Abstract
To evaluate the prevalence of high myopia in Chinese cataract surgery candidates and analyse their biometric characteristics, we conducted a 10-year retrospective consecutive case series of 17,325 cataract patients (22,479 eyes) classified by axial length (AL) into a high myopia group (defined as an AL ≥ 26.00 mm) and a non-high myopia group. A total of 2943 eyes (13.1%) had high myopia, with the highest prevalence of high myopia (41.2%) in patients aged 40–49 years. In the high myopia group, the mean age was 59.5 ± 12.6 years, younger than the non-high myopia group (68.9 ± 11.0 years, P < 0.001). The AL, corneal diameter, anterior chamber depth, and corneal astigmatism (CA) were all greater in the high myopia group than in the non-high myopia group (P < 0.001 for all). In the high myopia group, 12.7% of the eyes had flat corneas, and 67.4% of the eyes had moderate to high CA, which were higher than the proportions in the non-high myopia group (P < 0.001 for both). CA was positively correlated with age in the two groups (r = 0.165 and 0.274, respectively; P < 0.001 for both) after the age of 50. Fully understanding these characteristics may help inform public health guidelines and cataract surgery decisions for high myopia patients.
Similar content being viewed by others
Introduction
High myopia is characterized by axial elongation and is typically defined as an axial length (AL) ≥ 26.00 mm1,2,3 or a spherical equivalent ≤-6.00 diopters (D)4,5. It is a common eye disorder and a public health burden in Asian countries, especially in China, with a high prevalence in young adults (10–20%)6,7, which was reported to reach 38.4% in university freshmen in Taiwan8. Owing to advances in phacoemulsification techniques, biometric devices, and intraocular lens (IOL) power calculations, cataract surgery is routinely performed in patients with high myopia. However, compared with those without high myopia, cataract surgery is significantly more challenging in highly myopic eyes for several reasons, including the accuracy of the AL measurements and the choice of IOL calculation formulas preoperatively9,10. Long ALs also affect cataract surgeries in many ways and are associated with intraoperative posterior capsular rupture, postoperative retinal detachment, high intraocular pressure and refractive hyperopic error9,11. High myopia is a common risk factor for cataracts, with a 3.8-fold increase in the odds for nuclear cataracts and a 1.29-fold increase in the odds for posterior subcapsular cataracts12,13. The number of cataract patients with high myopia has shown an increasing trend accompanied by a significant increase in the number of high myopia patients globally14. However, to the best of our knowledge, there is little evidence on the prevalence of high myopia in cataract surgery candidates, and few reports have systematically evaluated the distribution of biometric parameters in patients with high myopia before cataract surgery.
In this study, we retrospectively collected biometric data measured by an optical biometry device (IOLMaster) and demographic data before cataract surgery over a 10-year period to evaluate the prevalence of high myopia in Chinese cataract surgery candidates and to assess the biometric characteristics of highly myopic eyes.
Patients and methods
Study design
This retrospective study of medical records covered a 10-year period, from 1 January 2014 to 31 December 2023. Consecutive Chinese patients aged 18 years or older who underwent cataract surgery at the Department of Ophthalmology, the First Affiliated Hospital, Jiangxi Medical College, Nanchang University (Jiangxi, Central China) were reviewed. Ethics approval was obtained from the Human Ethics Committee of the First Affiliated Hospital, Jiangxi Medical College, Nanchang University (No. (2024)CDYFYYLK(12−006)), and informed consent was obtained from all patients. All procedures in this study were performed in accordance with the tenets of the Declaration of Helsinki. Patients with a history of ocular surgeries or ocular trauma, corneal or ocular surface diseases, uveitis, glaucoma, lens dislocation, wearing contact lenses within the previous two weeks, or severe cataracts that could not be measured by IOLMaster were excluded.
Ophthalmic examinations and definitions
After relevant past medical history data were collected, all cataract patients underwent a standard ophthalmological examination including visual acuity, intraocular pressure, slit-lamp biomicroscopy and a fundus examination through dilated pupils. Biometric parameters in both eyes of each patient were measured preoperatively using an optical biometry device (IOLMaster, version 5.3, or 7.5, or IOLMaster 700, Carl Zeiss Meditec, Jena, Germany). The anterior chamber depth (ACD) was defined as the distance from the anterior corneal surface to the anterior lens surface. Corneal power was measured in two meridians: flat keratometry (K1) and steep keratometry (K2). The keratometry (K) value was the mean of K1 and K2. The refractive index value used by the IOLMaster was n = 1.337515,16. The ACD was divided into three subgroups: ACD ≤ 3.00 mm, ACD between 3.01 mm and 3.49 mm, and ACD ≥ 3.50 mm17. Corneal power was divided into three subgroups according to K: flat corneas (< 42.00 D), medium (42.00–46.00 D) and steep corneas (> 46.00 D)18. Corneal astigmatism (CA) was calculated as the absolute difference between K2 and K1 and was divided into three subgroups according to the astigmatism severity as follows: low (< 0.75 D), moderate (0.75–2.50 D) and high astigmatism (> 2.50 D)16,19,20. We classified CA by axis as “with-the-rule” (WTR) when the axis of the correcting minus cylinder was within 180 ± 30 degrees (the steep corneal meridian was within 90 ± 30 degrees in this case), as “against-the-rule” (ATR) when the correcting minus cylinder axis was within 90 ± 30 degrees, and as oblique when it was other degree values16,21.
In this study, high myopia was defined as an AL ≥ 26.00 mm1,2,3. For the analysis of biometric parameters, patients were classified into two groups: the high myopia group included cataract patients with high myopia and the non-high myopia group included cataract patients with normal ALs (defined as 22.00 mm ≤ AL ≤ 25.00 mm)3,16,17. Additionally, we divided the highly myopic eyes into three subgroups according to the AL (indicating myopic severity) as follows: mild (26.00 mm ≤ AL < 28.00 mm), moderate (28.00 mm ≤ AL < 30.00 mm) and extremely high myopia (≥ 30.00 mm)2,3.
The biometric parameters of all patients were measured routinely by two experienced technicians within four weeks before cataract surgery. Three or more measurements were performed for each parameter, and the values were averaged. Patient demographics, AL, corneal power (K1, K2 and K), corneal diameter (CD) in the horizontal direction, ACD, CA (cylinder and axis of astigmatism), AL/corneal radius of curvature (CR) ratio and ACD/AL ratio were recorded. The measurement data for each eye recorded on the closest date to the cataract surgery were selected for analysis.
Statistical analysis
Data analyses were performed using Excel 2016 (Microsoft Corp., Redmond, WA, USA) and SPSS 23.0 (IBM Corp., Armonk, N.Y., USA). For patients with both eyes eligible, the first-operated eye was used for the analysis of the biometric characteristics. The normality of the variable distributions was checked with the Kolmogorov‒Smirnov test. Variables are reported as the mean ± standard deviation (SD) or as the median (range) depending on the distribution of the data. Differences between groups were compared using an independent t test or one-way analysis of variance (ANOVA) for normally distributed variables and the Mann–Whitney U test or Kruskal‒Wallis test for nonnormally distributed variables. Trend analysis was performed to detect statistically significant trend changes with age and myopic severity. The χ2 test was used to determine differences in categorical variables between groups, and the resulting odds ratios (ORs) and 95% confidence intervals (CIs) are presented. Possible correlations between variables were assessed using the Pearson or Spearman correlation coefficient depending on the parameter distributions. Propensity score matching (PSM) was used to remove the interference of confounding factors. All P values were two-sided, and a P value < 0.05 was considered statistically significant.
Results
The prevalence of high myopia in cataract surgery candidates
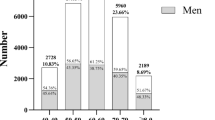
A total of 22,479 eyes of 17,325 patients were included in this study. The distribution of the ALs in the patients is shown in (Fig. 1), and the mean AL was 24.26 ± 2.27 mm (range, 18.95–37.34 mm). Among the cataract surgery candidates (22479 eyes), 2943 eyes (13.1%, 95% CI 12.7–13.5%) had high myopia. The prevalence of high myopia stratified by age is shown in (Fig. 2a). The highest prevalence of high myopia (41.2%, 95% CI 38.5–44.0%) was observed in patients aged 40 to 49 years, and the prevalence of high myopia decreased significantly with age after the age of 40. The prevalence of high myopia in men was 14.2% (95% CI 13.5–14.9%), which was higher than the prevalence in women (12.3%, 95% CI 11.7–12.9%; P = 0.001). The sex- and age-specific prevalence of high myopia is shown in (Fig. 2b).
Demographic characteristics of the study participants in the high myopia and non-high myopia groups
For the analysis of biometric parameters, 2206 patients (2206 eyes) with high myopia (high myopia group) and 13,429 patients (13,429 eyes) with normal ALs (non-high myopia group) were included in this analysis. Table 1 shows the demographic characteristics of the study participants in the two groups. The AL distribution for the highly myopic eyes, which indicates the distribution of myopic severity, is shown in (Fig. 3). There were 743 eyes (33.7%) with extremely high myopia (AL ≥ 30.00 mm). Figure 4 shows the distribution of patients in the high myopia and non-high myopia groups according to age group. In the high myopia group, 1064 patients (48.2%) were younger than 60 years, which was higher than the proportion in the non-high myopia group (16.2%, P < 0.001).
Distribution of biometric parameters in the high myopia and non-high myopia groups
The differences in the distributions of the biometric parameters between the high myopia group and the non-high myopia group are shown in (Table 2). In the high myopia group, the AL, CD, ACD, CA and AL/CR ratio were greater than those in the non-high myopia group (P < 0.001 for all). Additionally, Fig. 5 shows the distribution of the biometric parameters in the two groups according to age.
Distribution of the biometric parameters in the high myopia and non-high myopia groups according to age group. (a) The flat keratometry (K1) values in the two groups. (b) The steep keratometry (K2) values in the two groups. (c) The corneal diameter (CD) values in the two groups. (d) The anterior chamber depth (ACD) values in the two groups. (e) The corneal astigmatism (CA) values in the two groups. (f) The AL/corneal radius of curvature (CR) ratio values in the two groups. *P < 0.05, **P < 0.01, ***P < 0.001; independent t test (a–d); Mann‒Whitney U test (e,f).
The corneal power distributions of the two groups are shown in (Fig. 6a). In the high myopia group, 280 eyes (12.7%) had flat corneas, which was higher than the proportion in the non-high myopia group (6.0%, P < 0.001), and the highly myopic eyes were more likely to have a flat corneas than the eyes with normal ALs (OR = 2.28), as shown in (Fig. 6b).
Distribution of the corneal power in the high myopia and non-high myopia groups. (a) Bar graph showing the frequency distribution of the corneal power in 2.00 D steps for the two groups. (b) The percentage of flat corneas (as K < 42.00 D), medium (as K between 42.00 D and 46.00 D), and steep corneas (as K > 46.00 D) in the two groups. (K = keratometry). P values were determined with the χ2 test.
Moreover, in the high myopia group, 1031 eyes (46.7%) had an ACD ≥ 3.50 mm, which was higher than the proportion in the non-high myopia group (16.1%, P < 0.001), as shown in (Fig. 7a). However, in the high myopia group, the ACD and ACD/AL ratio were both negatively correlated with the AL (r = -0.080 and -0.603, respectively; P < 0.001 for both) (Fig. 7b, c), but both the ACD and ACD/AL ratio were positively correlated with the AL in the non-high myopia group (r = 0.379 and 0.160, respectively; P < 0.001 for both) (Fig. 7d, e).
Differences in the anterior chamber depth between the high myopia group and the non-high myopia group. (a) Comparisons of three subgroups according to the anterior chamber depth (ACD) between the two groups. (b) A negative correlation was observed between the ACD and the axial length (AL) in the high myopia group (r = -0.080, P < 0.001). (c) A negative correlation was observed between the ACD/AL ratio and the AL in the high myopia group (r = -0.603, P < 0.001). (d) A positive correlation was observed between the ACD and the AL in the non-high myopia group (r = 0.379, P < 0.001). (e) A positive correlation was observed between the ACD/AL ratio and the AL in the non-high myopia group (r = 0.160, P < 0.001). P values were determined with the χ2 test (a). P values were determined with Spearman‒related coefficient (b,c) or Pearson‒related coefficient (d,e).
The bar graph shows the frequencies (%) of astigmatism cylinders in 0.50 D steps in the high myopia and non-high myopia groups (Fig. 8a). In the high myopia group, 1822 eyes (82.6%) had CA ≥ 0.50 D, 1138 eyes (51.6%) had CA ≥ 1.00 D, and 623 eyes (28.2%) had CA ≥ 1.50 D, all of which were higher than the respective proportions observed in the non-high myopia group (P < 0.001 for all) (Fig. 8b). In the high myopia group, 1340 eyes (60.7%) had moderate CA, and 147 eyes (6.7%) had high CA, both of which were higher than the respective proportions in the non-high myopia group (P < 0.001 for both), and the highly myopic eyes were more likely to have moderate to high CA than the eyes with normal ALs (OR = 1.90), as shown in (Fig. 8c). A significantly higher proportion of WTR astigmatism was found in the high myopia group (922 eyes, 41.8%) than in the non-high myopia group (28.2%, P < 0.001), as shown in (Fig. 8d).
Differences in corneal astigmatism between the high myopia group and the non-high myopia group. (a) Bar graph showing the frequencies (%) of astigmatism cylinders in 0.50 D steps in the high myopia group (n = 2206) and the non-high myopia group (n = 13429). (b) Line chart comparing the cumulative percentages of eyes in 0.50 D steps in the two groups. (c) Comparisons of three categories according to astigmatism severity in the two groups. (d) The proportions of WTR, ATR, and oblique astigmatism in the two groups. (CA corneal astigmatism, D dioptres; WTR with-the-rule, ATR against-the-rule). P values were determined with the χ2 test.
Table 3 shows the correlation coefficients matrix of the biometric parameters in the two groups. In the high myopia group, the K value was positively correlated with the AL (r = 0.056, P = 0.008), but the K value was negatively correlated with the AL in the non-high myopia group (r=-0.553, P < 0.001). In the high myopia group, the CD value was negatively correlated with the AL (r=-0.046, P = 0.030), but the CD value was positively correlated with the AL in the non-high myopia group (r = 0.363, P < 0.001). Additionally, in the high myopia group, in those older than 50 years, CA was positively correlated with age (r = 0.165, P < 0.001), which was consistent with the correlation in the non-high myopia group (r = 0.274, P < 0.001).
Distribution of the biometric parameters in the high myopia patients by sex, age, and myopic severity
The distributions of the biometric parameters in the patients with high myopia according to sex, age, and myopic severity are summarized in (Table 4). Among the high myopia patients, the AL, K1, K2 and CA were greater in women than in men (P < 0.01 for all). K and CA showed tended to increase with increasing age (P < 0.001 for both). Additionally, the AL, K and CA tended to increase as the myopic severity increased (P < 0.05 for all). The proportion of high CA increased significantly with age (P < 0.001), and the proportion of moderate CA increased with myopic severity (P = 0.009). Figure 9 shows the differences in the distributions of the biometric parameters between men and women among the high myopia patients according to the age group.
Distribution of the biometric parameters in the high myopia patients stratified by sex and age. (a) Comparisons of the median axial length (AL) according to age between men (n = 1036) and women (n = 1170). (b,c) Comparisons of the mean flat keratometry (K1) and steep keratometry (K2) according to age in the two sex subgroups. (d,e) Comparisons of the mean corneal diameter (CD) and anterior chamber depth (ACD) according to age in the two sex subgroups. (f) Comparisons of the median corneal astigmatism (CA) values according to age in the two sex subgroups.
Distribution of the biometric parameters in the two groups after adjusting for sex and age by PSM
PSM was applied to adjust for the confounding factors of sex and age in the high myopia and non-high myopia groups, as shown in (Table 5). After matching, the AL, CD, ACD and CA in the high myopia group were greater than those in the non-high myopia group (P < 0.05 for all). Moreover, in the high myopia group, 12.7% of the eyes had flat corneas, and 67.3% of the eyes had moderate to high CA, both of which were higher than the proportions observed in the non-high myopia group (5.6%, and 47.4%, respectively; P < 0.001 for both).
Discussion
In this large, retrospective study conducted over 10 years, we provided data on the prevalence and distribution of preoperative ocular biometry for high myopia in cataract surgery patients using an optical biometry device (IOLMaster).The prevalence of high myopia of 13.1% in Chinese cataract surgery candidates was comparable to that reported in young adults (10–20%) in Asian countries6,7. Moreover, the prevalence of high myopia was up to 41.2% in the cataract surgery candidates aged 40 to 49 years. This prevalence was significantly higher than the prevalence of high myopia reported in Chinese middle-aged and elderly adults (≥ 40 years) (2.4–5.0%)22,23,24.
In the present study, an AL ≥ 26.00 mm was used as the definition of high myopia because of refractive changes caused by the cataract itself25. Moreover, high myopia is strongly associated with nuclear cataracts, which are well known for their myopic shift in refraction12,13,26. Patients with high myopia tend to suffer cataracts at a younger age than those without high myopia1,27and high myopia is a significant factor associated with the need for cataract surgery28,29. In our study, the average age of the high myopia patients was 59.5 years, which was much younger than that of the patients with normal ALs (68.9 years, P < 0.001; almost a 10-year difference) as well as those of patients with age-related cataracts in China (70.56 years)30, Thailand (68.21 years)31, and the UK (79 years)21. Moreover, almost half of the high myopia patients (48.2%) were relatively young (< 60 years of age), which was higher than the proportion of patients with normal ALs (16.2%; P < 0.001). These findings indicate that patients with high myopia underwent cataract surgery much earlier than those with normal ALs and age-related cataracts did. This finding is consistent with several other studies suggesting that high myopia patients develop cataracts, particularly nuclear cataracts, at a younger age12,32.
With the prevalence of myopia increasing over the past few decades, the prevalence of myopia in teenagers and young adults has reached 90% in China33, accompanied by an increasing prevalence of high myopia (10–20%)6. As young adults grow older in the next few decades, the prevalence of high myopia will undoubtedly increase in these age groups and approach the prevalence observed in young adults in the next few decades7,14. Given the increase in the prevalence of high myopia, a high proportion of this new generation of adults will probably require cataract surgery approximately 10 years earlier, according to our findings. The particularly high prevalence of high myopia among cataract surgery patients is an important public health concern because cataract patients with high myopia are more likely to develop myopic macular degeneration and even retinal detachment after cataract surgery, which can lead to low vision or irreversible blindness9,10,34,35. Moreover, nearly 50% of the high myopia patients had cataracts and required cataract surgery at a relatively young age (< 60 years old, which is considered a working age34). All these factors significantly increase the burden of high myopia in the population. Accordingly, preventive measures are necessary to limit the occurrence of myopia and its progression to high myopia.
In this study, almost 1/3 of the highly myopic eyes had ALs ≥ 30.00 mm, indicating that extreme ALs are very common in the high myopia patients undergoing cataract surgery. The mean ACD was 3.45 mm in the high myopia group, which was significantly deeper than that in the non-high myopia group (3.09 mm, P < 0.001), consistent with the findings of a previous study36. However, in the highly myopic eyes, the ACD was weakly correlated with the AL (r = -0.080), and the ACD/AL ratio was negatively correlated with the AL (r = -0.603), indicating that the ACD did not increase in parallel with the vitreous length in the highly myopic eyes and that the vitreous length may increase faster in extreme AL eyes that develop posterior staphyloma37.
Corneal stromal thickness and corneal stiffness are reduced in myopia and are negatively associated with myopic severity38,39. In our study, the mean K in the high myopia group was smaller than that in the non-high myopia group (43.80 D versus 44.19 D, P < 0.001). Additionally, in the high myopia group, 12.7% of the eyes had flat corneas, which was significantly higher than the proportion in the non-high myopia group (6.0%, P < 0.001), indicating that eyes with a longer AL had, on average, a lower corneal power, and flat corneas are very common in highly myopic eyes. This finding is consistent with the findings that the AL was significantly and negatively correlated with the corneal power, as reported in the previous studies40,41.
In our study, the mean CA value in the high myopia group was 1.20 D, which was significantly greater than that in the non-high myopia group (0.93 D, P < 0.001). The CA value in patients with high myopia was also greater than that in patients with age-related cataracts reported in the UK (1.06 D)21, Thailand (1.05 D)31, and China (1.01 D)30. Moreover, more than 80% (82.6%) of the eyes in the high myopia group had a CA value ≥ 0.50 D (which is clinically relevant21), and more than half (51.6%) of the highly myopic eyes had a CA value of at least 1.00 D, both of which were significantly higher than the corresponding proportions in the non-high myopia group (71.9% and 35.9%, respectively; P < 0.001 for both) and the proportions of the age-related cataracts reported in the UK in a previous study (78% and 42%, respectively)21. Moreover, in the cataract surgery eyes with high myopia, almost 70% of the eyes had moderate to high CA values (CA ≥ 0.75 D, as a general indication for toric IOL implantation42,43), which was much higher than the proportion in the eyes with normal ALs (52.2%, P < 0.001). Thus, in the new highly myopic generation, there may be a greater requirement for toric IOL implantation.
Because of the significantly different distributions of both sex and age in the high myopia and non-high myopia groups, comparisons of the biometric parameters between the two groups were made by PSM. After matching, the high myopia patients presented significantly greater AL, CD, ACD and CA values; a higher proportion of flat corneas, and a higher proportion of moderate to high CA than the normal AL patients did, which was consistent with the results before matching in our study.
A main limitation of this study was that it was a retrospective study and that the patients came from one centre, which may not completely represent the prevalence and biometric characteristics of high myopia in the Chinese cataract surgery population. Only a community-based epidemiologic survey could provide conclusive evidence. Another limitation of our study was the biometric parameters of patients measured by two optical biometry devices (IOLMaster 500 and IOLMaster 700), which may cause measurement errors and influence the relationship between biometric parameters. However, several previous studies have shown that the results of these two devices in measuring AL, K, CD, ACD, and CA in cataract patients are of high agreement and the measured values of the biometric parameters are interchangeable between the two instruments44,45.
In conclusion, a high prevalence of high myopia was observed in Chinese cataract surgery candidates. Patients with high myopia, especially men, underwent cataract surgery at much younger ages than patients with normal ALs did. The preoperative biometric data in this large cohort were measured by the IOLMaster device and may provide a useful reference for surgery decisions in cataract eyes with high myopia. Our findings also raise a considerable public health challenge for China. As this more myopic younger generations ages, an increasing proportion of those with high myopia (10–20% of the age cohort) are likely to require cataract surgery at a younger age, which will be made more challenging by a longer AL, deeper ACD, and greater CA. This increase in the need for cataract surgery will add considerably to the public health burden associated with the epidemic of myopia.
Data availability
All data generated or analysed during this study are included in the manuscript.
References
Zhang, M., Jing, Q., Chen, J. & Jiang, Y. Analysis of corneal higher-order aberrations in cataract patients with high myopia. J. Cataract Refract. Surg. 44, 1482–1490 (2018).
Zhang, J. et al. Effect of axial length adjustment methods on intraocular Lens power calculation in highly myopic eyes. Am. J. Ophthalmol. 214, 110–118 (2020).
Tan, Y. et al. Effect of cataract surgery on vision-related quality of life among cataract patients with high myopia: a prospective, case-control observational study. Eye (Lond). 36, 1583–1589 (2022).
Wang, S. K. et al. Incidence of and factors associated with myopia and high myopia in Chinese children, based on refraction without cycloplegia. JAMA Ophthalmol. 136, 1017–1024 (2018).
Tailor, P. D., Xu, T. T., Tailor, S., Asheim, C. & Olsen, T. W. Trends in myopia and high myopia from 1966 to 2019 in olmsted county, Minnesota. Am. J. Ophthalmol. 259, 35–44 (2024).
Morgan, I. G. et al. The epidemics of myopia: aetiology and prevention. Prog Retin Eye Res. 62, 134–149 (2018).
Saw, S. M., Matsumura, S. & Hoang, Q. V. Prevention and management of myopia and myopic pathology. Invest. Ophthalmol. Vis. Sci. 60, 488–499 (2019).
Wang, T. J., Chiang, T. H., Wang, T. H., Lin, L. L. & Shih, Y. F. Changes of the ocular refraction among freshmen in National Taiwan university between 1988 and 2005. Eye (Lond). 23, 1168–1169 (2009).
Yao, Y. et al. Efficacy and complications of cataract surgery in high myopia. J. Cataract Refract. Surg. 47, 1473–1480 (2021).
Elhusseiny, A. M. & Salim, S. Cataract surgery in myopic eyes. Curr. Opin. Ophthalmol. 34, 64–70 (2023).
Fesharaki, H. et al. A comparative study of complications of cataract surgery with phacoemulsification in eyes with high and normal axial length. Adv. Biomed. Res. 1, 67 (2012).
Praveen, M. R., Vasavada, A. R., Jani, U. D., Trivedi, R. H. & Choudhary, P. K. Prevalence of cataract type in relation to axial length in subjects with high myopia and emmetropia in an Indian population. Am. J. Ophthalmol. 145, 176–181 (2008).
Pan, C. W. et al. Differential associations of myopia with major age-related eye diseases: the Singapore Indian eye study. Ophthalmology 120, 284–291 (2013).
Holden, B. A. et al. Global prevalence of myopia and high myopia and Temporal trends from 2000 through 2050. Ophthalmology 123, 1036–1042 (2016).
Özyol, P. & Özyol, E. Agreement between Swept-Source optical biometry and Scheimpflug-based topography measurements of anterior segment parameters. Am. J. Ophthalmol. 169, 73–78 (2016).
Tan, Y. et al. Evaluation of preoperative corneal astigmatism using swept-source optical biometry in Chinese cataract surgery candidates with high myopia: a prospective, comparative observational study. Ann. Transl Med. 9, 618 (2021).
Gökce, S. E. et al. Accuracy of 8 intraocular lens calculation formulas in relation to anterior chamber depth in patients with normal axial lengths. J. Cataract Refract. Surg. 44, 362–368 (2018).
Melles, R. B., Holladay, J. T. & Chang, W. J. Accuracy of intraocular Lens calculation formulas. Ophthalmology 125, 169–178 (2018).
Tan, Q. Q. et al. Optical quality in low astigmatic eyes with or without cylindrical correction. Graefes Arch. Clin. Exp. Ophthalmol. 258, 451–458 (2020).
Jun, I. et al. Clinical outcomes of SMILE with a triple centration technique and corneal Wavefront-Guided transepithelial PRK in high astigmatism. J. Refract. Surg. 34, 156–163 (2018).
Day, A. C. et al. Distribution of preoperative and postoperative astigmatism in a large population of patients undergoing cataract surgery in the UK. Br. J. Ophthalmol. 103, 993–1000 (2019).
Cheng, C. Y., Hsu, W. M., Liu, J. H., Tsai, S. Y. & Chou, P. Refractive errors in an elderly Chinese population in taiwan: the Shihpai eye study. Invest. Ophthalmol. Vis. Sci. 44, 4630–4638 (2003).
Xu, L. et al. Refractive error in urban and rural adult Chinese in Beijing. Ophthalmology 112, 1676–1683 (2005).
He, M. et al. Refractive error and biometry in older Chinese adults: the Liwan eye study. Invest. Ophthalmol. Vis. Sci. 50, 5130–5136 (2009).
Díez Ajenjo, M. A. & García Domene, M. C. Peris martínez, C. Refractive changes in nuclear, cortical and posterior subcapsular cataracts. Effect of the type and grade. J. Optom. 8, 86–92 (2015).
Samarawickrama, C., Wang, J. J., Burlutsky, G., Tan, A. G. & Mitchell, P. Nuclear cataract and myopic shift in refraction. Am. J. Ophthalmol. 144, 457–459 (2007).
Zhang, M., Qian, D., Jing, Q., Chen, J. & Jiang, Y. Analysis of corneal spherical aberrations in cataract patients with high myopia. Sci. Rep. 9, 1420 (2019).
Kanthan, G. L., Mitchell, P., Rochtchina, E., Cumming, R. G. & Wang, J. J. Myopia and the long-term incidence of cataract and cataract surgery: the blue mountains eye study. Clin. Exp. Ophthalmol. 42, 347–353 (2014).
Tan, A. G. et al. Six-Year incidence of and risk factors for cataract surgery in a Multi-ethnic Asian population: the Singapore epidemiology of eye diseases study. Ophthalmology 125, 1844–1853 (2018).
Chen, W. et al. Prevalence of corneal astigmatism before cataract surgery in Chinese patients. J. Cataract Refract. Surg. 39, 188–192 (2013).
Lekhanont, K., Wuthisiri, W., Chatchaipun, P. & Vongthongsri, A. Prevalence of corneal astigmatism in cataract surgery candidates in bangkok, Thailand. J. Cataract Refract. Surg. 37, 613–615 (2011).
Pan, C. W., Cheng, C. Y., Saw, S. M., Wang, J. J. & Wong, T. Y. Myopia and age-related cataract: a systematic review and meta-analysis. Am. J. Ophthalmol. 156, 1021–1033e1021 (2013).
Dolgin, E. The myopia boom. Nature 519, 276–278 (2015).
Naidoo, K. S. et al. Potential lost productivity resulting from the global burden of myopia: systematic review, Meta-analysis, and modeling. Ophthalmology 126, 338–346 (2019).
Shi, H. et al. Global prevalence of myopic macular degeneration in general population and patients with high myopia: A systematic review and meta-analysis. Eur. J. Ophthalmol. 34, 631–640 (2024).
Zhao, Y. et al. Capsular adhesion to intraocular lens in highly myopic eyes evaluated in vivo using ultralong-scan-depth optical coherence tomography. Am. J. Ophthalmol. 155, 484–491e481 (2013).
Ohno-Matsui, K. & Jonas, J. B. Posterior Staphyloma in pathologic myopia. Prog Retin Eye Res. 70, 99–109 (2019).
Kim, B. J., Ryu, I. H., Lee, J. H. & Kim, S. W. Correlation of sex and myopia with corneal epithelial and stromal thicknesses. Cornea 35, 1078–1083 (2016).
Chen, L. et al. Corneal Biomechanical properties demonstrate anisotropy and correlate with axial length in myopic eyes. Invest. Ophthalmol. Vis. Sci. 64, 27 (2023).
Hoffmann, P. C. & Hütz, W. W. Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J. Cataract Refract. Surg. 36, 1479–1485 (2010).
Cui, Y. et al. Biometry and corneal astigmatism in cataract surgery candidates from Southern China. J. Cataract Refract. Surg. 40, 1661–1669 (2014).
Kessel, L. et al. Toric intraocular lenses in the correction of astigmatism during cataract surgery: A systematic review and Meta-analysis. Ophthalmology 123, 275–286 (2016).
Keshav, V. & Henderson, B. A. Astigmatism management with intraocular Lens surgery. Ophthalmology 128, e153–e163 (2021).
Srivannaboon, S., Chirapapaisan, C., Chonpimai, P. & Loket, S. Clinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometer. J. Cataract Refract. Surg. 41, 2224–2232 (2015).
Jiang, J. et al. A comparison of iolmaster 500 and iolmaster 700 in the measurement of ocular biometric parameters in cataract patients. Sci. Rep. 12, 12770 (2022).
Acknowledgements
The authors gratefully acknowledge Prof. Qing Liu for providing statistical assistance and Ian G. Morgan for the English language editing.
Funding
This study was supported by grants from the Science and Technology Research Project of the Education Department of Jiangxi Province (Grant No. GJJ210153), the Science and Technology Project of Jiangxi Provincial health Commission (Grant No. 202210443), the Key Research and Development Program of Jiangxi Province (Grant No. 20203BBG73059), and the National Key Research and Development Program of China (Grant No. 2017YFC1104603). The funding organization had no role in the design or conduct of this research or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
Y.T., Y.S., L.L., and Z.P. designed the research; Y.T., Y.S., Z.P., M.P., Y.W., Y.X., X.Z., and X.W. performed research; Y.T., Y.S., L.L., M.P., Y.W., Y.X., X.Z., and X.W. analysed the data; and Y.T., Y.S, L.L., Y.W., Y.X., X.Z., and X.W. wrote the manuscript. All the authors reviewed and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tan, Y., Shao, Y., Liu, L. et al. A 10-year retrospective study on the prevalence and biometric characteristics of high myopia in Chinese cataract surgery candidates. Sci Rep 15, 22698 (2025). https://doi.org/10.1038/s41598-025-07697-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07697-w