Abstract
Lung squamous cell carcinoma (LUSC) is a prevalent subtype of lung cancer. This retrospective cohort study aims to explore the effect of postoperative chemotherapy on survival in patients with Stage III LUSC and to assess its heterogeneity across different patient subgroups. Patients diagnosed with postoperative Stage III LUSC between 2010 and 2015 were identified in the Surveillance, Epidemiology, and End Results (SEER) database, and cases with missing information were excluded. The primary outcome measure was overall survival (OS). Propensity score matching (PSM) was employed to balance confounders. Kaplan-Meier (KM) curve was used to assess the OS of patients in different groups. The prognostic risk factors of patients with OS were screened and analyzed through Cox regression analysis. The cohort consisted of 1,784 patients (65.3% receiving chemotherapy), and postoperative chemotherapy was associated with a modest survival benefit: the adjusted hazard ratio (HR) was 0.62 (95%CI: 0.55–0.69, P < 0.001), corresponding to an absolute 5-year OS improvement from 28% (Non-chemotherapy) to 42% (Chemotherapy). Overall, no significant difference was observed in OS between the PSM group and the non-PSM group, except for the variable tumor size, which became significant for OS after matching. Subgroup analyses revealed that chemotherapy improved survival for patients across nearly all characteristics. Univariate and multivariate Cox regression analyses identified marital status, race, gender, and age as significant prognostic factors influencing OS. In conclusion, postoperative chemotherapy significantly ameliorates the survival in most patients with Stage III LUSC, with the most pronounced effects observed in those with N1-2 stage disease and undergoing resection of the lobe, bilobectomy, or pneumonectomy. Our findings provide valuable insights for clinical decision-making and related studies on the application of chemotherapy in patients with Stage III LUSC resection.
Similar content being viewed by others
Introduction
Lung cancer, a major public health challenge, has the highest morbidity and mortality rates worldwide, with approximately two million new cases and 1.76 million death cases annually1. Non-small cell lung cancer (NSCLC) accounts for nearly 85% of all lung cancers, and lung adenocarcinoma (LUAD) and lung squamous cell carcinoma (LUSC) are two main subtypes. LUSC accounts for 25-30% of all lung cancer cases, with two-thirds being central type and 1/3 one-third being peripheral type. Central types may exhibit cavity formation and be polypoid toward the bronchial lumen2. Recent advancements in targeted therapy and immunotherapy have revolutionized LUAD management, but LUSC remains largely refractory to these approaches due to its distinct molecular landscape3,4,5. Despite the approval of several drugs for the treatment of LUSC, the 5-year overall survival (OS) rate remains below 18%, with most patients eventually developing resistance to therapy3,4. LUSC is generally believed to originate from squamous metaplasia of bronchial epithelium induced by smoking. Based on the differentiation degree of carcinomatous keratinocytes, LUSC is divided into high, medium, and low differentiation6,7. LUSC frequently metastasizes via lymphatic and hematogenous routes, with direct invasion into mediastinal lymph nodes and peribronchial soft tissues, which leads to a higher incidence of local recurrence after surgery in comparison to other lung cancer types8.
The stages of LUSC are mainly divided into Stage I, Stage II, Stage III, and Stage IV according to the TNM classification (T: primary tumor), N:lymph node involvement, and M: metastasis), which correspond to early, middle, and late clinical stages9,10. Clinically, treatment plans are tailored based on the stage. Stage III patients were categorized into Stage IIIA (T1-3N2M0, T3N1-2M0, T4N0-1M0) and Stage IIIB (T1-4N3M0, T4N2-3M0) corresponding to TNM stages. For Stage IIIA patients, most diagnostic and treatment guidelines recommend a combination of surgery and adjuvant chemotherapy or radical chemoradiotherapy. For Stage IIIB patients who are not suitable for surgery, concurrent chemoradiotherapy is generally employed to control disease progression.
In contrast to LUAD, LUSC exhibits distinct epidemiological characteristics, a lack of effective targeted treatment options, and poor clinical prognosis. The eighth edition of the TNM staging system developed by the American Joint Committee on Cancer (AJCC) is currently utilized for predicting the prognosis of LUSC, but only involves three parameters: tumor size, lymph node, and metastasis11. Therefore, identifying multiple prognostic risk factors through retrospective and prospective studies is crucial to inform individualized treatment strategies for the LUSC population. Existing retrospective and prospective studies related to LUSC have primarily addressed early and advanced cases with patients unsuitable for surgery12,13. Only a few studies have focused on Stage III LUSC patients.
This study leverages the Surveillance, Epidemiology, and End Results (SEER) database to explore the effect of postoperative chemotherapy on OS in patients with Stage III LUSC. Additionally, subgroup analysis was conducted to investigate the effects of postoperative chemotherapy on Stage III LUSC patients, and Cox regression analysis was carried out to identify the risk factors associated with the prognosis of LUSC.
Materials and methods
Data source
The data were sourced from the publicly accessible SEER database, and all authors had access to it. Relevant data were extracted and analyzed via SEER*Stat 8.4.3.
Patient data screening process
LUSC data from the SEER database (n = 59,922) were retrieved. The inclusion criteria were: (1) The years of diagnosis were 2010–2015; (2) The tumor was located in the lung and bronchus; (3) Histology recode: “8050–8089: squamous cell neoplasm”; (4) The follow-up data was complete. The exclusion criteria were: age, race, grade, marital status, and diagnosis confirmation were unknown (n = 23,905); The cases have incomplete follow-up data, unknown survival time, or diagnosis based solely on a death certificate or autopsy (n = 296); Bone, brain, and liver metastases were unknown (n = 1,065). A total of 34,656 cases with complete follow-up data were retrieved. Non-Stage III patients were subsequently excluded (n = 26,257), and information on 8,399 patients with Stage III LUSC was gathered. Further exclusions included cases without surgery (n = 6,527), and those with unknown T stage, N stage, tumor size, and radiotherapy (n = 88). The final cohort comprised 1,784 Stage III patients who underwent surgery. The data filtering process is provided in Fig. 1.
Statistical analysis
All statistical analyses were performed with the help of R (Version 4.4.1). The “MatchIt” and “cowplot” packages were employed for PSM analysis. In this study, the Nearest Neighbor Matching method was employed with a caliper width of 0.05, based on recommendations to balance bias and variance in propensity score matching (PSM)14. Sensitivity analyses performed using alternative caliper widths (0.01 and 0.1) proved the robustness of the matching results (Figures S1-2). Univariate and multivariate Cox regression analysis and Kaplan-Meier (KM) analysis were carried out through the “survival” and “survminer” packages. The proportional hazards assumption was tested. The results are detailed in Supplementary Table 1. Subgroup analysis of the data was conducted with the help of the “jstable” package. Statistical significance was defined as p < 0.05 (two-sided).
Results
Analysis of the incidence trend of LUSC patients
Data on LUSC patients from the SEER database from 2000 to 2019 were divided into two groups by sex to analyze the overall incidence. The results are presented in Fig. 2. Overall, the incidence of LUSC was higher in men than in women. The number of male LUSC patients decreased from 2000 to 2004 and from 2012 to 2016, increased from 2005 to 2012, and fluctuated after 2016. For women, the incidence was stable from 2000 to 2004, showed a significant upward trend from 2004 to 2016, and fluctuated similarly to male LUSC patients after 2016.
Basic characteristics of stage III LUSC patients
PSM was performed for Stage III LUSC patients who underwent surgery between 2010 and 2015. After PSM, the absolute standardized mean difference (AMD) of each variable was < 0.05 (Fig. 3). 619 patients did not receive postoperative chemotherapy before PSM, and 1,165 patients with Stage III LUSC received postoperative chemotherapy. However, after PSM, some unmatched data were excluded, resulting in 492 patients with Stage III LUSC who received postoperative chemotherapy and those who did not receive chemotherapy. This greatly narrowed the gap in the number of patients between the two groups. At the same time, most variables before PSM showed significant differences between patients who received and those who did not, indicating unbalanced baseline characteristics across the two groups. After PSM, all variables except age demonstrated no significant differences between the two groups, suggesting the baseline characteristics across the two groups were largely balanced (Table 1).
Survival and prognosis analysis of stage III LUSC patients
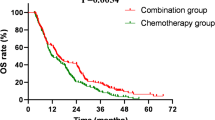
A total of 1,784 samples were selected for OS analysis of different variables before and after PSM. The analysis revealed that patients with left-sided tumors had a markedly lower survival rate in comparison to those with right-sided tumors (P = 0.0051), and the notable difference was reduced after PSM (P = 0.041) (Fig. 4A). The survival rate of patients with different tumor sizes showed significant differences after PSM (Fig. 4B, P = 0.05 before PSM, P = 0.0053 after PSM). Patients with primary tumors located in the upper lobe had higher survival probabilities than those with tumors in the lower or middle lobes. Significant differences in survival rates were observed before PSM (P = 0.00064). However, the significance of this difference was reduced after PSM (P = 0.027) (Fig. 4C). Resection of the lobe or bilobectomy led to the highest survival rate in the early stage, while resection of the total lung resulted in the highest survival rate after 60 months. The survival probability of different groups was significantly different (P = 0.00016), and the significance of the difference was reduced after PSM (P = 0.0091) (Fig. 4D). Patients who received chemotherapy exhibited a significantly higher 5-year OS rate in comparison to those who did not (42% vs. 28%, P < 0.001)(Fig. 4E). This absolute survival benefit remained stable in both unadjusted and propensity score-matched cohorts (P < 0.001).
Survival analysis of patients with Stage III LUSC under different factors and before and after PSM. A: OS analysis of patients with different laterality before (left) and after (right) matching (blue: left; Red: right); B: OS analysis of patients with different tumor sizes before (left) and after (right) matching (dark blue: ≤3 cm; Red: ≥7 cm; green: 3–5 cm; light blue: 5–7 cm); C: OS analysis of patients at different primary sites before (left) and after (right) matching (dark blue: upper lobe; red: lower leaf; green: middle lobe; light blue: other); D: OS analysis of patients with different surgical methods before (left) and after (right) matching (blue: resection of lobe or bilobectomy; red: other; green: pneumonectomy); E: OS analysis of patients who received or did not receive chemotherapy before (left) and after (right) matching (blue: No; red: Yes).
Subgroup analysis of stage III LUSC patients
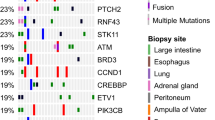
Subgroup analysis demonstrated that chemotherapy was beneficial across nearly all patient characteristics (HR < 1, P < 0.05), except in patients with N0 (HR = 0.93, 95%CI: 0.71–1.22, P = 0.621) or N3 (HR = 0.67, 95%CI: 0.28–1.6, P = 0.367) nodal stages. Notably, the greatest benefit was observed in patients with N1-2 stage and those who underwent pneumonectomy surgery, suggesting the stage- and surgery-dependent efficacy of chemotherapy The two variables, N stage and surgery method, had significant interaction with chemotherapy (P for interaction < 0.05). Detailed results are presented in Fig. 5.
Analysis of risk factors in stage III LUSC patients
The results of the Cox analysis of risk factors in patients with Stage III LUSC are displayed in Table 2. In univariate analysis results, some data in the variables of primary site, tumor size, T stage, and surgery method showed no significant difference (P > 0.05). Given that these data were not representative overall, these factors were not excluded. Subsequently, variables with significant univariate analysis results: age, sex, race, primary site, laterality, tumor size, T stage, surgery method, and chemotherapy were selected (P < 0.05) for multivariate Cox regression analysis. Multivariate Cox regression analysis results indicated that age, sex, race, primary site, tumor size, surgery method, and chemotherapy had significant effects on OS in Stage III LUSC patients.
Discussion
This study is a retrospective cohort research based on the SEER database. The OS of LUSC patients before and after PSM was compared in terms of tumorigenesis and treatment-related factors. Our subgroup analyses revealed that chemotherapy for stage N1-2 patients and patients undergoing surgery yielded greater treatment benefits than patients with other characteristics. Cox regression analysis was performed to screen and obtain important prognostic risk factors for LUSC, including age, sex, race, primary site, tumor size, surgery method, and chemotherapy. These factors are of significant clinical relevance, particularly in guiding postoperative chemotherapy decisions for stage III LUSC. Our findings align with emerging evidence from trials such as CheckMate-816 (neoadjuvant immunotherapy) but highlight the distinct role of postoperative chemotherapy in the absence of immunotherapy15. Recent trials, including KEYNOTE-671, have validated the integration of systemic therapies such as pembrolizumab into multimodal regimens for advanced LUSC16.
PSM is a widely utilized statistical method to mitigate the baseline difference between treatment and control groups in observational studies, thereby simulating the effects of randomized controlled trials. It controls the influence of confounders and reduces the bias of dependent variables by matching individuals with similar propensity scores. It has been extensively applied in some LUSC-related population studies, such as the selection of surgical methods for Stage IA LUSC patients17a comparative study of lobectomy and segmental resection in patients with T stage (> 2 cm and 3 cm) N0M0 NSCLC5and the efficacy of radiotherapy combined with first-line immunotherapy and chemotherapy in advanced LUSC treatment18. PSM is used both in retrospective and prospective studies19. In our study, approximately half of the characteristic variables had AMD values greater than 0.05 between patients who received chemotherapy and those who did not before PSM, while AMD values of the characteristic variables in both groups were less than 0.05 after PSM. PSM significantly balanced the baseline characteristics of the two groups.
It has been proved by ample evidence that PSM alters survival outcomes. For example, in a study assessing the effects of postoperative radiotherapy on the survival of patients with Stage III NSCLC, OS did not significantly differ between patients in the radiotherapy group and non-radiotherapy group (P > 0.05) before PSM, while there was a notable difference in OS between patients in the two group after PSM (P < 0.05)20. In a comparative study of lobectomy and sublobar resection in elderly patients with Stage IA NSCLC (≥ 70 years), before PSM, lobectomy had an obvious advantage in lung cancer-specific survival (p < 0.001). The difference in lung cancer-specific survival was insignificant between the two types of surgery after PSM (p = 0.191)21. In our study, the survival analysis results of patients before and after PSM showed that PSM reduced the significance of factors such as laterality, primary site, and surgical method on the survival of Stage III LUSC patients. Moreover, after PSM, tumor size and chemotherapy markedly ameliorated the survival of patients with Stage III LUSC. These findings also revealed that PSM can effectively reduce the bias of analysis results.
Surgery and chemotherapy are common treatment methods for LUSC. Gao Lin et al. leveraged the SEER database and population data from Chinese hospitals and demonstrated that surgical resection significantly ameliorates OS and LUSC in patients with Stage III NSCLC22. Several clinical studies have also indicated that surgery combined with chemotherapy can improve the prognosis of LUSC patients23. Gu Chen et al. found through a retrospective study that minimizing the treatment interval between neoadjuvant immunochemotherapy and surgery is conducive to achieving better treatment outcomes for LUSC24. The combination of chemotherapy and neoadjuvant therapy is also the first-line treatment for LUSC patients who cannot be surgically resected25. Kazuya Takamochi et al. confirmed that chemotherapy combined with concurrent radiotherapy and surgery in Stage IIIA (N2) LUSC treatment has better therapeutic benefits26. Yuanshan Yao et al. proved that neoadjuvant immune chemotherapy is feasible and relatively safe for patients with resectable Stage III primary NSCLC27. Currently, no studies investigate the effects of postoperative chemotherapy on OS in patients with Stage III LUSC. This study focused on LUSC patients undergoing surgery at Stage III and proved that chemotherapy was beneficial for most LUSC patients with most characteristics. Notably, the greatest therapeutic benefit was brought by postoperative chemotherapy to patients at stage N1-2 and patients with resection of lobe or bilobectomy or pneumonectomy, which aligns with the trend found in previous studies.
While TNM staging stratifies anatomic disease extent, precision oncology necessitates the integration of molecular biomarkers (e.g., PD-L1, STK11/LKB1 mutations) to predict therapeutic response, as evidenced by Lung-MAP and other biomarker-driven platforms28,29. As modern medicine advances and tumor heterogeneity is better understood, precision medicine has garnered increasing attention. Therefore, the staging of patients based on the three factors of TNM can no longer meet the requirements of precision medicine, and further screening of clinically accessible prognostic risk factors is necessary30. In prior studies, Yuting Liu et al. identified age, T stage, N stage, bone metastasis, brain metastasis, liver metastasis, surgery, chemotherapy, and radiotherapy as independent prognostic factors affecting the OS of metastatic LUSC31. Feng Yang et al. highlighted the significance of age, N stage, T stage, liver metastasis, chemotherapy, bone metastasis, and radiotherapy in predicting the survival rate of LUSC patients aged over 45 with brain metastases32. In this study, based on SEER and through Cox regression analysis, age, sex, race, primary site, tumor size, surgery method, and chemotherapy were demonstrated to be significantly correlated with LUSC. Our findings partly align with previous research results, which may arise from the difference in databases, data, and statistical analysis methods.
To our knowledge, this is the first study to evaluate the effects of postoperative chemotherapy on survival in patients with Stage III LUSC. However, the study has several limitations. First, the retrospective design may lead to selection bias, particularly regarding unmeasured confounders such as chemotherapy regimens, dose intensity, and patient adherence. The SEER database lacks granular details on these factors, which possibly influence survival outcomes. Although multiple imputation was considered for handling missing data, the lack of underlying variables limited its application. Consequently, our findings are primarily hypothesis-generating and require further validation through randomized evidence. Secondly, potential factors, such as specific surgical margin information, local recurrence after treatment, the specific type and use plan of chemotherapy drugs, and tobacco use, may be overlooked, thereby affecting patient prognosis. In addition, to obtain as much eligible data as possible, this study selected LUSC patient data from the SEER database from 2010 to 2015. Given the advancements in medical technology since this period, these results have limitations and warrant further validation with updated data. In future studies, we will also include cutting-edge treatments such as immunotherapy and targeted therapy, and combine molecular pathways for further analysis.
Conclusion
In conclusion, this study proves that postoperative chemotherapy significantly improves the prognosis of most Stage III LUSC patients with most characteristics. Notably, patients with N1-2 stage and resection of lobe or bilobectomy or pneumonectomy can obtain the greatest therapeutic benefits through chemotherapy. Moreover, seven factors, namely, age, sex, race, primary site, tumor size, surgery method, and chemotherapy, substantially influence the prognosis of Stage III LUSC. These findings offer valuable insights for clinical decision-making and related studies on the application of chemotherapy in patients with Stage III LUSC resection.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Rao, J. et al. A nomogram for predicting postoperative overall survival of patients with lung squamous cell carcinoma: A SEER-based study. Front. Surg. 10, 1143035. https://doi.org/10.3389/fsurg.2023.1143035 (2023).
Song, G. Q. et al. The necroptosis signature and molecular mechanism of lung squamous cell carcinoma. Aging (Albany NY). 15, 12907–12926. https://doi.org/10.18632/aging.205210 (2023).
Chen, M. et al. Divergent tumor and immune cell reprogramming underlying immunotherapy response and immune-related adverse events in lung squamous cell carcinoma. J. Immunother Cancer. 11 https://doi.org/10.1136/jitc-2023-007305 (2023).
Yang, M. et al. Identification of a cytokine-dominated immunosuppressive class in squamous cell lung carcinoma with implications for immunotherapy resistance. Genome Med. 14, 72. https://doi.org/10.1186/s13073-022-01079-x (2022).
Wang, L., Ge, L., You, S., Liu, Y. & Ren, Y. Lobectomy versus segmentectomy in patients with stage T (> 2 cm and = 3 cm) N0M0 non-small cell lung cancer: a propensity score matching study</at. J. Cardiothorac. Surg. 17, 110. https://doi.org/10.1186/s13019-022-01867-x (2022).
Gomez-Lopez, S., Whiteman, Z. E. & Janes, S. M. Mapping lung squamous cell carcinoma pathogenesis through in vitro and in vivo models. Commun. Biol. 4, 937. https://doi.org/10.1038/s42003-021-02470-x (2021).
Xiao, Z. et al. A TNFR1-UBCH10 axis drives lung squamous cell carcinoma dedifferentiation and metastasis through a cell-autonomous signaling loop. Cell. Death Dis. 13, 885. https://doi.org/10.1038/s41419-022-05308-4 (2022).
Niu, Z., Jin, R., Zhang, Y. & Li, H. Signaling pathways and targeted therapies in lung squamous cell carcinoma: mechanisms and clinical trials. Signal. Transduct. Target. Ther. 7, 353. https://doi.org/10.1038/s41392-022-01200-x (2022).
Gubens, M. A., Davies, M. N. C. C. N. & Guidelines Updates New immunotherapy strategies for improving outcomes in Non-Small cell lung Cancer. J. Natl. Compr. Canc Netw. 17, 574–578. https://doi.org/10.6004/jnccn.2019.5005 (2019).
Mitsudomi, T. et al. Expert consensus recommendations on biomarker testing in metastatic and nonmetastatic NSCLC in Asia. J. Thorac. Oncol. 18, 436–446. https://doi.org/10.1016/j.jtho.2022.10.021 (2023).
Jia, M. et al. Comprehensive analysis of spread through air spaces in lung adenocarcinoma and squamous cell carcinoma using the 8th edition AJCC/UICC staging system. BMC Cancer. 20, 705. https://doi.org/10.1186/s12885-020-07200-w (2020).
Yang, Q. F. et al. Development and validation of an individualized immune prognostic model in stage I-III lung squamous cell carcinoma. Sci. Rep. 11, 12727. https://doi.org/10.1038/s41598-021-92115-0 (2021).
Santos, E. S. & Rodriguez, E. Treatment considerations for patients with advanced squamous cell carcinoma of the lung. Clin. Lung Cancer. 23, 457–466. https://doi.org/10.1016/j.cllc.2022.06.002 (2022).
Austin, P. C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar. Behav. Res. 46, 399–424. https://doi.org/10.1080/00273171.2011.568786 (2011).
Forde, P. M. et al. Neoadjuvant nivolumab plus chemotherapy in resectable lung Cancer. N Engl. J. Med. 386, 1973–1985. https://doi.org/10.1056/NEJMoa2202170 (2022).
Wakelee, H. et al. Perioperative pembrolizumab for Early-Stage Non-Small-Cell lung Cancer. N Engl. J. Med. 389, 491–503. https://doi.org/10.1056/NEJMoa2302983 (2023).
Shao, S. et al. Selection of the surgical approach for patients with cStage IA lung squamous cell carcinoma: A population-based propensity score matching analysis. Front. Oncol. 12, 946800. https://doi.org/10.3389/fonc.2022.946800 (2022).
Qin, J. et al. Efficacy of radiotherapy in combination with first-line immunotherapy and chemotherapy for advanced lung squamous cell carcinoma: a propensity score analysis. Front. Immunol. 14, 1138025. https://doi.org/10.3389/fimmu.2023.1138025 (2023).
Henschke, C. I. et al. Prospective cohort study to compare Long-Term lung Cancer-Specific and All-Cause survival of clinical early stage (T1a-b; =20 mm) NSCLC treated by stereotactic body radiation therapy and surgery</at. J. Thorac. Oncol. 19, 476–490. https://doi.org/10.1016/j.jtho.2023.10.002 (2024).
Wu, K. et al. The impact of postoperative radiotherapy on the survival of patients with stage III non-small cell lung cancer: A CONSORT-compliant analysis using the SEER database. Med. (Baltim). 102, e34015. https://doi.org/10.1097/MD.0000000000034015 (2023).
Zhang, B. et al. Comparison of lobectomy and sublobar resection for stage IA elderly NSCLC patients (>/=70 Years): A Population-Based Propensity Score Matching’s Study. Front. Oncol. 11, 610638. https://doi.org/10.3389/fonc.2021.610638 (2021).
Gao, L., Shen, L., Wang, K. & Lu, S. Propensity score matched analysis for the role of surgery in stage III small cell lung cancer based on the eighth edition of the TNM classification: a population study of the US SEER database and a Chinese hospital. Lung Cancer. 162, 54–60. https://doi.org/10.1016/j.lungcan.2021.10.009 (2021).
Novello, S. et al. Pembrolizumab plus chemotherapy in squamous Non-Small-Cell lung cancer: 5-Year update of the phase III KEYNOTE-407 study. J. Clin. Oncol. 41, 1999–2006. https://doi.org/10.1200/JCO.22.01990 (2023).
Gu, C. et al. Impact of treatment interval between neoadjuvant immunochemotherapy and surgery in lung squamous cell carcinoma. BMC Cancer. 24, 585. https://doi.org/10.1186/s12885-024-12333-3 (2024).
Ren, S. et al. Camrelizumab plus carboplatin and Paclitaxel as First-Line treatment for advanced squamous NSCLC (CameL-Sq): A phase 3 trial. J. Thorac. Oncol. 17, 544–557. https://doi.org/10.1016/j.jtho.2021.11.018 (2022).
Takamochi, K. et al. S-1 + Cisplatin with concurrent radiotherapy followed by surgery for stage IIIA (N2) lung squamous cell carcinoma: results of a phase II trial. Ann. Surg. Oncol. 29, 8198–8206. https://doi.org/10.1245/s10434-022-12490-4 (2022).
Yao, Y., Tang, D., Gao, W. & Zhang, H. Neoadjuvant Immuno-Chemotherapy: A new perspective for stage III NSCLC? Front. Surg. 9, 843987. https://doi.org/10.3389/fsurg.2022.843987 (2022).
Skoulidis, F. et al. STK11/LKB1 mutations and PD-1 inhibitor resistance in KRAS-Mutant lung adenocarcinoma. Cancer Discov. 8, 822–835. https://doi.org/10.1158/2159-8290.CD-18-0099 (2018).
Zhang, C. & Wang, H. Therapeutic utility of Lung-MAP: ushering into an era of genomic and biomarker-driven clinical trials. Signal. Transduct. Target. Ther. 6, 141. https://doi.org/10.1038/s41392-021-00557-9 (2021).
Ng, H. Y. et al. Circulating tumor DNA dynamics as prognostic markers in locally advanced and metastatic esophageal squamous cell carcinoma. JAMA Surg. 158, 1141–1150. https://doi.org/10.1001/jamasurg.2023.4395 (2023).
Liu, Y. et al. Construction and validation of prognosis nomogram for metastatic lung squamous cell carcinoma: A Population-Based study. Technol. Cancer Res. Treat. 21, 15330338221132035. https://doi.org/10.1177/15330338221132035 (2022).
Yang, F., Gao, L., Wang, Q. & Gao, W. Development and validation of prognostic nomograms for lung squamous cell carcinoma with brain metastasis in patients aged 45 years or older: A Population-Based study. Cancer Control. 30, 10732748231202953. https://doi.org/10.1177/10732748231202953 (2023).
Acknowledgements
Not applicable.
Funding
This work was supported by the Medical and Health Science and Technology Project of Zhejiang Province (No. 2024KY1752)
Author information
Authors and Affiliations
Contributions
BX: Conception, investigation, statistical analysis, writing and editing.XH: Conception, supervision, critical review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting, or dissemination plans of this research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, B., He, X. Survival benefit of postoperative chemotherapy in stage III lung squamous cell carcinoma based on SEER database analysis through propensity score matching. Sci Rep 15, 22210 (2025). https://doi.org/10.1038/s41598-025-07766-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07766-0