Abstract
Idiopathic granulomatous mastitis (IGM) is rare globally and infrequent in some middle-east regions. Sex-hormonal factors have been mentioned as predisposing factors for IGM, recent large-sale studies indicate a 7.5-fold increased risk in women who have breastfed. This study investigates BF-related factors that contribute to IGM development. We conducted a multicenter case–control study and recorder BF-related events in 730 IGM patients and healthy 760 controls. The mean age of participants was 36.63 ± 6.49 in the Case and 36.96 ± 6.11 years in the Control Group (p = 0.31). IGM occurred more frequently in the contralateral breast in one-sided BF (p < 0.001), with discordance between the affected side and BF side in 68.3% of cases (p = 0.005). Multivariate analysis revealed significant associations between IGM and one-sided BF (OR = 4.21), post-weaning breast engorgement (OR = 3.06), lactational mastitis (OR = 1.93), and oral medication use for infants (OR = 2.59). The study achieved 100% statistical power for both primary and secondary objectives, with narrow confidence intervals indicating high precision. This study provides robust evidence supporting the milk stasis hypothesis, demonstrating that BF-related issues leading to milk stasis are strongly associated with IGM development. Preventive strategies to minimize milk stasis and encourage bilateral BF may help reduce IGM risk.
Similar content being viewed by others
Introduction
Idiopathic granulomatous mastitis (IGM) is a chronic benign breast disease associated with significant morbidity1. While rare globally, it is more prevalent in certain regions, including Turkey, Iran, China, India, and among the Hispanic population in the United States2. The exact incidence of IGM remains unknown; Zhou et al.3 report an incidence of 6 per 100,000 in the Hispanic, and one per 100,000 in the non-Hispanic population in the USA. Reports suggest a gradual increase in areas where it is more common3,4.
The etiology of IGM is unclear. Proposed risk factors include prior pregnancies, lactation, use of oral contraceptive pills (OCPs), and autoimmune mechanisms5. A recent large-scale case–control study in Iran involving over 1000 participants reported a 7.5-fold increased risk of IGM among women who had breastfed6. Similarly, a case–control study in China highlighted breastfeeding (BF) as a major risk factor, with nipple inversion and discharge significantly more frequent in IGM patients1. Evidence also suggests IGM predominantly occurs within the first five years postpartum or following lactation7,8.
The milk stasis hypothesis, first proposed by Omranipour et al. in 20139, posits that milk retention increases ductal permeability, leading to milk leakage into the breast parenchyma. This presumably triggers an inflammatory response, with T-cell and macrophage migration, ultimately resulting in non-caseous granuloma formation10. Supporting this hypothesis, retrospective studies have reported higher rates of breast infections among IGM patients11. Other studies have suggested that IGM is more frequent in the contralateral breast of women who primarily breastfed from one side12,13,14,15,16. However, these studies were limited by very small sample sizes or the absence of control groups.
While BF is highly beneficial for both mother and child, irregularities associated with BF, rather than BF itself, may underlie the pathogenesis of IGM. This study was designed to explore BF-related factors associated with IGM. Specifically, we investigated the relationship between one-sided BF and IGM and examined lactation-related events as potential triggers for the disease.
Results
Participants and descriptive data
A total of 1490 women were included in the study, comprising 730 women with histologically confirmed IGM (Case Group), and 760 healthy women (Control Group). The mean age was similar between the groups, with the Case Group averaging 36.63 years (± 6.49) and the Control Group averaging 36.96 years (± 6.11), a difference that was not statistically significant (p = 0.31). IGM occurred in the left breast in 371 patients (50.8%), in the right breast in 276 women (37.8%), and bilaterally in 80 patients (11%); three were missing (uncertainty about the laterality due to unprecise intermittent use of the right and left forms by the physician). The reproductive characteristics of all participants are summarized in Table 1.
Outcome data and main results
The first stage of the study analysed data from the IGM group exclusively. Figure 1 presents the association between IGM laterality and one-sided BF; it shows that IGM was significantly less frequent in the dominant lactating breast (p < 0.001). After excluding patients with bilateral disease (n = 80) and those who had breastfed equally from both breasts (n = 279), it was observed that the side of the disease was discordant with the dominant BF side in 68.3% (254/372) of cases, while concordance was observed in 31.7% of cases.
Table 2 further breaks down this data for preferred one-sided BF (those who had breastfed more frequently from one breast), versus exclusive one-sided BF (those who had breastfed from only one side). The analysis reveals that IGM was significantly more common in the contralateral breast among women who exclusively breastfed from either the right or left side compared to those who used both breasts but showed a preference for one side.
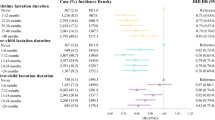
Table 3 presents the findings from the second phase of the study, comparing BF-related habits and events between the two groups. One-sided BF was significantly more frequent among IGM patients (p < 0.001). Additionally, lactational mastitis, severe breast engorgement, infant oral infections, use of topical nipple medications, and use of oral drops by infants were all significantly more common in the IGM group (p < 0.001). Furthermore, after weaning, IGM patients experienced breast engorgement at a much higher rate, and a larger proportion continued milk production for three months or longer (p < 0.001).
Multivariate logistic regression analysis showed that one-sided BF, breast engorgement after weaning, lactational mastitis, and using oral drops for the baby are significantly associated with future development of IGM (Table 4). However, BF duration was excluded as a risk factor.
We further examined the reasons for reduced or absent BF from one side in the IGM group. Among women with one-sided BF (n = 183), the most common cause was nipple problems, such as nipple inversion or flat nipple, reported by 59 participants (32.2%). Less frequent causes included maternal preference or comfort, child preference, or breast pain.
Discussion
This multicentre study evaluated whether BF-related milk stasis and associated issues could act as initiators of IGM. Our findings provide robust evidence supporting the milk stasis hypothesis and suggest preventive measures to mitigate IGM risk.
The first phase of the study focused on the laterality of IGM in relation to the dominant side of BF. Consistent with previous studies1,9,11,17,18,19, IGM was more common on the left side. Not many studies in the existing literature report on the side of IGM and BF. One study mentions a higher rate of one-sided BF in IGM (relative to other benign breast diseases)20, and others report a more frequent occurrence of IGM in the breast not used for BF12,13,14,15. However, these studies are limited by very small sample sizes, lack of control groups, or inconclusive statistical results. A more recent study by Cetin16 evaluated 220 IGM patients and found out that around 44% had not breastfed from the affected side.
Our study, the largest to date, demonstrated that one-sided BF was four times more frequent in IGM cases. Importantly, there was nearly 70% discordance between the side of BF and the side of IGM, with this pattern worsening when one breast was not used for nursing.
While strongly supporting the milk stasis hypothesis, we also found that 30% of IGM cases occurred in the breast used for BF, and many patients had breastfed bilaterally; necessitating further investigation of other contributing factors. Therefore, in the second phase, we explored additional indicators of milk stasis and its consequences.
Studies evaluating these factors are scarce in the present literature. In their retrospective study on 720 IGM patients, Uysal et al.11 found a 30% rate of previous breast infections. Raam et al.15 found a higher but non-significant frequency of breast pump use, nipple cracks, and breast infection in 30 IGM patients. They also found a significant lower rate of hand-washing, and a non-significant lower rate of nipple cleaning before BF in IGM patients. Their overall impression was that events related to BF were probably related to IGM. Zeng et al.1 compared more than 1634 IGM cases with 186 healthy controls and found that nipple discharge, nipple inversion, and serum prolactin levels were significantly higher in the IGM group. They concluded that there is a close association between BF-related issues and IGM. It is interesting that our study also showed a very high rate of nipple flatness or inversion in IGM patients, which was the main cause for one-sided BF. This strongly highlights the effect of milk stagnation on the development of IGM.
Cetin16 found that half of their 220 patients had experienced BF-related problems, and mastitis with or without abscess formation had occurred in 17% of their cohort. In our study, post- weaning breast engorgement happened three times more commonly in IGM patients than healthy women. As cessation of breastfeeding is done suddenly in Middle Eastern countries like Turkey and Iran21,22, areas with the highest rates of IGM2; this factor probably contributes to the higher incidence of IGM. After weaning, milk expression persists in some women. This had occurred around 1.5 times more commonly in patients with IGM than in healthy women in this study. On the other hand, the oral use of medications by the infants during the BF period was more than 2.5 times more frequent in IGM, while the multivariate analysis did not confirm a higher rate of oral infection in the child. This raises the question of whether the medications are transferred into milk ducts at the time of sucking, and exacerbate inflammatory processes in the presence of stasis.
Lactational mastitis, which was twice more common in IGM cases, may act as a trigger for milk stasis-related inflammation. However, Staphylococcus species are typically associated with lactational mastitis23, while microbial agents such as Corynebacterium have been implicated in IGM7. Whether these infections and microbial factors contribute to IGM development warrants further research.
The strengths of this study are the very high statistical power, the large sample size, the prospective setting and the case–control design. Based on this study, it can be said with great consistency that milk stasis is the initiating phase in the pathophysiology of IGM. Therefore, several preventive measures can be proposed to women in populations where the disease is more common or increasing. Adherence to bilateral BF, an early approach to milk stasis, milk evacuation after nursing, early management of lactational mastitis, and following a smooth process at the time of weaning could help decrease the risk of IGM. From the perspective of the mother’s breast health, a suitable weaning would be done gradually to allow for adjustments in milk production, reducing the risk of engorgement24.
Our study had some limitations. We did not measure serum prolactin levels, nor could we assess differences in milk composition or microbiome between breasts. Additionally, recall bias may have influenced participants’ accounts of BF-related events.
Our findings strongly support the milk stasis hypothesis as a primary pathophysiological mechanism in IGM. Preventive strategies to reduce milk stasis such as bilateral BF, early management of mastitis, addressing nipple issues, and gradual weaning may decrease the risk of IGM. Future studies should further investigate the microbial and immunological mechanisms underlying this condition.
Methods
Study design and settings
This multicenter, survey-based, case–control study was conducted between December 2021 and November 2024 in 14 centers in Iran. The study was approved by the Ethics Committee of the Deputy of Research of Tehran University of Medical Sciences, Tehran, Iran (Ethics Approval Code: IR.TUMS.IKHC.REC.1402.200), and was carried out according to the Helsinki Declaration of Ethical Principles. All participants signed an informed consent.
Participants
The study population consisted of women attending outpatient private or public breast clinics in 6 provinces of Iran; the case group had attended Breast Clinics and Offices, and the control group were women who had visited clinics other than the Breast, Gynecology, or Endocrinology Clinics in University Hospitals in the same cities.
The inclusion criteria for the case group were histologically proven IGM, a positive history of pregnancy, age 18 or above, and willing to participate. The same criteria applied to the control group, except that they had no history of IGM and other breast disease. Participants unable to provide complete reproductive or BF history were excluded.
Variables and measurement
Collected variables included:
-
Demographics and reproductive factors: Age, gravidity, age at first birth, infertility history, BF duration, and BF side.
-
BF-related events: Nipple issues (cracking or ulceration, inversion), breast engorgement, mastitis, and milk retention during and post-BF.
-
Other BF-related factors: Maternal medication use during BF, infant oral infections, infant medication use, and hygienic practices (handwashing, nipple washing).
Data was collected via structured interviews conducted by trained staff. BF duration was calculated as the sum of all periods of lactation. For the side of BF, we proposed five possible categories (Both breasts equally, mostly right breast, mostly left breast, right breast only, left breast only, no breastfeeding), and patients clarified their relevant category according to their overall history of BF. To evaluate the association between the side of BF and the occurrence of IGM, we grouped the categories as dominant right breast (mostly right breast and right breast only) and dominant left breast (mostly left breast and left breast only), and evaluated the laterality of IGM in relation to these groups. We then compared those who had breastfed exclusively from the left or right side with those who had preferably breastfed from one side. We also compared the rates and causes of one-sided BF between the case and control groups.
Breast engorgement and milk accumulation were considered both during BF and after cessation of BF. We considered lactational mastitis and local or one-sided engorgement as one variable, because the discrimination was difficult based on history; but we only included bouts of engorgement that had received medical attention and treatment.
Mothers were enquired about their reasons for lactating from one breast by an open-ended question, and similar answers were grouped together. Ultimately, “the reason for one-sided BF” yielded a binary variable categorized as “nipple problems” and “other causes”.
Study power
The primary objective was to assess the relationship between one-sided BF and IGM, observed in 54% of cases and 20% of controls (Table 3), yielding a statistical power of 100%. The calculated power for other BF-related outcomes (breast engorgement after weaning, post-weaning persistence of breast milk production, lactational mastitis) was approximately 100%. Furthermore, the narrow confidence intervals (CIs) achieved in our results indicated a high level of statistical precision for the study. Thus, the sample size used in this study was sufficiently large to provide a reliable point estimate with a narrow CI, effectively addressing our research questions.
Statistical methods
The statistical analysis was conducted using SPSS (Version 18, SPSS Inc., IL, USA). Differences in means between the case and control groups were assessed using the Student’s t-test. Categorical variable differences were evaluated with the Chi-square test . A two-sided p-value of less than 0.05 was considered statistically significant. Multivariate binary logistic regression was employed to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for associations between BF-related events and IGM. Variables with a p-value < 0.05 in univariate analysis, including BF duration, BF side, lactational mastitis, post-weaning breast engorgement or milk production, infant oral infections, and use of maternal or infant medications during BF; were included in the multivariate model.
Data availability
Data is available on reasonable request from the first author (sadafalipour@yahoo.com).
References
Zeng, Y. et al. Risk factors for granulomatous mastitis and establishment and validation of a clinical prediction model (Nomogram). Risk Manag. Healthc. Policy 16, 2209–2222 (2023).
Metanat, S. et al. Global distribution of idiopathic granulomatous mastitis: A scoping review: IGM global distribution. Arch. Breast Cancer 9, 261–271 (2022).
Zou, J., Nelson, N., Botnar, K., Khanipov, K. & Klimberg, V. S. Clinical trends in granulomatous mastitis incidence, prevalence, and treatment: A retrospective study highlighting ethnic differences in care. J. Surg. Res. 302, 732–738 (2024).
Koksal, H. What are the new findings with regard to the mysterious disease idiopathic granulomatous mastitis?. Surg. Today 51, 1158–1168 (2021).
Alipour, S. et al. Idiopathic granulomatous mastitis and history of hypothyroidism: Intervening data of a prospective multicenter trial and meta-analysis of the existing literature: IGM and hypothyroidism. Arch. Breast Cancer 10, 38–47 (2023).
Alipour, S. et al. Predisposing factors for idiopathic granulomatous mastitis: A large prospective multicentric study. Iran J. Public Health. 54, 645 (2025).
Dilaveri, C. et al. Idiopathic granulomatous mastitis. Breast J. 2024, 6693720 (2024).
Krawczyk, N. et al. Idiopathic granulomatous mastitis as a benign condition mimicking inflammatory breast cancer: Current status, knowledge gaps and rationale for the GRAMAREG study (EUBREAST-15). Cancers 16, 3387 (2024).
Omranipour, R., Mohammadi, S. F. & Samimi, P. Idiopathic granulomatous lobular mastitis-report of 43 cases from Iran; introducing a preliminary clinical practice guideline. Breast Care. 8, 439–443 (2013).
Yuan, Q. Q. et al. Management of granulomatous lobular mastitis: An international multidisciplinary consensus (2021 edition). Mil. Med. Res. 9, 20 (2022).
Uysal, E., Soran, A., Sezgin, E., Granulomatous Mastitis Study Group. Factors related to recurrence of idiopathic granulomatous mastitis: What do we learn from a multicentre study?. ANZ J. Surg. 88, 635–639 (2018).
Baslaim, M. M., Khayat, H. A. & Al-Amoudi, S. A. Idiopathic granulomatous mastitis: A heterogeneous disease with variable clinical presentation. World J. Surg. 31, 1677–1681 (2007).
Altintoprak, F. et al. Idiopathic granulomatous mastitis: An autoimmune disease?. Sci. World J. 2013, 148727 (2013).
Elzahaby, I. A. et al. Etiologic revelation and outcome of the surgical management of idiopathic granulomatous mastitis; An Egyptian centre experience. Breast Dis. 36, 115–122 (2016).
Raam, M. Etiological evaluation of idiopathic granulomatous mastitis by a prospective case control study: Doctoral dissertation, Christian Medical College, Vellore. (2018).
Çetin, K. Breastfeeding and secretory factors in idiopathic granulomatous mastitis: Unveiling etiological insights. World J. Surg. 20, 12426 (2024).
Azizi, A. et al. Idiopathic granulomatous mastitis: Management and predictors of recurrence in 474 patients. Breast J. 26, 1358–1362 (2020).
Kiyak, G. et al. Management of idiopathic granulomatous mastitis: Dilemmas in diagnosis and treatment. BMC Surg. 14, 1–5 (2014).
Kaviani, A. et al. Idiopathic granulomatous mastitis: Looking for the most effective therapy with the least side effects according to the severity of the disease in 374 patients in Iran. Breast J. 25, 672–677 (2019).
Oltean, H. N. et al. Risk factors for chronic mastitis in Morocco and Egypt. Int. J. Inflamm. 2013, 184921 (2013).
Zare, P., Mirahmadizadeh, A. R., Sayadi, M., Moradi, F. & Mohammadi, S. Pattern of complete weaning and its related factors in Fars Province. Pars. J. Med. Sci. 11, 31–37 (2022).
Oflu, A. Weaning practices of Turkish mothers: A mixed-model research. Breastfeed. Med. 15, 109–113 (2020).
Barbosa-Cesnik, C., Schwartz, K. & Foxman, B. Lactation mastitis. JAMA 289, 1609–1612 (2003).
Grueger, B. Canadian Paediatric Society, community paediatrics. Weaning from the breast. J. Paediatr. Child Health 18, 210–211 (2013).
Acknowledgements
We would like to acknowledge the Cancer Institute and the Deputy of Research of Tehran University of Medical Sciences, Tehran, Iran. We also acknowledge Drs. Shahla Astaraki, Najmeh Ahmadi, Reyhaneh Aghajani, Narges Dehghani, Najmeh Dabbagh, Asieh Fattahi, Maryam GhariniAhmadi, Mohammadreza Hakimian, Maria Hashemian, Sima Molavi, Roghayeh Jalili, Asieh Olfatbakhsh, Azam Salati, Seyed-Mohammadreza Javadi, Zohreh Zahernia-Shahrbabaki, Fataneh Ziaee for sharing knowledge and data; and Matina Noori, Marzieh Orouji, Behnaz Khajeh-Ali-Beiki, and Shiller Hessamiazar for their assistance in data collection.
Funding
This research was funded by a grant from the Cancer Institute, Tehran University of Medical Sciences, Tehran, Iran; Grant Number: 1402-2-417-67494.
Author information
Authors and Affiliations
Contributions
SA and BE: Study conception and design. SA, MT, PA, PB, MF, NN, FM, AS, AM, MD, RO, RH and PF: Study conception and Data collection. AO: Data managing and cleaning. BE: data analysis. SA and BE: writing the original draft. All authors: reviewing and editing the manuscript. All authors read and approved the final version of manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Ethics Committee of the Deputy of Research of Tehran University of Medical Sciences, Tehran, Iran (Ethics Approval Code: IR.TUMS.IKHC.REC.1402.200), and was carried out according to the Helsinki Declaration of Ethical Principles. All participants signed an informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alipour, S., Tabatabaian, M., Aziminezhadan, P. et al. From hypothesis to robust evidence in a nationwide multicenter case–control study on 1490 women: milk stasis and idiopathic granulomatous mastitis. Sci Rep 15, 37576 (2025). https://doi.org/10.1038/s41598-025-10784-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-10784-7