Abstract
This cross-sectional study involved 7514 pre-myopic male adolescents and examined the refraction and ocular biological parameters of these 15- to 19-year-old adolescents across various regions in China. By comparing the differences in these parameters among different geographic regions and age groups and analyzing the correlations between SER and ocular biological parameters, we found that there were slight variations in the refraction and ocular biological parameters of pre-myopic adolescents across different ages and regions. Specifically, SER was highest in the southern region and AL was lowest in the northern region. This study also revealed negative correlations between SER and variables such as the AL/CR, AL, ACD, PS and age. Notably, AL exhibited the most significant change in pre-myopic adolescents from 15 to 16 years old, followed by gradual stabilization. Other ocular biological parameters, including ACD, LT, and the AL/CR, showed significant changes after the age of 16. These results suggest that AL may be the earliest ocular biological parameter to indicate the onset of myopia, with changes in ACD, LT, and the AL/CR occurring approximately 1 year after changes in AL.
Similar content being viewed by others
Introduction
Myopia is a common disease that mainly occurs during childhood and adolescence. Current epidemiological models predict a substantial increase in myopia prevalence worldwide, with rates expected to rise from 23 to 54% by 20501. The prevalence of high myopia will increase to nearly 1 billion people, accounting for 9.8% of the global population2. Any degree of myopia will increase the risk of pathological changes of ocular tissue, and early-onset myopia is more likely to develop into high myopia3. High myopia and pathological myopia may lead to irreversible vision impairment and even blindness4. Over the past three decades, myopia has not only emerged as a significant public health challenge due to its soaring prevalence, but extensive research efforts have also been dedicated to identifying the risk factors contributing to its onset5. Therefore, it is crucial to find early prognostic indicators of myopia onset and to early identify high-risk groups of myopia in order to proceed timely interventions.
In 2019, the International Myopia Institute (IMI) formally defined ‘pre-myopia’ as a refractive state greater than −0.50 diopter (D) and less than or equal to + 0.75 D in children, as outlined in its white paper on myopia prevention and control6. However, some prior researches3,4 demonstrated that the incidence of myopia remained elevated among adolescents with spherical equivalent refraction (SER, calculated as spherical degree + 1/2 cylinder degree) less than + 1.00 D over a 3-year high school period. Notably, individuals with SER values less than + 0.75 D exhibited a persistently high risk of myopia progression. Therefore, we have consequently extended the application of the “pre-myopia definition” to encompass adolescents. Furthermore, there is a significant likelihood that individuals falling into this category may develop myopia in the future, and it is deemed worthwhile to implement preventative intervention measures. The ocular biological measurement is the measurement of different structural parameters of the eyeball using a variety of examination methods, such as anterior chamber depth (ACD), lens thickness (LT) and axial length (AL). Many studies have reported a high correlation between ocular biometrics and refractive error, with AL to corneal radius of curvature ratio (AL/CR) having the highest correlation with SER ranging from −0.78 diopter (D) to −0.89 D in young adults and −0.61 D to −0.78 D in school-aged children7,8,9. Previous research has primarily focused on the development rules of ocular biometric parameters in myopic children or younger children3,10. However, there was limited research on the changes in refraction and ocular biometric characteristics in pre-myopic adolescents.
It has been gradually recognized that changes in ocular biometric parameters can early indicate the occurrence and development of myopia11,12, and it is also considered as a potential biomarker for evaluating refraction status in children and adolescents13. In this extensive cross—sectional study focusing on Chinese high school students, ocular biometric data were gathered from 7514 pre-myopic adolescents hailing from diverse regions and age groups across the nation. Parameters including LT, ACD, AL, flat keratometry (K1), steep keratometry (K2), central corneal thickness (CCT), white to white distance (WTW), pupil size (PS), AL/CR were analyzed to examine alterations in ocular structures among pre-myopic adolescents, explore the correlations between SER and various biological parameters, and identify potential early indicators of myopia.
Methods
Study design and subjects
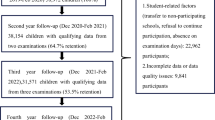
This study was a cross-sectional study on pre-myopic adolescents conducted nationwide from December 2023 to April 2025. A total of 7514 pre-myopic male adolescents aged between 15 to 19 years (17.4 ± 0.9) with −0.50D < SER ≤ + 0.75D and cylinder refraction of 1.50 D or less in both eyes were recruited from the five major regions of China: the Eastern (E) region, mainly encompassing Jiangsu, Anhui, Zhejiang, Jiangxi, and Fujian provinces; the Western (W) region, mainly including Sichuan, Shanxi, Chongqing, Guizhou, and Gansu provinces; the Southern (S) region, mainly covering Hunan, Hubei, Guangxi, and Guangdong provinces; the Northern (N) region, which mainly includes Inner Mongolia, Hebei, Liaoning, Jilin, and Heilongjiang provinces; and the Central (C) region, mainly comprising Henan and Shandong provinces. These adolescents underwent comprehensive ocular examinations conducted by well-trained optometrists and ophthalmologists. Adolescents with a history of ocular trauma, surgery, and pre-existing ocular morbidity that affected vision were excluded14. The study followed the principles of the Declaration of Helsinki. Ethical approval for the study (2023-162-S01, dated 07-13-2023) was obtained from the Air Force Medical Center. Written informed consents were obtained from the students and their parents or legal guardians.
Data collection
Measurements of ocular biometric parameters (CCT, ACD, LT, AL, WTW, PS, K1, K2, and AL/CR) were performed with an ocular biometry system (OA-2000, TOMEY, Japan) in a natural light environment, and the mean of three measurements was taken as the final measurement value15.
Before refraction test was performed, pupils of both eyes were dilated using 0.5% tropicamide-phenylephrine ophthalmic solution (Mydrin-P, Santen, Japan) every 5 min for 4 times. Pupil dilation was determined after 20 min when the fourth drop was instilled. Retinoscopy (Professional Combi, Keeler, UK) was then performed by two experienced optometrists16. The mean value of SER measured by the two optometrists separately was calculated for analysis.
Statistical analysis
All statistical analyses were performed using prism10.1.2 software (GraphPad Software, California, USA). The Kolmogorov‒Smirnov test and the normal distribution histogram method were used to assess the normality of the distributions of the continuous variables15. All measurement data was presented as the mean ± standard deviation (\(\overline{{\text{x}}}\) ± s). The comparisons between groups were made using analysis of variance (one-way ANOVA). Bonferroni method was conducted for pairwise comparisons. The 95% confidence intervals (CIs) were calculated for pairwise comparisons of different paired samples. Simple linear regression analysis was performed between K1, K2, AL, ACD, LT, CCT, PS, WTW, AL/CR and SER. Data from the right eyes were included for statistical analysis. The significance level was set at P < 0.05.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Refractions and ocular biological parameters of all pre-myopic adolescents
The average SER refraction in all pre-myopic adolescents was 0.20 ± 0.37 D. The ocular biological parameters were 42.00 ± 1.28 D for K1, 43.05 ± 1.40 D for K2, 23.93 ± 0.66 mm for AL, 3.61 ± 0.26 mm for ACD, 3.59 ± 0.20 mm for LT, 541.30 ± 32.62 μm for CCT, and 5.67 ± 0.88 mm for PS, 12.07 ± 0.49 mm for WTW and AL/CR was 3.01 ± 0.06 (Fig. 1).
Comparison of refractions and ocular biological parameters in pre-myopic adolescents in different geographical groups
The K1 and K2 of pre-myopic adolescents in northern region were significantly higher than those in other regions (K1: N vs. S, P = 0.001; N vs. W, P = 0.037; N vs. E, P = 0.003; N vs. C, P = 0.002) (K2: N vs. S, P < 0.001; N vs. W, P = 0.001; N vs. E, P = 0.000; N vs. C, P = 0.002), while AL was significantly lower than that in other regions (N vs. S, P = 0.000; N vs. E, P = 0.005; N vs. C, P = 0.009). The ACD in central region was significantly lower than that in other regions (C vs. S, P < 0.001; C vs. W, P < 0.001; C vs. E, P < 0.001; C vs. N, P = 0.011). The CCT in western region was significantly lower than that in other regions (W vs. S, P < 0.001; W vs. N, P = 0.012; W vs. C, P = 0.008). The PS was lower in southern and central regions than that in other regions (P < 0.001). SER was highest in southern region (0.25 ± 0.37 D), followed by western (0.21 ± 0.37 D), northern (0.20 ± 0.37 D), eastern (0.18 ± 0.36 D) and central region (0.14 ± 0.35 D), as shown in Table 1 and Fig. 2.
Comparison of refractions and ocular biological parameters in pre-myopic adolescents of different age groups
The AL of adolescents in the 15 years old group was significantly lower than that in 16 and 17 years old group (15 vs. 16, P = 0.009, 15 vs. 17, P = 0.013), and there was no significant difference among 16–19 year old groups (16 vs. 17, P = 0.999, 16 vs. 18, P = 0.640, 16 vs. 19, P = 0.843, 17 vs. 18, P = 0.999, 17 vs. 19, P = 0.999, 18 vs. 19, P = 0.999). The ACD and LT of the 15 years old group were significantly lower than those among the 17–19 years old groups (15 vs. 17, P < 0.001, 15 vs. 18, P < 0.001, 15 vs. 19, P < 0.001), and there were no significant differences in ACD and LT among 17–19 years old groups (P = 0.999). The CCT of 15 years old group and 16 years old group was significantly higher than that among 17–19 years old groups (15 vs. 17, P < 0.001, 15 vs. 18, P < 0.001, 15 vs. 19, P < 0.001, 16 vs. 17, P < 0.001, 16 vs. 18, P < 0.001, 16 vs. 19, P < 0.001), and no significant difference was seen among 17–19 years old groups (P = 0.999). The PS increased with age among 15–17 years old groups (P < 0.001), and there was no significant difference among 17–19 years old groups (17 vs. 18, P = 0.086, 17 vs. 19, P = 0.999, 18 vs. 19, P = 0.765). The AL/CR of 15 years old groups was significantly lower than that among 16–19 years old groups (15 vs. 16, P = 0.013, 15 vs. 17, P = 0.005, 15 vs. 18, P < 0.001, 15 vs. 19, P = 0.000), and no significant difference was seen among 16 to 19 years old groups (16 vs. 17, P = 0.999, 16 vs. 18, P = 0.999, 16 vs. 19, P = 0.999, 17 vs. 18, P = 0.135, 17 vs. 19, P = 0.999, 18 vs. 19, P = 0.999). There were no significant differences in K1 (P = 0.416) and K2 (P = 0.063) among the 15 to 19 years old groups (Table 2, Fig. 3).
Correlation analysis between SER and ocular biological parameters
Pearson correlation analysis showed that SER was positively correlated with LT (r = 0.132, P < 0.001) and WTW (r = 0.034, P = 0.002) and negatively correlated with AL (r = −0.206, P < 0.001), ACD (r = −0.168, P < 0.001), PS (r = −0.034, P = 0.003), AL/CR (r = −0.306, P < 0.001) and age (r = −0.090, P < 0.001) as shown in Table 3. There was no significant correlation between SER with K1 (r = −0.018, P = 0.115), K2 (r = −0.016, P = 0.165), and CCT (r = −0.009, P = 0.420) (Table 3, Fig. 4). The correlation between SER and AL and AL/CR is higher than the other ocular biological parameters.
Discussion
This study investigated the refraction and ocular biological parameters of 15–19 years old pre-myopic adolescents across all regions of China, compared the differences of these parameters according to different geographic regions and different age groups, and analyzed the correlations between SER and ocular biological parameters. This study showed that the refraction and ocular biological parameters of pre-myopic adolescents were slightly different in separate ages and geographic regions. The SER was highest in the southern region and the lowest was in middle region, which further suggested that we should pay more attention to the refractive status and myopia onset of adolescents in the middle region.
This study found that SER had negative correlations with variables such as AL/CR, AL, ACD and age, which is consistent with the findings of several studies17,18,19. AL is closely associated with the development of myopia and often changes significantly especially with the growth of children and adolescents20. Compared with European and American children, axial lengths generally perform faster in Asian children21. Studies have shown that AL grows rapidly after birth and could reach the level of emmetropic eye of about 23 mm at the age of 3, and then growing at a rate of about 0.1 mm per year, reaching adult level at the age of 13–1422, and this conclusion is consistent with the findings of this study, which indicate that the AL of adolescents aged 15–19 tends to stabilize. A previous study found that there was a weak correlation between SER and AL in pre-myopic adolescent students, which may be related to the involvement of multiple ocular biometric parameters in the onset and progression of myopia13. Interestingly, this study found that AL exhibited the most pronounced changes in pre-myopic adolescents between 15 and 16 years of age, followed by gradual stabilization. Other ocular biological parameters such as ACD, LT, and AL/CR showed significant changes after the age of 16, suggesting that AL may be the earliest ocular biological parameter for the myopia shift, while changes of ACD, LT, and AL/CR occurred about 1 year after the change of AL.
The AL/CR is considered to be a surrogate indicator for the detection of cycloplegic refraction and can be used to assess the risk of myopia incidence and progression. Grosvenor and Scott23 first proposed the correlation between AL/CR and SER and they found that even small changes in AL/CR led to significant changes in SER. In an investigation of 3922 children aged 6–12 years, He et al6. found that the correlation between AL/CR and SER was lower in emmetropic children and higher in children with moderate hyperopia and myopia. This study demonstrates a weak negative correlation between SER and the AL/CR in pre-myopic adolescents, which is largely in line with the findings of He’s study. Moreover, AL/CR > 3 is considered to be a high-risk indicator for the myopia onset8. The higher the AL/CR is, the greater the possibility of myopia occurrence24, indicating that AL/CR can cooperate with AL changes to analyze and predict the occurrence and development of myopia, and providing a strong basis for early intervention of myopia25. The study participants were adolescents in the pre-myopic stage, exhibiting an AL/CR that fluctuated around 3. This observation implies that screening high—risk students by considering the AL/CR and changes in AL could be instrumental in implementing timely intervention strategies.
ACD is an important component of AL, and studies have shown that ACD gradually increases during the development from hyperopia to high myopia20,21,22,23,24,25,26. This study found that ACD deepened with decreasing SER in pre-myopic adolescents, which was similar to the findings of Dogan et al.27. However, this study also found that the correlation between ACD and SER was not significant in pre-myopic adolescents, which may be related to the low correlation between AL and SER.
The relationship between pupil diameter and myopia remains controversial. A previous study has demonstrated that pupil-related parameters can exert an influence on myopia development28, and larger pupil diameter had an inhibitory effect on myopia progression29,30,31. Another study showed that increase of pupil area will increase peripheral defocus, thus accelerating the development of myopia32. However, a subsequent study found that there was no significant correlation between pupil diameter and myopia33. Recently, Xu et al.34 first proposed a nonlinear correlation between pupil diameter and SER, that is, pupil diameter decreases as SER becomes negative, pupil diameter tends to increase when SER near hyperopia, and when SER further approaches hyperopia, pupil diameter tends to stabilize instead of increase. This finding may explain the low negative correlation between pupil diameter and SER in this study.
Unlike other studies, the advantage of this study is that focus on the pre-myopic adolescents aged 15–19 years old across different regions of China in a large sample size. So, the results of this study can better reflect the current refractive status and ocular biological parameters in pre-myopic Chinese adolescents. The limitations of this study are as follows: First, this was a cross-sectional study, which cannot better reflect the pattern of change in refraction and ocular biologic parameters than follow-up study. Nonetheless, the students in this study had a high degree of similarity in their living and learning environments in China, so this present cross-sectional study may also reflect the pattern of change in refraction and ocular biologic parameters to some extent. Second, only male subjects were included in this study. Tao et al.35 found that there were some differences of ocular biological parameters in different genders among adolescents aged 15–21 years. Third, regions and age groups were not randomly selected, however, the students who participated in the physical examinations were not pre-screened. The current study delineated the distribution characteristics and evolutionary patterns of refractive errors and ocular biological parameters across varying age groups and geographical regions among male adolescents. We will further expand the scope of research subjects, including different genders in the future.
To summarize, this study revealed that there were certain differences in ocular biological parameters of pre-myopic adolescents in separate regions or at different ages, and a variety of factors were involved in the onset and development of myopia. SER was positively correlated with LT and WTW, and negatively correlated with AL, ACD, PS, AL/CR, and age. There was no significant correlation between SER and K1, K2, and CCT, AL/CR had a higher correlation with SER than other ocular biological parameters. In addition, the change of AL was about 1 year earlier than the change of ACD, LT and AL/CR, indicating that AL may be the earliest ocular biological parameter for myopia onset. Therefore, regular monitoring of AL and AL/CR enables early detection and intervention of high-risk adolescents, which is an important strategy to reduce the incidence of myopia.
Data availability
data is provided within the manuscript files.
References
Dong, J., Zhu, Z., Xu, H. & He, M. Myopia control effect of repeated low-level red-light therapy in Chinese children: A randomized, double-blind, controlled clinical trial. Ophthalmology 130(2), 198–204. https://doi.org/10.1016/j.ophtha.2022.08.024 (2023).
Holden, B. A. et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123(5), 1036–1042. https://doi.org/10.1016/j.ophtha.2016.01.006 (2016).
Hu, Y. et al. Association of age at myopia onset with risk of high myopia in adulthood in a 12-year follow-up of a Chinese cohort. JAMA Ophthalmol. 138(11), 1129–1134. https://doi.org/10.1001/jamaophthalmol.2020.3451 (2020).
Bullimore, M. A. & Brennan, N. A. Myopia control: Why each diopter matters. Optom. Vis. Sci. 96(6), 463–465. https://doi.org/10.1097/opx.0000000000001367 (2019).
Baird, P. N. et al. Myopia. Nat. Rev. Dis. Primers 6(1), 99. https://doi.org/10.1038/s41572-020-00231-4 (2020).
Flitcroft, D. I. et al. IMI - defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Invest. Ophthalmol. Vis. Sci. 60(3), M20-m30. https://doi.org/10.1167/iovs.18-25957 (2019).
He, X. et al. Normative data and percentile curves for axial length and axial length/corneal curvature in Chinese children and adolescents aged 4–18 years. Br. J. Ophthalmol. 107(2), 167–175. https://doi.org/10.1136/bjophthalmol-2021-319431 (2023).
He, X. et al. Axial length/corneal radius ratio: Association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS ONE 10(2), e0111766. https://doi.org/10.1371/journal.pone.0111766 (2015).
Kimura, S., Hasebe, S., Miyata, M., Hamasaki, I. & Ohtsuki, H. Axial length measurement using partial coherence interferometry in myopic children: Repeatability of the measurement and comparison with refractive components. Jpn. J. Ophthalmol. 51(2), 105–110. https://doi.org/10.1007/s10384-006-0410-5 (2007).
Jones-Jordan, L. A. et al. Myopia progression as a function of sex, age, and ethnicity. Invest. Ophthalmol. Vis. Sci. 62(10), 36. https://doi.org/10.1167/iovs.62.10.36 (2021).
Loughman, J. & Flitcroft, D. I. Are digital devices a new risk factor for myopia? Lancet Digit Health 3(12), e756–e757. https://doi.org/10.1016/s2589-7500(21)00231-4 (2021).
Morgan, I. G. et al. IMI risk factors for Myopia. Invest. Ophthalmol. Vis. Sci. 62(5), 3. https://doi.org/10.1167/iovs.62.5.3 (2021).
Zhang, Z. et al. Correlation between refractive errors and ocular biometric parameters in children and adolescents: A systematic review and meta-analysis. BMC Ophthalmol. 23(1), 472. https://doi.org/10.1186/s12886-023-03222-7 (2023).
Yao, L. et al. Refractive change and incidence of myopia among a group of highly selected senior high school students in China: A prospective study in an aviation cadet prerecruitment class. Invest. Ophthalmol. Vis. Sci. 60(5), 1344–1352. https://doi.org/10.1167/iovs.17-23506 (2019).
Xiang, Y. et al. Myopia prevalence and ocular biometry in children and adolescents at different altitudes: A cross-sectional study in Chongqing and Tibet, China. BMJ Open 14(5), e078018. https://doi.org/10.1136/bmjopen-2023-078018 (2024).
Qi, L. S. et al. Risk factors for incident myopia among teenaged students of the experimental class of the air force in China. J. Ophthalmol. 2019, 3096152. https://doi.org/10.1155/2019/3096152 (2019).
Hashemi, H. et al. Axial length to corneal radius of curvature ratio and refractive errors. J. Ophthal. Vis. Res. 8(3), 220–226 (2013).
Rozema, J., Dankert, S., Iribarren, R., Lanca, C. & Saw, S. M. Axial growth and lens power loss at myopia onset in singaporean children. Invest. Ophthalmol. Vis. Sci. 60(8), 3091–3099. https://doi.org/10.1167/iovs.18-26247 (2019).
Zhang, Y. et al. The guiding significance of ocular biometry in evaluating the refractive status of preschool children. Ophthal. Res. 66(1), 1213–1221. https://doi.org/10.1159/000533782 (2023).
Zadnik, K. et al. Ocular component data in schoolchildren as a function of age and gender. Optom. Vis. Sci. 80(3), 226–236. https://doi.org/10.1097/00006324-200303000-00012 (2003).
Wong, Y. L. et al. Percentile charts for normal axial length changes in chinese schoolchildren with stable emmetropia. Invest. Ophthalmol. Vis. Sci. 62(8), 2323–2323 (2021).
Park, S. H., Park, K. H., Kim, J. M. & Choi, C. Y. Relation between axial length and ocular parameters. Ophthalmologica 224(3), 188–193. https://doi.org/10.1159/000252982 (2010).
Grosvenor, T. & Scott, R. Role of the axial length/corneal radius ratio in determining the refractive state of the eye. Optom. Vis. Sci. 71(9), 573–579. https://doi.org/10.1097/00006324-199409000-00005 (1994).
Li, S. M. et al. Annual incidences and progressions of myopia and high myopia in Chinese schoolchildren based on a 5-year cohort study. Invest. Ophthalmol. Vis. Sci. 63(1), 8. https://doi.org/10.1167/iovs.63.1.8 (2022).
Xu, G. et al. Distribution of white-to-white corneal diameter and anterior chamber depth in chinese myopic patients. Front. Med. (Lausanne). 8, 732719. https://doi.org/10.3389/fmed.2021.732719 (2021).
Khorrami-Nejad, M., Moradi, R., Akbarzadeh Baghban, A. & Khosravi, B. Effect of axial length and anterior chamber depth on the peripheral refraction profile. Int. J. Ophthalmol. 14(2), 292–298. https://doi.org/10.18240/ijo.2021.02.17 (2021).
Dogan, M., Elgin, U., Sen, E., Tekin, K. & Yilmazbas, P. Comparison of anterior segment parameters and axial lengths of myopic, emmetropic, and hyperopic children. Int. Ophthalmol. 39(2), 335–340. https://doi.org/10.1007/s10792-017-0816-8 (2019).
Pan, C. W. et al. Iris colour in relation to myopia among Chinese school-aged children. Ophthal. Physiol. Opt. 38(1), 48–55. https://doi.org/10.1111/opo.12427 (2018).
Chen, X. et al. Factors determining the myopia control effect of an orthokeratology lens: A two-year multi-level model. Ophthal.ic Physiol. Opt. 42(4), 786–796. https://doi.org/10.1111/opo.12990 (2022).
Fang, J. et al. Machine learning for predicting the treatment effect of orthokeratology in children. Front. Pediatr. 10, 1057863. https://doi.org/10.3389/fped.2022.1057863 (2022).
Xu, S. et al. Development and validation of a prediction model for axial length elongation in myopic children treated with overnight orthokeratology. Acta Ophthalmol. 99(5), e686–e693. https://doi.org/10.1111/aos.14658 (2021).
Charman, W. N. Aberrations and myopia. Ophthal. Physiol. Opt. 25(4), 285–301. https://doi.org/10.1111/j.1475-1313.2005.00297.x (2005).
Orr, J. B., Seidel, D., Day, M. & Gray, L. S. Is pupil diameter influenced by refractive error? Optom. Vis. Sci. 92(7), 834–840. https://doi.org/10.1097/opx.0000000000000627 (2015).
Xu, S. et al. Association between myopia and pupil diameter in preschoolers: Evidence from a machine learning approach based on a real-world large-scale dataset. Ophthalmol. Ther. 13(7), 2009–2022. https://doi.org/10.1007/s40123-024-00972-5 (2024).
Tao, Y. et al. Changes in ocular biological parameters after cycloplegia based on dioptre, age and sex. Sci. Rep. 12(1), 22470. https://doi.org/10.1038/s41598-022-25462-1 (2022).
Author information
Authors and Affiliations
Contributions
Siyuan Chen. and Lu Yao. designed study and wrote the paper. Xuefeng Wang. Chen Zhao. Yan Tang. and Yu Wang. Zhikang Zou.analyzed data. Yong Liu. and Linsong Qi. revised the paper. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, S., Yao, L., Wang, X. et al. Comparative analysis of refractive errors and ocular biological parameters among pre-myopic adolescents across different age groups and geographical regions. Sci Rep 15, 23836 (2025). https://doi.org/10.1038/s41598-025-08658-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08658-z