Abstract
This study examined the association between circulating interleukin-37 (IL-37) levels and systemic lupus erythematosus (SLE), as well as the relationship between IL-37 gene polymorphisms and susceptibility to SLE. Relevant studies were identified through extensive searches of the Medline, Embase, and Web of Science databases up to December 2024. A meta-analysis was conducted to compare serum/plasma IL-37 levels in SLE patients with those in controls and to evaluate the association between IL-37 gene polymorphisms and SLE risk. Twelve studies comprising 1,229 SLE patients and 745 controls were analyzed. The meta-analysis revealed higher IL-37 levels in SLE patients compared to controls (SMD: 0.570, 95% CI-0.070–1.210, p = 0.0803), though the difference was not statistically significant. Subgroup analysis showed a significant association in Asians (SMD: 0.730, 95% CI: 0.151–1.310, p = 0.010), but not in Arabs (SMD: 0.410, 95% CI: -0.780–1.600, p = 0.500). Analysis of the original data indicated significant results (SMD: 1.026, 95% CI: 0.505–1.547, p < 0.001), while the re-calculated data did not. Studies conducted before 2019 revealed a significant association (SMD: 0.906, 95% CI: 0.438–1.374, p < 0.001), unlike more recent studies. Higher IL-37 levels were observed in patients with lupus nephritis, although these findings were not statistically significant. Genetic analysis of IL-37 rs3811047 polymorphism revealed no significant association in Arabs (OR: 1.432, 95% CI: 0.607–3.373, p = 0.413), whereas a significant association was noted in Asians (OR: 0.649, 95% CI: 0.448–0.941, p = 0.023). The meta-analysis demonstrated significantly elevated IL-37 levels in SLE patients among Asians, along with a significant association between IL-37 polymorphisms and SLE.
Similar content being viewed by others
Introduction
Systemic lupus erythematosus (SLE) is a complex autoimmune disease characterized by chronic inflammatory processes and multisystem involvement1,2. The clinical manifestations of the disease, which include arthritis, nephritis, rash, and hematological abnormalities, complicate its diagnosis and management3. Despite significant advances, the precise pathogenic mechanisms of SLE remain elusive, with a combination of genetic, environmental, and immunological factors acknowledged as crucial to its development4.
Interleukin-37 (IL-37), a member of the IL-1 cytokine family, has attracted attention for its anti-inflammatory properties5. Unlike other cytokines that promote inflammation, IL-37 serves as a natural immune suppressor by attenuating proinflammatory responses. This is achieved through the inhibition of nuclear factor-kappa B (NF-κB) and mitogen-activated protein kinase (MAPK) pathways, as well as by augmenting anti-inflammatory cytokines such as IL-10. Elevated circulating IL-37 levels have been observed in inflammatory and autoimmune conditions, suggesting a potential compensatory role in reducing excessive immune activation6. Nevertheless, the relationship between IL-37 and SLE remains contentious. Whereas certain studies report elevated IL-37 levels in SLE patients, others find no significant differences compared to healthy controls, thus highlighting inconsistencies that necessitate further investigation7,8,9,10,11,12,13,14,15,16,17,18.
In addition to circulating levels of IL-37, genetic variations in the IL-37 gene may influence susceptibility to SLE. Polymorphisms in IL-37 have been suggested to modulate cytokine expression or activity, thereby affecting disease risk. For example, single nucleotide polymorphisms (SNPs) such as rs3811047 have been investigated in the context of autoimmune diseases, including SLE, with varying results7,8,9,18. This variability in outcomes among studies may be due to differences in study design, population ethnicity, or sample size. A comprehensive review and meta-analysis are essential to elucidate the correlation between IL-37 and SLE, as previous studies have yielded inconsistent results19,20. This meta-analysis aimed to assess the relationship between blood IL-37 levels and/or genetic variations and the risk of SLE.
Materials and methods
Selecting relevant studies and data extraction
We conducted a thorough review of the scientific literature to identify studies that assess circulating IL-37 levels (in serum or plasma) and their correlation with SLE, as well as those investigating IL-37 gene polymorphisms in SLE. Searches were executed in Medline, Embase, and Web of Science databases for articles published up to December 2024, employing the search terms “IL-37,” “serum OR plasma OR circulating OR blood,” “polymorphism,” and “systemic lupus erythematosus.” Additionally, the reference lists of identified studies were scrutinized to unearth pertinent publications not indexed in these databases.
Studies were included if they conformed to the following criteria: (1) case-control, cohort, or group-based studies; (3) examined IL-37 gene polymorphisms in both SLE and control populations. Exclusion criteria comprised review articles, case reports, studies with overlapping data, those devoid of adequate information, or studies deviated from Hardy-Weinverg equilibrium (HWE) for meta-analysis. Data extraction encompassed author names, publication year, study location, participant ethnicity, adjustments for age and sex, participant numbers, IL-37 levels (mean and standard deviation), and allele/genotype frequencies of IL-37 polymorphisms. For articles reporting medians, interquartile ranges, or ranges, means and standard deviations were computed using established formulae21,22. Two independent reviewers performed the data extraction and analysis, with any discrepancies resolved through consensus. This research is in the process of being officially recorded with PROSPERO (ID 1074104). The meta-analysis was conducted in accordance with PRISMA guidelines23.
Statistical analysis
A meta-analysis was conducted to explore the association between IL-37 levels and SLE, as well as the allelic effects of IL-37 gene variants. Continuous variables were analyzed using standardized mean differences (SMDs) and 95% confidence intervals (CIs), while dichotomous variables were assessed using odds ratios (ORs) and 95% CIs. Cochran’s Q-statistics were utilized to evaluate heterogeneity both within and between studies, with a significance threshold set at P < 0.1024. A random-effects model was employed in cases of significant heterogeneity, whereas a fixed-effects model was adopted in its absence25,26. The degree of inconsistency among the studies was quantified using the I2 statistic, with values of 25%, 50%, and 75% indicating low, moderate, and high heterogeneity, respectively. Statistical analyses were conducted utilizing Review Manager software (RevMan version 5.4).
Quality assessment, sensitivity test and publication Bias
The quality of included studies was assessed using the Newcastle-Ottawa Scale, with scores ranging from six to nine indicating high methodological quality27. Meta-regression analyses explored potential sources of heterogeneity, including gender ratio, lupus nephritis, Systemic Lupus Erythematosus Disease Activity Index (SLEDAI), mean allele frequency in control group, mean age and disease duration. Sensitivity analyses were conducted to evaluate the influence of individual studies on the overall effect size. Publication bias was assessed using funnel plots and Egger’s linear regression test28which evaluated asymmetry in funnel plots predicated on SMDs or ORs on a natural logarithmic scale.
Results
Studies included in the meta-analysis
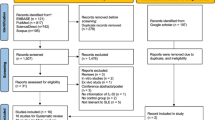
We identified 140 records through manual and computerized search techniques, drawing from sources including Medline, Embase, and Web of Science. Sixteen reports were assessed for eligibility, of which five were excluded for reasons such as data unavailability, their nature as review articles, or focus on other diseases. Ultimately, twelve studies met the inclusion criteria and were incorporated in the meta-analysis7,8,9,10,11,12,13,14,15,16,17,18 (Fig. 1). The meta-analysis primarily investigated the IL-37 polymorphism rs3811047. Four studies addressed the IL-37 polymorphism rs3811047 exclusively. Further, rs3811046 was explored in one study and rs2723186, rs2723176, and rs4364030 in another. In each case, the IL-37 polymorphisms in the control groups complied with HWE. Each study received a quality rating of five to eight on the NOS. Details of participant demographics and quality evaluations are presented in Table 1.
Circulating IL-37 levels and SLE susceptibility
The meta-analysis demonstrated that circulating IL-37 levels were elevated in patients with SLE compared to controls, yielding an overall SMD of 0.570 (95% CI: − 0.070–1.210, p = 0.080); however, this finding did not reach statistical significance (Table 2). Subgroup analyses by ethnicity revealed a significant association in Asian populations (SMD: 0.730, 95% CI: 0.151–1.310, p = 0.010), while no significant 0association was detected in Arab populations (SMD: 0.410, 95% CI: 0.780–1.600, p = 0.500) (Table 2; Fig. 2). Studies with a sample size greater than or equal to 100 reported an SMD of 0.726 (95% CI: − 0.296–1.747, p = 0.164), whereas studies with fewer than 100 participants showed an SMD of 0.430 (95% CI: − 0.054–0.914, p = 0.082), with neither group achieving statistical significance. Results from original studies indicated a significant association (SMD: 1.026, 95% CI: 0.505–1.547, p < 0.001), in contrast to those calculated, which did not show significance (SMD: 0.350, 95% CI: − 0.512–1.212, p = 0.426). Stratification by publication year showed that older studies (published before 2019) demonstrated a significant association (SMD: 0.906, 95% CI: 0.438–1.374, p < 0.001), while more recent studies (published in or after 2019) did not (SMD: 0.143, 95% CI: − 1.149–1.436, p = 0.828) (Table 2). Additionally, in studies comparing patients with and without LN, IL-37 levels were found to be higher in LN + patients (SMD: 0.560, 95% CI: − 0.071–1.191, p = 0.082), although the results were not statistically significant. The meta-analysis of correlation coefficients revealed no significant relationship between IL-37 levels and Systemic Lupus Erythematosus Disease Activity Index (correlation coefficient: 0.266, 95% CI: − 0.570–0.607, p = 0.215). Notably, significant heterogeneity was observed across most subgroups, highlighting variability in the study findings.
IL-37 rs3811047 polymorphisms and SLE susceptibility
This meta-analysis did not confirm a significant association between the IL-37 rs3811047 A vs. G polymorphism and SLE (OR = 1.178, 95% CI = 0.549–2.526, p = 0.675) (Table 3). The analysis for the Arab population also indicated no significant association (OR = 1.393, 95% CI = 0.568–3.419, p = 0.469). However, the Asian population exhibited a borderline significant association with this polymorphism (OR = 0.725, 95% CI = 0.525–1.000, p = 0.050) (Fig. 3). The dominant model (AA + AG vs. GG) similarly revealed no significant overall association (OR = 1.148, 95% CI = 0.514–2.562, p = 0.777). The Arab population again showed no significant association, while the Asian population demonstrated a significant association with the polymorphism (OR = 0.649, 95% CI = 0.448–0.941, p = 0.023).
Heterogeneity, sensitivity test and publication bias
Heterogeneity among the studies was observed in the meta-analysis examining IL-37 levels in patients with SLE (Table 2). Significant variability was noted, influenced by factors such as sample size, publication year, data format, and ethnicity (p < 0.05). Meta-regression analysis showed that gender ratio, lupus nephritis, SLEDAI, and mean allele frequency in control group, but not mean age and disease duration, had significant impacts on heterogeneity in the meta-analyses of IL-37 (Supplementary data). Sensitivity testing indicated that the exclusion of two particular studies significantly impacted the results of the meta-analysis8,10. Sensitivity analysis showed that no individual study significantly affected the pooled effect size in IL-37 levels except for Nijeeb 20248, indicating that the results of this meta-analysis are robust. Additionally, meta-analyses of IL-37 polymorphisms displayed inter-study variability (Table 3). Although publication bias is a common concern in meta-analyses, characterized by an overrepresentation of positive findings, no evidence of publication bias was detected in this instance. The funnel plot exhibited no asymmetry, and Egger’s regression test yielded p-values above 0.05.
Discussion
This meta-analysis demonstrated that circulating IL-37 levels are higher in patients with SLE compared to healthy controls, although the overall difference did not achieve statistical significance. However, subgroup analyses revealed a significant association in Asian populations, where the effect size suggests moderately elevated levels of IL-37. This finding corresponds with studies suggesting that IL-37 serves as a compensatory anti-inflammatory cytokine, mitigating the pro-inflammatory environment of autoimmune diseases such as SLE. The absence of a significant association in Arab populations and in the overall pooled analysis could be ascribed to the heterogeneity of study designs, variations in assay techniques, and differences in patient characteristics such as disease severity or treatment regimens.
The observed ethnic variability in IL-37 levels is particularly notable. Ethnic differences in immune responses and genetic predispositions, well-documented in SLE, reveal that Asians generally exhibit higher disease severity and distinct cytokine profiles compared to other populations. These findings highlight the critical importance of considering ethnicity in immunological research and suggest that IL-37 may play a more central role in SLE pathogenesis in certain populations. Interestingly, the meta-analysis identified a significant association in studies conducted before 2019, whereas more recent studies did not confirm this relationship. This discrepancy could reflect advances in SLE management, including the widespread use of immunosuppressants and biologics, which might influence cytokine levels. Alternatively, variations in study quality or reporting biases could explain this trend. Although IL-37 levels appeared elevated in patients with LN compared to those without, this difference did not reach statistical significance. Given IL-37’s known anti-inflammatory properties, its elevation in LN patients might represent a compensatory response to increased renal inflammation. However, the limited number of studies addressing this specific subgroup and their small sample sizes underscore the need for further research.
The analysis of IL-37 genetic variants, particularly the rs3811047 polymorphism, revealed an association with SLE susceptibility in Asians, but not in Arabs. Specifically, the rs3811047 polymorphism was protective in Asian populations, significantly reducing SLE risk. This observation underscores the potential role of genetic variations in modulating IL-37 expression or function, thereby influencing SLE pathogenesis. The absence of a significant association in Arabs could be attributed to differences in linkage disequilibrium patterns, allele frequencies, or environmental factors that affect gene-environment interactions. Additionally, the relatively small number of studies focusing on Arab populations may reduce the statistical power needed to detect subtle genetic effects. These findings emphasize the necessity for larger, ethnically diverse cohorts to better understand the genetic determinants of IL-37 in SLE.
The current meta-analysis differs from previous studies in several crucial aspects29,30. It expands upon these findings by incorporating a wider range of studies up to December 2024, covering diverse populations beyond the Chinese demographic, unlike earlier analyses. It evaluates both circulating IL-37 levels and multiple IL-37 gene polymorphisms, including rs3811047, in relation to SLE susceptibility. Furthermore, it conducts subgroup analyses to examine the effects of ethnicity, study publication date, and specific clinical manifestations such as lupus nephritis on IL-37 levels and genetic associations. This comprehensive approach offers a more detailed exploration of IL-37’s role in SLE across various populations and clinical contexts. Rs3811047 has not been reported as an eQTL for IL-37. However, this means there isn’t direct evidence that this SNP influences IL-37 expression levels in tissues.
This meta-analysis identifies several limitations. Heterogeneity presents an opportunity for deeper insight through subgroup and meta-regression analyses; however, the between-studies heterogeneity observed in this study posed a limitation. Despite this, meta-regression analysis provided valuable findings, demonstrating that gender ratio, the prevalence of lupus nephritis, SLEDAI scores, and the mean allele frequency in the control group significantly influenced the heterogeneity observed in the meta-analyses of IL-37. Moreover, the cross-sectional design of most studies prevents causal interpretations concerning the relationship between IL-37 and SLE. Future research should prioritize longitudinal studies to evaluate changes in IL-37 levels in relation to disease activity and treatment. Mechanistic investigations are also necessary to elucidate the pathways through which IL-37 influences SLE. Additionally, broader genetic analyses that include other IL-37 polymorphisms and multi-ethnic studies will provide a fuller understanding of its genetic implications.
In conclusion, this meta-analysis demonstrated that Asian SLE patients exhibited notably higher IL-37 levels, with a significant correlation between IL-37 gene polymorphisms and SLE susceptibility in this group. Conversely, no significant associations were found among Arab populations, highlighting the impact of ethnic and study-specific factors on IL-37 levels in SLE. Further research is imperative to validate these findings and to further explore the mechanisms by which IL-37 contributes to SLE pathogenesis.
Data availability
All data generated or analyzed in this study are presented within the article. Any additional inquiries should be directed to the corresponding author.
References
Han, J. Y., Cho, S. K. & Sung, Y. K. Epidemiology of systemic lupus erythematosus in Korea. J. Rheum. Dis. 30, 211–219. https://doi.org/10.4078/jrd.2023.0037 (2023).
Bang, S. Y. & Shim, S. C. Early human migration determines the risk of being attacked by wolves: Ethnic gene diversity on the development of systemic lupus erythematosus. J. Rheum. Dis. 31, 200–211. https://doi.org/10.4078/jrd.2024.0051 (2024).
Jung, J. I. et al. Successful treatment of hemophagocytic lymphohistiocytosis in a patient with systemic lupus erythematosus with ruxolitinib: A case report. J. Rheum. Dis. 31, 125–129. https://doi.org/10.4078/jrd.2023.0027 (2024).
Yu, J. Y. et al. Macrophage activation syndrome in neonatal lupus presenting with fever and rash. J. Rheum. Dis. 31, 49–53. https://doi.org/10.4078/jrd.2023.0039 (2024).
Boraschi, D. et al. IL-37: A new anti-inflammatory cytokine of the IL-1 family. Eur. Cytokine Netw. 22, 127–147 (2011).
Ren, C. et al. IL-37 alleviates TNF-α-induced pyroptosis of rheumatoid arthritis fibroblast-like synoviocytes by inhibiting the NF-κB/GSDMD signaling pathway. Immunobiology 228, 152382 (2023).
Gaber, W. et al. Genetic variations of Interleukin 32 (rs28372698) and Interleukin 37 (rs3811047), and their serum levels in systemic lupus erythematosus patients. Egypt. Rheumatol. 46, 207–212 (2024).
Nijeeb, R. A., Aljber, A. A. & Ad’hiah, A. H. Exon 2 variants (rs3811046 and rs3811047) of the IL37 gene are associated with susceptibility to systemic lupus erythematosus. Egypt. J. Basic. Appl. Sci. 11, 269–280 (2024).
Wu, Q. et al. Association between IL-37 and systemic lupus erythematosus risk. Immunol. Investig. 51, 727–738 (2022).
Zhan, Y. et al. Interleukin (IL)-1 family cytokines could differentiate primary immune thrombocytopenia from systemic lupus erythematosus-associated thrombocytopenia. Ann. Transl. Med. 9 (2021).
Yuan, Z. C. et al. Elevated expression of interleukin-37 in patients with rheumatoid arthritis. Int. J. Rheum. Dis. 22, 1123–1129. https://doi.org/10.1111/1756-185X.13539 (2019).
Ghobrial, E. E., Marzouk, H. M., Khorshied, M. M. & Sayed, M. G. Level of Interleukin 37 (IL-37) in children with systemic lupus erythematosus and its correlation with disease activity. Iran. J. Pediatrics 28 (2018).
Tawfik, M. G., Nasef, S. I., Omar, H. H. & Ghaly, M. S. Serum Interleukin-37: A new player in lupus nephritis? Int. J. Rheum. Dis. 20, 996–1001. https://doi.org/10.1111/1756-185X.13122 (2017).
Godsell, J. et al. Clinical associations of IL-10 and IL-37 in systemic lupus erythematosus. Sci. Rep. 6, 34604. https://doi.org/10.1038/srep34604 (2016).
Wu, G. C. et al. Elevated plasma interleukin-37 levels in systemic lupus erythematosus patients. Lupus 25, 1377–1380. https://doi.org/10.1177/0961203316646462 (2016).
Ye, L. et al. IL-37 inhibits the production of inflammatory cytokines in peripheral blood mononuclear cells of patients with systemic lupus erythematosus: Its correlation with disease activity. J. Transl. Med. 12, 69. https://doi.org/10.1186/1479-5876-12-69 (2014).
Song, L. et al. Glucocorticoid regulates interleukin-37 in systemic lupus erythematosus. J. Clin. Immunol. 33, 111–117. https://doi.org/10.1007/s10875-012-9791-z (2013).
Nasef, S. I. et al. Double risk of interleukin-37 rs3811047 A allele polymorphism with lupus nephritis in an Egyptian population. Egypt. Rheumatol. 45, 303–308 (2023).
Lee, Y. H. & Song, G. G. Circulating leptin and its correlation with rheumatoid arthritis activity: A meta-analysis. J. Rheum. Dis. 30, 116–125. https://doi.org/10.4078/jrd.2023.0005 (2023).
Lee, Y. H. & Song, G. G. Associations between Circulating interleukin-18 levels and adult-onset still’s disease: A meta-analysis. J. Rheum. Dis. 32, 48–56. https://doi.org/10.4078/jrd.2024.0095 (2025).
Hozo, S. P., Djulbegovic, B. & Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 5, 13 (2005).
Ridout, K. K., Ridout, S. J., Price, L. H., Sen, S. & Tyrka, A. R. Depression and telomere length: A meta-analysis. J. Affect. Disord. 191, 237–247 (2016).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6, e1000097. https://doi.org/10.1371/journal.pmed.1000097 (2009).
Egger, M., Smith, G. D. & Phillips, A. N. Meta-analysis: Principles and procedures. Bmj 315, 1533–1537 (1997).
Lee, Y. H. An overview of meta-analysis for clinicians. Kor. J. Intern. Med. 33, 277 (2017).
Lee, Y. H. Meta-analysis of genetic association studies. Ann. Lab. Med. 35, 283 (2015).
Wells, G. et al. (2000).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 (1997).
Lee, Y. H. & Song, G. G. Circulating interleukin-37 levels in rheumatoid arthritis and systemic lupus erythematosus and their correlations with disease activity: A meta-analysis. J. Rheum. Dis. 27, 152–158 (2020).
Lin, X. Y. et al. Association between Interleukin 37 (rs3811047) polymorphism and multiple autoimmune diseases in a Chinese population: A PRISMA-compliant meta-analysis. Medicine 97, e0386 (2018).
Funding
This research did not receive any specific funding.
Author information
Authors and Affiliations
Contributions
Young Ho Lee contributed to the study’s conception and design, data acquisition, data analysis and interpretation, manuscript drafting, and critical revision for intellectual content. Gwan Gyu Song contributed to the study’s conception and design, data acquisition, data analysis and interpretation, and critical revision of the manuscript for significant intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
This study does not require an ethics statement as it relies solely on previously published literature.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, Y.H., Song, G.G. Association of IL-37 levels and genetic variants with systemic lupus erythematosus: a meta-analysis. Sci Rep 15, 24000 (2025). https://doi.org/10.1038/s41598-025-08818-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08818-1