Abstract
Cervical cancer is a major public health issue in China, characterized by rising incidence and mortality rates over the past years. This study aims to analyze the epidemiological trends of cervical cancer from 2005 to 2018, providing valuable insights for public health policy and intervention strategies. Data were extracted from the publicly available China Cancer Registry Annual Reports (2005–2018), employing joinpoint log-linear regression models to evaluate changes in incidence and mortality rates. The analysis focused on geographic disparities between urban and rural areas, examining how these differences influence overall trends. Incidence and mortality rates were age-standardized using the the Segi’s world population and the fifth Chinese national census of 2000 as references. The incidence of cervical cancer in China increased significantly, rising from 9.10 per 100,000 women in 2005 to 18.10 per 100,000 in 2018, with an average annual percent change (AAPC) of 5.38%. Notably, rural areas exhibited a higher AAPC of 6.28%, compared to 4.54% in urban settings, highlighting the disparities in healthcare access. In 2018, there were 46,626 new cases of cervical cancer in Chinese cancer registry areas, representing 6.63% of all newly diagnosed cancers among women, with 14,737 deaths, making it the seventh leading cause of cancer deaths among females. The age-standardized incidence rate by Segi’s world standard population was 12.00 per 100,000, while the age-standardized mortality rate was 3.49 per 100,000. The incidence was low until age 20, then increased sharply, peaking at 50–54 years, while mortality remained low until age 25 and rose steadily, peaking in the 80–84 age group. Geographic disparities were significant, with the highest incidence and mortality rates found in central and rural regions. The accelerating burden-particularly in rural and Central China-underscores the need to expand organised screening, improve HPV-vaccination uptake, and narrow urban-rural health disparities. Targeted efforts for middle-aged and underserved populations are essential to advance China toward WHO cervical‑cancer‑elimination goals.
Similar content being viewed by others
Introduction
Cervical cancer remains one of the most prevalent malignant tumors affecting women worldwide and represents a significant public health challenge on a global scale. According to the GLOBOCAN 2020 estimates, the age-standardized incidence rate of cervical cancer is 13.3 per 100,000 women, resulting in approximately 600,000 new cases each year. Furthermore, the age-standardized mortality rate is reported at 7.3 per 100,000, translating to around 340,000 deaths annually, which positions cervical cancer as the fourth most lethal cancer among women, following breast, lung, and colorectal cancers1. Notably, the incidence of cervical cancer has exhibited a concerning upward trend in recent years, particularly in developing countries where access to preventive measures remains limited2. This increase is often attributed to various factors, including the prevalence of high-risk human papillomavirus (HPV) infections, lack of awareness about preventive strategies, and inadequate healthcare infrastructure3. In China, the National Cancer Center reported that the incidence of cervical cancer reached 17.69 per 100,000 in 2016, making it the sixth most common cancer among women in the country4.
To gain a comprehensive understanding of the epidemiological characteristics and disease burden associated with cervical cancer in China over recent years, this study analyzes cervical cancer data collected from 2005 to 2018. Given the substantial increase in cervical cancer cases and related deaths, particularly in rural areas where healthcare resources are scarce, it is imperative to optimize prevention strategies5. This includes enhancing public awareness campaigns about cervical cancer and the importance of regular screenings, as well as ensuring that HPV vaccinations are accessible and affordable6.
Data and methods
Source of information
The data utilized in this study were extracted from the China Cancer Registry Annual Reports spanning the years 2005 to 2018, as published by the National Cancer Center. This extensive dataset includes crucial information on both the incidence and mortality rates associated with various cancers, including cervical cancer. The reports provide a comprehensive overview of cancer statistics across different regions in China, allowing for an in-depth analysis of trends and patterns in cancer occurrence and outcomes7. This study utilized data from the National Cancer Registry Annual Report, which consists of anonymous and aggregated information without any personal or identifiable data. The study did not involve direct participation of human subjects or animal experiments, and therefore, no additional ethical approval was required. All data handling procedures strictly adhered to relevant laws and regulations to ensure privacy and confidentiality. The design and implementation of this study followed ethical guidelines, including the Declaration of Helsinki.
Geographic definitions
The classification of urban and rural areas was based on the Administrative Division Codes of the People’s Republic of China (GB/T 2260 − 2007), where prefecture-level cities and above were categorized as urban areas, and counties and county-level cities as rural areas, while also taking into account regional economic conditions and lifestyle factors. The division of Eastern, Central, and Western regions followed the standards of the National Bureau of Statistics.
Quality evaluation
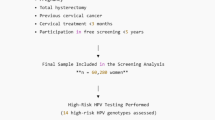
To ensure the reliability and completeness of the data, a rigorous quality evaluation was conducted in accordance with the China Cancer Registry Guidance Manual (2016)8. This evaluation process involved the use of several key quality indicators, which were referenced from Volume XI of Cancer Incidence in Five Continents, published by the International Agency for Research on Cancer (IARC) and the International Association of Cancer Registries (IACR)9,10. The indicators used included the percentage of morphological verification (MV%), the percentage of death certificate notification (DCO%), and the mortality/incidence ratios (M/I).
In particular, the tumor registration data for the year 2018 underwent stringent quality control measures, with a thorough consideration of regional coverage. The final annual report incorporated qualified data from a total of 700 registries, which collectively covered a population of 523,160,249 individuals (comprising 265,488,549 males and 257,671,700 females) in 2018. This figure represents 37.22% of the total Chinese population of 1,405,410,000 that year. Among these registries, 267 were located in urban areas, accounting for a population of 236,047,481 and representing 45.12% of the selected tumor registered areas. In contrast, 433 tumor registries were situated in rural areas, covering a population of 287,112,768, which accounts for 54.88% of the total population in these regions7. This comprehensive coverage enhances the robustness of the data, allowing for meaningful statistical analysis.
Statistical analysis
The analysis of incidence and mortality information for cervical cancer from 2005 to 2018 was derived from the Annual Report of Chinese Cancer Registration. Statistical analyses were performed using SPSS 25.0 (Windows version 25.0; SPSS Inc., IBM Corporation, USA), which facilitated data processing and calculation of incidence and mortality rates. For the purpose of this study, the incidence and mortality rates per 100,000 person-years were age-standardized using Chinese population in 2000 and Segi’s world standard population4.
To assess trends over time, the annual percentage change (APC) and the corresponding 95% confidence interval (CI) were calculated utilizing the Joinpoint regression model. By employing a joinpoint log-linear regression model, we aim to elucidate the trends in disease burden, which can significantly inform public health policies and resource allocation. This method allows for a nuanced examination of the changes in incidence and mortality rates over time, identifying critical turning points in the trends that may reflect the impact of public health interventions, such as HPV vaccination programs and screening initiatives. This statistical approach is particularly valuable for identifying significant changes in trends at specific points in time, providing insights into the dynamics of cervical cancer incidence and mortality. Furthermore, the continuous percentage change in annual rates was analyzed using a linear log model, which helps to capture the overall trend more effectively. Trend analyses were conducted using the Joinpoint software (Joinpoint Regression Program, Version 4.8.0.1, April 2020, Statistical Research and Applications Branch, National Cancer Institute)10.
Results
Epidemiological characteristics of cervical cancer in China in 2018
In 2018, cervical cancer ranked fifth among female cancers in China. The total number of new cases reported was 46,626, representing 6.63% of all newly diagnosed cancers in women. Of these, 20,109 cases were reported in urban areas, while 26,517 cases occurred in rural regions. The crude incidence rate was 18.10 per 100,000, with the age-standardized incidence rate by Chinese population in 2000 (ASIRC) at 12.95 per 100,000 and the age-standardized incidence rate by Segi’s world population (ASIRW) at 12.00 per 100,000. Notably, the incidence rate in rural areas was higher than in urban areas, with the ASIRC in rural regions being 1.14 times that of urban areas (Table 1).
In terms of mortality, cervical cancer ranked seventh among female cancer deaths in 2018. A total of 14,737 new deaths were recorded, accounting for 4.49% of all cancer deaths in women. Among these deaths, 6318 were reported in urban areas, while 8419 occurred in rural areas. The crude mortality rate for cervical cancer was 5.72 per 100,000, with the age-standardized mortality rate by Chinese population in 2000 (ASMRC) at 3.62 per 100,000 and the age-standardized mortality rate by Segi’s world population (ASMRW) at 3.49 per 100,000. Similar to incidence rates, mortality rates were higher in rural areas compared to urban areas, with the ASMRC in rural regions being 1.15 times that of urban regions (Table 1).
Overall, both the incidence and mortality rates of cervical cancer were higher in rural areas compared to urban settings. Geographically, the highest incidence and mortality rates were observed in the central region of China, followed by the western region, with the lowest rates found in the eastern region (Table 1).
The incidence of cervical cancer remained low prior to the age of 20, after which it increased rapidly, peaking in the 50 to 54 age group, before gradually declining. Conversely, the age-specific mortality rate remained low until age 25, after which it increased progressively, reaching its highest point in the 80–84 age group (Fig. 1).
Trends in cervical cancer incidence rates
The incidence rates of cervical cancer in Chinese cancer registration areas from 2005 to 2018 showed a consistent increase across all regions, as presented in Fig. 2 and Supplementary Tables S1. In the total female population, the crude incidence rate rose from 9.10 per 100,000 in 2005 to 18.10 per 100,000 in 2018, with an average annual percent change (AAPC) of 5.38% (95% CI: 4.69–6.08, P < 0.0001). Age-standardized incidence rates by the Chinese and World standard population also demonstrated significant increases, with AAPCs of 7.11% (95% CI: 5.20–9.06) and 4.81% (95% CI: 3.97–5.66), respectively (P < 0.0001). Urban areas showed a crude rate AAPC of 4.54% (95% CI: 3.75–5.33), while rural areas experienced a higher AAPC of 6.28% (95% CI: 4.64–7.95), reflecting a more rapid rise in rural incidence rates. Figure 2 illustrates this trend, with significant annual percent changes (APCs) in the general female population: 12.12% from 2005 to 2007, 4.52% from 2007 to 2012, and 2.73% from 2012 to 2018. The figure highlights a deceleration in incidence rate increases over time, with similar trends observed across urban and rural settings.
Trends in cervical cancer mortality rates
Cervical cancer mortality rates also increased significantly from 2005 to 2018 (Fig. 2 and Supplementary Tables S2). For the overall female population, the crude mortality rate rose from 2.41 per 100,000 in 2005 to 5.72 per 100,000 in 2018, with an AAPC of 7.27% (95% CI: 6.75–7.78, P < 0.0001). The ASMRC and ASMRW also displayed significant increases, with AAPCs of 9.00% (95% CI: 6.10-11.97) and 6.74% (95% CI: 6.10–7.38), respectively. In urban areas, the AAPC for the crude mortality rate was 7.30% (95% CI: 4.98–9.67), while the ASMRW had an AAPC of 7.99% (95% CI: 6.29–9.72). Rural areas exhibited a slower, but still significant increase, with a crude rate AAPC of 5.32% (95% CI: 2.17–8.58). Figure 2 highlights the regional variations in mortality trends. In the rural areas, the mortality rate initially increased sharply, with an APC of 11.64% from 2005 to 2007, followed by a more moderate increase of 5.78% from 2010 to 2018. Urban areas, in contrast, experienced an APC of 11.48% from 2005 to 2010, which slowed to 5.87% from 2010 to 2018.
Discussion
This study provides essential insights into the epidemiology of cervical cancer in China based on 2018 data and offers a detailed analysis of trends in incidence and mortality from 2005 to 2018. The results indicate that cervical cancer incidence in China has been increasing annually by approximately 5%, while mortality rates have grown at a rate of about 7% per year. This trend stands in contrast to the significant declines observed in many high-income countries, where organized screening programs, expanded HPV vaccination coverage, and improved healthcare infrastructure have contributed to lowering cervical cancer rates11.
Epidemiological evidence shows that the sustained global decline in cervical‑cancer incidence and mortality over recent decades is chiefly attributable to the widespread roll‑out of organised screening programmes, rather than to concurrent improvements in hygiene, socioeconomic status, or reductions in sexually transmitted infections12,13,14. However, the situation in China is quite different, as data reveal a continuous rise in both incidence and mortality, signaling the need for more effective public health strategies. Despite rising cervical cancer risk among younger women in Europe, Oceania, and North America, screening programs have accelerated in these regions, including Japan15,16,17. This trend may be linked to changes in sexual behavior and increased HPV transmission, which cytological screening inadequately addresses18,19. In the early 2000s, cervical cancer incidence decreased in the Caribbean and parts of Central and South America (e.g., Argentina, Chile, Costa Rica, Brazil, Colombia), but rates remain high20. Conversely, ineffective screening has contributed to increased premature cervical cancer mortality in Eastern Europe and Central Asia in recent generations21.
In 2018, the incidence of cervical cancer in China was 12.00 per 100,000, slightly lower than the estimated global incidence of 13.3 per 100,000 in 2020, but higher than in Eastern Asia (10.8 per 100,000) and North America (6.2 per 100,000)1. Therefore, it is crucial to note that the incidence of cervical cancer in China remains significantly above the WHO’s target for elimination (4.0 per 100,000)22. These rates emphasize the ongoing public health challenge that cervical cancer presents in China, and the urgent need to increase efforts to achieve the WHO’s goal of eliminating cervical cancer as a public health concern.
A key finding of this study is the significant disparity in cervical cancer incidence and mortality between urban and rural areas. This geographical disparity underscores the need for targeted public health interventions to address the higher burden of cervical cancer in rural and central areas of the country. Rural regions experience higher rates of both incidence and mortality, likely due to lower cancer screening rate, elevated HPV infection rates, limited access to medical resources, lower health awareness regarding early treatment, and a greater degree of population aging compared to urban areas23,24. These findings highlight the necessity for public health interventions focused on rural areas, where increased awareness, preventive screening, and early detection efforts could help mitigate this growing burden. The trends in mortality rates show an initial annual percentage change of 15.68% in rural areas from 2005 to 2007, moderating to 4.58% from 2010 to 2018, while urban areas experienced a decrease in APC from 8.24% in 2005–2010 to 1.62% from 2010 to 2018. These disparities underscore the importance of closing the urban-rural gap in healthcare access and resources for cervical cancer prevention and treatment.
Several contextual factors appear to underpin the marked urban-rural disparities. National survey data indicate that only about 29.5% of Chinese women aged 20–64 have ever participated in cervical‑cancer screening, with coverage dipping below 25% in many western rural counties yet exceeding 35% in eastern metropolitan areas25. The pooled prevalence of high‑risk HPV infection was roughly 16% among mainland Chinese women and there was a higher rate (nearly 20%) in under-developed northeastern areas26. Tobacco exposure further amplifies risk, and active smoking remains relatively uncommon among women ( 2.8% nationally and up to 3.1% in rural areas)27. Finally, substantial inequities in diagnostic quality and treatment capacity persist—tertiary oncology centres offering HPV testing equipment, colposcopy, pathology, and radiotherapy are concentrated in urban settings, whereas many rural facilities lack specialised personnel and equipment—contributing to later‑stage presentation and poorer outcomes28.
The age distribution of cervical cancer incidence and mortality reveals important trends. In 2018, cervical cancer incidence in China increased sharply with age, remaining low before 20 and rising rapidly starting at ages 20–24, peaking in the 50–54 age group before declining. This suggests that middle-aged and elderly women bear a significant burden, likely due to lower HPV vaccine coverage and limited screening. Although China started “two-cancer” screening program in 2009 by offering free cervical and breast cancer screening for women aged 35–64 in 200929, rising incidence rates among younger women indicate a need to lower the age threshold for screening. Factors such as early sexual initiation, abortions, and contraceptive use contribute to higher risk in young age group, highlighting the importance of expanding screening and prevention efforts30,31.
High-risk HPV is the leading cause of cervical cancer. While expanding HPV vaccination remains critical for achieving long‑term elimination goals, the current upward trend is more plausibly explained by sub‑optimal screening coverage, and persistent urban–rural disparities; the population‑level benefits of vaccination will manifest mainly in the coming decades. Although the introduction of HPV vaccination in China in 2016 marked a pivotal advancement32, uptake remains limited, particularly in rural areas where economic constraints and low awareness impede access. Given the significant population in these underserved regions, expanding vaccination coverage is essential to curbing the rising incidence of cervical cancer. Prioritizing young women in these areas and bolstering public health outreach could help China address regional disparities and reduce the disease burden significantly over the long term.
The WHO recommends HPV vaccination for girls aged 9–13 and regular screening for women aged 30–49, especially in resource-limited settings33. Combining HPV vaccination with effective screening practices offers a powerful approach to reducing cervical cancer rates, aligned with the WHO’s “90-70-90” targets to prevent millions of cases and deaths worldwide34. Lowering the age threshold for cervical cancer screening could bring further benefits in China, where incidence begins to rise markedly from age 35, as noted in this study. Integrating screening into premarital health exams could prevent invasive cancer by detecting and removing precancerous lesions, and alleviate the social and economic burdens on affected families.
This study has several limitations. First, the analysis relies on data from China’s cancer registration system, which may exhibit regional inconsistencies in reporting and completeness, particularly in underdeveloped areas. Second, the absence of detailed data on tumor stage, histological grade, and treatment modalities restricted our ability to conduct more in-depth analyses of outcomes. Future research should explicitly address these factors. Despite these limitations, this study provides valuable insights into cervical cancer and serves as a foundation for future investigations into this critical area.
Conclusion
This study sheds light on the current cervical cancer burden in China, highlighting the urgent need for enhanced public health efforts to curb rising incidence and mortality rates. Despite global progress in reducing cervical cancer cases, China continues to experience significant increases, especially in rural areas where healthcare access and preventive measures are less accessible. Findings indicate that expanded HPV vaccination, broader screening coverage, and improved public awareness are essential to address regional disparities and achieve the WHO’s elimination goals. Strengthening public health infrastructure, ensuring equitable healthcare access, and prioritizing cervical cancer prevention strategies across China will be crucial in reducing the disease burden and promoting the health and quality of life for women nationwide. The findings from this study will not only contribute to the existing body of knowledge regarding cervical cancer epidemiology in China but also provide valuable insights for healthcare policymakers aimed at reducing the burden of this disease. By highlighting the urgency of effective cervical cancer prevention and control measures, we hope to support efforts to improve women’s health and well-being across the nation.
Data availability
The dataset analyzed during the current study was available from the corresponding author on reasonable request or at https://www.pmphmall.com/gdsdetail/647514-325111.
Abbreviations
- HPV:
-
Human papillomavirus
- APC:
-
Annual percent change
- AAPC:
-
Average annual percent change
- IARC:
-
International Agency for Research on Cancer
- IACR:
-
International Association of Cancer Registries
- MV%:
-
Percentage of morphological verification
- DCO%:
-
The percentage of death certificate notification
- M/I:
-
Mortality/incidence ratios
- CI:
-
Confidence interval
- ASIRC:
-
Age-standardized incidence rate by Chinese population in 2000
- ASIRW:
-
Age-standardized incidence rate by Segi’s world population
- ASMRC:
-
Age-standardized mortality rate by Chinese population in 2000
- ASMRW:
-
Age-standardized mortality rate by Segi’s world population
References
Sung, H. et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021)
Zhang, X., Zeng, Q., Cai, W. & Ruan, W. Trends of cervical cancer at global, regional, and National level: Data from the global burden of disease study 2019. BMC Public. Health. 21(1), 894. https://doi.org/10.1186/s12889-021-10907-5 (2021)
Reza, S. et al. Public health concern-driven insights and response of low- and middle-income nations to the world health organization call for cervical cancer risk eradication. Gynecol. Oncol. Rep. 54, 101460 (2024)
Zheng, R. S. et al. Cancer incidence and mortality in China, 2016. J. Natl. Cancer Cent. 2(1), 1–9 (2022)
Zhang, M., Sit, J. W. H., Chan, D. N. S., Akingbade, O. & Chan, C. W. H. Educational interventions to promote cervical cancer screening among rural populations: A systematic review. Int. J. Environ. Res. Public. Health. 19(11), 6874 (2022)
Wirtz, C. et al. Integrating HPV vaccination programs with enhanced cervical cancer screening and treatment, a systematic review. Vaccine 40(Suppl 1), A116–A123 (2022)
National Cancer Center. China Cancer Registry Annual Report [in Chinese and English]. Beijing: People’s Health Press, 2023.6 (2021)
National Cancer Center. Chinese Guideline for Cancer Registration [in Chinese] (People’s Medical Publishing House Co., LTD, 2016)
Bray, F. & Parkin, D. M. Evaluation of data quality in the cancer registry: Principles and methods. Part I: Comparability, validity and timeliness. Eur. J. Cancer. 45, 747–755 (2009)
Kim, H. J. et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 19(3), 335–351 (2000)
Dillner, J. et al. Decline of HPV infections in Scandinavian cervical screening populations after introduction of HPV vaccination programs. Vaccine 36(26), 3820–3829 (2018)
Vaccarella, S. et al. Preventable fractions of cervical cancer via effective screening in six baltic, central, and Eastern European countries 2017-40: A population-based study. Lancet Oncol. 17(10), 1445–1452 (2016)
Arbyn, M. et al. Accuracy and effectiveness of HPV mRNA testing in cervical cancer screening: A systematic review and meta-analysis. Lancet Oncol. 23(7), 950–960 (2022)
Yao, H. et al. Epidemiological trends and attributable risk burden of cervical cancer: An observational study from 1990 to 2019. Int. J. Clin. Pract. 2022, 3356431 (2022)
Bray, F. et al. Incidence trends of adenocarcinoma of the cervix in 13 European countries. Cancer Epidemiol. Biomarkers Prev. 14(9), 2191–2199 (2005)
Bray, F. et al. Trends in cervical squamous cell carcinoma incidence in 13 European countries: Changing risk and the effects of screening. Cancer Epidemiol. Biomarkers Prev. 14(3), 677–686 (2005)
Utada, M. et al. Increasing risk of uterine cervical cancer among young Japanese women:comparison of incidence trends in Japan, South Korea and Japanese-Americans between 1985 and 2012. Int. J. Cancer. 144(9), 2144–2152 (2019)
Castanon, A. & Sasieni, P. Is the recent increase in cervical cancer in women aged 20–24 years in England a cause for concern? Prev. Med. 107, 21–28 (2018)
McDonald, S. A. et al. Disease burden of human papillomavirus infection in the Netherlands,1989–2014: The gap be-tween females and males is diminishing. Cancer Causes Control. 28(3), 203–214 (2017)
Pilleron, S. et al. Cervical cancer burden in Latin America and the caribbean: Where are we? Int. J. Cancer. 147(6), 1638–1648 (2020)
Bray, F. et al. Patterns and trends in human papillomavirus-related diseases in central and eastern Europe and central Asia. Vaccine 31(suppl 7), H32–H45 (2013)
Wang, L. Accelerating cervical cancer prevention and control in China to achieve cervical cancer elimination strategy objectives. China CDC Wkly. 4(48), 1067–1069 (2022)
Zhao, Y. Q. et al. Real-world research on cervical cancer screening program and effect evaluation for Chinese population [in chinese]. Zhonghua zhong liu za zhi. 40(10), 764–771 (2018)
Chan, C. K., Aimagambetova, G., Ukybassova, T., Kongrtay, K. & Azizan, A. Human papillomavirus infection and cervical cancer: Epidemiology, screening, and vaccination-review of current perspectives. J. Oncol. 2019, 3257939 (2019)
Zhang, M. et al. Cervical Cancer screening Coverage - China, 2018–2019. China CDC Wkly. 4(48), 1077–1082 (2022)
Zhu, B. et al. The prevalence, trends, and geographical distribution of human papillomavirus infection in China: The pooled analysis of 1.7 million women. Cancer Med. 8(11), 5373–5385 (2019)
Xia, X. et al. Prevalence of cigarette use and addiction among Chinese females by age and province: Findings from nationwide China health literacy survey during 2018–19. Drug Alcohol Depend. 258, 111258 (2024)
Li, Y. et al. A study on service capacity of primary medical and health institutions for cervical cancer screening in urban and rural areas in China. Chin. J. Cancer Res. 31(5), 838–848 (2019)
Di, J., Rutherford, S. & Chu, C. Review of the cervical cancer burden and population-based cervical cancer screening in China. Asian Pac. J. Cancer Prev. 16(17), 7401–7407 (2015)
Kastbom, Å. A., Sydsjö, G., Bladh, M., Priebe, G. & Svedin, C. G. Sexual debut before the age of 14 leads to poorer psychosocial health and risky behaviour in later life. Acta Paediatr. 104(1), 91–100 (2015)
Gadducci, A., Cosio, S. & Fruzzetti, F. Estro-progestin contraceptives and risk of cervical cancer: A debated issue. Anticancer Res. 40(11), 5995–6002 (2020)
Wong, L. P. et al. Current issues facing the introduction of human papillomavirus vaccine in China and future prospects. Hum. Vaccin Immunother. 15(7–8), 1533–1540 (2019)
World Health Organization. WHO guidelines for the use of thermal ablation for cervical pre-cancer lesions [EB/OL]. https://www.who.int/publications/i/item/9789241550598. (2019). [Last accessed on 2024 April 16]
World Health Organization (WHO). WHO Director-General calls for all countries to take action to help end the suffering caused by cervical cancer [EB/OL].WHO; https://www.who.int/news/item/18-05-2018-who-dg-calls-for-all-countries-to-take-action-to-help-end-the-suffering-caused-by-cervical-cancer. (2018). [Last accessed on 2024 April 16]
Funding
This study was supported by the Zhejiang Provincial Medical and Health Science and Technology Plan Project (Award Numbers: 2024KY826, 2021KY574), the Zhejiang Provincial Traditional Chinese Medicine Science and Technology Plan Project (Award Number: 2023ZL294), and the 2022 Digestive Tract Early Cancer Physician Growth Plan Research Project (Award Number: GTCZ-2022-ZJ-33-0001). These funding sources had no role in the design, conduct, or reporting of the study.
Author information
Authors and Affiliations
Contributions
R.L. conceptualized the idea of this study. R.L., P.L. Y.Z., and H.Z. participated in extraction and critical review of literature. R.L. was responsible for statistical analysis, data curation, and visualization of the study results. R.L. and P.L. wrote the first draft of this manuscript. All four authors have critically read the text and contributed with inputs and revisions, and all have also read and approved the final version of manuscript. R.L. supervised and administered the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent of participants
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, P., Zhu, Y., Zhou, H. et al. Trends and urban–rural disparities in cervical cancer epidemiology in China, 2005–2018. Sci Rep 15, 25021 (2025). https://doi.org/10.1038/s41598-025-09004-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09004-z