Abstract
Antimicrobial Stewardship Programs (ASP) have demonstrated efficacy in lowering hospital expenditures and enhancing the judicious use of antibiotics. However, many hospitals in China have not yet established an ASP management model, and there is limited literature reporting successful ASP experiences. This study aimed to investigate the impact of ASP on Antibiotics Use Density (AUD). We conducted a retrospective study from October 2023 to September 2024 in a tertiary general hospital in Hangzhou, China. Based on audits of antibiotic orders conducted from October 1, 2023, to March 31, 2024, we identified potential factors contributing to high AUD. In line with the guidelines for implementing ASP, we established an ASP team and implemented comprehensive improvement strategies from April 1, 2024, to September 30, 2024. Following the implementation of ASP, the AUD decreased significantly by 31.01% from 54.20 prior to intervention to 37.39 post-intervention. The total Defined Daily Doses (DDDS) declined by 30.06% from 98,311.52 to 68,751.82, while the total cost of antibiotics fell by 5.81% from $1,798,309.53 to $1,693,918.44. Among 33 clinical departments within the hospital, 31 demonstrated a reduction in AUD. Furthermore, the AUD proportion of tetracyclines and quinolone antibacterials decreased from 6.68 to 2.54% and from 25.63 to 21.10%, respectively. This study demonstrates that ASP is a viable and effective approach for reducing AUD and DDDS of antibiotics, as well as lowering the overall cost of antibiotics, and has the potential to enhance the quality of antimicrobial prescribing.
Similar content being viewed by others
Introduction
Antimicrobial agents play a pivotal role in modern medicine and are among the most frequently prescribed medications during hospital admissions1. However, their irrational use has emerged as a significant public health concern globally, with estimates indicating that approximately 30–50% or more of inpatient antibiotic usage is unnecessary or suboptimal2. In China, despite the issuance of key documents such as the Guiding Principles for the Clinical Application of Antibiotics, the Notice on Continuing to Enhance Management of Clinical Antibiotic Use, and the National Action Plan for Containment of Microbial Resistance (2022–2025) in recent years aimed at strengthening antibiotic management practices, issues related to irrational antibiotic use and escalating antimicrobial resistance remain pressing challenges that require urgent attention.
The Antibiotics Use Density (AUD) serves as an important metric reflecting both the breadth and depth of antimicrobial drug utilization3; it is a critical indicator for assessing the rationality of antimicrobial use within hospitals. Following the normalization of COVID-19 prevention and control measures alongside centralized procurement processes for national pharmaceuticals in China, standardized application protocols for antimicrobials have faced considerable obstacles. Disparities in clinicians’ understanding of antimicrobials, coupled with inconsistent levels of clinical management across healthcare institutions—have contributed to persistently elevated AUD and instances of irrational antimicrobial usage.
In response to this challenge, a study has revealed that 82% of leading US hospitals have established Antimicrobial Stewardship Programs (ASP) to promote the rational use of antimicrobial agents through scientific and systematic management measures4.ASP encompasses a series of interventions aimed at optimizing antimicrobial use while ensuring sustainable access to effective therapies for all patients in need5,6 Evidence indicates that ASP, which has demonstrated efficacy in lowering hospital expenditures and enhancing the judicious use of antibiotics, was crucial for mitigating antimicrobial resistance7. Implementation of a multidisciplinary ASP for high-risk neutropenia patients was associated with lower carbapenem and glycopeptide use and improved clinical outcomes8. Pediatric ASPs have a significant impact on the reduction of targeted and empiric antibiotic use, healthcare costs, and antimicrobial resistance in both inpatient and outpatient settings9. However, to our knowledge, many hospitals in China have not yet established ASP management model10and there are few literature reports on successful experiences with ASP11. This study aims to investigate the impact of Antimicrobial Stewardship Programs on Antibiotics Use Density in a tertiary general hospital.
Methods
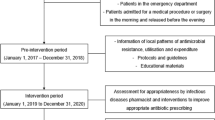
Study design, setting, and ethics
The present study was conducted in the Cuiyuan District of Tongde Hospital of Zhejiang Province, a tertiary general hospital in China. The hospital consists of 33 clinical departments and serves approximately 50,000 discharged patients while accommodating around 1.5 million outpatient visits annually. Based on the analysis of audits on antibiotic orders conducted from October 1, 2023, to March 31, 2024, we identified potential factors contributing to high Antibiotic Use Density (AUD). This study was approved by Tongde hospital of Zhejiang province. In line with the guidelines for implementing ASP12we established an ASP team and implemented comprehensive improvement strategies from April 1, 2024, to September 30, 2024. The effectiveness of the ASP strategy was evaluated by comparing relevant antibiotic usage indicators before and after the intervention. All data were obtained through the Hospital Information System (HIS) and BI Decision Analysis System. This study was conducted in accordance with the Declaration of Helsinki. As this research was a methodological study concentrating solely on management and does not pertain to patient privacy, the Ethics Committee of Tongde Hospital of Zhejiang Province has exempted it from ethical approval and the need to obtain informed consent.
Outcomes and measurement
The primary outcome measures included the variations in AUD before and after the ASP intervention, changes in Defined Daily Doses (DDDS), the total cost of antibiotics administered, variations in AUD across different clinical departments, shifts in AUD for various antibiotic classes, as well as the AUD ratio and AUD descender.
The Antibiotic Use Density (AUD), measured as Defined Daily Doses (DDDs) consumed per 100 patient-days (DDDs/100 PD), quantifies the intensity of antibiotic exposure among inpatients by normalizing total antimicrobial usage against cumulative patient hospitalization time. As a critical indicator for institutional antibiotic stewardship, AUD is also a key metric in the performance evaluation of third-tier public hospitals in China, with a compliance threshold of ≤ 40 DDDs/100 PD for third-tier general hospitals. The Defined Daily Dose (DDD), established by the World Health Organization (WHO) as the assumed average daily maintenance dose for a drug’s primary adult indication, serves as the foundational metric for quantifying antimicrobial consumption. In this study, the total Defined Daily Doses (DDDs) were calculated by summing standardized daily doses across all antimicrobials: for each drug, DDDs was derived by dividing total milligram consumption by its WHO-assigned DDD (mg/DDD) for the relevant therapeutic indication, with values sourced from the 2024 WHO ATC/DDD Index13. The AUD was calculated using total DDDs divided by total length of stay × 100.
The total cost of antibiotics was defined as the cumulative expenditure for all antibiotics administered during the study period. The exchange rate used was 1 USD = 7.316 CNY.
Based on the Anatomical Therapeutic Chemical (ATC) classification system of WHO in 202413, the impact of clinicians on their propensity to prescribe specific antimicrobials was assessed using the AUD ratio and AUD descender. The AUD ratio (%) was calculated as the proportion of AUD for a particular class of antibacterial agents, either prior to or following ASP intervention, relative to the overall AUD across all classes during that period, multiplied by 100%. The AUD descender (%) was computed as (AUD after ASP intervention—AUD before ASP intervention) / AUD before ASP intervention × 100%.
Potential factors contributing to high AUD
In accordance with the antibiotic usage data from Tongde Hospital of Zhejiang Province, the expert group on rational use of antibiotics conducted an evaluation of antibiotic utilization within the hospital from October 1, 2023 to March 31, 2024 (before ASP intervention group). This review encompasses aspects such as indications for use, selection of antibiotic varieties, timing and routes of administration, and treatment duration. The primary factors contributing to high AUD were identified as follows: (1) Absence of clear indications for antibiotic use; (2) Inappropriate selection of antibiotics; (3) Unreasonable duration of antibiotic therapy; (4) Inappropriate combination therapies; and (5) Insufficient support from information technology systems.
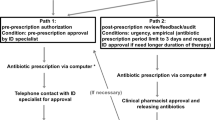
Antimicrobial stewardship programs
The ASP-based intervention was formally implemented on April 1, 2024 and announced to clinical departments within the hospital. The ASP team consists of medical department, hospital infection control department, clinical anti-infection experts, clinical pharmacists, microbiological examination experts, and radiologists. The specific responsibilities of each component are shown in Fig. 1. The ASP management team held a regular meeting every two weeks to analyze and discuss the current status of antimicrobial drug management and difficult clinical cases, put forward opinions and suggestions, and clarify the key work direction in the next stage.
To assist clinicians in making precise evaluations of drug efficacy, the ASP team has successfully established a monitoring program for antimicrobial drug blood concentration and compiled the Standard Manual of Therapeutic Drug Monitoring in Tongde Hospital of Zhejiang Province, which is aimed at guiding clinicians and nurses in standardized sampling operations. At present, the blood concentration of twenty-two commonly used antibiotics (such as carbapenems, beta-lactam drugs, vancomycin, tigacycline, etc.) can be monitored in our hospital. Based on the results of blood drug concentration monitoring, clinical pharmacists collaborate with clinicians to optimize the selection, dosage, and administration frequency of antibiotics. For dosage adjustment, they compare measured blood drug concentrations against the target therapeutic range. When the concentration falls below the effective threshold, the dosage is increased to ensure sufficient antimicrobial activity. Conversely, if the concentration exceeds the therapeutic window, potentially posing a risk of toxicity, the dosage is promptly reduced. In terms of administration frequency optimization, guided by the pharmacokinetic and pharmacodynamic (PK/PD) properties of antibiotics, the administration frequency is tailored. For concentration-dependent antibiotics, such as aminoglycosides, a once-daily high-dose regimen is often recommended to maximize the peak concentration-to-minimum inhibitory concentration (Cmax/MIC) ratio. In contrast, for time-dependent antibiotics like β-lactams, more frequent dosing or extended infusions are preferred to maintain the drug concentration above the MIC for an optimal duration. In addition, clinical pharmacists conducted routine pharmaceutical rounds and reviewed physician orders, performed targeted analyses of drug utilization, provided education on rational drug use, and delivered tailored training regarding antibiotic selection, dosing regimens, and treatment duration based on the specific disease types managed by each department.
In terms of information system improvement, the ASP team has first enhanced the Rational Drug Use Information System purchased from Hangzhou Yiyao Information Technology Co., Ltd. in 2019. This system enables real-time review of physicians’ prescriptions/medical orders and triggers alerts for irrational medication14. To further promote rational antibiotic use, the ASP team has integrated clinical guidelines for judicious antibiotic use into the system and implemented proactive prompts and real-time reminders to enhance clinicians’ compliance with evidence-based antibiotic prescribing practices. Furthermore, information technology was applied to establish specific protocols and limits for clinician accounts based on the classification of various antibiotics in the Hospital Information System (HIS). Additionally, the ASP team has devised a program for prophylactic antimicrobial use during the perioperative period to mitigate instances of misuse.
Statistical methods
All statistical analyses were conducted using SPSS statistical software (version 25.0). All data are expressed as number and percentage. The Chi-square test and T test were employed for intergroup comparisons, with a significance level set at p < 0.05.
Results
The change of AUD and DDDs before and after ASP
Table 1 shows that there was a significant reduction in AUD with the implementation of ASP intervention, decreasing by 31.01% from 54.20 DDDs/100PD to 37.39 DDDs/100PD (P < 0.05). Moreover, DDDS also decreased by 30.06% from 98,311.52 before ASP intervention to 68,751.82 after ASP intervention, showing a significant difference (P < 0.05). However, no significant decrease was observed in total length of stay of discharged patients in the same period after the ASP intervention (181,389 vs. 183,887, p = 0.883), as it was shown in Table 2.
The change of total cost of antibiotics, the AUD in different clinical departments before and after ASP
With the implementation of ASP, the total cost of antibiotics for inpatients declined by 5.81%from $1,798,309.53 prior to the intervention to$1,693,918.44 after the intervention, as it was shown in Fig. 2. Table 3 presents the alteration results of AUD in clinical departments. This study encompassed 33 clinical departments in our hospital, and AUD decreased in 31 of them after the ASP intervention.
The change of AUD, AUD descender and AUD ratio in main classification before and after ASP
Another aspect of our investigation focused on the influence of ASP interventions on clinicians’ antibiotic prescribing practices. Following ASP intervention, the AUD ratio was observed to decline with Tetracyclines (6.68% vs. 2.54%), Quinolone antibacterials (25.63% vs. 21.10%), Antimycotics for systemic use (9.50% vs. 7.44%), Macrolides, Lincosamides and Streptogramins (6.11% vs. 5.43%), Aminoglycoside antibacterials (0.48% vs. 0.40%), Other antibacterials (6.05% vs. 4.81%). In contrast, the AUD ratio for Beta-lactam antibacterials, Penicillins rose from 12.20 to 13.75%, while that for Other Beta-lactam antibacterials increased from 33.36 to 44.53%. The detailed results are presented in Table 4.
Discussion
Antimicrobial management is a critical component of clinical medical quality governance, with the AUD serving as the primary evaluation criterion for the use and rationality of antibacterial agents15. It also functions as a key performance indicator in assessing national public hospitals in China. In certain hospitals within developing countries16,17the AUD remains elevated due to evolving disease profiles, limited availability of alternative antibacterial drug options, clinicians’ empirical experiences with antibiotics, and instances of irrational antibiotic usage—factors that contribute to increased bacterial drug resistance. Consequently, there is an urgent need for an effective management paradigm.
Our research findings indicate that following the implementation of an Antimicrobial Stewardship Program over six months, the AUD for antimicrobial agents decreased by 31.01% from 54.20 DDDs/100PD to 37.39 DDDs/100PD. The change in AUD before and after ASP intervention reveals that it peaked at 61.39 DDDs/100PD in November 2023, significantly exceeding the target value of 40. However, subsequent to implementing ASP measures, there was a gradual decline in AUD for antibacterial drugs; each month’s AUD fell below the target threshold of 40. Simultaneously, DDDS also diminished by 30.06% from 98,311.52 to 68,751.82 (p < 0.05). In comparison, a German study reported a 25% reduction in total antibiotic use (p < 0.001), with pre-intervention levels of 129.078 DDDs/100 patient days dropping to 96.826 DDDs/100 patient days post-intervention18. Meanwhile, an Indian study observed an 18.72% reduction in total DDDs per 100 patient days following ASP implementation19. Overall, these research findings underscore the significant regional disparities in management intervention strategies. Our study demonstrated the most substantial reduction in DDDs, potentially attributable to the proactive implementation of policies. Conversely, the decline in DDDs observed in Germany and India aligns with the characteristics of their respective healthcare environments and the scope of interventions.
Reductions in AUD were observed across 31 out of the hospital’s total of 33 clinical departments. The significant reduction in AUD (more than 50%) in the Radiotherapy Department, Reproductive Immunology Department, Obstetrics Department and Ophthalmology Department can be attributed to targeted interventions. In the Radiotherapy Department, antimicrobial prophylaxis was optimized by reducing systemic antibiotics and prioritizing topical agents for radiation-induced conditions. The Reproductive Immunology Department shifted from empiric to targeted therapy, eliminating unnecessary antibiotics for unproven infections. In the Obstetrics Department, perioperative antibiotic prophylaxis was rationalized, shortening durations for cesarean sections and restricting use in vaginal deliveries. The Ophthalmology Department transitioned from systemic to topical antimicrobials for most eye infections. Conversely, in the Critical Care Medicine, a 20% increase in bed capacity combined with the introduction of advanced life support technologies (e.g., ECMO) has led to a higher influx of critically ill patients with heightened susceptibility to infections. Prolonged invasive interventions (e.g., mechanical ventilation, vascular catheters) and extended hospital stays in this population contribute to an elevated risk of multidrug-resistant (MDR) infections, consequently driving the need for broader-spectrum antibiotic use and increased AUD. In the Neurosurgery Department, the establishment of a brain trauma diagnosis and treatment center has resulted in a surge of postoperative patients with central nervous system (CNS) infections or severe traumas, primarily due to the referral of more complex cases requiring specialized care. The high-risk nature of neurosurgical procedures and the severity of traumatic injuries necessitate extended periods of antibiotic prophylaxis and targeted therapy to prevent or treat infections like meningitis. This has directly contributed to increase AUD in the department, reflecting both the volume of high-complexity cases and the clinical imperative for aggressive antimicrobial stewardship in neurocritical care.
Economic data indicated that ASP significantly influenced antibiotic utilization, resulting in a $104,391.08 reduction in the total cost of antibiotics for inpatients .Many studies have confirmed that ASP intervention can effectively reduce patients’ economic expenditure, such as the study from Hongyan Gu et al.20antimicrobial stewardship demonstrated a significant financial return on investment with the median cost of antibiotics decreased markedly from $836.30 to $362.15 per patient stay, while the median cost of all medications fell from $2,868.18 to $1,941.50 per patient stay, which is consistent with our findings. Another study by Anne M. Voermans in the Netherlands demonstrated that procalcitonin-guided therapy achieved significant cost savings in infectious disease management21aligning with our findings. The intervention resulted in $25,611 in cost savings per sepsis case and $3,630 per lower respiratory tract infection case by reducing unnecessary antibiotic exposure and optimizing treatment duration. This supports the effectiveness of diagnostic stewardship—such as using biomarkers like procalcitonin to guide antimicrobial decisions—as a key component of ASPs. Notably, there was no statistically significant change in total length of stay of discharged patients in the same period after the ASP intervention (181,389 vs. 183,887, p = 0.883), this suggests that our ASP initiative effectively reduced the aggregate quantity of antimicrobials administered to patients.
An evaluation of the change of AUD ratio for antibacterial agents before and after ASP intervention indicates that our efforts primarily curtailed usage among Tetracyclines, Quinolone antibacterials and Antimycotics for systemic use. Conversely, the AUD ratio for Beta-lactam antibacterials, Penicillins rose from 12.20 to 13.75%, while Other Beta-lactam antibacterials increased from 33.36 to 44.53%. As reported by Antonios Markogiannakis et al., only 47% of antifungal prescriptions were appropriate before intervention22underscoring the critical need for antimicrobial stewardship in this domain. Our study demonstrated a statistically significant 46.02% reduction in the AUD for systemic antimycotics (J02A), which dropped from 5.15 to 2.78 DDDs/100 patient-days, with the ratio falling from 9.50 to 7.44%. This was primarily attributed to ASP interventions, including shifting from empiric to diagnostics-guided therapy (requiring microbiological confirmation before prescribing), optimizing doses, restricting prophylaxis to evidence-based high-risk populations, educating clinicians on resistance risks, and aligning with international guidelines (e.g., IDSA and ECIL recommendations).It also shows that the ASP expert group has a guiding effect on the rational use of broad-spectrum antibiotics, which is consistent with the results of other studies23,24.
ASP is essential for optimizing clinical outcomes, preventing infections, and minimizing healthcare costs25. In addition to the 6-month ASP intervention, this study presents several notable advantages. The implementation of ASP not only yields measurable outcomes such as a reduction in AUD, but also generates significant intangible benefits. For instance, through targeted training and education, ASP enhances medical staff’s awareness regarding the rational use of antimicrobials, fosters knowledge advancement and professional development, and facilitates interdisciplinary collaboration and information exchange among clinicians, clinical pharmacists, and microbiological experts.
The study has several limitations. Firstly, as a single-center, six-month pre-post ASP intervention study, the management models of antimicrobial drugs and the responsibilities of ASP working groups personnel vary across hospitals, which may limit the generalizability of our research methods and results to other settings. Additionally, the study did not assess changes in antimicrobial resistance (AMR) patterns of pathogenic bacteria associated with ASP implementation, which is critical for evaluating the program’s long-term impact on curbing resistance. Furthermore, throughout the ASP implementation, clinicians’ knowledge gaps regarding antimicrobial drugs were evident, with empirical prescribing persisting in certain departments, highlighting the need for continuous education on drug mechanisms of action and standardized use. To address these limitations, future studies should incorporate more rigorous designs, such as prospective multi-seasonal monitoring, integration of real-time epidemiological data, and longitudinal tracking of AMR trends.
Conclusions
In conclusion, this study demonstrates that ASP is a viable and effective approach for reducing AUD and DDDS of antibiotics, as well as lowering the overall cost of antibiotics, and has the potential to enhance the quality of antimicrobial prescribing. Further research is necessary to validate these findings and identify specific activities associated with the greatest benefits.
Data availability
The datasets used in this study are available from the corresponding author upon request.
References
Zay Ya, K. et al. Association between antimicrobial stewardship programs and antibiotic use globally: A systematic review and meta-analysis. JAMA Netw. Open 6(2), e2253806 (2023).
Johnson, M. D. et al. Top myths of diagnosis and management of infectious diseases in hospital medicine. Am. J. Med. 135(7), 828–835 (2022).
GBD 2021 Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance 1990–2021: A systematic analysis with forecasts to 2050. Lancet 404(10459), 1199–1226 (2024).
Nhan, D., Lentz, E. J. M., Steinberg, M., Bell, C. M. & Morris, A. M. Structure of antimicrobial stewardship programs in leading US hospitals: Findings of a nationwide survey. Open. Forum Infect. Dis. 6(4), ofz104. https://doi.org/10.1093/ofid/ofz104 (2019). PMID: 30968055; PMCID: PMC6451647.
Nelson, G. E. et al. Principles and practice of antimicrobial stewardship program resource allocation. Infect. Dis. Clin. North. Am. 37(4), 683–714 (2023).
Murphy, C. V. et al. Antimicrobial stewardship in the ICU. Semin Respir Crit. Care Med. 43(1), 131–140 (2022).
Taylor, M. G. & Palazzi, D. L. Antimicrobial stewardship in the pediatric primary care setting. Pediatr. Ann. 51(5), e196–e201 (2022).
Contejean, A. et al. Antimicrobial stewardship in high-risk febrile neutropenia patients. Antimicrob. Resist. Infect. Control. 11(1), 52 (2022).
Knowles, R. et al. A systematic review of national interventions and policies to optimize antibiotic use in healthcare settings in England. J. Antimicrob. Chemother. 79(6), 1234–1247 (2024).
Lee, C. F. et al. Impact of antibiotic stewardship programmes in asia: A systematic review and meta-analysis. J. Antimicrob. Chemother. 73 (4), 844–851. https://doi.org/10.1093/jac/dkx492 (2018).
Ji, W. et al. Antimicrobial stewardship programs in Northwest china: A Cross-Sectional survey of perceptions, involvement, and perceived barriers among hospital pharmacists. Front. Pharmacol. 12, 616503. https://doi.org/10.3389/fphar.2021.616503 (2021).
Frey, E. et al. 2022 AAFP/AAHA antimicrobial stewardship guidelines. J. Am. Anim. Hosp. Assoc. 58(4), 1–5 (2022).
WHO Collaborating Centre for Drug Statistics Methodology. ATC classification index with DDDs (Oslo, Norway, 2024). https://atcddd.fhi.no/atc_ddd_index/
Guo, S., Du, W., Chen, S., Guo, X. & Ju, X. Exploring the impact of the rational antibiotic use system on hospital performance: the direct effect and the spillover effect. Int. J. Environ. Res. Public. Health 16(18), 3463. https://doi.org/10.3390/ijerph16183463 (2019).
Durand, C. et al. Efficacy of an antimicrobial stewardship intervention for early adaptation of antibiotic therapy in high-risk neutropenic patients. Antimicrob. Resist. Infect. Control 13(1), 5 (2024).
Park, M. et al. The effectiveness of an antimicrobial stewardship program in an Australian rural hospital. Aust J. Rural Health. 31(3), 522–531 (2023).
Divecha, C. A., Tullu, M. S. & Karande, S. Challenges in implementing an antimicrobial stewardship program (ASP) in developing countries. J Postgrad. Med 10 (2024).
Feihl, S. et al. Effect of an intensified antibiotic stewardship program at an orthopedic surgery department. Surg. Infect. (Larchmt) 23(2), 105–112. https://doi.org/10.1089/sur.2021.040 (2022).
Zirpe, K. G. et al. Impact of an antimicrobial stewardship program on broad spectrum antibiotics consumption in the intensive care setting. Indian J. Crit. Care Med. 27(10), 737–742. https://doi.org/10.5005/jp-journals-10071-24543 (2023).
Gu, H. et al. Benefits of pharmacist intervention in the critical care patients with infectious diseases: A propensity score matching retrospective cohort study. Aust Crit. Care 36(6), 933–939 (2023).
Voermans, A. M., Mewes, J. C., Broyles, M. R. & Steuten, L. M. G. Cost-effectiveness analysis of a procalcitonin-guided decision algorithm for antibiotic stewardship using real-world U.S. hospital data. OMICS 23(10), 508–515. https://doi.org/10.1089/omi.2019.0113 (2019).
Markogiannakis, A. et al. Impact of a non-compulsory antifungal stewardship program on overuse and misuse of antifungal agents in a tertiary care hospital. Int. J. Antimicrob. Agents 57(1), 106255. https://doi.org/10.1016/j.ijantimicag.2020.106255 (2021).
Pasquau-Liaño, J. et al. Timing in antibiotic therapy: When and how to start, de-escalate and stop antibiotic therapy. Proposals from a stablished antimicrobial stewardship program. Rev. Esp. Quimioter 35 (Suppl 3(Suppl 3), 102–107 (2022).
Tuon, F. F. et al. eHealth and mHealth in antimicrobial stewardship to reduce mortality in empirical antimicrobial therapy and a systematic review with a Meta-Analysis of adequate therapy. Infect. Dis. Rep. 16(4), 707–723 (2024).
Telles, J. P. et al. Optimization of antimicrobial stewardship programs using therapeutic drug monitoring and pharmacokinetics-pharmacodynamics protocols: A cost-benefit review. Ther. Drug Monit. 45(2), 200–208 (2023).
Acknowledgements
The authors thank the clinical staff at Tongde Hospital of Zhejiang Province for their excellent work.
Funding
This work was supported by Zhejiang Traditional Chinese Medicine Science and Technology Program (grant number: 2024ZF044, 2022ZA033).
Author information
Authors and Affiliations
Contributions
C.X, Y.T and M.Z designed the study; B.Y, L.P, B.Z, Y.Y, P.F, W.Y, H.J, J.Z and B.H collected data; Q.Z and Y.L analyzed the data; C.X wrote the first draft of the manuscript; M.Z and Y.T provided feedback, interpreted the data, and assisted in the review of the final manuscript; all authors commented on previous versions of the manuscript and read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xin, C., Yang, B., Pang, L. et al. Antimicrobial stewardship reduces antibiotic use density and cost in a Chinese tertiary hospital. Sci Rep 15, 23609 (2025). https://doi.org/10.1038/s41598-025-06622-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-06622-5