Abstract
Recently, dolutegravir (DTG) has been associated with weight gain, dyslipidemia, and hyperglycemia, which in turn raise(s) the risk of hypertension. However, little is known about the burden of hypertension among people living with HIV (PLHIV) taking DTG-based therapy in Ethiopia. This study aimed to assess the prevalence and factors associated with hypertension among PLHIV taking DTG-based therapy. We conducted a cross-sectional study on 415 selected PLHIV aged 18 years or older who had been on DTG-based therapy for at least six months at the antiretroviral therapy (ART) clinic of Dessie Comprehensive Specialized Hospital from February 5 to April 5, 2023. Participants with a diagnosis of hypertension before DTG-based ART initiation, pregnant women, and patients who were seriously ill and unable to respond were excluded from the study. Data on sociodemographic, behavioral, and clinical characteristics were collected using a structured questionnaire and patient chart review. Blood pressure, anthropometric, and biochemical measurements were done. Hypertension was defined as systolic and/or diastolic blood pressure ≥ 140 mmHg and 90 mmHg, respectively. A multivariable logistic regression was carried out to determine factors associated with hypertension. Variables with a p-value < 0.05 were considered statistically significant. The prevalence of hypertension was 15.2% (95% CI: 11.9–19). Sex (AOR = 3.01, 95% CI: 1.56–5.79, p = 0.001), duration of taking DTG-based therapy (AOR = 3.61, 95% CI: 1.72–7.59, p = 0.001), family history of hypertension (AOR = 3.51, 95% CI: 1.54–8.04, p = 0.003), body mass index (BMI) (AOR = 1.92, 95% CI: 1.02–3.64, p = 0.044), and fasting blood glucose level (FBG) (AOR = 2.33, 95% CI: 1.01–5.39, p = 0.047) were significantly associated with hypertension among PLHIV on DTG-based ART in Ethiopia. Hypertension is not uncommon in PLHIV taking DTG-based therapy. Sex, duration of taking DTG-based therapy, family history of hypertension, BMI, and FBG levels were significant correlates of hypertension among PLHIV taking DTG-based therapy. These findings highlight the need for routine hypertension screening and lifestyle interventions for PLHIV on DTG-based therapy, particularly among males, those with prolonged use of DTG-based therapy, a family history of hypertension, elevated BMI, or increased FBG.
Similar content being viewed by others
Background
Hypertension is a major global health concern and is estimated to affect 1.13 billion individuals around the world, with approximately two-thirds residing in low- and middle-income nations1. It is currently the most common non-communicable illness among people living with HIV (PLHIV), especially in individuals aged 40 years and older2,3. More than half of the deaths among PLHIV were caused by non-infectious health conditions, with cancer and cardiovascular diseases (CVD) being the most frequent comorbidities4. According to several investigations, PLHIV are twice as likely to develop CVDs as HIV-negative people5,6. The heightened risk is partially linked to HIV-related factors such as long-term antiretroviral therapy (ART) side effects, hypercoagulation, early development of atherosclerosis, immune system activation, and elevated levels of systemic inflammatory markers6,7.
The magnitude of hypertension among PLHIV varies globally8,9. However, Sub-Saharan Africa (SSA) bears the greatest burden of the dual challenge posed by HIV and hypertension, a situation further exacerbated by widespread poverty10,11. A systematic review of articles published between 2000 and 2017 found that the prevalence of hypertension among PLHIV in SSA varied from 6 to 22%12. Studies conducted in East Africa have found that the magnitude of hypertension among PLHIV ranges from 7.98%13 to 43.3%14. In Ethiopia, studies have shown that the magnitude of hypertension in PLHIV varied from 11 to 41.3%15,16,17. Hypertension in PLHIV has been associated with various associated factors, including older age, black ethnicity, being male, and modifiable lifestyle factors like obesity, physical inactivity, smoking, and alcohol consumption11. In addition, some HIV-related health factors, including the specific type of ART regimens used, the prolonged effects of ART treatment, and the duration of HIV/AIDS infection, have also been associated with hypertension in PLHIV18.
Several studies have shown that using some types of ART, especially protease inhibitors and integrase strand transfer inhibitors (INSTIs), may increase the incidence of metabolic syndrome and weight gain, which in turn raises the risk of hypertension19,20,21. Dolutegravir (DTG) is an INSTI that has been linked to cardiometabolic risk21,22, including a possible increased risk of hypertension. The mechanisms underlying the link between DTG and weight gain are not entirely known; however, enhanced adipose tissue activation and renin-angiotensin-aldosterone system (RAAS) modulation may play a role, potentially increasing the risk of hypertension23. The drug suppresses insulin secretion and signaling, possibly via magnesium (Mg2+) chelation, leading to increased insulin resistance and elevated blood glucose levels24. In addition, DTG has been linked to alterations in lipid metabolism, contributing to low high-density lipoprotein cholesterol (HDL-C) and elevated triglyceride and cholesterol levels25. These metabolic disturbances can promote endothelial dysfunction and vascular inflammation, ultimately raising the risk of developing hypertension26.
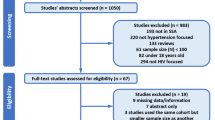
A cross-sectional study conducted in Uganda among 430 PLHIV on DTG-based ART revealed that the magnitude of hypertension was 27.2%27. An observational multicenter longitudinal study in Ghana reported a hypertension prevalence of 37.3% among PLHIV who were initiated on DTG-based ART28. Since 2018, DTG-based regimens have become the preferred first-line ART in Ethiopia and many other SSA countries29. With the growing use of DTG, concerns about its metabolic side effects have highlighted the need for local evidence. However, most existing studies in Ethiopia either predate the introduction of DTG or do not specifically focus on this drug. To the best of our knowledge, there are no reports on the prevalence of hypertension and its associated factors among PLHIV on DTG-based ART, particularly in the study area. Therefore, this study aimed to determine the prevalence of hypertension and its associated factors among PLHIV on DTG-based ART at Dessie Comprehensive Specialized Hospital (DCSH), Northeast Ethiopia.
Method
Study setting, design, and population
We conducted an institutional-based cross-sectional study among PLHIV receiving DTG-based ART. The study was carried out from February 5 to April 5, 2023, at the ART clinic of DCSH in Northeast Ethiopia. PLHIV aged 18 years or older who had been on DTG-based ART for more than 6 months27 and who volunteered to participate were included. Patients with a diagnosis of hypertension before DTG-based ART initiation, pregnant women, and patients who were seriously ill and unable to respond were excluded.
Sample size determination and sampling technique
The study determined the sample size using a formula for a single population proportion, with certain assumptions: a 5% margin of error (d = 0.05), a 95% confidence interval (Za/2 = 1.96), accounting for a 10% nonresponse rate, and considering the prevalence of hypertension among DTG-treated patients at 50%, as there were no prior studies in the region. This led to a total sample size of 423 individuals. Study participants were selected using a computer-generated simple random sampling technique. A list containing the medical registration numbers of all PLHIV on DTG-based ART (n = 772) who will have follow-up visits at DCSH during the study period was obtained from the Health Management Information System unit of DCSH. Random numbers were generated for each patient using Microsoft Excel, and these numbers were used to randomly select a sample of 423 participants. No stratification was applied during the sampling process.
Data collection procedures
We collected data using a questionnaire adapted from the WHO STEP-wise approach to chronic disease risk factor surveillance30. The questionnaire was translated into the Amharic language and then back into English by another person to check for consistency. The questionnaire was pretested on 5% (21) of the sample size at Boru Meda General Hospital. This questionnaire is divided into three sections: the first focuses on sociodemographic, behavioral, and clinical aspects; the second on physical measurements; and the third on biochemical measurements. All data were gathered by nurse professionals and laboratory technologists under the close supervision of the principal investigator. The data collectors were trained for two days on the purpose of the study, the procedures of data collection, and how to gather information from participants.
Sociodemographic data such as age, sex, education, marital status, monthly income, occupation, and residence, and behavioral characteristics including alcohol drinking status, smoking status, and physical exercise were collected from the patient interview. HIV-related factors such as WHO clinical staging of AIDS, duration of HIV/AIDS infection, duration of ART treatment, duration of DTG-based ART treatment, history of opportunistic infections, and drug adherence levels were extracted from patients’ medical records using a checklist, and other related clinical characteristics [family history of hypertension, CVD, and diabetes mellitus (DM)] were obtained from patient interviews. Body weight and height were measured using a digital balance with a height measurement attached to it. Body mass index (BMI) was calculated by dividing weight in kilograms (kg) by height in meters squared (m2). According to their risk of hypertension, BMI was classified into two categories (< 25 and ≥ 25)31. Waist circumference (WC) and hip circumference (HC) were measured using a flexible, non-elastic tape. The reference ranges were WC > 80 cm for females and > 94 cm for males, as well as a waist-to-hip ratio ≥ 0.85 for females32.
Blood pressure (BP) was measured using a mercury sphygmomanometer BP cuff of appropriate size, covering two-thirds of the upper arm, with the participant in a sitting position. The BP measurement was taken from the left arm, which was supported on a flat surface. Participants were advised to rest for a minimum of 5 min, and if they had consumed caffeinated beverages, they were allowed to rest for 30 min before the measurement. Two measurements were taken 5 min apart, and the average of the two readings was recorded.
Laboratory analysis
About 8 ml of blood was collected from each study participant by a laboratory technologist after an overnight fast. Following serum separation from the whole blood, fasting blood glucose (FBG) and lipid profile levels were measured using the enzymatic method on the Dimension EXL 200 System chemistry analyzer, utilizing a commercially available auto analyzer kit. CD4 count (cells/µl) samples were collected in EDTA containers and analyzed using a Becton Dickinson flow cytometer. Viral load (VL) (copies/mL) samples were also collected in EDTA containers and analyzed with the COBAS® Ampliprep/COBAS® TaqMan PCR analyzer.
Operational definition
Hypertension was defined as systolic blood pressure (SBP) and/or diastolic blood pressure (DBP) greater than or equal to 140 mmHg and 90 mmHg, respectively33.
Smoking status was defined as “smoker” for participants who had smoked at least one cigarette within the last one year16.
Alcohol drinking status was defined as “alcohol drinker” for participants who consumed any type of alcoholic beverage more than once per week in the past year regardless of the amount34,35.
Khat chewing status was defined as “chewer” for participants who consumed any amount of khat in the last one year; otherwise, they were classified as “non-chewer”36.
Participants were classified as engaging in regular physical activity if they reported performing at least 30 min of intense exercise once a week or more16.
Comorbid disease was defined as a chronic disease with a confirmed diagnosis of the disease other than HIV infection, like cardiovascular disease, mental health disorders, TB, etc37.
Statistical analysis
Data were checked for completeness and entered in Epi-Data version 4.6 and analyzed using SPSS version 26.0. Categorical data were presented using frequency distribution, while continuous data were expressed as the median ± interquartile range (IQR). Logistic regression analysis was used to evaluate the associations between the correlates and hypertension. Variables with p-values less than 0.25 in the bivariate logistic regression analysis were included in a multivariable logistic regression model to account for potential confounding factors. Crude and adjusted odds ratios with 95% confidence intervals (CI) are reported, and a p-value of less than 0.05 was considered statistically significant. Multicollinearity between the independent variables was assessed, and the variance inflation factor (VIF) was determined to be within an acceptable range (since the VIF was < 2 in this study). In addition, the model’s fit was assessed using the Hosmer and Lemeshow test.
Ethics approval and consent to participate
An ethical clearance letter was obtained from Debre Markos University, School of Medicine, ethical review committee with reference number SOM/229/44/23 and date 20/01/2023. A collaboration letter for data collection was also obtained from DCSH. It was confirmed that the study met the ethical and scientific standards outlined in national and international guidelines. Written informed consent was obtained from all participants, or from legal guardian in cases where participants were unable to read or write, prior to the start of the study.
Result
Sociodemographic and behavioral characteristics
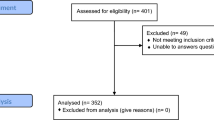
A total of 415 participants were included in this study, achieving a 98.1% response rate. Of these, the majority (60.2%) are females, with a median age of 42 years (IQR: 38, 50), 60.7% residing in rural areas, and 29.9% being farmers. Concerning behavioral characteristics, about 58.6% didn’t do regular physical exercise, 12.8% were alcohol drinkers, and 5.1% were cigarette smokers (see Table 1).
Clinical characteristics of the study participants
Over half of the study participants (56.1%) had CD4 counts below 500 cells/mm³; almost half (50.6%) of participants had been living with HIV for more than 10 years; and 57.8% had been using a DTG-based regimen for more than 2 years. Approximately 8% of participants had a history of opportunistic infections in the last 6 months, and 11.3% had a family history of hypertension (see Table 2).
Anthropometric characteristics of the study participants
About 37.6% of participants were classified as having excessive body weight (overweight/obese), 35.2% had a raised waist circumference, and 40.2% had elevated waist-to-hip ratios (Table 3).
Biochemical characteristics of the study participants
More than half of the study participants (57.3%) had low HDL-C levels, and 13% exhibited hyperglycemia (Table 4).
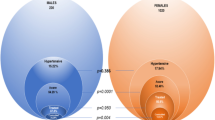
Prevalence of hypertension among PLHIV taking DTG-based ART
The prevalence of hypertension was found to be 63 cases (15.2%), with a 95% CI ranging from 11.9 to 19% (see Fig. 1). Among hypertensive study participants, the mean values of SBP and DBP were 149.4 ± 15.3 mmHg and 96.8 ± 9.2 mmHg, respectively, whereas those among the normotensive study participants were 117.4 ± 9 mmHg and 75.26 ± 7.3 mmHg, respectively.
Factors associated with hypertension among PLHIV taking DTG-based ART
Factors such as age, sex, physical exercise, alcohol drinking status, CD4 T-cell counts, duration of living with HIV, duration of taking ART, duration of taking DTG-based ART treatment, family history of hypertension, family history of DM, comorbidities, BMI, waist circumference, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and FBG were associated with hypertension in bivariable logistic regression. In multivariable logistic regression, sex (AOR = 3.01, 95% CI: 1.56–5.79, p = 0.001), duration of taking DTG-based therapy (AOR = 3.61, 95% CI: 1.72–7.59, p = 0.001), family history of hypertension (AOR = 3.51, 95% CI: 1.54–8.04, p = 0.003), BMI (AOR = 1.92, 95% CI: 1.02–3.64, p = 0.044), and FBG level (AOR = 2.33, 95% CI: 1.01–5.39, p = 0.047) were significantly associated with hypertension among PLHIV taking DTG-based ART (see Table 5).
Discussion
The purpose of this study was to look at the prevalence of hypertension and its associated factors in PLHIV taking DTG-based ART. In this study, the prevalence of hypertension among PLHIV on DTG-based ART was 15.2% (95% CI: 11.9–19). We also found that sex, duration of taking DTG-based ART, family history of hypertension, BMI, and FBG levels were significant correlates of hypertension among PLHIV on DTG-based ART.
The prevalence in our study is in line with the findings from Benin (16.8%)38 and southern Ethiopia (17.3%)39. However, this prevalence is higher than that reported in a previous study conducted in Northwest Ethiopia (7.21%)40. In addition, the prevalence in our study was higher compared to the ADVANCE clinical study conducted in South Africa reported the prevalence of hypertension after 192 weeks was 10.5%41. On the other opposing, the prevalence in this study was lower than that reported in previous studies conducted in Uganda (27.2%)27, Northwest Ethiopia (42%)17, Kenya (24.2%)42, and Ghana (21%)43. In addition, an observational multicenter longitudinal study was undertaken from 2020 to 2022 in Ghana to investigate the prevalence of hypertension among PLHIV taking DTG-based ART, and the prevalence rate was 37.3%, which is higher than the current result28. Furthermore, the prevalence of hypertension in our study was lower compared to a study in Tanzania conducted among 430 participants, 99.3% of whom were on DTG-based ART, which reported a prevalence of 24.8%44. Moreover, the NASMAL clinical study conducted in Cameroon showed that the prevalence of hypertension among PLHIV taking DTG-based ART was 33.33% after 192 weeks, which is higher than the current study41. Within the general population of Ethiopia, the pooled prevalence of hypertension was found to be 20.63%45. This result indicates that the prevalence of hypertension among PLHIV on DTG-based ART is lower than that observed in the general population of Ethiopia. This inconsistency might be because of variations in socioeconomic and demographic conditions, lifestyle factors, genetic predispositions, study methodologies (differences in study populations, inclusion criteria, and sample size), comorbidity prevalence, local ART guidelines, and duration of HIV infections and ART treatment. For instance, the studies done in Northwest Ethiopia40 and Ghana28 were cohort studies, whereas our study used an institutional-based cross-sectional study design. In addition, a study conducted in Tanzania44 included those who were ART-naïve individuals; however, our study included those who were ART-experienced individuals. Furthermore, a study conducted in Uganda27 included higher proportions of participants with a BMI ≥ 25 kg/m² (59.6% vs. 37.6%) and a history of alcohol use (20% vs. 12.8%) compared to our study. Moreover, a study conducted in Northwest Ethiopia40 included 30.8% of participants with comorbidities, compared to 10.8% in our study. These factors may account for the difference.
Sex, duration of taking DTG-based ART, family history of hypertension, BMI, and FBG levels were significantly associated with hypertension among PLHIV taking DTG-based ART. Accordingly, male participants were 3.01 times more likely to have hypertension as compared to female participants. Similar findings were reported in Uganda27 and Kenya42. This difference in sex may be explained by hormonal differences that protect women from hypertension. It is possible that female hormones, especially estrogen, may play a role in protecting them from developing hypertension due to their vasodilatory effect on the blood vessels46. In men, androgens raise blood pressure through activation of the renin-angiotensin system (RAS). This triggers oxidative stress, resulting in the production of vasoconstrictive substances and a decrease in nitric oxide availability47. Furthermore, men are more susceptible to behavioral factors such as alcohol consumption, smoking, and other substance use, which are directly associated with a higher risk of developing hypertension compared to women.
Duration of taking DTG-based ART treatment was significantly associated with hypertension. Patients who had been on DTG-based ART for longer than 2 years were 3.61 times more likely to have hypertension as compared to those who had been on DTG-based ART for less than or equal to 2 years. This finding is consistent with previous studies from Uganda27, Ethiopia46, and Tanzania10. The relationship between the duration of ART treatment and hypertension might be directly influenced by alterations in endothelial function, or it could be associated with longevity and age-related conditions, including ART-induced changes in body composition and weight gain48,49.
The findings of the current study reveal that having a family history of hypertension is significantly associated with hypertension. Participants with a family history of hypertension were 3.51 times more likely to develop hypertension compared to those without a similar history. This is similar to previous studies in South Africa50, Rwanda51, and Ethiopia52. This association might be explained by the family members sharing genes that increase susceptibility to elevated blood pressure and stroke. In addition, this could be because of family members sharing similar lifestyle habits, such as dietary habits, exercise, and alcohol consumption, which can negatively impact health53,54.
BMI was another factor significantly associated with hypertension among PLHIV on DTG-based ART. Participants with a BMI of ≥ 25 kg/m2 were 1.92 times more likely than their counterparts to develop hypertension. This finding is consistent with studies conducted in Benin38, Ghana43, Burundi55, and Ethiopia53. Several mechanisms have been proposed to explain the association between obesity and hypertension. It is commonly believed that the buildup of visceral and ectopic fat in various tissues and organs disrupts metabolic and hemodynamic processes56. Furthermore, insulin resistance and inflammation may contribute to changes in vascular function in obese individuals, leading to the development of hypertension57. Although the mechanism of interaction between DTG and obesity is not fully understood, multiple studies have identified a link between DTG use and excess body weight21,58. This indicates that preventive strategies focused on weight management and a healthy diet are essential for reducing excess body weight in PLHIV who are taking DTG27.
Moreover, FBG level was found to be significantly associated with hypertension. Individuals who had a FBG level ≥ 110 mg/dl were 2.33 times more likely to develop hypertension as compared to those who had FBG level < 110 mg/dl. This result is consistent with findings from Southern Ethiopia59 and Northeast Ethiopia60. This association could be attributed to elevated blood glucose levels, which lead to plaque formation that obstructs normal blood flow and may, in turn, raise blood pressure61,62. In addition, as blood glucose levels rise, widespread damage to blood vessels occurs. This results in a loss of blood vessel elasticity and an increase in body fluid volume, both of which may elevate the risk of hypertension63.
Strengths and limitations of the study
This is one of the first studies to assess hypertension in PLHIV taking DTG-based ART in Ethiopia, providing the framework for future research. Despite its strength, this study has certain weaknesses. Since we excluded patients with known hypertension prior to DTG initiation, the prevalence estimate may be skewed downward. Data collection relied on a questionnaire with self-reported variables, which may have led participants to provide desirable responses. In addition, as the study sample came from a single institution, the results should be interpreted carefully. Furthermore, the study lacked data on participants’ renal function, dietary intake, and salt consumption, which could potentially confound the observed prevalence of hypertension. Moreover, due to its cross-sectional design, this study cannot establish a temporal link between hypertension and associated factors.
Conclusion
Hypertension is not uncommon in PLHIV taking DTG-based ART. Sex, duration of taking DTG-based ART, family history of hypertension, BMI, and FBG levels were significant correlates of hypertension among PLHIV on DTG-based ART. These findings highlight the need for routine hypertension screening and lifestyle interventions for PLHIV on DTG, particularly among males, those with prolonged use of DTG-based ART, a family history of hypertension, elevated BMI, or increased FBG. In addition, we suggest that researchers conduct a prospective cohort study to investigate the effect of DTG-based ART on hypertension.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- PLHIV:
-
People living with HIV
- CVD:
-
Cardiovascular diseases
- DTG:
-
Dolutegravir
- INSTI:
-
Integrase strand transfer inhibitor
- WHO:
-
World Health Organization
- SSA:
-
Sub-Saharan Africa
- DCSH:
-
Dessie Comprehensive Specialized Hospital
- BMI:
-
Body mass index
- HDL-c:
-
High-density lipoprotein cholesterol
- LDL-c:
-
Low-density lipoprotein cholesterol
- FBG:
-
Fasting blood glucose
- CD4:
-
Cluster of differentiation 4
- ART:
-
Antiretroviral therapy
- INSTI:
-
Integrase strand transfer inhibitor
- HIV:
-
Human immunodeficiency virus
- WC:
-
Waist circumference
- DM:
-
Diabetes mellitus
- CI:
-
Confidence interval
- AOR:
-
Adjusted odd ratio
References
(WHO) WHO & Hypertension [ (2021). Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension
Albrecht, S. et al. Age-related comorbidities and mortality in people living with HIV in rural Tanzania. AIDS (London England). 33 (6), 1031–1041 (2019).
Brennan, A. T. et al. Prevalence, incidence, predictors, treatment, and control of hypertension among HIV-positive adults on antiretroviral treatment in public sector treatment programs in South Africa. PLOS ONE. 13 (10), e0204020 (2018).
Pourcher, V., Gourmelen, J., Bureau, I. & Bouee, S. Comorbidities in people living with HIV: an epidemiologic and economic analysis using a claims database in France. PLOS ONE. 15 (12), e0243529 (2020).
Chhoun, P. et al. High prevalence of non-communicable diseases and associated risk factors amongst adults living with HIV in Cambodia. PLOS ONE 12(11):e0187591. (2017).
Baekken, M., Os, I., Sandvik, L. & Oektedalen, O. Hypertension in an urban HIV-positive population compared with the general population: influence of combination antiretroviral therapy. Journal of Hypertension 26(11):2126–2133. (2008).
Vecchiet, J. et al. Antihypertensive and metabolic effects of Telmisartan in hypertensive HIV-Positive patients. Antiviral Therapy 16(5):639–645. (2011).
Xu, Y., Chen, X. & Wang, K. J. J. A. S. H. Global prevalence of hypertension among people living with HIV: a systematic review and meta-analysis. Journal of the American Society of Hypertension 11(8):530–540. (2017).
Gonah, L., Moodley, I., Hlongwana, K. W. J. A. J. P. H. C. & Medicine, F. Prevalence of diabetes mellitus and hypertension in people living with human immunodeficiency virus on antiretroviral therapy in Gweru district. Zimbabwe 12 (1), 1–6 (2020).
Kagaruki, G. B. et al. Magnitude and risk factors of non-communicable diseases among people living with HIV in tanzania: a cross sectional study from Mbeya and Dar Es Salaam regions. 14:1–9. (2014).
Mogaka, J. N. et al. Prevalence and factors associated with hypertension among adults with and without HIV in Western Kenya. PLoS One 17(1):e0262400. (2022).
Hyle, E. P. et al. The association between HIV and atherosclerotic cardiovascular disease in sub-Saharan africa: a systematic review. BMC Public Health 17:1–15. (2017).
Sander, L. D. et al. Hypertension, cardiovascular risk factors and antihypertensive medication utilisation among HIV-infected individuals in R Akai. U Ganda. 20 (3), 391–396 (2015).
Memiah, P. et al. Hypertension and associated inflammatory markers among HIV-infected patients in Tanzania. Journal of Interferon & Cytokine Research 41(8):291–301. (2021).
Lukas, K., Markos, E., Belayneh, F. & Habte, A. The magnitude of hypertension and associated factors among clients on highly active antiretroviral treatment in Southern ethiopia, 2020: A hospital-based cross-sectional study. PLOS ONE. 16 (10), e0258576 (2021).
Gebrie, A. Hypertension among people living with human immunodeficiency virus receiving care at referral hospitals of Northwest ethiopia: A cross-sectional study. PLOS ONE. 15 (8), e0238114 (2020).
Sewale, Y., Afenigus, A. D., Haile, D. & Shiferaw, W. S. Magnitude of hypertension and associated factors among human immunodeficiency virus positive adults receiving Anti-Retroviral therapy at Debre Markos referral hospital (2020)., Northwest, Ethiopia. HIV/AIDS (Auckland, NZ). HIV AIDS (Auckl) 12:629–637 .
Lackland, D. T., Keil, J. E., Gazes, P. C., Hames, C. G. & Tyroler, H. A. Outcomes of black and white hypertensive individuals after 30 years of follow-up. Clin. Experimental Hypertens. (New York NY: 1993). 17 (7), 1091–1105 (1995).
Dillon, D. G. et al. Association of HIV and ART with cardiometabolic traits in sub-Saharan africa: a systematic review and meta-analysis. Int J Epidemiol 42(6):1754–1771. (2013).
Musekwa, R., Hamooya, B. M., Koethe, J. R., Nzala, S. & Masenga, S. K. J. P. A. M. J. Prevalence and correlates of hypertension in HIV-positive adults from the Livingstone central hospital. Zambia 39(1), 237. (2021).
Jemal, M. A review of dolutegravir-associated weight gain and secondary metabolic comorbidities. SAGE Open Med 12:20503121241260613. (2024).
Goldberg, R. N., Kania, A. T., Michienzi, S. M., Patel, M. & Badowski, M. E. J. J. I. A. P. A. C. Weight gain in incarcerated individuals living with HIV after switching to integrase strand inhibitor-based therapy. J Int Assoc Provid AIDS Care 20:2325958221996860. (2021).
Leggio, M. et al. The relationship between obesity and hypertension: an updated comprehensive overview on vicious twins. Hypertens Res 40(12):947–963. (2017).
Kamal, P. & Sharma, S. J. J. E. S. SUN-187 dolutegravir causing diabetes. ;3(Supplement_1):SUN-187. (2019).
Kigongo, V. J. et al. Dyslipidemia among adult people living with HIV on dolutegravir - based antiretroviral therapy at a private tertiary hospital in kampala, uganda: burden and determinants. BMC Infect. Dis. 24 (1), 53 (2024).
Petrie, J. R., Guzik, T. J. & Touyz, R. M. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can. J. Cardiol. 34 (5), 575–584 (2018).
Kasoma Mutebi, R. et al. Prevalence of and factors associated with hypertension among adults on Dolutegravir-Based antiretroviral therapy in uganda: A cross sectional study. Integr. Blood Press. Control. 16, 11–21 (2023).
Lartey, M. et al. Hypertension among cohort of persons with human immunodeficiency virus initiated on a Dolutegravir-Based antiretroviral regimen in Ghana. Open. Forum Infect. Dis. 11 (3), ofae061 (2024).
FMoHo, E. J. G. W. H. O. National consolidated guidelines for comprehensive HIV prevention, care and treatment. (2020).
Organization, W. H. STEPwise approach to NCD risk factor surveillance (STEPS) Geneva: World Health Organization; [ (2012). Available from: https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps
Nuttall, F. Q. Body mass index: obesity, BMI, and health: A critical review. Nutr. Today. 50 (3), 117–128 (2015).
Consultation WEJRoaWECGWHO. Waist circumference and waist-hip ratio. 2008:8–11. (2008).
Williams, B. et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur. Heart J. 39 (33), 3021–3104 (2018).
Beyene Kassaw, A., Tezera Endale, H., Hunie Tesfa, K. & Derbew Molla, M. Metabolic syndrome and its associated factors among epileptic patients at Dessie comprehensive specialized hospital, Northeast ethiopia; a hospital-based comparative cross-sectional study. PLoS One. 17 (12), e0279580 (2022).
EPH A. On Alcohol, Substance, Khat and Tobacco. 22nd Annual Conference of EPHAApril 2012.
Tesfaye, F., Byass, P., Wall, S., Berhane, Y. & Bonita, R. Association of smoking and Khat (Catha Edulis Forsk) use with high blood pressure among adults in addis ababa, ethiopia, 2006. Prev. Chronic Dis. 5 (3), A89 (2008).
Manual FMoHJP. National Comprehensive HIV Prevention, Care and Treatment Training for Health care Providers. :1-123. (2018).
Assogba, C. O. et al. Prevalence and associated factors of hypertension among people living with HIV/AIDS on antiretroviral therapy in benin’s National teaching hospital. Sci. Rep. 14 (1), 17035 (2024).
Hirigo, A. T., Yilma, D., Astatkie, A. & Debebe, Z. The association between dolutegravir-based antiretrovirals and high blood pressure among adults with HIV in Southern ethiopia: a cross-sectional study. Ther Adv Infect Dis 11:20499361241306942. (2024).
Mulugeta, H. et al. Incidence and Predictors of Hypertension Among HIV Patients Receiving ART at Public Health Facilities, Northwest Ethiopia: A One-Year Multicenter Prospective Follow-Up Study. HIV/AIDS (Auckland, NZ). ;13:889–901. (2021).
Venter, W. (ed) Risks of hypertension with first-line dolutegravir and tenofovir alafenamide in the NAMSAL and ADVANCE trials-OALBB05. 12th IAS Conference on HIV Science Brisbane, Australia; (2023).
Mbuthia, G. W., Magutah, K. & McGarvey, S. T. The prevalence and associated factors of hypertension among HIV patients. Int. J. Hypertens. 2021 (1), 5544916 (2021).
Denu, M. K. I., Revoori, R., Buadu, M. A. E., Oladele, O. & Berko, K. P. Hypertension among persons living with HIV/AIDS and its association with HIV-related health factors. AIDS Res. Therapy. 21 (1), 5 (2024).
Mwakyandile, T. M. et al. Hypertension and traditional risk factors for cardiovascular diseases among treatment Naïve HIV- infected adults initiating antiretroviral therapy in urban Tanzania. BMC Cardiovasc. Disord. 23 (1), 309 (2023).
Tesfa, E. & Demeke, D. Prevalence of and risk factors for hypertension in ethiopia: A systematic review and meta-analysis. Health Sci. Rep. 4 (3), e372 (2021).
Dubey, R. K., Oparil, S., Imthurn, B. & Jackson, E. K. Sex hormones and hypertension. Cardiovascular. Res. 53 (3), 688–708 (2002).
Reckelhoff, J. F. J. H. Gender differences in the regulation of blood pressure. Hypertension 37(5):1199–1208. (2001).
Getahun, Z., Azage, M., Abuhay, T. & Abebe, F. Comorbidity of HIV, hypertension, and diabetes and associated factors among people receiving antiretroviral therapy in Bahir Dar City. Ethiopia J. Comorbidity. 10, 2235042x19899319 (2020).
McGettrick, P., Alvarez Barco, E. & Mallon, P. W. (eds) Ageing with HIV (MDPI, 2018).
Tsuro, U., Oladimeji, K. E., Pulido-Estrada, G. A. & Apalata, T. R. Risk factors attributable to hypertension among HIV-Infected patients on antiretroviral therapy in selected rural districts of the Eastern cape province, South Africa. Int. J. Environ. Res. Public Health 19(18). (2022).
Uwanyirigira, D. et al. Prevalence and factors associated with hypertension among HIV positive patients on antiretroviral therapy: A Hospital-Based Cross-Sectional study in Rwanda. Vasc. Health Risk Manag. 19, 857–870 (2023).
Badacho, A. S. & Mahomed, O. H. Prevalence of hypertension and diabetes and associated risk factors among people living with human immunodeficiency virus in Southern Ethiopia. Front. Cardiovasc. Med. 10, 1173440 (2023).
Haile, M., Degelo, T., Adilo, T. M., Adem, F. M. & Gidisa, B. Prevalence of Hypertension and Its Associated Factors Among Adults Living with HIV on Antiretroviral Treatment in Selected Public Hospitals in Addis Ababa, Ethiopia. HIV/AIDS (Auckland, NZ). ;16:109 – 22. (2024).
Tozawa, M. et al. Family history of hypertension and blood pressure in a screened cohort. Hypertens Res 24(2):93–98. (2001).
Harimenshi, D., Niyongabo, T., Preux, P. M., Aboyans, V. & Desormais, I. Hypertension and associated factors in HIV-infected patients receiving antiretroviral treatment in burundi: a cross-sectional study. Sci. Rep. 12 (1), 20509 (2022).
Ferrara, D., Montecucco, F., Dallegri, F. & Carbone, F. Impact of different ectopic fat depots on cardiovascular and metabolic diseases. J. Cell. Physiol. 234 (12), 21630–21641 (2019).
Goodpaster, B. H. et al. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. Jama 304 (16), 1795–1802 (2010).
Menard, A. et al. effect? Dolutegravir and weight gain: an unexpected bothering side. AIDS 31(10):1499–1500. (2017).
Zewudie, B. T. et al. The magnitude of undiagnosed hypertension and associated factors among HIV-positive patients attending antiretroviral therapy clinics of Butajira general hospital, gurage zone, Southern Ethiopia. SAGE Open. Med. 10, 20503121221094454 (2022).
Fiseha, T., Belete, A. G., Dereje, H. & Dires, A. Hypertension in HIV-Infected patients receiving antiretroviral therapy in Northeast Ethiopia. Int. J. Hypertens. 2019, 4103604 (2019).
Tatsumi, Y. et al. SAKU STUDY 39:e15–e6. (2021).
Tegegne, K. D. et al. Prevalence and factors associated with hypertension among peoples living with HIV in East africa, a systematic review and meta-analysis. BMC Infect. Dis. 23 (1), 724 (2023).
Cheung, B. M. & Li, C. Diabetes and hypertension: is there a common metabolic pathway? Curr. Atheroscler. Rep. 14 (2), 160–166 (2012).
Acknowledgements
We would like to begin by expressing our sincere appreciation to Debre Markos University for providing us the opportunity to conduct this research. Our thanks also extend to the DCSH for granting us the necessary data access authorization, which made this study possible. We are especially grateful to our study participants for their voluntary involvement, which was vital to the success of this research.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
MJ: conceptualization, manuscript draft, design, manuscript writing-up, manuscript editing, and validation. AA: conceptualization, writing-original draft, writing-review and editing. DA: writing-original draft, writing-review and editing, and validation. TM: conceptualization, writing-original draft, writing-review and editing. WA: conceptualization, writing-original draft, writing-review and editing. DA: writing-original draft, writing-review and editing, and validation. DA: writing-original draft, writing-review and editing, validation, and supervision. YTW: conceptualization, visualization, supervision, writing-original draft, writing-review and editing, and validation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jemal, M., Abebaw, D., Workineh, Y.T. et al. Hypertension among people living with HIV receiving dolutegravir-based antiretroviral therapy in ethiopia: a cross-sectional study. Sci Rep 15, 23267 (2025). https://doi.org/10.1038/s41598-025-06145-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-06145-z