Abstract
To evaluate whether the Spring Festival has an effect on the outcomes of patients undergoing their first embryo transfer (ET) via in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI). We conducted a retrospective cohort study involving 11,625 first ET cycles were performed at a university-affiliated hospital between January 2014 and March 2022. Women who underwent ET during the peri-Spring Festival periods were designated as the Festival Group, while the remainder were categorized as the Non-Festival Group. Multivariate logistic regression and propensity score matching (PSM) were applied to assess the impact of the “Spring Festival Effect” on pregnancy outcomes. Prior to PSM, patients in Festival Group had lower clinical pregnancy rate (44.39% vs. 52.50%, P < 0.001), implantation rate (34.41% vs. 40.43%, P < 0.001), ongoing pregnancy rate (38.71% vs. 47.15%, P < 0.001), and live birth rate (37.33% vs. 44.82%, P < 0.001). After controlling for confounders, a similar trend remained in the PSM analysis with matching ratios ranging from 1:1 to 1:4. In the multivariable regression analysis, the Spring Festival was found to be an independent risk factor for poor prognosis. These findings indicated that sociocultural events, represented by the Spring Festival, decreased the chances of IVF/ICSI success, underscoring the importance for clinicians and patients to be more vigilant with healthcare during major social events.
Similar content being viewed by others
Introduction
The increasing prevalence of infertility among reproductive-aged couples worldwide has been driven by rapid societal development, lifestyle changes, and environmental shifts, with China reporting a notable rise from 12.0 to 18.0% from 2007 to 20201.Since the first infant was conceived with assisted reproductive technology (ART) in 1978, more than 5 million babies have been born through in vitro fertilization and embryo transfer (IVF-ET) around the world2. There were over 500 assisted reproductive centers in mainland China by the end of 2019, and the number of ART cycles exceeded 1 million in 2016 and reached 1.15 million in 20173. ART has become increasingly mature, with implantation rates ranging from less than 5.0% per embryo transferred initially to more than 50.0% currently4. The overall success rate of ART in China reflects a clinical pregnancy rate of 30.0% and a live birth rate of 28.8%, aligning closely with international levels3. Nevertheless, UK statistics revealed that the birth rate per embryo transferred for all IVF patients was only 23% in 20185. Therefore, various factors that may negatively affect success rates are gradually being identified, and researchers are exploring approaches to improve ART outcomes.
The routine procedures of IVF-ET involve controlled ovarian stimulation (COS), oocyte retrieval and sperm collection, IVF to form embryos, and embryo transfer (ET). Given this, the quality of oocyte, sperm, embryo, and the endometrium is essential for the success of ART. Moreover, aspects such as emotional well-being6,7stress8physical activity9,10and even sleep quality11also have implications for pregnancy outcomes, in addition to the abovementioned biological concerns. Beyond the intrinsic factors of the infertile couples, external environmental factors, including temperature, light duration and seasonal variation were the most studied12,13,14. Specifically, a significant correlation was found between monthly fertilization rates and the Δ (increase/decrease) in light hours12. Sperm concentration was significantly lower in autumn and fast motility was lower in summer than in the other seasons, suggesting seasonal variation15.
In contrast to the well-documented effects of natural environmental variation, the potential impact of socio-cultural influences, ranging from beliefs and values to customs and traditions, has been largely overlooked. The Spring Festival is the most significant traditional festival in China and an integral part of Chinese cultural heritage. This annual celebration usually occurs in early February, with preparations and festivities often spanning several weeks before and after the event. Deeply embedded in the daily lives of Chinese people, the festival provides a unique context for exploring how external sociocultural factors may influence human health. On the one hand, during the festival, individuals may transition abruptly from their regular routines to indulgent behaviors, such as overeating, excessive alcohol consumption, disrupted sleep schedules, and heightened emotional states. Type 1 diabetes mellitus (T1DM) patients undergoing multiple daily insulin injections exhibited poorer glycemic control during the Spring Festival compared to those using continuous subcutaneous insulin infusion, suggesting that reduced self-management during the holiday period may negatively impact health16. On the other hand, limited medical resources and delays in seeking care might be responsible for high mortality during the festival17.
This study sheds light on how socio-cultural events may influence ART outcomes. We hypothesized that both patients and reproductive specialists might be influenced by the festival atmosphere during the Spring Festival, potentially affecting the success of ART. We conducted a retrospective analysis of infertile women who underwent their first ET at our reproductive medicine center between 2014 and 2022. Pregnancy outcomes were compared between those who underwent ET during the “peri-Spring Festival” period and those who underwent the procedure outside of this timeframe.
Materials and methods
Ethical approval
This study was a retrospective analysis approved by the ethical committee of Xiangya Hospital of Central South University (CSU) (No. 2022011), and was in accordance with the Helsinki Declaration.
Data source and study population
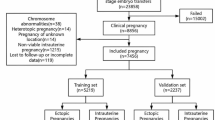
In this population-based retrospective cohort study, clinical records of 16,121 couples who underwent their first ET between January 1, 2014 and March 1, 2022 at the Reproductive Medicine Center of Xiangya Hospital, CSU, were initially screened. The study design and the inclusion/exclusion criteria are described in Fig. 1. Women aged 20–40 years with a body mass index (BMI) of 18.5–28.0 kg/m2 were included. Patients with endometrial abnormalities such as endometrial polyps, endometrial hyperplasia, submucosal fibroids, severe intrauterine adhesions or untreated chronic endometritis were excluded. Patients with hypertension, diabetes, chronic kidney disease, autoimmune disorders or other systemic diseases were also excluded. After applying the inclusion and exclusion criteria, 11,625 patients were included in the final analysis.
The cohort was subdivided into two groups based on the date of ET. The term “peri-Spring Festival” refers to the period spanning three weeks prior to Chinese New Year’s Eve (i.e., Laba Festival) and two weeks after the Lantern Festival. Patients who underwent ETs during the “peri-Spring Festival” period were assigned to the Festival Group, while the remaining cases were designated as the Non-Festival Group.
Demographic data collection included maternal age, BMI, educational level, family residence, occupational status, occupational exposure, infertility duration, type of infertility, gravidity, parity, main indication for ART, anti-Mullerian hormone (AMH) levels, thyroid-stimulating hormone (TSH), serum lipids (triglyceride, total cholesterol, low-density lipoprotein, high-density lipoprotein), fasting blood glucose, fasting insulin, basal antral follicle count (AFC), and basal reproductive hormone levels such as follicle stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2) and testosterone (T).
Cycle-specific variables were also collected, including the type of cycle (fresh and frozen-thawed), method of fertilization [IVF, intracytoplasmic sperm injection (ICSI) and IVF + ICSI], date of ET, endometrial thickness and morphological type measured on the day of ovulation trigger for fresh cycles and on the day of endometrial preparation for frozen-thawed cycles. Embryonic data, such as the stage of embryo development (cleavage or blastocyst), the number and grade of embryos transferred, were collected. In addition, the clinician’s title and gender who performed ET were recorded.
Clinical management of fresh and frozen ET cycles
For the fresh ET cycle, the standard protocols for COS included the GnRH agonist long protocol (using either short-acting or long-acting preparations), ultra-long protocol, short protocol, and the GnRH antagonist protocol, as described previously18,19. Briefly, in the GnRH agonist protocol, COS was initiated once sufficient down-regulation of the pituitary was achieved (serum E2 level < 50 pg/ml and a maximum follicle diameter < 10 mm with no ovarian cysts). In the GnRH short protocol and GnRH antagonist protocol, COS was initiated on day 2 or day 3 or the menstrual cycle. The initial dose of exogenous gonadotropins (Gn) ranged from 112.5 to 300.0 IU/day, depending on the individuals’ body weight and ovarian reserve. The Gn dosage was then adjusted based on follicular development assessed by transvaginal ultrasonography and serum E2 levels. When the follicles reached a size indicating maturity (dominant follicles ≥ 18 mm in diameter), human chorionic gonadotrophin (hCG) or a GnRH agonist was used to simulate the LH surge and trigger final oocyte maturation. Oocytes were usually retrieved 36 h after triggering and fertilized by IVF or ICSI 4–6 h after retrieval. Fresh embryos were transferred on day 3 or day 5 after fertilization.
For frozen-thawed embryo transfer (FET) cycles, various protocols were used for endometrial preparation at our center, including natural cycles (also encompassing stimulated natural cycles), hormone replacement therapy (HRT) cycles, and GnRH agonist + HRT cycles. Among these, natural and HRT cycles were the most commonly applied20,21. Natural FET cycles were recommended for women with regular ovulatory menstrual cycles, and ovulation was monitored by transvaginal ultrasonography starting from day 10 of the menstrual cycle until follicular rupture. For HRT cycles, estradiol valerate was initiated on day 3 of the menstrual cycle and continued for at least 12 days. Progesterone was added to induce endometrial transformation when the endometrial thickness exceeded 7 mm. In natural FET cycles, cleavage-stage embryos or blastocysts were transferred on day 3 or day 5 after ovulation, respectively. In HRT cycles, embryos were transferred on the corresponding days after the initiation of progesterone supplementation.
Vaginal micronized progesterone (Utrogestan; Besins-Iscovesco Pharmaceuticals, Paris, France) at 600 mg/day and oral progesterone capsules (Qining; Aisheng, Hangzhou, China) at 200 mg/day were administrated for luteal support. Serum hCG levels were measured 12 days after ET, and transvaginal ultrasound was conducted 28 days after transfer to confirm clinical pregnancy.
Pregnancy outcomes
The primary outcomes included clinical pregnancy rate and live birth rate. Clinical pregnancy refers to the number of patients with intrauterine pregnancy per ET cycle. Live birth was defined as the delivery of any viable neonate who was 28 weeks of gestation or older.
The secondary outcome were positive hCG rate, biochemical pregnancy rate, implantation rate (IR), ectopic pregnancy rate, early miscarriage rate, late miscarriage rate, ongoing pregnancy rate, preterm birth rate and term birth rate. We defined a positive pregnancy test as β-hCG > 10IU/L. Biochemical pregnancy was defined as a very early spontaneous abortion after a positive pregnancy had been determined and with a fall in serum β-hCG concentration before the ultrasonic detection of gestational sacs. IR refers to the number of gestational sacs observed divided by the number of embryos transferred. Ectopic pregnancy was defined as any extrauterine implantation, including heterotopic pregnancies.
Ongoing pregnancy was defined as a sustained pregnancy beyond 12 weeks of gestation. Early miscarriage was classified as occurring before 12 weeks, while late miscarriage was defined as occurring between 12 and 28 weeks. Preterm birth was defined as the delivery between 28 weeks and less than 37 weeks of gestation. Term birth was defined as delivery at 37 weeks of gestation or beyond.
Statistical analysis
All statistical analyses were performed using SPSS (version 25.0) and R (version 4.3.3). The Kolmogorov–Smirnov test was used to assess the normality of continuous variables. If the data followed a normal distribution, they were expressed as mean ± standard deviation (SD); otherwise, they were described as median and interquartile range (IQR; 25th and 75th percentiles). Categorical variables were presented as frequencies (n) and percentages (%).
For comparison between the two groups, the independent t-test and Wilcoxon rank-sum test were used to determine significance for continuous variables as appropriate, and Pearson’s chi-square test was conducted to evaluate differences in categorical variables. Unadjusted and adjusted odds ratios (ORs) with 95% confidence intervals (CIs) were reported for reproductive outcomes.
To minimize potential baseline differences and reduce selection bias between the Festival Group and Non-Festival Group, a propensity score matching (PSM) analysis was performed using the MatchIt package in R based on the methodological and reporting guidelines proposed by Yao et al.22. Matched outcomes were analyzed and presented in accordance with these guidelines.
Propensity scores were estimated via logistic regression using covariates that were selected with the aim of achieving adequate matching with minimal model complexity. Specifically, variables that showed significant differences between groups in the unmatched cohort (based on independent t-tests or chi-square tests), as well as those deemed clinically relevant based on prior knowledge or expert opinion, were incorporated into the model (see Supplementary Table 1 for details). No missing values existed in the covariates for propensity score estimation.
Nearest-neighbor matching without replacement was performed using four different matching ratios: 1:1, 1:2, 1:3, and 1:4, with a caliper width of 0.02 on the logit of the propensity score. Baseline characteristics between the matched groups were compared to assess the quality of the match. Standardized mean differences (SMDs) were calculated for all covariates after matching, with an SMD < 0.1 considered indicative of adequate balance.
Prior to multivariate analysis, univariate logistic regression was performed for each outcome variable to identify potential covariates (see Supplementary Tables 3–6). Binary logistic regression models were then applied to evaluate the independent effect of the Spring Festival period on positive β-hCG, intrauterine pregnancy, ongoing pregnancy, and live birth, respectively. For example, for the outcome of positive β-hCG, the model was adjusted for maternal age at embryo transfer, education level, current career status, duration of infertility, type of infertility, main indication for ART, basal FSH, basal LH, fertilization method, endometrial thickness, endometrial type, stage of embryo development and number of embryos transferred. Statistical significance was assigned to two-sided P values below 0.05 (p < 0.05).
Results
Characteristics of the study population before PSM and after PSM
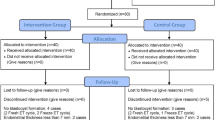
A total of 16,121 first ET cycles were performed from January 1 2014 to March 1 2022, of which 11,625 cycles (corresponding to 11,625 patients) met the inclusion criteria and were included in the final analysis (Fig. 1). We conducted 1:1, 1:2, 1:3, and 1:4 PSM analyses; in this part, only the results from the 1:4 matching are presented, while results from other matching ratios are provided in Supplementary Tables 1 and 2. The Festival group consisted of 874 participants before matching and 860 participants after PSM. The Non-Festival group comprised 10,751 patients before matching and 3,354 after PSM. The demographics and clinical parameters before and after matching are summarized in Table 1.
Before PSM, the Festival Group had a lower BMI, a higher proportion of women with a college education or above, a greater proportion residing in Changsha City, and more patients who were employed compared to the Non-Festival Group (P < 0.05 for all). Additionally, the Festival Group exhibited a shorter mean duration of infertility, lower proportion of tubal factor infertility as the main indication for ART, lower fasting insulin levels, and fewer cycles involving fresh ET. All of these differences reached statistical significance (P < 0.05). The Festival Group also showed a lower proportion of patients with type A endometrium and a higher proportion with type B endometrium (P = 0.011). Additionally, more blastocyst-stage embryos were transferred in the Festival group compared to the Non-Festival group (13.27% vs. 8.73%, P < 0.001). The mean number of embryos transferred per cycle was slightly lower (1.73 ± 0.44 vs. 1.80 ± 0.40, P < 0.001), and the rate of good-quality embryo transfer was significantly lower (88.84% vs. 92.10%, P < 0.001). Other parameters including maternal age at ET, occupational exposure, type of infertility, gravidity, parity, AMH, reproductive hormones, AFC, TSH, serum lipids, fasting blood glucose, fertilization method, endometrial thickness, clinician’s title and clinician’s gender were comparable between the two groups (P > 0.05).
We performed a 1:4 PSM based on maternal age, BMI, duration of infertility, endometrial type, number and quality of embryos transferred, main indication for ART, type of cycle, stage of embryo development, and the title and gender of the embryo transfer physician. After 1:4 PSM, 860 participants remained in the Festival Group and 3,354 in the Non-Festival Group. Except for AMH (SMD = 0.104, P = 0.309), all other covariates had SMDs < 0.1 and P > 0.05 after matching, indicating adequate balance between groups. In addition, the baseline characteristics after 1:1 to 1:3 PSM, which effectively balanced the differences in confounding factors between the two groups, are presented in Supplementary Table 1.
Clinical outcomes of participants before and after PSM
Among the full cohort, both clinical pregnancy and live birth rate were significantly lower in the Festival Group than in the Non-Festival Group (clinical pregnancy: 44.39% vs. 52.50%; live birth: 37.33% vs. 44.82%; P < 0.001 for both comparisons, Table 2). Among secondary outcomes, the Festival Group also showed significantly lower positive β-hCG rate (55.03% vs. 62.56%), implantation rate (34.41% vs. 40.43%), ongoing pregnancy rate (38.71% vs. 47.15%) and term birth rate (29.72% vs. 35.94%) (all P < 0.001). There were no significant differences in biochemical pregnancy rate, ectopic pregnancy rate, miscarriage rate (including early and late miscarriage), preterm birth rate and the proportion of missing transfer outcomes (all P > 0.05).
After 1:4 PSM, the clinical pregnancy rate (44.53% vs. 50.98%, P = 0.001), live birth rate (37.50% vs. 44.20%, P < 0.001), positive β-hCG rate (55.12% vs. 61.87%, P < 0.001), implantation rate (34.49% vs. 40.00%, P < 0.001), ongoing pregnancy rate (38.90% vs. 46.00%, P < 0.001) and term birth rate (29.90% vs. 35.00%, P = 0.005) were significantly lower in the Festival Group compared to the Non-Festival Group. A similar trend was observed in the 1:1 to 1:3 PSM analyses (Supplementary Table 2).
Effects of “Spring Festival” period on reproductive outcomes after first ET
To investigate whether ET during the Spring Festival period independently affects reproductive outcomes, we conducted binary logistic regression analysis for key reproductive endpoints. After adjusting for relevant confounders (see Supplementary Tables 3–6 for details), ET during the Spring Festival remained significantly associated with worse outcomes, including reduced rates of positive β-hCG (adjusted OR 0.729, 95% CI: 0.631–0.841), clinical pregnancy (adjusted OR 0.717, 95% CI: 0.622–0.827), ongoing pregnancy (adjusted OR 0.708, 95% CI: 0.612–0.819), and live birth (adjusted OR 0.731, 95% CI: 0.631–0.847) (Table 3). The adjusted ORs suggest that undergoing ET during the Spring Festival period is associated with a 27–29% decrease in the likelihood of successful reproductive outcomes. Notably, the specific covariates included in each model differed by outcome and are detailed in Supplementary Tables 3–6.
Evaluating the impact of other holidays on ET outcomes
To investigate whether other national holidays exert similar effects on first ET outcomes as the Spring Festival, we compared baseline characteristics and pregnancy outcomes between transfers performed during the National Day of the People’s Republic of China (October 1 to October 7) versus Non-National Day periods, and the International Workers’ Day (i.e., Labour Day, May 1 to May 5) versus Non-Labour Day periods.
As shown in Supplementary Tables 7, 196 cycles involved ETs during the National Day period, compared to 11,429 cycles performed during Non-National Day periods. Baseline comparisons revealed statistically significant differences in patients’ fasting blood glucose levels and the title of the clinicians performing ET between the two groups (P = 0.037 and P = 0.024, respectively), while no other baseline characteristics showed significant differences (all P > 0.05). Regarding clinical outcomes, no statistically significant differences were observed between the two groups, except for a notably lower preterm birth rate in the National Day Group (3.59% vs. 8.96%, P = 0.009) (see Supplementary Table 8).
Similarly, among the entire study population, 108 cycles involved ETs during the Labour Day, while 11,517 cycles were performed outside this period. Baseline comparisons between the two groups revealed statistically significant differences in gravidity, AMH levels, cycle type, good-quality embryos transferred rate, and the gender of the ET physician (see Supplementary Table 7). However, no statistically significant differences were observed in clinical outcomes, including clinical pregnancy rate, positive β-hCG rate, implantation rate, miscarriage rate, and live birth rate (all P > 0.05) (see Supplementary Table 8).
To assess whether embryo transfers during the National Day holiday influence pregnancy outcomes, we conducted multivariate logistic regression analyses for various reproductive endpoints. After adjusting for potential confounders, the National Day period was significantly associated with a reduced risk of preterm birth (adjusted OR 0.375, 95% CI: 0.175–0.802, Supplementary Fig. 1d), while no significant associations were observed for other outcomes. As shown in Supplementary Fig. 2, after adjusting for relevant confounders, embryo transfer during the Labour Day period was not significantly associated with any pregnancy outcome, including β-hCG positivity, clinical pregnancy, ongoing pregnancy, or live birth.
Discussion
Our study focused on the impact of socio-cultural events on the pregnancy outcomes of IVF women undergoing their initial ET procedures. Both PSM and traditional multivariable-adjusted regression analysis confirmed a statistically significant and robust association between the “Spring Festival Effect” and reproductive outcomes. This large study reveals an intriguing phenomenon: patients undergoing ET during the “peri-Spring Festival” have less favorable clinical outcomes compared to those treated on Non-Spring Festival days, which suggests that socio-cultural events may influence ART outcomes.
In previous studies, the emphasis has been primarily on the impact of the endometrium and the embryo on assisted reproductive outcomes23. However, our study introduces an alternative perspective: external factors may exert a negative influence on the pregnancy outcomes of ART. In this study, we examined a multitude of social factors, including the educational level, occupational status, and residential location of patients, that could potentially influence the outcomes of ART. It has been shown that educational level is a significant factor in access to health care outcomes24,25. In our data, the population that experienced ET during the Spring Festival period had slightly higher education levels than those who underwent ET at other times. However, this difference was no longer present after PSM. A retrospective analysis conducted in China indicated that a mother’s educational attainment did not correlate with the probability of a successful live birth among patients undergoing either fresh or FET procedures26.
Our study also revealed that a higher percentage of employed patients opted for treatment during the Spring Festival compared to other periods. These findings indicate that, driven by their occupational status, working individuals prefer to utilize the extended holiday to undergo ART procedures. Moreover, an observational study reported that women who lived within 15 km of a fertility clinic were 21% more likely to undergo ART treatment than those who lived over 60 km away27. In our clinical center, the proportion of patients residing in Changsha undergoing IVF during the Spring Festival was greater than that during the non-festival periods. This suggests that a combination of geographical and holiday-related factors could potentially serve as confounding influences on women’s access to ART treatments.
To mitigate the impact of potential confounding bias as much as possible, we employed both PSM and multivariate logistic regression analysis to assess the impact of the “Spring Festival Effect” on pregnancy outcomes. We observed several interesting findings regarding the influence of socio-cultural factors on ART outcomes. In alignment with our observations, another fertility center in China has also reported that the live birth rate among patients who underwent ART during the Spring Festival period was statistically lower compared to those who underwent ET outside of this festive season28. In contrast to our results, a meta-analysis of prospective psychosocial studies demonstrated that emotional stress induced by fertility problems and life events does not compromise the chance of becoming pregnant29. This discrepancy may be attributed to the fact that the “festival effect” causes disturbances to both patients and doctors, rather than disturbing patients alone.
Furthermore, our analysis indicated that neither the National Day nor the Labour Day appeared to have a significant impact on the clinical outcomes of patients undergoing their first ET, with the exception of a reduced preterm birth rate observed during the National Day. These findings may be partially attributed to the relatively small sample size. Nevertheless, it also suggests that the Spring Festival, as the most significant traditional holiday in China, holds a more profound influence on daily life and behavior, including those of ART patients undergoing their first ET.
Several possible mechanisms may help explain why the Spring Festival could lead to unfavorable outcomes of ART. From the patients’ perspective, poor lifestyle habits during the festival (e.g., sleep deprivation, poor sleep quality, irregular diet, and binge eating) may negatively affect IVF/ICSI outcomes. A prospective study suggested that unhealthy sleep characteristics such as short nocturnal sleep, inappropriate sleep time, poor subjective sleep quality might impair occyte quantity, maturity, and fertilization, and reduce the chances of clinical pregnancy30. In addition, patients may find it difficult to strictly follow medication instructions under the holiday atmosphere. A population-based retrospective cohort study found that patients discharged during the December holiday period were less inclined to have timely outpatient follow-up and had a higher risk of readmission and death. This suggested that patients affected by the holiday period were more likely to deviate from medical orders, leading to adverse outcomes31.
From the clinician’s point of view, physicians’ attention might be distracted by festival events such as discussions on holiday-related topics, visits, and gift preparations, etc. An observational study comparing patients’ mortality after surgery on surgeons’ birthdays with that on other days showed higher postoperative mortality on surgeon’s birthday32. On the basis of these findings, it is possible that doctors may be distracted by life events unrelated to work, which may adversely affect patient prognosis.
Strengths and limitations
The strengths of this study include its sufficient sample size and the use of PSM to minimize bias as much as possible. Good covariate balance was achieved in all baseline characteristics after PSM. We evaluated a new candidate factor influencing ART outcome from a novel perspective, which is often underestimated but has clinical guiding significance.
Despite these strengths, this study has several limitations. First, in view of the intrinsic property of this retrospective study, potential confounding factors cannot be excluded. After matching, the Non-Festival group was reduced from 10,751 to 3,354 cases, with a matching ratio of 31.2%, which indicates incomplete matching and may have introduced bias. However, the Festival group retained 98.4% of samples, indicating that nearly all samples in the Festival group were successfully matched. Hence, the results should be interpreted with caution. Second, while we identified an association between the Spring Festival effect and adverse pregnancy outcomes, we did not further explore the specific contributing factors. In the future, prospective questionnaire-based studies are warranted to investigate potential influences on ART outcomes during the Spring Festival.
Conclusion
In conclusion, we demonstrated that sociocultural events, as exemplified by the Spring Festival, were associated with poor prognoses for patients undergoing IVF/ICSI. The clinical significance of this study underscores the need for clinicians to remain vigilant in patient care during major social events. Meanwhile, under the cheerful holiday atmosphere, patients should exercise stronger self-discipline to maintain healthy lifestyle habits that support favorable ART outcome.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AFC:
-
Antral follicle count
- AMH:
-
Anti-Müllerian hormone
- ART:
-
Assisted reproductive technology
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- DOR:
-
Diminished ovarian reserve
- E2:
-
Estradiol
- ET:
-
Embryo transfer
- FBG:
-
Fasting blood glucose
- FET:
-
Frozen-thawed embryo transfer
- FINS:
-
Fasting insulin
- FSH:
-
Follicle stimulating hormone
- Gn:
-
Gonadotrophin
- GnRH:
-
Gonadotrophin-releasing hormone
- hCG:
-
Human chorionic gonadotropin
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostatic model assessment for insulin resistance
- HRT:
-
Hormone replacement therapy
- ICSI:
-
Intracytoplasmic sperm injection
- IVF-ET:
-
In vitro fertilization and embryo transfer
- IQR:
-
Interquartile range
- LDL-C:
-
Low-density lipoprotein cholesterol
- LH:
-
Luteinizing hormone
- OR:
-
Odds ratio
- P4:
-
Progesterone
- PSM:
-
Propensity score matching
- RSA:
-
Recurrent spontaneous abortion
- SD:
-
Standard deviation
- SMD:
-
Standardized mean differences
- T:
-
Testosterone
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- TSH:
-
Thyroid-stimulating hormone
References
Feng, J., Wu, Q., Liang, Y., Liang, Y. & Bin, Q. Epidemiological characteristics of infertility, 1990–2021, and 15-year forecasts: an analysis based on the global burden of disease study 2021. Reprod. Health. 22, 26. https://doi.org/10.1186/s12978-025-01966-7 (2025).
Sandin, S., Nygren, K. G., Iliadou, A., Hultman, C. M. & Reichenberg, A. Autism and mental retardation among offspring born after in vitro fertilization. Jama 310, 75–84. https://doi.org/10.1001/jama.2013.7222 (2013).
Qiao, J. et al. A lancet commission on 70 years of women’s reproductive, maternal, newborn, child, and adolescent health in China. Lancet 397, 2497–2536. https://doi.org/10.1016/s0140-6736(20)32708-2 (2021).
Niederberger, C. et al. Forty years of IVF. Fertil. Steril. 110, 185–324e185. https://doi.org/10.1016/j.fertnstert.2018.06.005 (2018).
Statistics, U. Fertility treatment 2018: trends and figures. Report No. 978 92 4 006831 5, (UK fertility regulator). https://www.hfea.gov.uk/about-us/publications/research-and-data/fertility-treatment-2018-trends-and-figures (2020).
Lang, J. et al. First trimester depression and/or anxiety disorders increase the risk of low birthweight in IVF offspring: a prospective cohort study. Reprod. Biomed. Online. 39, 947–954. https://doi.org/10.1016/j.rbmo.2019.09.002 (2019).
Nik Hazlina, N. H., Norhayati, M. N. & Bahari, S. Nik Muhammad arif, N. A. Worldwide prevalence, risk factors and psychological impact of infertility among women: a systematic review and meta-analysis. BMJ Open. 12, e057132. https://doi.org/10.1136/bmjopen-2021-057132 (2022).
Zhou, F. J., Cai, Y. N. & Dong, Y. Z. Stress increases the risk of pregnancy failure in couples undergoing IVF. Stress 22, 414–420. https://doi.org/10.1080/10253890.2019.1584181 (2019).
Rao, M., Zeng, Z. & Tang, L. Maternal physical activity before IVF/ICSI cycles improves clinical pregnancy rate and live birth rate: a systematic review and meta-analysis. Reprod. Biol. Endocrinol. 16, 11. https://doi.org/10.1186/s12958-018-0328-z (2018).
Palomba, S. et al. Physical activity before IVF and ICSI cycles in infertile obese women: an observational cohort study. Reprod. Biomed. Online. 29, 72–79. https://doi.org/10.1016/j.rbmo.2014.03.006 (2014).
Philipsen, M. T. et al. Sleep, psychological distress, and clinical pregnancy outcome in women and their partners undergoing in vitro or intracytoplasmic sperm injection fertility treatment. Sleep. Health. 8, 242–248. https://doi.org/10.1016/j.sleh.2021.10.011 (2022).
Rojansky, N. et al. Seasonal variability in fertilization and embryo quality rates in women undergoing IVF. Fertil. Steril. 74, 476–481. https://doi.org/10.1016/s0015-0282(00)00669-5 (2000).
Wang, W. W. & Gunderson, A. R. The physiological and evolutionary ecology of sperm thermal performance. Front. Physiol. 13, 754830. https://doi.org/10.3389/fphys.2022.754830 (2022).
Gindes, L. et al. Pregnancy rate fluctuations during routine work in an assisted reproduction technology unit. Hum. Reprod. 18, 2485–2488. https://doi.org/10.1093/humrep/deg455 (2003).
Levitas, E., Lunenfeld, E., Weisz, N., Friger, M. & Har-Vardi, I. Seasonal variations of human sperm cells among 6455 semen samples: a plausible explanation of a seasonal birth pattern. Am. J. Obstet. Gynecol. 208, 406e401–406e406. https://doi.org/10.1016/j.ajog.2013.02.010 (2013).
Guo, K. et al. Effect of the Chinese new year public holiday on the glycemic control of T1DM with intensive insulin therapy. Front. Endocrinol. (Lausanne). 13, 915482. https://doi.org/10.3389/fendo.2022.915482 (2022).
He, G. et al. The spring festival is associated with increased mortality risk in china: A study based on 285 Chinese locations. Front. Med. (Lausanne). 9, 761060. https://doi.org/10.3389/fmed.2022.761060 (2022).
Yang, T. et al. Homeostatic model assessment for insulin resistance is associated with late miscarriage in Non-Dyslipidemic women undergoing fresh IVF/ICSI embryo transfer. Front. Endocrinol. (Lausanne). 13, 880518. https://doi.org/10.3389/fendo.2022.880518 (2022).
Hou, Z. et al. Value of endometrial echo pattern transformation after hCG trigger in predicting IVF pregnancy outcome: a prospective cohort study. Reprod. Biol. Endocrinol. 17 https://doi.org/10.1186/s12958-019-0516-5 (2019).
Jing, Z. et al. Oestrogen dose tapering during luteal phase does not affect clinical outcomes after hormone replacement treatment-frozen-thawed embryo transfer cycles: a retrospective analysis. Hum. Reprod. 34, 1479–1484. https://doi.org/10.1093/humrep/dez096 (2019).
He, A. et al. The role of transcriptomic biomarkers of endometrial receptivity in personalized embryo transfer for patients with repeated implantation failure. J. Transl Med. 19, 176. https://doi.org/10.1186/s12967-021-02837-y (2021).
Yao, X. I. et al. Reporting and guidelines in propensity score analysis: A systematic review of cancer and cancer surgical studies. J. Natl. Cancer Inst. 109 https://doi.org/10.1093/jnci/djw323 (2017).
Hernández-Vargas, P., Muñoz, M. & Domínguez, F. Identifying biomarkers for predicting successful embryo implantation: applying single to multi-OMICs to improve reproductive outcomes. Hum. Reprod. Update. 26, 264–301. https://doi.org/10.1093/humupd/dmz042 (2020).
Graf, G. H. J. et al. Educational mobility, Pace of aging, and lifespan among participants in the Framingham heart study. JAMA Netw. Open. 7, e240655. https://doi.org/10.1001/jamanetworkopen.2024.0655 (2024).
Lan, G. et al. Association and mediation between educational attainment and respiratory diseases: a Mendelian randomization study. Respir Res. 25, 115. https://doi.org/10.1186/s12931-024-02722-4 (2024).
Liu, X., Shi, J., Mol, B. W. & Bai, H. Impact of maternal education level on live birth rate after in vitro fertilization in china: a retrospective cohort study. J. Assist. Reprod. Genet. 38, 3077–3082. https://doi.org/10.1007/s10815-021-02345-4 (2021).
Lazzari, E., Baffour, B. & Chambers, G. M. Residential proximity to a fertility clinic is independently associated with likelihood of women having ART and IUI treatment. Hum. Reprod. 37, 2662–2671. https://doi.org/10.1093/humrep/deac205 (2022).
Zhai, J., Zhang, J., He, J., Li, G. & Hao, G. Declined live birth rate from in vitro fertilization fresh cycles performed during Chinese new year holiday season. Risk Manag Healthc. Policy. 16, 1703–1718. https://doi.org/10.2147/rmhp.S422969 (2023).
Boivin, J., Griffiths, E. & Venetis, C. A. Emotional distress in infertile women and failure of assisted reproductive technologies: meta-analysis of prospective psychosocial studies. Bmj 342, d223. https://doi.org/10.1136/bmj.d223 (2011).
Yao, Q. Y. et al. Associations of sleep characteristics with outcomes of IVF/ICSI treatment: a prospective cohort study. Hum. Reprod. 37, 1297–1310. https://doi.org/10.1093/humrep/deac040 (2022).
Lapointe-Shaw, L. et al. Death and readmissions after hospital discharge during the December holiday period: cohort study. Bmj 363, k4481. https://doi.org/10.1136/bmj.k4481 (2018).
Kato, H., Jena, A. B. & Tsugawa, Y. Patient mortality after surgery on the surgeon’s birthday: observational study. Bmj 371, m4381. https://doi.org/10.1136/bmj.m4381 (2020).
Acknowledgements
We sincerely thank all participants for participating in this study.
Funding
This study was supported by the National Natural Science Foundation of China (82371682), the Postdoctoral Fellowship Program of CPSF (GZC20233157) and the Natural Science Foundation of Hunan Province, China (2025JJ60672).
Author information
Authors and Affiliations
Contributions
TL.Y. and YY.Y. were responsible for the data collection, article review and draft of the manuscript. ZJ.H. contributed to the data verification and manuscript writing. HY.Q., T.C., NH.L., and DE.L. contributed to the data verification. YM.L., J.Z. and Q.Z. performed the statistical analysis. ZY.Y. and F.T. were responsible for manuscript revision and the design of tables and figures. TL.Y. and YP.L. are the corresponding authors, and they critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was conducted in accordance with the Helsinki Declaration and was approved by the ethics committee at the Reproductive Medicine Center, Xiangya Hospital of CSU (No. 2022011).Due to the retrospective nature of the study, the ethics committee at the Reproductive Medicine Center, Xiangya Hospital of CSU waived the need of obtaining informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, Y., Hou, Z., Qiu, H. et al. Impact of spring festival on pregnancy outcomes in patients undergoing first embryo transfer: a retrospective cohort study. Sci Rep 15, 23339 (2025). https://doi.org/10.1038/s41598-025-05029-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-05029-6