Abstract
This multicenter prospective study investigated factors influencing mid-term health-related quality of life (HRQoL) among intensive care unit (ICU) survivors in Korea. Among 2,002 patients, 189 who completed follow-up assessments at 90 days post-discharge were included in the final analysis. HRQoL was measured using the five-level EuroQoL 5-Dimension (EQ-5D-5L) and Hospital Anxiety and Depression Scale (HADS) at 30 and 90 days after discharge. Multivariable regression identified older age, infection as the cause of ICU admission, higher clinical frailty scale (CFS), and baseline HADS scores as independent predictors of lower EQ-5D-5L scores at 90 days. Initial HADS and CFS were also significantly associated with persistent anxiety and depression symptoms. Specific domains of HRQoL, such as mobility, self-care, and usual activity, were particularly affected by these factors. The findings underscore the importance of early psychological and frailty assessments in ICU patients, as these measures can help identify individuals at risk for poor recovery trajectories. Routine evaluation and targeted interventions for patients with high anxiety, depression, or frailty at ICU admission may improve long-term outcomes and overall quality of life after critical illness.
Similar content being viewed by others
Introduction
Survivors of intensive care units (ICUs) frequently encounter enduring physical, psychological, and social challenges that markedly impair their health-related quality of life (HRQoL). Recent evidence indicates that, although the survival rates from severe illnesses have improved, the quality of life for these survivors often remains significantly compromised following discharge1,2,3,4. Accordingly, HRQoL has emerged as a pivotal outcome measure for ICU survivors, transcending mere survival to encompass recovery, societal reintegration, and overall well-being.
The demographic and clinical profiles of ICU survivors are heterogeneous, encompassing a range of pre-existing health conditions and severity of the illnesses necessitating ICU admission. These individuals commonly face a complex interplay of ongoing physical disabilities, cognitive impairments, and emotional disturbances, a condition collectively recognized as post-intensive care syndrome (PICS)5. Factors that influence HRQoL among ICU survivors are manifold, including the presence of preexisting comorbidities, such as cardiovascular, hepatic, and respiratory diseases, severity of the initial illness, nature of medical interventions received during ICU stay, psychological factors, and a spectrum of social determinants, such as socioeconomic status3,6,7,8.
Despite advances in empirical research, discerning the myriad factors that influence HRQoL continues to present significant challenges, largely due to variability among patient populations and therapeutic approaches. Therefore, a multicenter observational study that systematically and thoroughly assesses these factors across diverse settings is necessary. To address this gap, we have undertaken a multicenter prospective analysis aimed at elucidating the factors that affect HRQoL in ICU survivors.
Results
Baseline characteristics
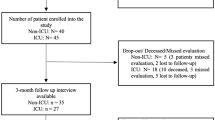
A total of 2002 patients were screened during the study period. Of these, 1,763 were excluded (refusal to provide consent, n = 1,525; inability to communicate because of neurological status, n = 238). A total of 239 patients were included in this study, of whom 189 completed the EQ-5D-5L assessment on day 90 and were included in the final analysis (Fig. 1).
Baseline characteristics of the patients are shown in Table 1. The median age of the patients was 63.0 years (IQR, 53.0–71.0), 59.3% were male, 67 (35.4%) were retired, 63 (33.3%) were employed, and 134 (70.9%) had completed higher education. Most patients were admitted to the medical ICU (91.5%). The median length of stay in the ICU was 7 (4.0–12.0) days. The mean initial SAPS III score was 60.9 ± 16.0, while the median sequential organ failure assessment (SOFA) score on day 1 was 6.0 (IQR, 3.0–9.0). Median scores for the CFS and CCI were 5.0 (IQR, 3.0–7.0) and 4.0 (IQR, 2.0–6.0), respectively. The median HADS score on day 1 was 13.0 (IQR, 7.0–18.0).
Factors associated with EQ-5D-5L scores at 90 days post-discharge
At 90 days post-discharge, several factors were significantly associated with decreased HRQoL among ICU survivors, as measured by the EQ-5D-5L questionnaire (Table 2). Older age was significantly associated with increased problems with mobility (P = 0.002), self-care (P < 0.001), and usual activities (P = 0.005). Lower BMI was correlated with more severe issues in mobility (P = 0.005), self-care (P = 0.010), usual activities (P = 0.003), and anxiety/depression (P = 0.002). Longer ICU length of stay was associated with more severe problems in mobility (P < 0.001), self-care (P < 0.001), usual activities (P = 0.002), and pain/discomfort (P = 0.013). Higher severity of illness scores, such as SAPS III, were associated with poorer outcomes in mobility (P = 0.002), self-care (P = 0.001), and usual activities (P = 0.001). Similarly, frailty, as measured by the CFS, was significantly associated with mobility (P = 0.001), self-care (P < 0.001), usual activities (P < 0.001), and anxiety/depression (P = 0.049). Opioid use in the ICU was significantly associated with increased problems in mobility (P = 0.006) and self-care (P = 0.015). Mechanical ventilation was also significantly associated with increased problems with mobility (P = 0.022), self-care (P = 0.045), and usual activities (P = 0.015). Lower educational levels were linked to increased problems in mobility (P = 0.013) and anxiety/depression (P = 0.042). Vasopressor use in the ICU was associated with increased pain levels (P = 0.029). Higher HADS scores on day 1 were significantly associated with increased problems in pain/discomfort (P < 0.001) and anxiety/depression (P = 0.002).
Table 3 shows the results for the multivariate analysis of factors influencing EQ-5D-5L dimensions at 90 days post-discharge. After adjusting for potential confounding factors, older age was significantly associated with poorer outcomes in multiple dimensions, including increased pain/discomfort (P = 0.004), reduced ability to perform usual activities (P < 0.001), diminished self-care capacity (P < 0.001), and impaired mobility (P < 0.001). Lower BMI was linked to difficulties in self-care (P = 0.002), mobility (P = 0.006), and anxiety/depression symptoms (P = 0.006). Higher HADS scores on day 1 were strongly associated with increased pain/discomfort (P < 0.001), anxiety/depression symptoms (P = 0.002), and reduced ability to perform usual activities (P < 0.001). Admission due to infection was a significant predictor of impairments in usual activities (P = 0.003). CFS was consistently associated with poorer outcomes across multiple dimensions, including pain/discomfort (P = 0.042), usual activities (P < 0.001), self-care (P < 0.001), and mobility (P < 0.001). Socioeconomic factors also played a role: retired status was linked to worse outcomes in usual activities (P = 0.037), self-care (P = 0.002), and mobility (P = 0.007). Higher education levels were associated with better outcomes in self-care (P = 0.019) and mobility (P = 0.015).
Table 4 presents the factors affecting EQ-5D-5L total scores at 90 days post-discharge. In the multivariate regression analysis, older age (coefficient = −0.002, 95% CI: −0.004 to −0.001, P = 0.001), infection as the admission diagnosis (coefficient = −0.069, 95% CI: −0.116 to −0.022, P = 0.004), higher CFS scores (coefficient = −0.016, 95% CI: −0.024 to −0.007, P = 0.001), and higher baseline HADS total scores (coefficient = −0.005, 95% CI: −0.007 to −0.002, P = 0.001) were significantly associated with lower EQ-5D-5L total scores.
Factors associated with HADS scores at 90 days post-discharge
Multivariate regression analysis identified significant predictors of anxiety and depression symptoms 90 days post-discharge, as measured by the HADS (Table 5). For the anxiety subscale, higher CFS scores (coefficient = 0.308, 95% CI: 0.132 to 0.484, P = 0.001) and higher baseline HADS total scores (coefficient = 0.189, 95% CI: 0.135 to 0.243, P < 0.001) were significantly associated with increased anxiety symptoms. For the depression subscale, older age (coefficient = 0.075, 95% CI: 0.038 to 0.112, P < 0.001) and higher baseline HADS total scores (coefficient = 0.215, 95% CI: 0.142 to 0.289, P < 0.001) were significant predictors of higher depression scores. For the total HADS score, higher CFS scores (coefficient = 0.529, 95% CI: 0.150 to 0.909, P = 0.007) and higher baseline HADS total scores (coefficient = 0.385, 95% CI: 0.268 to 0.501, P < 0.001) were significantly associated with increased overall anxiety and depression symptoms (Table 6).
Relationship between initial HADS, CFS, and outcomes at 90 days post-discharge
Figure 2 illustrates the relationships between initial HADS scores, CFS, and outcomes at 90 days, specifically follow-up HADS scores and EQ-5D-5L total scores.
Correlation among initial HADS, CFS, and outcomes 90 days post-discharge. (A) Correlation between initial HADS scores and 90-day outcomes. (B) Correlation between clinical frailty scale and 90-day outcomes. HADS hospital anxiety and depression scale, EQ-5D-5L five-level version of EuroQoL 5-Dimension.
The associations between day 1 HADS scores and 90-day outcomes are depicted in Fig. 2A. A positive correlation was observed between day 1 HADS scores and 90-day follow-up HADS scores (correlation: 0.435, P < 0.001), suggesting that higher anxiety and depression levels at ICU admission are associated with persistent psychological distress at 90 days. Additionally, a negative correlation was noted between day 1 HADS scores and 90-day EQ-5D-5L total scores (correlation: −0.192, P = 0.008), indicating that greater baseline anxiety and depression are linked to poorer HRQoL at 90 days. Figure 2B shows the association between CFS scores and 90-day outcomes. A positive correlation between CFS and 90-day follow-up HADS scores (correlation: 0.205, P < 0.001) indicates that higher frailty levels are associated with increased psychological distress. Conversely, a negative correlation between CFS and 90-day EQ-5D-5L total scores (correlation: −0.298, P = 0.008) suggests that greater frailty is linked to poorer HRQoL at 90 days. These findings highlight the combined impact of psychological distress and frailty on long-term patient outcomes.
Changes in EQ-5D-5L domain scores over time
Changes in each of the five EQ-5D-5L domains between day 30 and day 90 post-discharge were also analyzed separately from the total EQ-5D-5L scores (Table S1). Significant improvements were observed in the domains of mobility (mean score: 2.04 to 1.84, P < 0.01), self-care (1.78 to 1.61, P < 0.01), and usual activities (2.12 to 1.90, P < 0.01). The total EQ-5D-5L index score also increased significantly from 0.73 ± 0.18 at day 30 to 0.76 ± 0.16 at day 90 (P < 0.01). In contrast, no statistically significant changes were noted in the pain/discomfort and anxiety/depression domains. These findings suggest that physical function domains tend to improve more clearly over time than psychological or emotional dimensions.
Discussion
This multicenter prospective study provides important insights into the factors influencing HRQoL and psychological outcomes among ICU survivors 90 days post-discharge, emphasizing the impact of initial psychological states and clinical characteristics. The findings contribute to the limited body of research on mid-term HRQoL predictors in critically ill patients, with a focus on anxiety, depression, and functional recovery.
Previous evidence indicates varied outcomes for ICU survivors, with a general decline in HRQoL, particularly in physical functioning3. This decline is more pronounced in patients who suffer from severe conditions, such as acute respiratory distress syndrome or sepsis9,10. Most studies utilized the SF-36 and EQ-5D scores, which are well-recognized measures of HRQoL2,3,11,12,13. Factors associated with HRQoL include frailty status, length of ICU stay, mechanical ventilation duration, and sedation duration. Additionally, PICS, unemployment, low income, and advanced age are significantly associated with declines in mental and functional health3,4,14,15.
Clinical frailty, as measured by the CFS, is a significant determinant of both HRQoL and psychological outcomes among ICU survivors16. Frailty, a critical marker of resilience and recovery capacity, was strongly associated with worse mobility, reduced self-care ability, and heightened psychological distress at 90 days post-discharge. Frail patients demonstrated diminished independence, impaired physical function, and increased anxiety and depression, highlighting the interplay between physical and mental health during recovery. These findings emphasize the importance of assessing frailty at ICU admission to guide individualized rehabilitation strategies and post-ICU care. This observation aligns with previous studies linking frailty to poor recovery trajectories, underscoring its predictive value for long-term outcomes and its role in optimizing post-ICU interventions.
The HADS was developed to assist in identifying anxiety disorders and depression in patients hospitalized due to various illnesses17. Comprising a total of 14 items, this questionnaire is known to be more useful and appropriate for evaluating and supporting the mental health of hospitalized patients than diagnosing and treating psychiatric patients18. Since its development in 1983, the HADS has been validated in numerous countries worldwide. In South Korea, a systematic translation process led to the creation of the Korean version of HADS, which has demonstrated reliability and validity19. Evidence indicates that a score of 8 or above on both the HADS-Anxiety (HADS-A) and HADS-Depression (HADS-D) subscales offers the optimal sensitivity and specificity for case definition20.
Our results indicate that initial HADS scores significantly influence both mid-term HADS and EQ-5D-5L scores among ICU survivors, consistent with previous research indicating that early psychological distress can adversely affect long-term HRQoL. For instance, Davydow et al. demonstrated that higher baseline anxiety and depression levels are associated with poorer HRQoL outcomes in ICU survivors4. Similarly, Needham et al. highlighted the importance of early psychological assessments in predicting post-ICU recovery trajectories21. The current results expand on such findings by demonstrating the important association between initial HADS scores on multiple EQ-5D-5L domains, including mobility, self-care, pain/discomfort, and anxiety/depression, underscoring the interconnectedness of psychological and physical recovery.
Uniquely, these findings establish initial HADS scores as a central predictor, not only of persistent psychological distress but also of mid-term functional outcomes, emphasizing the necessity for routine psychological assessment during ICU admission. Early identification of patients with high anxiety and depression scores could enable targeted interventions, such as psychological counseling or structured post-discharge follow-ups, to mitigate the long-term effects. Furthermore, the results support the development of multidisciplinary recovery programs, integrating mental health support to address the sustained challenges faced by ICU survivors. These findings highlight the importance of proactive mental health management to optimize recovery and improve overall HRQoL in this vulnerable population.
This study has several strengths. First, it is the first large-scale prospective observational study conducted in Korea to explore factors affecting the HRQoL of ICU survivors. Second, by including all ICU patients rather than focusing on a specific disease group, this study identified influential factors that are broadly applicable to any patient admitted to the ICU. This comprehensive approach enhances the clinical utility of the findings, as they can inform strategies for a wide range of critically ill patients, regardless of their underlying conditions.
Despite its strengths, this study has limitations. First, the sample was relatively small compared to the number of patients initially screened, which may limit the generalizability of the findings. The high rate of refusal to provide consent among eligible patients could have introduced selection bias. Previous studies suggest that cultural factors, including stigma and reluctance to disclose psychological distress, can affect research participation, particularly in studies involving mental health assessments22,23. Second, the study population was confined to patients in South Korean tertiary medical centers, and cultural or healthcare system differences may impact the applicability of these results to other settings. Third, the reliance on telephone interviews for HRQoL assessments may have introduced reporting bias, limited the ability to capture subtle psychological or functional impairments, and excluded patients with communication barriers. Fourth, we did not evaluate skeletal muscle loss or strength, which are known to significantly affect post-ICU physical recovery24. Fifth, subgroup analyses based on categorical divisions of HRQoL scores, such as severe impairment categories, involved relatively small samples, and the results should, therefore, be interpreted with caution. Lastly, although multivariate regression was employed to adjust for a wide range of variables, we cannot exclude the influence of unmeasured confounders, such as pre-ICU functional status and post-discharge social support, which may have affected the outcomes.
Conclusion
Through this large-scale prospective observational study, we demonstrated that initial HADS scores and clinical frailty are significant predictors of mid-term HRQoL outcomes in ICU survivors, influencing both psychological well-being and functional recovery. Frailty, a critical marker of resilience and recovery capacity, was consistently associated with worse outcomes across multiple dimensions, including mobility, self-care, and psychological distress. This finding highlights the importance of systematically assessing both HADS scores and frailty at the onset of ICU admission or as early as possible during the ICU stay. Early identification of patients with high anxiety or depression levels and those with significant frailty enables targeted interventions, such as psychological support, tailored physical rehabilitation, and structured follow-ups, to mitigate long-term impairments in HRQoL. Additionally, the results underscore the need for a multidisciplinary approach to ICU recovery, integrating mental health management alongside individualized rehabilitation strategies to optimize outcomes. These findings provide critical evidence to guide clinical practice and improve overall quality of care for this vulnerable population.
Methods
Study design and participants
This multicenter prospective cohort study was conducted at four tertiary/academic medical centers in South Korea from June 2021 to September 2022. From day 1 to ICU discharge, the researchers assessed patients for delirium using the 4 A’s test (4AT) and Confusion Assessment Method for the ICU (CAM-ICU), documenting its presence throughout the ICU stay.
On day 1, defined as the day of admission to the ICU, baseline characteristics, including sex, age, living arrangement, employment status, education level, smoking history, alcohol history, and body mass index (BMI), were collected. Additionally, psychological and subjective assessments, such as the Hospital Anxiety and Depression Scale (HADS) and Visual Analog Scale (VAS), were measured. Key laboratory data, including protein and albumin levels, were also recorded at ICU admission. During the ICU stay, the researchers documented key clinical variables, including ICU length of stay (LOS), presence of infection as the reason for admission, previous history of delirium, Simplified Acute Physiology (SAPS) III score, SOFA score, Charlson Comorbidity Index (CCI), Clinical Frailty Scale (CFS), and the use of vasopressors, sedatives, opioids, mechanical ventilation, and renal replacement therapy (RRT).
Inclusion criteria were adults aged 20 and over, admitted to the ICU for more than 24 h, and with no cognitive dysfunction before ICU admission. Exclusion criteria were failure to provide informed consent, inability to communicate due to a history of psychiatric problems, Parkinson’s disease, or stroke, or inability to participate in the HRQoL assessment interview 90 days post-discharge.
HRQoL measurement
HRQoL was assessed through telephone interviews conducted 30- and 90-days post-discharge. HRQoL assessments included the new five-level version of EuroQoL 5-Dimension (EQ-5D-5L) and Hospital Anxiety and Depression Scale (HADS). All research nurses and intensivists involved in this study were trained to properly administer these questionnaires. The HADS was measured on day 1 and 30 and 90 days after discharge, while the EQ-5D-5L was assessed 30- and 90-days post-discharge. Post-discharge interviews were conducted via telephone. The EQ-5D-5L, developed by the EuroQoL Group, is a standardized tool used to evaluate a patient’s health status across five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, each rated on a five-level scale ranging from 1 (no problems) to 5 (extreme problems)25. The total EQ-5D-5L score is calculated by summing responses across all domains, with lower scores indicating poorer quality of life and higher scores indicating better quality of life. The HADS score is employed to evaluate the patient’s levels of anxiety and depression, comprising 14 items split into two subscales assessing anxiety and depression, each item scored from 0 (no symptoms) to 3 (severe symptoms), with higher scores indicating more severe anxiety or depression6.
Statistical analysis
Continuous variables are reported as means with standard deviations or medians with interquartile ranges, depending on their distribution. Categorical variables are presented as numbers (%). Differences between groups were analyzed using the independent t-test or Mann−Whitney U test for continuous variables, and the chi-squared or Fisher’s exact test for categorical variables, as appropriate. Prior to analysis, an a priori power calculation was performed to estimate the minimum required sample size for multivariable regression. Using conventional parameters (α = 0.05, power = 0.80, and medium effect size f2 = 0.15) and assuming 10 explanatory variables, the estimated, minimum sample size was approximately 50 patients. Multivariate logistic regression analyses with stepwise selection were performed to identify significant predictors of 90-day HRQoL outcomes. To assess potential multicollinearity among independent variables included in the regression models, variance inflation factors (VIFs) were calculated. All VIF values were below commonly accepted thresholds (VIF < 5), indicating no significant collinearity. Detailed results are presented in Table S2. In addition to initial HADS scores, the model included clinically meaningful variables: demographic factors (sex, age, living arrangement, employment status, education level, smoking history, alcohol history, BMI), ICU-related variables (ICU LOS, use of vasopressors, sedatives, opioids, mechanical ventilation, RRT), clinical factors at ICU admission (protein level, albumin level, infection as the reason for admission, SAPS III, SOFA, CCI, CFS, VAS), and delirium incidence and prior history (presence of delirium, previous history of delirium). Clinical parameters with a P value of 0.05 in the univariate logistic regression were included in the multivariate logistic regression. To evaluate the goodness-of-fit of the logistic regression model, we used the Hosmer−Lemeshow test26. The test results indicated an adequate fit between the model and the observed data. The goodness-of-fit was computed to assess the relevance of the logistic regression model. Odds ratios (ORs) and the corresponding 95% confidence intervals (CIs) were calculated. Longitudinal changes in HRQoL from Day 30 to Day 90 were analyzed using repeated-measures approaches, and correlations between initial HADS scores, CFS, and 90-day HRQoL were assessed with linear regression. All tests were two-sided, and P-values < 0.05 were considered statistically significant. Statistical analyses were conducted using Python software version 3.13.0 (Python Software Foundation, Beaverton, Oregon, United States).
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Fan, E. et al. Physical complications in acute lung injury survivors: a two-year longitudinal prospective study. Crit. Care Med. 42, 849–859. https://doi.org/10.1097/ccm.0000000000000040 (2014).
Parsons, E. C. et al. Post-discharge insomnia symptoms are associated with quality of life impairment among survivors of acute lung injury. Sleep. Med. 13, 1106–1109. https://doi.org/10.1016/j.sleep.2012.05.010 (2012).
Dowdy, D. W. et al. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Med. 31, 611–620. https://doi.org/10.1007/s00134-005-2592-6 (2005).
Davydow, D. S., Gifford, J. M., Desai, S. V., Bienvenu, O. J. & Needham, D. M. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med. 35, 796–809. https://doi.org/10.1007/s00134-009-1396-5 (2009).
Hopkins, R. O. & Girard, T. D. Medical and economic implications of cognitive and psychiatric disability of survivorship. Semin Respir Crit. Care Med. 33, 348–356. https://doi.org/10.1055/s-0032-1321984 (2012).
Ridley, S., Biggam, M. & Stone, P. A cost-utility analysis of intensive therapy. II: quality of life in survivors. Anaesthesia 49, 192–196. https://doi.org/10.1111/j.1365-2044.1994.tb03419.x (1994).
Boyle, M. et al. The effect of chronic pain on health related quality of life amongst intensive care survivors. Aust Crit. Care. 17, 104–106. https://doi.org/10.1016/s1036-7314(04)80012-2 (2004).
Deana, C. et al. Quality of Life in COVID-Related ARDS Patients One Year after Intensive Care Discharge (Odissea Study): A Multicenter Observational Study. J. Clin. Med. 12, 1. https://doi.org/10.3390/jcm12031058 (2023).
Davidson, T. A., Caldwell, E. S., Curtis, J. R., Hudson, L. D. & Steinberg, K. P. Reduced quality of life in survivors of acute respiratory distress syndrome compared with critically ill control patients. Jama 281, 354–360. https://doi.org/10.1001/jama.281.4.354 (1999).
Heyland, D. K., Hopman, W., Coo, H., Tranmer, J. & McColl, M. A. Long-term health-related quality of life in survivors of sepsis. Short form 36: a valid and reliable measure of health-related quality of life. Crit. Care Med. 28, 3599–3605. https://doi.org/10.1097/00003246-200011000-00006 (2000).
Spadaro, S. et al. Fatigue in intensive care survivors one year after discharge. Health Qual. Life Outcomes. 14, 148. https://doi.org/10.1186/s12955-016-0554-z (2016).
Yang, X. et al. Prognosis and antibody profiles in survivors of critical illness from COVID-19: a prospective multicentre cohort study. Br. J. Anaesth. 128, 491–500. https://doi.org/10.1016/j.bja.2021.11.024 (2022).
Paul, N. et al. Subjective ratings of mental and physical health correlate with EQ-5D-5L index values in survivors of critical illness: A construct validity study. Crit. Care Med. 51, 365–375. https://doi.org/10.1097/ccm.0000000000005742 (2023).
Bagshaw, S. M. et al. Long-term association between frailty and health-related quality of life among survivors of critical illness: a prospective multicenter cohort study. Crit. Care Med. 43, 973–982. https://doi.org/10.1097/ccm.0000000000000860 (2015).
Demoro, G. et al. Long-term consequences in survivors of critical illness. Analysis of incidence and risk factors. Ann. Ist Super Sanita. 56, 59–65. https://doi.org/10.4415/ann_20_01_09 (2020).
Muscedere, J. et al. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 43, 1105–1122. https://doi.org/10.1007/s00134-017-4867-0 (2017).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr Scand. 67, 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x (1983).
Michopoulos, I. et al. Hospital Anxiety and Depression Scale (HADS): validation in a Greek general hospital sample. Ann. Gen. Psychiatry 7, 1. https://doi.org/10.1186/1744-859x-7-4 (2008).
Choi, J. H. et al. The reliability and validity of the Korean version of hospital anxiety and depression scale using Rasch measurement theory in patients with parkinson’s disease. J. Korean Neurol. Assoc. 39, 312–321. https://doi.org/10.17340/jkna.2021.4.7 (2021).
Wu, Y. et al. Accuracy of the hospital anxiety and depression scale depression subscale (HADS-D) to screen for major depression: systematic review and individual participant data meta-analysis. BMJ 373, n972. https://doi.org/10.1136/bmj.n972 (2021).
Needham, D. M. et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med 40, 502–509. https://doi.org/10.1097/CCM.0b013e318232da75 (2012).
Hughes-Morley, A., Young, B., Waheed, W., Small, N. & Bower, P. Factors affecting recruitment into depression trials: systematic review, meta-synthesis and conceptual framework. J. Affect. Disord. 172, 274–290. https://doi.org/10.1016/j.jad.2014.10.005 (2015).
George, S., Duran, N. & Norris, K. A systematic review of barriers and facilitators to minority research participation among African americans, latinos, Asian americans, and Pacific Islanders. Am. J. Public. Health. 104, e16–31. https://doi.org/10.2105/ajph.2013.301706 (2014).
Deana, C. et al. Bioimpedance-assessed muscle wasting and its relation to nutritional intake during the first week of ICU: a pre-planned secondary analysis of nutriti study. Ann. Intensive Care. 14, 29. https://doi.org/10.1186/s13613-024-01262-w (2024).
Herdman, M. et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 20, 1727–1736. https://doi.org/10.1007/s11136-011-9903-x (2011).
Lemeshow, S. & Hosmer, D. W. A review of goodness of fit statistics for use in the development of Logistic-Regression models. Am. J. Epidemiol. 115, 92–106. https://doi.org/10.1093/oxfordjournals.aje.a113284 (1982).
Acknowledgements
The authors wish to acknowledge the financial support of the Catholic Medical Center Research Foundation made in the program year of 2022.
Funding
This research was supported by a grant of Patient-Centered Clinical Research Coordinating Center (PACEN) funded by the Ministry of Health & Welfare, Republic of Korea (grant number: RS-2020-KH094340).
Author information
Authors and Affiliations
Contributions
KHK and JL analyzed and interpreted the patient data and drafted the manuscript. JML, YSL, KSC, and CRC made substantial contributions to the study conception. YSL, KSC, CRC, and JL designed the study, interpreted the data, and substantively revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
This study was conducted in accordance with the relevant legislation and approved by the Ethics Committee of Seoul St. Mary’s Hospital (KC21ONDI0504). The study complied with the Declaration of Helsinki and Good Clinical Practice Guidelines, and all patients provided informed consent for inclusion in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, K.H., Lee, J.M., Lee, Y.S. et al. Factors affecting health-related quality of life in ICU survivors. Sci Rep 15, 25829 (2025). https://doi.org/10.1038/s41598-025-11431-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-11431-x