Abstract
The ratio of non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol (NHHR) is an emerging lipid parameter. An association has been demonstrated with cardiovascular mortality. This study aimed to investigate the link between NHHR and mortality among hypertensive patients.This study utilized data from the National Health and Nutrition Examination Survey (NHANES) conducted in the United States from 1999 to 2018. The NHHR was derived from the lipid index. The association between NHHR and mortality in hypertensive patients was evaluated using multivariate Cox regression and Kaplan-Meier survival analysis, with restricted cubic spline curves (RCS) illustrating the nonlinear relationship. Subgroup analyses were conducted to assess the association’s stability. The study included 16,259 patients with hypertension. Multivariate Cox regression analyses, adjusted for covariates, indicated that patients in NHHR quartiles Q2 and Q3 exhibited a 14% and 16% reduced risk of all-cause mortality, and a 32% and 33% reduced risk of cardiovascular mortality, respectively, compared to those in Q1. RCS analyses revealed a U-shaped relationship between NHHR and both all-cause and cardiovascular mortality in patients with hypertension. Subgroup analyses further maintained the robustness of this association across most subgroups. In hypertensive patients, NHHR exhibits a U-shaped relationship with both all-cause and cardiovascular mortality. This finding suggests that NHHR may serve as a new predictor of future mortality risk in hypertensive patients, providing a new marker for prognostic prevention in this special population.
Similar content being viewed by others
Introduction
The Global Burden of Disease Study estimates that hypertension will account for 226 million disability-adjusted life years (DALYs) in 2021. The United States ranks among the top five countries with the highest absolute global burden. In 2021, hypertension-related deaths are projected to reach 10.85 million, with an age-standardized mortality rate of 131.10 per 100,000 individuals1. The global burden of DALYs attributable to hypertension has increased approximately twofold over the past three decades2. Globally, hypertension is the leading cause of cardiovascular disease (CVD) and significantly contributes to heart failure, renal failure, and stroke in adults3,4,5. CVD represents the primary cause of mortality among hypertensive patients, with an elevated risk of death attributable to structural alterations in the heart, vascular occlusion, and arrhythmias precipitated by hypertension6,7. The search for convenient and effective biomarkers is important because of the high mortality rate and the insidious nature of hypertension in the early stages.
Previous studies have shown that non-high-density lipoprotein cholesterol (non-HDL-C), low-density lipoprotein (LDL), and total cholesterol (TC) are associated with an increased risk of hypertension8,9. There are also studies combining different lipid metrics, such as the association of the lipid ratio TC/ high-density lipoprotein cholesterol (HDL-C) with cardiovascular mortality in the general population, and LDL/HDL-C is associated with all-cause mortality in an elderly hypertensive population10,11. However, they did not take into account non-HDL, which is strongly associated with hypertension. The newly established metric, the non-HDL-C to HDL-C ratio (NHHR), offers significant insights into the impact of lipid particles on CVD development. This metric has been shown to have a more pronounced impact on disease risk than traditional lipid markers, highlighting the potential benefits of incorporating NHHR into risk assessment tools12,13,14. An increasing number of diseases are associated with NHHR15. Patients with hypertension often exhibit lipid metabolism disorders16. These disorders elevate the risk of cardiovascular disease and are linked to higher mortality, especially from CVD. Nonetheless, the link between NHHR and mortality in hypertensive patients remains insufficiently explored.
This research examined the relationship between NHHR and both all-cause and cardiovascular mortality in hypertensive patients using extensive, long-term data from the National Health and Nutrition Examination Survey (NHANES), highlighting NHHR’s potential significance in this demographic. The study’s findings could aid in advancing research on developing effective prevention strategies and interventions.
Methods
Study population
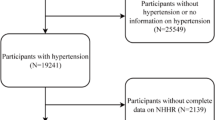
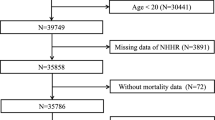
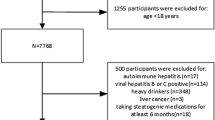
The data used in this study were obtained from the NHANES database, which includes the records of participants from 1999 to 2018. In total, 59,064 individuals were recruited for the study. The National Center for Health Statistics (NCHS) Research Ethics Review Board approved the study protocol, and all participants gave informed consent to the Declaration of Helsinki17. The exclusion criteria included: (1) individuals with normal blood pressure, (2) those lacking data necessary for NHHR calculation, (3) participants aged 20 years or younger, and (4) subjects with incomplete data on essential covariates. A total of 16,259 hypertension patients were included for further analysis (Fig. 1).
Data collection
The data set comprised basic clinical information and test indicators collected from the cohort of hypertensive patients included in the study. Collected basic information comprised age, sex, race, body mass index (BMI), poverty income ratio (PIR), education, marital status, and tobacco and alcohol use. Electrolyte indicators included sodium, potassium, and calcium. Blood biochemical indicators analyzed included urea nitrogen, creatinine, uric acid, alanine aminotransferase (ALT), and aspartate aminotransferase (AST). Furthermore, all individuals with hypertension were included in the analysis to examine the relationship between hypertension and CVD.
NHHR
TC and HDL-C levels were extracted from the NHANES database. The NHHR is calculated using the formula: NHHR = (TC - HDL-C) / HDL-C.
Statistical analyses
Comparisons between multiple groups of continuous variables were conducted using either a one-way ANOVA and were expressed as mean ± standard error. Categorical variables were presented as counts and percentages, with group differences assessed via the chi-square test. Kaplan-Meier survival analysis assessed the relationship between NHHR and both all-cause and cardiovascular mortality in hypertensive patients. Three Cox proportional hazards regression models were employed to analyze the association between NHHR and mortality in hypertensive populations, with restricted cubic splines (RCS) illustrating the dose-response relationship. Subgroup analyses were performed to assess the consistency of the relationship between NHHR and mortality rates across various subgroups.
Analyses were conducted using R software (version 4.1.3), with statistical significance set at P < 0.05.
Results
Baseline characteristics of participants
A total of 16,259 patients with hypertension were included in this study (Table 1). The male population constituted 49.85%, with an average age of 56.62 ± 0.21 years. The entire population was divided into four groups according to the NHHR values (Q1 ≤ 2.063, 2.063 < Q2 ≤ 2.836, 2.836 < Q3 ≤ 3.843 and Q4 > 3.843). Patients in Q4 had the highest BMI, the lowest PIR, the least non-Hispanic Black and above high school, and the most married. In terms of laboratory data, patients in Q4 had the highest sodium, calcium, uric acid, ALT, and AST. In terms of lifestyle habits, participants in Q4 had the highest number of smokers and heavy drinkers. In terms of lifestyle habits, participants in Q4 had the highest number of smokers and heavy drinkers. Q4 participants exhibited the highest incidence of comorbid diabetes and the lowest incidence of comorbid CVD (P < 0.05).
Kaplan-Meier survival curves analyzing mortality among hypertensive patients
Kaplan-Meier curve analysis was conducted to evaluate the association between NHHR and the cumulative risk of all-cause and cardiovascular mortality in hypertensive patients. Kaplan-Meier curves indicated that, without covariate adjustment, hypertensive patients with higher NHHR levels exhibited lower all-cause mortality (Fig. 2A, log-rank P < 0.001). Cardiovascular mortality initially decreased and then increased with rising NHHR levels, reaching its lowest in patients with NHHR in Q3 (Fig. 2B, log-rank P < 0.001).
Analysis of multivariate regression on the link between NHHR and mortality in patients with hypertension
To investigate the independent correlation between NHHR and mortality in hypertensive patients, three different models were developed (Table 2). Model 1 was unadjusted, Model 2 included adjustments for age, sex, race, and PIR, while Model 3 incorporated additional adjustments for BMI, sodium, potassium, calcium, urea nitrogen, creatinine, uric acid, ALT, AST, alcohol consumption, smoking, marital status, diabetes, and CVD. In Model 1, an increase in NHHR was associated with a decreased risk of all-cause mortality, while the risk of cardiovascular mortality initially increased before decreasing (P < 0.05). In Model 3, patients in the NHHR Q2 and Q3 groups exhibited a significantly reduced risk of all-cause mortality by 14% and 16%, and cardiovascular mortality by 22% and 23%, respectively, compared to the Q1 group (P < 0.05). No significant differences were observed for patients in Q4 relative to Q1 (P > 0.05).
Investigation of the dose-response relationship between NHHR and mortality in hypertensive patients
A dose-response model utilizing restricted cubic splines (RCS) was employed to examine nonlinear trends in the association between NHHR and both all-cause and cardiovascular mortality. The RCS analysis revealed a significant U-shaped association between NHHR and both all-cause mortality (P overall < 0.05, P nonlinear < 0.001, Fig. 3A) and cardiovascular mortality (P overall < 0.05, P nonlinear = 0.003, Fig. 3B). As NHHR increases, all-cause mortality and cardiovascular mortality in hypertensive patients show a first decrease, which reaches a minimum and then increases. And this lowest threshold is 2.84.
Analysis of the relationship between NHHR and mortality among hypertensive patients, focusing on specific subgroups
The study further examined the robustness of the NHHR-mortality relationship by analyzing subgroups categorized by clinical characteristics, including age, gender, smoking, drinking, diabetes, and CVD (Fig. 4). The study found a strong association between NHHR and both all-cause and cardiovascular mortality in hypertensive patients across most subgroups. Additionally, diabetes significantly influenced the relationship between NHHR and all-cause mortality in these patients (P for interaction < 0.05).
Discussion
This extensive study of 16,259 hypertension patients revealed a significant U-shaped relationship between NHHR and both all-cause and cardiovascular mortality. Furthermore, the all-cause mortality was found to be lower for non-diabetic individuals compared to those with diabetes in the subgroup analyses. After adjusting for confounding factors, the association between NHHR and mortality remained significant. Hypertensive patients in the Q2 and Q3 quartiles exhibited a reduced risk of all-cause and cardiovascular mortality, respectively, compared to those in the Q1 quartile.
NHHR is a newly developed composite lipid indicator extensively studied in numerous research works. A significant correlation has been identified between NHHR and an increased prevalence of depression and sleep disorders among US adults18,19. In terms of renal pathology, elevated NHHR concentrations are strongly associated with an elevated risk of kidney stone occurrence and recurrence, and several studies have demonstrated a significant “J” shaped relationship between NHHR and diabetic nephropathy20,21,22. Moreover, NHHR has a strong correlation with low muscle mass, hyperuricemia, and the development of gallbladder stones23,24,25. An increased NHHR is associated with a higher risk of type 2 diabetes mellitus (T2DM) in metabolic diseases26. Additionally, a negative correlation has been observed between NHHR and vitamin D in patients with T2DM27. Among US adults with diabetes or prediabetes, a U-shaped association exists between NHHR and all-cause mortality, while an L-shaped association is observed between NHHR and cardiovascular mortality28. NHHR is a reliable predictor of coronary artery disease severity in ST-elevated myocardial infarction (STEMI) patients and serves as a significant independent risk factor, especially for those without prior lipid-lowering treatment29. Furthermore, a U-shaped relationship exists between its levels and the incidence of cardiovascular events in patients undergoing percutaneous coronary intervention30.
Our findings suggest that NHHR is U-shaped and associated with all-cause mortality and cardiovascular mortality in hypertensive patients, and the mechanisms behind this may be several. Firstly, NHHR may affect cardiovascular outcomes by influencing the inflammatory response. Studies have shown that oxidized non-HDL particles interacting with immune cells and endothelial cells can activate the inflammatory process, whereas HDL exerts an anti-inflammatory effect by increasing α-1-antitrypsin binding31,32,33. This association suggests that the NHHR may increase cardiovascular risk by promoting the inflammatory response. In hypertensive patients, the inflammatory state may further exacerbate the development of vascular endothelial dysfunction and atherosclerosis, thereby affecting cardiovascular outcomes. Furthermore, NHHR represents the ratio of non-HDL-C to HDL-C, where HDL-C is known as ‘good cholesterol’ due to its role in removing cholesterol from blood vessel walls and lowering atherosclerosis risk. Elevated NHHR indicates higher non-HDL-C levels compared to HDL-C, potentially promoting atherosclerosis and increasing mortality risk28. Low NHHR indicates high blood HDL-C levels, but extensive studies from China and Copenhagen reveal that excessively high HDL is associated with increased all-cause and cardiovascular mortality, demonstrating a U-shaped relationship between HDL and mortality34,35. These results align with our findings.
The results of our subgroup analyses showed that diabetes mellitus affected the relationship between NHHR and all-cause mortality in hypertensive patients, and the negative association between NHHR and all-cause mortality was more pronounced in nondiabetic patients. First, diabetic patients usually have abnormal lipid metabolism manifested by elevated non-HDL-C levels and reduced HDL-C levels, which may lead to elevated NHHR, and this metabolic disorder may mask the predictive value of NHHR for mortality26. In addition, diabetic patients are usually in a state of chronic inflammation and oxidative stress, and in nondiabetic patients, lower levels of inflammation may make the predictive value of NHHR more significant36.
Our RCS curves show that hypertensive patients have the lowest risk of all-cause mortality and cardiovascular mortality when the NHHR is 2.84. At this time, NHHR can be used as a reference index to assess the risk of mortality in hypertensive patients in clinical practice. Several studies have shown that hypertension is closely associated with dyslipidemia and that hypertensive patients have high non-HDL, LDL, and TC37,38. However, these single indicators have limitations in predicting cardiovascular risk8,9. In contrast, the NHHR as a ratio of non-HDL cholesterol to HDL cholesterol ratio, which combines information from multiple lipoproteins, can reflect the impact of dyslipidemia on cardiovascular risk more comprehensively.
It should be noted that this study is not without certain limitations. Since this study’s data originates from the US population, further research is needed to determine if the findings apply to other populations. Secondly, despite incorporating numerous potential confounding variables associated with NHHR and mortality, the study acknowledges that some relevant variables were omitted due to database limitations. Thirdly, as this study was based on the NHANES database, a cross-sectional and retrospective analysis, it was not possible to establish a causal relationship between NHHR and mortality in hypertensive patients. In the future, prospective cohort studies of hypertensive patients could be conducted to regularly monitor NHHR levels and document mortality and associated cardiovascular events in patients. This would help to validate the causal relationship between NHHR and mortality. Finally, although this study found a U-shaped relationship between NHHR and all-cause mortality and cardiovascular mortality, it is unclear whether changing NHHR levels through interventions (e.g., lifestyle modification, medication, etc.) is effective in reducing the risk of death. In the future, randomized controlled trials (RCTs) can be designed to enroll hypertensive patients, intervene in NHHR levels through dietary control, exercise interventions, and lipid-lowering drug therapy, and observe the long-term effects on mortality and cardiovascular events.
Conclusion
This study shows that NHHR is associated with all-cause mortality and cardiovascular mortality in hypertensive patients. NHHR may serve as a novel mortality predictor in hypertensive populations, aiding clinicians in implementing targeted interventions to lower death risk.
Data availability
Data from this study are available upon reasonable request to the first author, Meijuan Ma.
References
Zhang, H. et al. Global burden of metabolic diseases, 1990–2021. Metabolism 160, 155999 (2024).
Abughazaleh, S., Obeidat, O., Tarawneh, M., Qadadeh, Z. & Alsakarneh, S. Trends of hypertensive heart disease prevalence and mortality in the united States between the period 1990–2019, global burden of disease database. Curr. Probl. Cardiol. 49, 102621 (2024).
Liu, J. et al. Global burden of cardiovascular diseases attributable to hypertension in young adults from 1990 to 2019. J. Hypertens. 39, 2488–2496 (2021).
Zhou, J. et al. National, regional and provincial prevalence of childhood hypertension in China in 2020: a systematic review and modelling study. Lancet Child. Adolesc. Health. 8, 872–881 (2024).
Crea, F. Focus on the European society of cardiology: guidelines on hypertension, atlas of cardiovascular disease statistics, and consensus statement on obesity. Eur. Heart J. 45, 3897–3900 (2024).
Mitro, S. D. et al. Hypertension, cardiovascular risk factors, and uterine fibroid diagnosis in midlife. JAMA Netw. Open. 7, e246832 (2024).
Tamura, K., Kanaoka, T., Fujiwara, N. & Hirota, K. Esaxerenone for nocturnal hypertension and possible future direction for treatment of hypertension-cardiovascular-kidney comorbidity. Hypertens. Res. 46, 2059–2061 (2023).
Chen, S. & Cheng, W. Relationship between lipid profiles and hypertension: A Cross-Sectional study of 62,957 Chinese adult males. Front. Public. Health. 10, 895499 (2022).
Deng, G., Li, Y. & Cheng, W. Association of lipid levels with the prevalence of hypertension in Chinese women: A Cross-Sectional study based on 32 health check centers. Front. Endocrinol. (Lausanne). 13, 904237 (2022).
Zhou, D., Liu, X., Lo, K., Huang, Y. & Feng, Y. The effect of total cholesterol/high-density lipoprotein cholesterol ratio on mortality risk in the general population. Front. Endocrinol. (Lausanne). 13, 1012383 (2022).
Yu, Y. et al. A U-shaped association between the LDL-cholesterol to HDL-cholesterol ratio and all-cause mortality in elderly hypertensive patients: a prospective cohort study. Lipids Health Dis. 19, 238 (2020).
Hou, K., Song, W., He, J. & Ma, Z. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and prevalence of periodontitis among US adults: a cross-sectional NHANES study. Sci. Rep. 14, 5558 (2024).
Hong, H., He, Y., Gong, Z., Feng, J. & Qu, Y. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and kidney stones: a cross-sectional study. Lipids Health Dis. 23, 102 (2024).
Qing, G. et al. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and suicidal ideation in adults: a population-based study in the united States. Lipids Health Dis. 23, 17 (2024).
Zhu, L. et al. Lipoprotein ratios are better than conventional lipid parameters in predicting coronary heart disease in Chinese Han people. Kardiol Pol. 73, 931–938 (2015).
Xie, H. et al. The relationship between lipid risk score and new-onset hypertension in a prospective cohort study. Front. Endocrinol. (Lausanne). 13, 916951 (2022).
Liu, B., Wang, J., Li, Y. Y., Li, K. P. & Zhang, Q. The association between systemic immune-inflammation index and rheumatoid arthritis: evidence from NHANES 1999–2018. Arthritis Res. Ther. 25, 34 (2023).
Qi, X. et al. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and risk of depression among US adults: A cross-sectional NHANES study. J. Affect. Disord. 344, 451–457 (2024).
Cai, Y., Zhou, Z. & Zeng, Y. Association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and sleep disorders in US adults: NHANES 2005 to 2016. Med. (Baltim). 103, e38748 (2024).
Du, Y. Z. et al. A cross-sectional analysis of the relationship between the non-high density to high density lipoprotein cholesterol ratio (NHHR) and kidney stone risk in American adults. Lipids Health Dis. 23, 158 (2024).
Chen, T. et al. Association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and kidney stone: evidence from NHANES 2007–2018. BMC Public. Health. 24, 1818 (2024).
Pan, J. et al. Association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and diabetic kidney disease in patients with diabetes in the united states: a cross-sectional study. Lipids Health Dis. 23, 317 (2024).
Cheng, Q. et al. Association of non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and gallstones among US adults aged = 50 years: a cross-sectional study from NHANES 2017–2020</at. Lipids Health Dis. 23, 265 (2024).
Wang, Z. et al. The relationship between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and hyperuricaemia. Lipids Health Dis. 23, 187 (2024).
Hao, J. Q. et al. The association between non–high–density lipoprotein cholesterol to high–density lipoprotein cholesterol ratio (NHHR) and low muscle mass in adults aged 20–59: a population-based study in the united States. Lipids Health Dis. 23, 274 (2024).
Tan, M. Y. et al. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio with type 2 diabetes mellitus: recent findings from NHANES 2007–2018. Lipids Health Dis. 23, 151 (2024).
Zhen, R. et al. The relationship between Non-HDL-C /HDL-C ratio (NHHR) and vitamin D in type 2 diabetes mellitus. Diabetes Metab. Syndr. Obes. 16, 2661–2673 (2023).
Yu, B. et al. The non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) as a predictor of all-cause and cardiovascular mortality in US adults with diabetes or prediabetes: NHANES 1999–2018. BMC Med. 22, 317 (2024).
Gao, P., Zhang, J. & Fan, X. NHHR: an important independent risk factor for patients with STEMI. Rev. Cardiovasc. Med. 23, 398 (2022).
Liu, J. et al. Association between the non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and cardiovascular outcomes in patients undergoing percutaneous coronary intervention: a retrospective study. Lipids Health Dis. 23, 324 (2024).
Zhong, S. et al. An update on lipid oxidation and inflammation in cardiovascular diseases. Free Radic Biol. Med. 144, 266–278 (2019).
Zhang, J. et al. The mediation effect of HDL-C: Non-HDL-C on the association between inflammatory score and recurrent coronary events. Heliyon 10, e23731 (2024).
Gordon, S. M. & Remaley, A. T. High density lipoproteins are modulators of protease activity: implications in inflammation, complement activation, and atherothrombosis. Atherosclerosis 259, 104–113 (2017).
Lu, J. et al. Association of high-density lipoprotein cholesterol with all-cause and cause-specific mortality in a Chinese population of 3.3 million adults: a prospective cohort study. Lancet Reg. Health West. Pac. 42, 100874 (2024).
Barter, P. J. & Rye, K. A. HDL cholesterol concentration or HDL function: which matters? Eur. Heart J. 38, 2487–2489 (2017).
Masenga, S. K., Kabwe, L. S., Chakulya, M. & Kirabo, A. Mechanisms of oxidative stress in metabolic syndrome. Int J. Mol. Sci. 24. (2023).
Borghi, C. et al. Serum cholesterol levels, blood pressure response to stress and incidence of stable hypertension in young subjects with high normal blood pressure. J. Hypertens. 22, 265–272 (2004).
Laaksonen, D. E. et al. Dyslipidaemia as a predictor of hypertension in middle-aged men. Eur. Heart J. 29, 2561–2568 (2008).
Funding
This study was supported by the Natural Science Foundation of Shaanxi Province (No.2024SF-YBXM-017), the Qin Chuangyuan Traditional Chinese Medicine Innovation Research and Development Transformation Project (No.2022-QCYZH-022), Shaanxi Provincial Key R&D Program, General Project-Social Development Field (No: 2024SF-YBXM-017), and the Key Basic Natural Science Foundation of Shaanxi Province (No.2022JZ-47).
Author information
Authors and Affiliations
Contributions
Meijuan Ma: Conceived the study, collected data, and led manuscript preparation and revisions.Jinxia Hao and Xiaoxiang Liu contributed to the study design, conducted data analysis, and critically revised the manuscript. Ying Lv and Fuqiang Liu: Assisted with data collection, and contributed to initial manuscript drafting. Na Wei provided expertise and contributed to the writing and revision of the manuscript. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The Ethics Review Board of the National Center for Health Statistics approved the human studies. The studies adhered to local legislation and institutional requirements. Participants gave written informed consent for study involvement.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, M., Hao, J., Liu, X. et al. U-shaped relationship between the non-HDL to HDL cholesterol ratio and mortality in hypertensive individuals in the study from NHANES database. Sci Rep 15, 20657 (2025). https://doi.org/10.1038/s41598-025-07141-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07141-z