? A randomized controlled trial. Clin. Rehabil. 33, 1908–1918. https://doi.org/10.1177/0269215519876675 (2019).
Demir, O., Atıcı, E. & Torlak, M. S. Therapeutic and stabilization exercises after manual therapy in patients with Non-Specific chronic neck pain: A randomised clinical trial. Int. J. Osteopath. Med. 47, 100639. https://doi.org/10.1016/j.ijosm.2022.10.001 (2023).
Lopez-Lopez, A. et al. Mobilization versus manipulations versus sustain apophyseal natural glide techniques and interaction with psychological factors for patients with chronic neck pain: randomized controlled trial. Eur. J. Phys. Rehabil Med. 51, 121–132 (2015).
Yesil, H., Hepguler, S., Dundar, U., Taravati, S. & Isleten, B. Does the use of electrotherapies increase the effectiveness of neck stabilization exercises for improving pain, disability, mood, and quality of life in chronic neck pain?? Spine (Phila Pa. 1976). 43, E1174–E1183. https://doi.org/10.1097/BRS.0000000000002663 (2018).
Singla, D., Veqar, Z. & Hussain, M. E. Photogrammetric assessment of upper body posture using postural angles: A literature review. J. Chiropr. Med. 16 (2), 131–138. https://doi.org/10.1016/j.jcm.2017.01.005 (2017).
Acknowledgements
Authors would like to thank CBP NonProfit, Inc. and the Foundation for the Advancement of Chiropractic Tenets and Science (FACTS) for partial funding of this manuscript.
Author information
Authors and Affiliations
Contributions
Authors G.A., I.M.M., A.Ah., A.Al. and D.E.H. all participated in the conception and design. G.A., I.M.M., A.Ah., A.Al. each participated in study implementation and data collection. G.A., I.M.M., A.Ah., A.Al., D.E.H. contributed to the statistical analysis and interpretation. I.M.M., A.Ah., A.Al. participated in supervision. G.A., I.M.M., A.Ah., A.Al. and D.E.H. all contributed to the interpretation of the results and wrote the drafts. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
DEH is the CEO of Chiropractic BioPhysics and lectures on rehabilitation methods, and distributes products for patient rehabilitation to physicians in the USA; none of these products were used in this manuscript. All the other authors declare that they have no competing interests. All the other authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Anwar, G., Moustafa, I.M., Ahbouch, A. et al. The magnitude of sagittal head posture displacement and patient demographics predict rehabilitation outcomes in patients with chronic nonspecific neck pain. Sci Rep 15, 18986 (2025). https://doi.org/10.1038/s41598-025-04187-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04187-x