Abstract
Overweight and obesity are major global public health concerns, and they are increasingly recognized as side effects of long-term antiretroviral therapy (ART) in people living with HIV (PLHIV). As ART improves life expectancy, weight gain and associated comorbidities have emerged as new challenges in HIV care. This study aimed to determine the prevalence and associated factors with overweight and obesity among people living with HIV(PLHIV) on antiretroviral therapy (ART) in Benin’s National Teaching Hospital. A prospective cross-sectional study was conducted over a three-month period, from December 17, 2023, to February 10, 2024. Data were collected through structured interviews and medical record reviews. Statistical analyses included descriptive statistics, univariable, and multivariable logistic regression to assess associations between overweight/obesity and demographic, clinical, and lifestyle factors. The prevalence of overweight and obesity in the study population was 49.4%, with a significantly higher prevalence in females (36.8%) than males (12.6%). Multivariable analysis identified female sex (aOR: 2.4; 95% CI: 1.5–4.1; p < 0.001) and hypertension (aOR: 2.5; 95% CI: 1.6–4.1; p < 0.001) as strong independent predictors of overweight and obesity. Conversely, a high viral load (> 1000 copies/ml) was inversely associated with excess weight (aOR: 0.4; 95% CI: 0.2–0.9; p = 0.050). In summary, nearly half of PLHIV on ART were overweight or obese. Female sex and hypertension increased the risk, while high viral load was linked to lower weight. These findings underline the need for integrated care approaches that address weight management in HIV treatment programs.
Similar content being viewed by others
Introduction
The global rise in overweight and obesity has become a major public health issue, with its prevalence having more than doubled since 19901. According to the World Health Organization (WHO), approximately 2.5 billion adults were overweight in 2022, including 890 million classified as obese, making up 43% of the global adult population2. Obesity significantly increases the risk of chronic diseases such as cardiovascular diseases (CVD), type 2 diabetes, and certain cancers, and was linked to approximately 5 million deaths in 20192. In sub-Saharan Africa, including Benin, obesity rates have been steadily increasing, especially in urban populations, due to changes in diet, physical activity, and socioeconomic factors3.
Historically, people living with HIV (PLHIV) were more often affected by undernutrition and wasting syndrome, especially before the advent of antiretroviral therapy (ART)4. However, this trend has shifted dramatically with the widespread use of ART5. As immune function improves and life expectancy increases many PLHIV are now experiencing significant weight gain6. Studies have reported that up to 50% of PLHIV on ART may be overweight or obese, with some data showing even higher rates among women and older adults7. This change is partly attributed to improved health status, ART-related metabolic changes, and lifestyle factors. Certain ART regimens, especially those containing integrase strand transfer inhibitors (INSTIs), have been strongly associated with weight gain, particularly among women and people of African descent4. This is not necessarily a beneficial effect, rather, it presents a new clinical concern as excess weight contributes to a growing burden of non-communicable diseases (NCDs) in this population8. PLHIV now face similar, if not higher, risks of metabolic disorders compared to the general population due to a combination of chronic HIV-related inflammation, long-term ART use, and traditional risk factors9,10. Overweight and obesity among PLHIV have been linked to hypertension, dyslipidemia, insulin resistance, and cardiovascular diseases, complicating HIV management and increasing healthcare burdens11. While organizations such as WHO and UNAIDS have acknowledged these emerging challenges, most HIV care programs in sub-Saharan Africa still focus heavily on virological suppression, with limited emphasis on overweight or obesity prevention and management12. Moreover, in Benin, evidence on the burden of overweight and obesity among PLHIV remains limited and there is a critical gap in understanding the evolving metabolic risks in this population. Therefore, our study aims to assess the prevalence of overweight and obesity among PLHIV in Benin and investigate its associated factors. Our findings will not only enhance clinical guidelines for weight management in PLHIV in Benin but also inform targeted interventions, policy recommendations, and future research in similar settings across sub-Saharan Africa.
Methods
Study design
This was a hospital-based cross-sectional study where the data was collected prospectively over a three-month period, from 17th December 2023 to 10th February 2024.
Study setting and population
The study was conducted at the largest medical facility in Benin, the Centre national Hospitalier et Universitaire Hubert Koutoukou Maga (CNHU-HKM) which provides a range of healthcare services to diverse populations, including individuals living with non-communicable diseases (NCDs), sero-discordant couples, adolescents, the elderly, pregnant women, and the most-at-risk populations (MARPs). All eligible PLHIV who visited HKM’s HIV clinic during the study period was included. Eligible participants were defined as HIV-infected adults, of both sexes, aged 18 years or older, who were on ART for more than 6 months and actively receiving care at the hospital, including pregnant women.
Sample size
We calculated the sample size using the SCHWARTZ formula. Considering the prevalence of overweight and obesity in the general population in Benin which is 30.1%8, a Z-score (standard normal critical value) of 1.96 for 95% confidence level and a margin error of 0.05, the initial sample size was 323. We further adjusted this sample size with the assumption that we may have 10% non-response rate in our study population, and this led to a total sample size of 359 subjects.
Data collection procedures and measurements
Data were systematically collected during the study period using standardized questionnaires, anthropometric measurements and data were also sourced from electronic medical health records and medical charts. Weight was measured using a calibrated scale, while height was measured using a stadiometer with a resolution of 0.1 cm. The body mass index (BMI) was calculated using the following formula:
BMI (kg/m²) = weight (in kg) / height² (in m²).
Participants were categorized into normal weight (18.5–24.9 kg/m²), overweight (25–29.9 kg/m²), and obesity (≥ 30 kg/m²)9.
Study variables
Dependent variable
Overweight and obesity.
Independent variables
Sociodemographic characteristics, health behaviors, physical activity, dietary habits, chronic conditions, and psychological factors.
Operational definitions
Demographic characteristics
Key demographic factors included sex (male or female), age (continuous variable), education level (none, primary, secondary, university), marital status (married or not married), and employment status (employed or not employed).
Health behaviors
Alcohol Use Disorders Identification Test – Consumption (AUDIT-C) questionnaire was used to assess alcohol consumption. The AUDIT-C is a three-item questionnaire, with each item scored from 0 to 4, producing a total score ranging from 0 to 12. A higher score indicates a greater likelihood of hazardous drinking, distinguishing between occasional drinkers and individuals with problematic alcohol use. In this study, participants were categorized into never drank, former drinkers, and current drinkers based on their responses.
The Lifetime Total Alcohol Consumption (LTAC) questionnaire was used to estimate the total quantity of alcohol consumed throughout an individual’s life by assessing drinking frequency, duration of use, and types of alcoholic beverages consumed. This measure provides a cumulative assessment of long-term alcohol exposure, complementing the AUDIT-C findings. Both AUDIT-C and LTAC have been validated across diverse populations and are widely used in epidemiological studies of alcohol consumption10,11.
Physical activity
Physical activity levels were assessed using the WHO STEPwise approach (STEPS), a standardized tool for evaluating behavioral risk factors for non-communicable diseases (NCDs). Activity levels were classified based on the metabolic equivalent of task (MET) scores, which were calculated as follows:
-
Vigorous-intensity activity: MET score = 8 × total minutes of vigorous activity.
-
Moderate-intensity activity: MET score = 4 × total minutes of moderate activity.
-
Walking: MET score = 3.3 × total minutes of walking.
A total MET score was computed for each participant, and physical activity levels were categorized as high (≥ 1500 MET-minutes from vigorous activity OR a total MET score ≥ 3000), moderate (600 to 2999 MET-minutes), or low (less than 600 MET-minutes)12.
Dietary habits
They were assessed using the Rapid Eating and Activity Assessment for Participants – Shortened Version (REAP-S), a validated tool designed to evaluate dietary quality. The questionnaire consists of 16 items covering various dietary components, including cereal, fruit, vegetable, dairy, protein, fat, and processed food consumption.
For this study, 13 items were used to compute a total dietary score, with possible values ranging from 13 to 39, where higher scores indicate better dietary habits. Participants were categorized into two groups based on their total score: weak diet (REAP-S score ≤ 26) and better diet (REAP-S score > 26). This tool provides a comprehensive evaluation of dietary patterns, allowing for a detailed assessment beyond simple food group consumption13.
Chronic conditions
The study also examined the prevalence of hypertension defined as a previous clinical diagnosis OR measured systolic blood pressure (SBP) ≥ 140 mmHg and/or diastolic blood pressure (DBP) ≥ 90 mmHg during the study.
Psychological factors
To evaluate psychological stress levels, the Perceived Stress Scale – 10 items (PSS-10) – was administered. This tool assesses stress perception over the past month, with each question scored from 0 to 4, generating a total score ranging from 0 to 40. Higher scores indicate greater perceived stress. Participants were categorized into low (PSS score ≤ 13), moderate (PSS score = 14–26), and high (PSS score ≥ 27) stress groups. The French version of the PSS-10 has been validated in multiple studies, demonstrating strong associations with mental health outcomes, cortisol levels, and overall well-being14,15.
Antiretroviral therapy (ART) regimens
Data on participants’ current ART regimens were collected to assess potential associations with overweight and obesity. The ART regimens were categorized into the following drug classes:
-
Nucleoside Reverse Transcriptase Inhibitors (NRTIs): Includes medications such as Lamivudine (3TC), Tenofovir Disoproxil Fumarate (TDF), Abacavir (ABC), and Zidovudine (AZT).
-
Integrase Strand Transfer Inhibitors (INSTIs): Primarily Dolutegravir (DTG), a widely used integrase inhibitor.
-
Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs): Includes Efavirenz (EFV) and Nevirapine (NVP).
Participants were classified based on their current ART regimen. If they were on combination therapy, they were included in multiple categories accordingly.
Data management and analysis
Data was collected using Open Data Kit (ODK) software on smartphones, with real-time monitoring to ensure completeness and validity. After collecting, the data was consolidated, cleaned, and checked for internal consistency.
Descriptive statistics were used to summarize the study variables. Categorical variables were presented as frequency counts and percentages, while continuous variables were summarized using means and standard deviations. The Chi-square test was used to assess associations between categorical variables and overweight/obesity status. In cases where expected cell counts were low, Fisher’s exact test was applied to ensure accurate statistical inference.
To examine the factors associated with overweight/obesity among PLHIV, logistic regression was performed. Variables with a p-value < 0.20 in univariable analysis and those previously identified in the literature as relevant were included in the multivariable model. Statistical significance in the final model was set at p < 0.05. The strength of associations was expressed as odds ratios (ORs) with 95% confidence intervals (CIs). Model fit was assessed using the Akaike Information Criterion (AIC), and multicollinearity was checked before finalizing the model. All analyses were conducted using R software version 4.4.2 (R Foundation, Vienna, Austria)16.
Ethics approval and consent to participate
The study obtained the approval of the Local Biomedical Research Ethics Committee of the University of Parakou under the reference number 455/2023/CLERB-UP/P/SP/R/SA. In addition, the study sought the authorization of the administration of the CNHU-HKM of Cotonou on the one hand and of the CNRRPEC on the other hand to allow data collection in the institution.
Written informed consent was obtained from all the subjects before the study. The study was also conducted following the Helsinki Declaration of research involving human subjects
Results
Socio-demographics, and clinical characteristics of the study population
Table 1 presents the socio-demographic and clinical characteristics of the study participants. 372 participants were enrolled, with females making up the majority (66.4%). 20.2% had no formal education, while 69.4% were married. Most participants (80.4%) were unemployed. In terms of lifestyle habits, 90.6% were current alcohol user, and 7.8% were current smokers. Physical activity levels were generally low, with 65.6% engaging in minimal activity. Additionally, 48.4% had hypertension, and 90.6% reported moderate stress levels. Viral load analysis showed that 83.6% had less than 50 copies/mL. 69.6% had been on ART treatment for over five years. Of all participants who used NRTIs, 97.3% received INSTIs, and 1.9% were on NNRTIs.
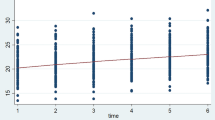
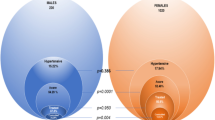
Prevalence of overweight and obesity
Figure 1 illustrates the prevalence of overweight and obesity among the study population, by sex. Among participants who are not overweight or obese, 21% were male, while 29.6% were female. Similarly, among those who were overweight or obese, 12.6% were male, whereas 36.8% are female.
Overall, the prevalence of overweight and obesity in the study population is 49.4% (95% CI: 44.3–54.5%). This data highlights a higher prevalence of overweight and obesity among females compared to males.
Factors associated with overweight and obesity among PLHIV on ART
Following a bivariate model, we conducted an adjusted multivariable analysis and found sex and hypertension to be statistically significant predictors of overweight and obesity as reported in Table 2. Female patients were 2.4 times more likely to be overweight or obese than male patients (aOR: 2.4; 95% CI: 1.5–4.1; p < 0.001). Similarly, patients with hypertension were 2.5 times more likely to develop overweight or obesity compared to those without hypertension (aOR: 2.5; 95% CI: 1.6–4.1; p < 0.001). These findings underscore sex and hypertension as key risk factors for overweight and obesity among PLHIV on ART.
Discussion
This study found that 49.4% of PLHIV on ART were either overweight or obese. Overweight and obesity were more common among females (36.8%) than males (12.6%). Sex and hypertension were the only significant predictors of overweight and obesity. Education level, alcohol consumption, and physical activity were not significantly associated.
The sex difference in the prevalence of overweight and obesity among PLHIV on ART in this study aligns with trends observed across sub-Saharan Africa, where women living with HIV consistently report higher rates of overweight and obesity compared to their male counterparts. Similar findings were reported in Uganda, where 46% of PLHIV were overweight or obese, with a higher prevalence in females (55%) than males (30%)17. Similarly, a study in Tanzania found that 24.7% of women were obese compared to 9% of men18. These observations reflect broader regional patterns showing an increasing prevalence of overweight and obesity, particularly among women19.
. Additionally, metabolic and hormonal differences, particularly related to estrogen, may predispose women to higher fat accumulation20. In this study, female was more than twice at risk to be overweight or obese than male.
Hypertension was also strongly associated with overweight/obesity. People with hypertension were more than twice as likely to be overweight or obese compared to those without hypertension. This relationship has been extensively documented, as excess body weight is a major risk factor for hypertension due to increased vascular resistance, inflammation, and metabolic dysregulation21,22. Previous research among PLHIV has highlighted a growing burden of non-communicable diseases (NCDs), including hypertension, in this population23. The high prevalence of hypertension in overweight or obese individuals suggests the need for integrated care models addressing both metabolic health and HIV management.
Education level and physical activity did not show a significant relationship with overweight or obesity in our study. This contrasts with findings from Kenya and Nigeria, where higher education and sedentary behavior were associated with weight gain among PLHIV24,25. The discrepancy may be due to cultural, environmental, or sample-specific differences. It also underscores the importance of context-specific investigations into behavioral risk factors. Studies in Tanzania and South Africa have shown that engaging in vigorous physical activities reduces the likelihood of obesity, while light-intensity activities are associated with higher rates of weight gain18,26. Promoting moderate to high levels of physical activity among PLHIV may therefore offer a valuable strategy for managing weight and improving overall health.
Conclusion and recommendations
This study reveals a high prevalence of overweight and obesity (49.4%) among PLHIV on ART, with women disproportionately affected. Hypertension was strongly associated with overweight/obesity, highlighting the growing burden of NCDs among PLHIV. However, education level and physical activity were not significantly linked to obesity, suggesting the need for further research on context-specific risk factors.
From our findings, it is clear that to improve health outcomes for PLHIV, it is essential to implement targeted weight management strategies, with a particular focus on women who may be at higher risk. Additionally, HIV care models should include components focused on metabolic health to improve long-term outcomes.
Data availability
The dataset used during this study is not publicly available to maintain confidentiality. However, they can be obtained from the corresponding author upon reasonable request.
References
Health effects of overweight and obesity in 195 countries over 25 Years, New England J. Med. 377, 1 13–27. (2017). https://doi.org/10.1056/NEJMoa1614362
Obesity and overweight. & Accessed Feb. 02, 2025. [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Danquah, F. I. et al. Prevalence, incidence, and trends of childhood overweight/obesity in Sub-Saharan africa: a systematic scoping review. Arch. Public. Health. 78, 109. https://doi.org/10.1186/s13690-020-00491-2 (2020).
Kalinjuma, A. V. et al. Body mass index trends and its impact of under and overweight on outcome among PLHIV on antiretroviral treatment in rural tanzania: A prospective cohort study. PLoS ONE. 18 (8), e0290445. https://doi.org/10.1371/journal.pone.0290445 (2023).
Nalugga, E. A. et al. Prevalence of overweight and obesity and associated factors among people living with HIV attending a tertiary care clinic in Uganda. BMC Nutr. 8, 107. https://doi.org/10.1186/s40795-022-00604-w (2022).
Nkanjo, B. M. F., Tambe, A. B., Wefuan, R. F. & Ufuan, A. A. Sam Denise Movuh, Asu Carine Ndum, and Tendongfor Nicholas. Prevalence of Overweight/Obesity, Comorbidities, and Associated Factors Among Persons Living With HIV/AIDS on ART in Two Treatment Centers in the Fako Division, Cameroon: A Cross-Sectional Study. Int. J. Tropical Disease & Health 46 (2) 52–67. (2025). https://doi.org/10.9734/ijtdh/2025/v46i21629
Bakal, D. et al. Beatriz grinsztejn, obesity following antiretroviral therapy (ART) initiation is common and influenced by both traditional and HIV-/ART-Specific risk factors. Open Forum Infect. Diseases, 4 S37–S38, (2017.)https://doi.org/10.1093/ofid/ofx162.091
Bailin, S. S. et al. Obesity and weight gain in persons with HIV. Curr. HIV/AIDS Rep. 17, 138–150. https://doi.org/10.1007/s11904-020-00483-5 (2020).
Ronald Galdamez, J. A. et al. Félix gutiérrez, Mar masiá, Short-term increase in risk of overweight and concomitant systolic blood pressure elevation in Treatment-Naïve persons starting INSTI-Based antiretroviral therapy. Open. Forum Infect. Dis. 6 (12), ofz491. https://doi.org/10.1093/ofid/ofz491 (2019).
Simon, C. B. et al. High test–retest reliability of the alcohol use disorders identification Test-Consumption (AUDIT-C) questionnaire completed by primary care patients in routine care. Alcohol: Clin. Experimental Res. 48 (2), 302–308. https://doi.org/10.1111/ACER.15245 (2024).
Van Hout, M. et al. Decentralising chronic disease management in sub-Saharan africa: a protocol for the qualitative process evaluation of community-based integrated management of HIV, diabetes and hypertension in Tanzania and Uganda. BMJ Open. 14, e078044. https://doi.org/10.1136/bmjopen-2023-078044 (2024).
Karen, B. H., Pedersen, S. D., Poulsen, T. & Benfield 1522. Predictors of weight gain in people living with HIV. Open. Forum Infect. Dis. 10, Issue Supplement_2, https://doi.org/10.1093/ofid/ofad500.1357 ofad500.1357. (2023).
Johnston, C. S., Bliss, C., Knurick, J. R. & Scholtz, C. of diet quality in healthy adult omnivores and vegetarians. Nutr. J. 17 (1), 1–7. https://doi.org/10.1186/S12937-018-0399-X/TABLES/3 (2018). Rapid Eating Assessment for Participants [shortened version] scores are associated with Healthy Eating Index-2010 scores and other indices.
APA PsycNet Buy Page. Accessed: Feb. 03, 2025. [Online]. Available: https://psycnet.apa.org/buy/2014-44666-001
Lesage, F. X., Berjot, S. & Deschamps, F. Psychometric properties of the French versions of the perceived stress scale. Int. J. Occup. Med. Environ. Health. 25, 178–184. https://doi.org/10.2478/S13382-012-0024-8 (2012). 2.
R. The R Project for Statistical Computing. Accessed: 03, 2025. [Online]. Available: https://www.r-project.org/
Nalugga, E. A. et al. Prevalence of overweight and obesity and associated factors among people living with HIV attending a tertiary care clinic in Uganda. BMC Nutr. 8 (1 107). https://doi.org/10.1186/s40795-022-00604-w (2022).
Shayo, G. A. & Mugusi, F. M. Prevalence of obesity and associated risk factors among adults in Kinondoni municipal district, Dar Es Salaam Tanzania. BMC Public. Health. 11, 1, 1–7. https://doi.org/10.1186/1471-2458-11-365/TABLES/2 (2011).
Agyemang, C., Boatemaa, S., Frempong, G. A. & de-Graft Aikins, A. Obesity in Sub-Saharan Africa. Metab. Synd.. 1–13. https://doi.org/10.1007/978-3-319-12125-3_5-1 (2015).
Kanter, R. & Caballero, B. Global gender disparities in obesity: a review. Adv. Nutr. 3 (4), 491–498. https://doi.org/10.3945/AN.112.002063 (2012).
Bloomfield, G. S. et al. Hypertension and obesity as cardiovascular risk factors among HIV seropositive patients in Western Kenya. PLoS One. 6, 7, e22288. https://doi.org/10.1371/JOURNAL.PONE.0022288 (2011).
Ogunmola, O. J., Oladosu, O. Y. & Olamoyegun, A. M. Association of hypertension and obesity with HIV and antiretroviral therapy in a rural tertiary health center in nigeria: a cross-sectional cohort study. Vasc Health Risk Manag. 10, 129. https://doi.org/10.2147/VHRM.S58449 (2014).
Dakum, P. et al. Prevalence and risk factors for obesity among elderly patients living with HIV/AIDS in a low-resource setting. Medicine 100, 15, (e25399). https://doi.org/10.1097/MD.0000000000025399 (2021).
Mkuu, R. et al. Prevalence and factors associated with overweight and obesity in Kenya. Prev. Med. Rep. 22, 101340. https://doi.org/10.1016/J.PMEDR.2021.101340 (2021).
Pengpid, S. & Peltzer, K. The prevalence and associated factors of underweight and overweight/obesity among adults in kenya: evidence from a National cross-sectional community survey. Pan Afr. Med. J. 36 (338 -338). https://doi.org/10.11604/PAMJ.2020.36.338.21215 (2020).
Malaza, A., Mossong, J., Bärnighausen, T. & Newell, M. L. Hypertension and obesity in adults living in a high HIV prevalence rural area in South Africa. PLoS One. 7 10 ,e47761. https://doi.org/10.1371/JOURNAL.PONE.0047761 (2012).
Acknowledgements
The authors would like to acknowledge the administration of the Centre National Hospitalier et Universitaire Hubert Koutoukou Maga (CNHU-HKM) of Cotonou for allowing data collection in the institution and for their support and collaboration throughout the research process. We also thank the data collectors and respondents.
Author information
Authors and Affiliations
Contributions
Conceptualization was led by B.M.A and O.A.J.A. Field data collection was conducted by O.L.K, S.G.A., A. R. K. A, K.G.D.D. Database design and management were overseen by O.A.J.A and E.Y. Data curation responsibilities were shared among O.A.J.A and B.M.A. Formal analysis was performed by O.A.J.A. and B.M.A. Methodology development involved contributions from B.M.A. Supervision was provided by B.M.A and F.B.G.A. Visualization tasks were handled by O.A.J.A. The original draft of the writing was prepared by O.A.J.A and B.M.A . Writing review and editing involved O.A.J.A, B.M.A , O.L.K, S.G.A., A. R. K. A, K.G.D.D, E.Y, N.N.W, C.O.A, H.T.Z, F.A, F.B. G.A.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ale, O.A.J., Ale, B.M., Koutangni, O.L. et al. Prevalence and associated factors of overweight and obesity among people living with HIV on antiretroviral therapy in a national hospital in Benin. Sci Rep 15, 43593 (2025). https://doi.org/10.1038/s41598-025-06449-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-06449-0