Abstract
Dietary habits are unique to geography and may exert crucial influence in the commencement of many diseases, including cancer. North-eastern region of India, exhibit unique food habits and are different from the rest of the country. This study investigates the association between dietary habits and site-specific cancer occurrence among patients registered with the North East Cancer Hospital and Research Institute (NECHRI) in 2022. A total of 511 cancer patients were initially accessed, of which 187 (81 female and 106 male patients) participated in the study by providing information about their dietary habits and addiction patterns to specific food beverages. The study employed multivariate linear regression analysis (MLRA) to correlate dietary habits with site-specific cancer incidence. One notable finding was the prevalence of raw betel nut consumption among female patients with cancers specific to female organs, such as cervical and ovarian cancers (21.4% for cervical cancer and 100% for ovarian cancer). Among the total cancer cases, 49.05% of male and 37.04% of female patients reported regular consumption of raw betel nut, indicating a potential association between betel nut consumption and cancer development. The MLRA also revealed a significant correlation between the regular consumption of smoked food and cancer incidence, affecting 31.13% of male and 25.93% of female patients with various types of cancer. Additionally, addiction to tobacco, smokeless tobacco, alcohol, and fermented alcohol showed a notable correlation with incidence of cancers in male, particularly in oral, esophageal, and alveolar. This is the first systematic study in north-east population of India to show the relationship between specific dietary habits and site-specific cancer occurrence among both male and female populations. The findings underscore the importance of right dietary habits and lifestyle modifications in cancer prevention strategies, particularly in regions where certain dietary habits are prevalent. Further research is warranted to elucidate the mechanisms underlying these associations and to develop targeted prevention and intervention strategies.
Similar content being viewed by others
Introduction
Various factors contribute to the development of cancer in humans, including genetic changes, lifestyle choices, environmental exposures, and dietary habits. Among these, dietary habits have a profound impact on health outcomes by influencing nutrient intake, antioxidant status, body weight, and hormonal balance, all of which ultimately affect the risk of developing cancer1,2.
The North-eastern region of India (NERI) has distinctive dietary practices, including the consumption of smoked and fermented foods3,4. These culinary traditions are conferred through unconventional methods or with indigenous ingredients, which may lead to fermentation and ultimately have a significant impact on human health. Additionally, prevalent among the populace the habit of addiction to tobacco, non-tobacco products, locally fermented alcoholic beverages, and betel nut chewing, further complicating health outcomes in this region4.
One significant dietary risk factor for cancer is the consumption of smoked and processed meats, which often contain carcinogenic chemicals like polycyclic aromatic hydrocarbons (PAHs), nitrosamines, and heterocyclic amines due to preservation methods5. According to the World Health Organization (WHO), smoked meats, alcohol, and tobacco are classified as cancer-causing agents6,7. Some studies have linked regular consumption of smoked meats to an increased risk of colorectal cancer8. Research conducted by the United States National Mortality Follow-up Survey found that factors like age, lifestyle, and especially diet have a big impact on cancer rates9. Surprisingly, while tobacco and alcohol use show lesser connections to various cancers, smoked meat consumption consistently correlate with higher cancer risks10,11. Long-term consumption of smoked red meat has been associated not only with colorectal cancer but also with cardiovascular disease and type 2 diabetes12,13. A Study also suggests a specific link between the consumption of smoked fish and an increased risk of prostate cancer, which is attributed to the formation of certain chemicals during smoking14. The influence of race and dietary practices on cancer risk has been explored, and it has been shown that increased breast cancer risks among certain ethnic groups with specific dietary habits and culinary findings15. Furthermore, it is not only consumption that poses a risk; occupational exposures in the meat industry have shown elevated lung cancer risks among workers, potentially assimilated with exposure to carcinogens during meat processing16,17. Other dietary factors such as obesity, hypertension, diabetes, and the ingestion of certain chemicals from cooked meats have also been associated with kidney and renal pelvis cancers18. Genetic variability in enzymes responsible for metabolizing carcinogens has also been explored in relation to breast cancer risk associated with the consumption of grilled and smoked meats15,19. Beyond meat consumption, habit such as betel nut chewing, though culturally significant, pose serious health risks due to their carcinogenic properties, implicated in liver and oral cancers20,21. For instance, a study attributed, chewing betel quid has been associated with approximately half of the oral cancer cases reported in the Indian subcontinent and Taiwan, with population attributable fractions of 53.7% for Taiwanese citizens and 49.5% for Indian citizens, but without detailed understanding22.
Epidemiology studies have revealed a higher prevalence of certain cancers of NERI compared to the national average23. The national center registry shows 150–200 cancer cases per lakh people in the NERI against the 80–110 instances of cancer per lakh population nationwide23. According to the ICMR annual report for 2021, the most prevalent cancer kinds in men are nasopharyngeal, stomach, and esophageal; while in women they are cervical, breast, and stomach cancer24. The report mentioned that the top cancer sites varied from registry to registry in the nation’s east and northeast and the northeastern state Tripura carries highest burden of lung cancer. The most common site of cancer among individuals of Dibrugarh, Kamrup Urban, Cachar, district of Assam and state of Meghalaya was the esophagus. In contrast, for those registered in Mizoram, Sikkim, Naharlagun, and Pasighat, stomach cancer was the most frequently reported24. Nasopharyngeal cancer was the most common cancer site recorded in the Nagaland registry. Lung cancer remained the most common cancer in the West India across all registries. The NERI has the greatest incidence of cancer for both sexes, according to a recent analysis of National Corrections Reporting Program (NCRP) data23,24.
The cancer incidence rates in this region are higher than the national average. While the harmful effects of alcohol, tobacco, and smoked foods are well-documented, there is limited research on how indigenous dietary habits, specific addictions, and genetic factors interact in North-east region of India (NERI). The role of these factors in gender-specific and site-specific cancer risks has largely been overlooked, especially in this high-risk area where dietary and cultural practices significantly influence health. Some studies link betel nut and dietary habits to cancers like oral and esophageal cancers, but few explore their connections to other cancers, such as breast, cervical, and ovarian cancers in women. This study aims to fill this gap by examining how dietary and addictive behaviors contribute to cancer risk within NERI’s unique cultural and dietary context. Advanced statistical methods, such as multivariate regression modeling, are used to analyze the impact of these factors on different cancer types.
Utilizing a hospital based patient registry, our study is an attempt in NERI to elucidate the complex interplay among specific addiction, dietary behaviors, and site-specific cancer susceptibility, with a particular emphasis on the distractive dietary practices prevalent in the north-east state Assam. This study is the first of its kind in the region aiming to examine the relationship between dietary patterns and the development of cancer at specific sites among in both men and women.
Methods and materials
Study design and sampling
The present study was conducted at the North East Cancer Hospital and Research Institute (NECHRI) using a cross-sectional survey design to investigate potential associations between cancer susceptibility and traditional dietary practices among cancer patients registered in 2022. The study involved the evaluation of clinical and demographic data from 511 cancer patients enrolled at NECHRI in 2022. Of these, 290 were male (56.7%) and 221 were female (43.3%). A structured data was collected for each patient through an interviews using a standardized form (validated through a dietician after a pilot study), documenting demographic information, cancer diagnosis details, and comprehensive dietary assessments, including the consumption of smoked and fermented foods, as well as alcohol and tobacco use. A total of 187 patients (36.6%), including 106 males (56.7%) and 81 females (43.3%), participated in the study. To ensure privacy, each participant provided informed consent before the interview, and responses were recorded anonymously. The dietary and lifestyle data were self-reported by participants. The findings highlight dietary patterns among indigenous populations and their potential role in cancer incidence. The study was approved by the University Human Ethics Committee (UHEC) (Approval No. AdtU/Ethics/Stdnt-lett/2023/190, Assam down town University), and strict adherence to NECHRI’s human ethical guidelines ensured participant anonymity and informed consent. The data analysis provided valuable insights into the correlations between dietary habits and cancer types, offering a foundation for future research and tailored public health strategies for this region.
Exclusion and inclusion criteria
The inclusion criteria for the cross-sectional survey conducted at NECHRI in 2023 included individuals who were diagnosed with cancer and registered at the hospital in 2022, were adults (aged 18 years and above), provided informed consent to participate, were accessible and reachable for interview during the survey period, and completed the structured survey conducted by trained interviewers. So accordingly the criteria were as follows-.
Inclusion
Adult patients diagnosed with cancer and registered at NECHRI in 2022, aged between 18 and 90 years, and residing in the NERI region.
Exclusion
Non-cancer patients, individuals outside the defined demographic area, those outside the specified age range, as well as patients who declined to provide informed consent or those for whom comprehensive data could not be collected due to incomplete responses or data quality issues. These criteria were essential to ensure the study focused on cancer patients and maximized the reliability and completeness of the collected data for analysis.
Statistical analysis
Multivariate linear regression analysis
The methodology for multivariate linear regression analysis on the habit-cancer matrix involves first collecting and organizing data on the prevalence of different habits (e.g., betel nut use, smoking, alcohol consumption) and the incidence of various cancer types. This data is structured into a matrix format (\(\:{y}_{i,j}\)) where rows represent different cancer types and columns represent different habits. Multivariate linear regression is then applied, modeling each cancer type as a dependent variable regressed against multiple habits as independent variables. The regression assumes different slopes and intercepts of the linear fits between the dependent and independent variables and is represented as
where, the subscripts\(\:\:i\) and \(\:j\), respectively, represent the types of cancer and food habit, with between cancer concurrent correlation \(COV\left( {\varepsilon _{{i,j}} ,\varepsilon _{{i,j}} } \right) = \sigma _{{i,j}}\).The regression analysis provides the estimates \(\:{a}_{j}\) and \(\:{b}_{j}\) along with \(\:{\sigma\:}_{i,j}\). MATLAB software is used for the multivariate linear regression analysis. By calculating “cut points” and comparing regression lines, the relative influence of each habit on specific cancer types is determined, allowing for qualitative assessment and conclusions about which habits are most influential across different cancers. Validation and sensitivity analysis ensure the robustness of the findings, supporting evidence-based insights for public health interventions or further research endeavors.
Results
Distribution of cancer risk by demographics and age-sex categories
The hospital-based patient study analyzed data from 511 patients, with 43.3% being female and 56.7% male (Fig. 1A). From this group, 187 patients were included in the analysis, comprising 106 males and 81 females who participated or consented to the study. The analysis revealed distinct age-related patterns in cancer vulnerability between genders (Fig. 1B,C). Among males, those aged > 60 years were identified as the most vulnerable age group for cancer detection, representing 55.7% of the male population studied. Conversely, females aged > 40-<60 years old were found to be the most vulnerable, comprising 51.9% of the female participants (Fig. 1B,C). These findings suggest differential cancer susceptibility based on age and gender within this patient cohort.
Analysis of site-specific cancer patterns across genders
The distribution of site-specific cancers among the male and female populations in the study reveals notable differences in prevalence (Table 1). Among males, esophageal cancer emerged as the most prevalent, accounting for 18.9% of total cancer cases, followed by lung cancer at 10.4%. In contrast, among females, breast cancer was the most diagnosed, affecting 19.8% of the female population studied, followed closely by cervical cancer at 17.3% and esophageal cancer at 16.0% (Fig. 2A). Interestingly, collectively, esophageal, lung, and tongue cancers exhibit the highest incidence rates across both genders within the studied population. These findings underscore the gender-specific patterns of cancer prevalence and highlight the significant burden posed by certain cancer types, suggesting potential areas for targeted intervention and research efforts.
Impact of lifestyle factors: food patterns and addictions
Further, the study examined the distribution of food patterns and specific beverage addictions among the male and female populations, considering factors such as tobacco and alcohol use, dietary habits, and family history of cancer (Fig. 2B) (Table 2). Among males, 31.1% were addicted to tobacco, 46.2% to smokeless tobacco, and 34.0% to marketed alcohol. Additionally, 31.1% of males and 25.9% of females reported frequent consumption (at least once in a week) of smoked food products. Notably, among both male and female participants diagnosed with cancer, 49.1% of males and 37.0% of females were found to have a regular habit of chewing raw betel nut, indicating a potential correlation between this habit and cancer incidence (Fig. 2B). These findings underscore the importance of assessing lifestyle factors such as tobacco and betel nut consumption in relation to cancer risk within the studied population.
Correlation between food habits and cancer types
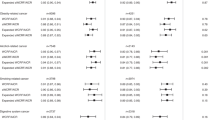
The regression analysis depicted in Fig. 3 explores the relationship between specific food habits and the likelihood of developing various types of cancer among the patient population. The regression coefficients derived from this analysis offer valuable insights into how each food habit impacts the risk and direction of different cancer types. This statistical approach helps to understand which dietary behaviors are associated with increased or decreased chances of developing particular cancers within the studied population. Each regression line has a different slope and intercept, leading to varying probabilities of any habit against a particular type of cancer, and can be qualitatively measured from the cut points of different regression lines from a vertical line drawn at any cancer type on the horizontal axis. For instance, in the case of ovary cancer in females, the habit of taking betel nuts (BN) is maximum, followed by the sequence of smoked food (SF), family background (FB), smokeless tobacco (ST), marketed alcohol (MA), fermented food (FF), and fermented alcohol (FA), and tobacco (T) being the minimum influence. An equivalent conclusion can be drawn for other cancer types following the same argument. The more apart the cut-points, the more influential the corresponding habits are on a particular cancer. Overall, BN has the maximum impact on all cancer types of females. On the contrary, the habit of ST is dominant over that of BN for male breast and Alveolus cancers. However, ST and BN have equal influence on Esophagus cancer.
This figure presents a multivariate linear regression analysis applied to the habit-cancer matrix. The analysis quantifies the relationship between the numbers of people addicted to a particular habit for specific cancer types. Here, Y-axis represents quantitative measure of a habit on a specific cancer type, X-axis denotes the cancer types, and the matrix captures the concurrent correlations between these factors.
Betel nut consumption and its correlation with cancer
The study found substantial links between particular cancer types and regular use of raw or fermented betel nuts. 21.4% of cervical cancer patients have this habit, while 100% of ovarian cancer cases are linked to regular betel nut use. Furthermore, 12.5% of breast cancer patients and a disturbing 61.5% of esophageal cancer patients describe similar behavior (Fig. 4). Esophageal cancer is the most common in male patients, accounting for 65% of cases connected to habitual betel nut usage (Fig. 4). Additionally, 36% of male lung cancer patients consume betel nuts (Fig. 4). These findings underscore a strong and alarming relationship between betel nut consumption and increased cancer risk across various types, impacting both male and female populations. This research highlights the critical need for targeted public health interventions to address betel nut use as a significant risk factor for cancer development.
Discussion
The primary purpose of this research article was to investigate the associations between dietary habits, addiction patterns, and site-specific cancer incidence among patients in North-east India25,26. The findings from this hospital-based case registry conducted at the North East Cancer Hospital and Research Institute (NECHRI), provide valuable insights into the complex interplay of these factors, highlighting distinct demographic and lifestyle-related vulnerabilities that may contribute to the cancer burden in this region. This research, carried out in 2023, contributes significantly to our understanding of cancer susceptibility in a region characterized by distinct dietary practices and prevalent addiction to substances such as tobacco, smoked food, traditional alcoholic beverage, and betel nut.
The study examined a cohort of 511 cancer patients, with a final sample of 187 participants (81 females and 106 males) who provided detailed information on their dietary habits and addiction patterns. The results reveal striking associations between specific dietary behaviors and cancer types, particularly highlighting the prevalence and potential impact of raw betel nut consumption, smoked food intake, and addiction to tobacco and alcohol on cancer development (Figs. 3 and 4).
Among female participants, a notable correlation was observed between raw/fermented betel nut consumption and cancers specific to female organs, notably cervical and ovarian cancers. For instance, 21.4% of cervical cancer cases and 100% of ovarian cancer cases were linked to regular betel nut use among female patients (Fig. 4). Similarly, in male patients, esophageal, oral, and alveolar cancers exhibited significant associations with tobacco, smokeless tobacco, and alcohol addiction. These findings underscore the critical role of lifestyle factors in cancer susceptibility and highlight the urgent need for targeted interventions or prevention strategies.
Furthermore, the study identified gender-specific patterns in cancer prevalence and vulnerability 6, 13). Esophageal cancer emerged as the most prevalent cancer among males (18.9%), while breast cancer was the most diagnosed among females (19.8%), followed closely by cervical cancer (17.3%) and esophageal cancer (16.0%) (Fig. 2A). These gender-specific variations suggest differential risk factors and the need for customized prevention approaches.
The distribution of dietary habits and substance addictions among study participants further emphasized their potential impact on cancer incidence. Notably, a significant proportion of both male and female patients reported regular betel nut consumption (49.1% of males and 37.0% of females), with specific cancers showing particularly strong correlations with this habit (Table 2). As evidenced, 21.4% of cervical cancer patients, over 12% of female breast cancer patients, and all ovarian cancer patients reported regular betel nut use, emphasizing the alarming link between betel nut consumption and cancer risk.
Several studies have shown that specific addictions, such as alcohol consumption and smoking, are linked to cancers like oral, lung, and stomach cancer5,6,13. However, currently there is limited conclusive research confirming the connection between nutrition and other addictions with various cancers across different populations. The consumption of betel nut, a common practice in many cultures of this region, has been associated with a spectrum of health implications, ranging from potential benefits to significant risks27,28. While some studies suggest a potential reduction in neonatal jaundice among offspring of mothers who chew betel nut during pregnancy, other research describes a concerning picture of its carcinogenic properties29. For example, aqueous extracts of betel nut have been linked to carcinogenesis in the liver of female mice through the activation of specific cellular pathways, including AMPK/Akt/mTOR, while chemical constituents have been implicated in inducing oral fibrosis via the TGF-β pathway30. Arecoline, a well-established carcinogenic compound found in betel nut, has been shown to trigger a DNA damage response cascade leading to oral cancer in animal models, and the anti-diabetic drug metformin appears to exacerbate this carcinogenic effect31. Moreover, epidemiological evidence underscores the association between betel nut chewing and oral cancer risk, with a dose-response relationship observed with both frequency and duration of use20. Additionally, adverse effects extend to pregnancy outcomes, with smokeless tobacco use, including betel nut chewing, exhibiting detrimental effects during gestation32. Mental health concerns also emerge, with long-term betel nut consumption correlating with common mental health disorders33. Mechanistically, betel nut’s aqueous fraction has been implicated further in activating immune cells and promoting pro-inflammatory cytokine release, contributing to inflammatory disorders among regular users28,34. Notably, epidemiological data from certain regions highlight betel quid chewing as a significant risk factor for breast cancer development among women27. However, studies that connect betel nut use with breast cancer risk are relatively limited, often focusing on specific cohorts and/or a specific sub-lines. For example, a study in North-east India highlights that betel quid chewing significantly increases breast cancer risk by nearly five-fold. Additionally, the absence of detoxification enzymes GSTT1 and GSTM1 is associated with a reduced risk, while the GSTP1 variant G allele is linked to a higher risk35. This limited focus, however, may restrict the broader applicability of the findings and potentially overlook other resistance mechanisms, introducing biases into the study36,37,38,39. Collectively, these findings underscore the complex interplay between betel nut consumption and health outcomes, emphasizing the need for comprehensive approaches to address its potential harms and benefits within affected communities25.
In conclusion, this study underscores the critical need for targeted public health interventions to address specific dietary habits and addiction patterns contributing to cancer incidence in North-east India26. The findings highlight the importance of lifestyle modifications and comprehensive approaches to cancer prevention, emphasizing the potential benefits of tailored interventions and strategic planning aimed at reducing betel nut use and other harmful dietary practices within affected communities. This study offers valuable insights into how diet and addictive behaviors influence cancer risk in North-east India, but it has some limitations. The cross-sectional design makes it difficult to establish a direct cause-and-effect relationship between cancer risk and specific behaviors. The reliance on self-reported data for substance use and eating habits may introduce recall bias, affecting the accuracy of the results. Although the sample size is relatively large, it only includes cancer patients from one hospital, which may limit the universal of the findings to the broader population. Additionally, the study does not consider other potential factors like genetic predisposition or exposure to environmental hazards. To overcome these limitations, future research could use longitudinal or case-control study designs to establish causal links. Including genetic and biomarker analyses could help provide a deeper understanding of how diet, addiction, and cancer risk interact. Public health strategies focusing on awareness, lifestyle changes, and region-specific screening programs should be prioritized to reduce cancer risk and improve health outcomes in North-east India. Additional investigation is required to understand the underlying mechanisms and develop effective cancer prevention and control strategies in that specific region. By integrating clinical observations with broader research on dietary influences in cancer, researchers can better understand the link between nutrition, addiction, and cancer risk. Expanding studies to include diverse cancer populations and clinical settings will help capture a wider range of factors and mechanisms, ultimately leading to more accurate and generalizable conclusions on how dietary habits, such as betel nut use, influence cancer development.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- MLRA:
-
Multivariate linear regression analysis
- NECHRI:
-
North East Cancer Hospital and Research Institute
- NERI:
-
North-east region of India
- PAHs:
-
Polycyclic aromatic hydrocarbons
- WHO:
-
World Health Organization
- ICMR:
-
Indian Council of Medical Research
- NCRP:
-
National Cancer Registry Programme
References
Steck, S. E. & Murphy, E. A. Dietary patterns and cancer risk. Nat. Rev. Cancer. 20 (2), 125–138. https://doi.org/10.1038/s41568-019-0227-4 (2020).
Thapa, R. et al. Unveiling the connection: Long-chain non-coding RNAs and critical signaling pathways in breast cancer. Pathol. Res. Pract. 249 154736. https://doi.org/10.1016/j.prp.2023.154736 (2023).
Devi, M. R., Ummalyma, S. B., Brockmann, A., Raina, V. & Rajashekar, Y. Nutritional properties of giant water bug, Lethocerus indicus a traditional edible insect species of North-East India. Bioengineered 14 (1), 2252669. https://doi.org/10.1080/21655979.2023.2252669 (2023).
Talukdar, J. et al. Altered expression of TGF-β1 and TGF-βR2 in tissue samples compared to blood is associated with food habits and survival in esophageal squamous cell carcinoma. Curr. Probl. Cancer. 45 (1), 100617. https://doi.org/10.1016/j.currproblcancer.2020.100617 (2021).
Khalili, F. et al. Polycyclic aromatic hydrocarbons (PAHs) in meat, poultry, fish and related product samples of iran: a risk assessment study. J. Environ. Health Sci. Eng. 21 (1), 215–224. https://doi.org/10.1007/s40201-023-00854-1 (2023).
Ersoy Guller, Z. et al. Diet and lifestyle in relation to small intestinal cancer risk: findings from the European prospective investigation into cancer and nutrition (EPIC). Cancer Causes Control 34 (10), 927–937. https://doi.org/10.1007/s10552-023-01731-w (2023).
Subramaniyan, V. et al. A review on epidermal growth factor receptor’s role in breast and non-small cell lung cancer. Chem. Biol. Interact. 351 109735. (2022).
Lewandowska, A., Rudzki, G., Lewandowski, T., Stryjkowska-Góra, A. & Rudzki, S. Risk factors for the diagnosis of colorectal Cancer. Cancer Control. 29, 10732748211056692. https://doi.org/10.1177/10732748211056692 (2022).
Li, Y. et al. Impact of healthy lifestyle factors on life expectancies in the US population. Circulation 138 (4), 345–355. https://doi.org/10.1161/CIRCULATIONAHA.117.032047 (2018).
Poorolajal, J., Moradi, L., Mohammadi, Y., Cheraghi, Z. & Gohari-Ensaf, F. Risk factors for stomach cancer: a systematic review and meta-analysis. Epidemiol. Health. 42, e2020004. https://doi.org/10.4178/epih.e2020004 (2020).
Hur, S. J., Yoon, Y., Jo, C., Jeong, J. Y. & Lee, K. T. Effect of dietary red meat on colorectal Cancer Risk-A review. Compr. Rev. Food Sci. Food Saf. 18 (6), 1812–1824. https://doi.org/10.1111/1541-4337.12501 (2019).
Grant, W. B., van Amerongen, B. M. & Boucher, B. J. Periodontal disease and other adverse health outcomes share risk factors, including dietary factors and vitamin D status. Nutrients 15 (12), 2787. https://doi.org/10.3390/nu15122787 (2023).
Maimaitiyiming, M. et al. Associations between an obesity-related dietary pattern and incidence of overall and site-specific cancers: a prospective cohort study. BMC Med. 21 (1), 251. https://doi.org/10.1186/s12916-023-02955-y (2023).
Torfadottir, J. E. et al. Consumption of fish products across the lifespan and prostate cancer risk. PLoS One. 8 (4), e59799. https://doi.org/10.1371/journal.pone.0059799 (2013).
Kerlikowske, K. et al. Population attributable risk of Advanced-Stage breast Cancer by race and ethnicity. JAMA Oncol. 10 (2), 167–175. https://doi.org/10.1001/jamaoncol.2023.5242 (2024).
Johnson, E. S. & Choi, K. M. Lung cancer risk in workers in the meat and poultry industries–a review. Zoonoses Public. Health. 59 (5), 303–313. https://doi.org/10.1111/j.1863-2378.2012.01459.x (2012).
Bhat, A. A. et al. MALAT1: A key regulator in lung cancer pathogenesis and therapeutic targeting. Pathol. Res. Pract. 253, 154991 (2024).
Aveta, A. et al. The impact of meat intake on bladder cancer incidence: is it really a relevant risk??. Cancers (Basel) 14 (19), 775. https://doi.org/10.3390/cancers14194775 (2022).
Nag, S. et al. Nanomaterials-assisted photothermal therapy for breast cancer: State-of-the-art advances and future perspectives. Photodiagnosis Photodyn Ther. 45, 103959 (2024).
Warnakulasuriya, S. & Chen, T. H. H. Areca nut and oral cancer: evidence from studies conducted in humans. J. Dent. Res. 101 (10), 1139–1146. https://doi.org/10.1177/00220345221092751 (2022).
Yadav, P. et al. Glutathione S-transferasesP1 AA (105Ile) allele increases oral cancer risk, interacts strongly with c-Jun kinase and weakly detoxifies areca-nut metabolites. Sci. Rep. 10 (1), 6032. https://doi.org/10.1038/s41598-020-63034-3 (2020).
Kimi, L. et al. Relevance of GSTM1, GSTT1 and GSTP1 gene polymorphism to breast cancer susceptibility in Mizoram population, Northeast India. Biochem. Genet. 54, 41–49 (2016).
Kulothungan, V. et al. Burden of cancers in India - estimates of cancer crude incidence, ylls, YLDs and dalys for 2021 and 2025 based on National Cancer registry program. BMC Cancer. 22 (1), 527. https://doi.org/10.1186/s12885-022-09578-1 (2022).
https://main.icmr.nic.in/sites/default/files/annual_repoorts/ICMR_AR_English_2021_22_1.pdf
Ngaihte, P., Zomawia, E. & Kaushik, I. Cancer in the North-East india: where we are and what needs to be done? Indian J. Public. Health. 63 (3), 251–253. https://doi.org/10.4103/ijph.IJPH_323_18 (2019).
Shanker, N. et al. Cancer scenario in North-East India & need for an appropriate research agenda. Indian J. Med. Res. 154 (1), 27–35. https://doi.org/10.4103/ijmr.IJMR_347_20 (2021).
Kaushal, M. et al. Betel quid chewing as an environmental risk factor for breast cancer. Mutat. Res. 703 (2), 143–148. https://doi.org/10.1016/j.mrgentox.2010.08.011 (2010).
Faouzi, M., Neupane, R. P., Yang, J., Williams, P. & Penner, R. Areca nut extracts mobilize calcium and release pro-inflammatory cytokines from various immune cells. Sci. Rep. 8 (1), 1075. https://doi.org/10.1038/s41598-017-18996-2 (2018).
de Costa, C. & Griew, A. R. Effects of betel chewing on pregnancy outcome. Aust N Z. J. Obstet. Gynaecol. 22 (1), 22–24. https://doi.org/10.1111/j.1479-828x.1982.tb01392.x (1982).
Nath, M., Bhattacharjee, K. & Choudhury, Y. Vildagliptin, a dipeptidyl peptidase-4 inhibitor, reduces betel-nut induced carcinogenesis in female mice. Life Sci. 266, 118870. https://doi.org/10.1016/j.lfs.2020.118870 (2021).
Khan, I., Kumar, N., Pant, I., Narra, S. & Kondaiah, P. Activation of TGF-β pathway by areca nut constituents: a possible cause of oral submucous fibrosis. PLoS One. 7 (12), e51806. https://doi.org/10.1371/journal.pone.0051806 (2012).
Kumar, S. Tobacco and areca nut chewing–reproductive impairments: an overview. Reprod. Toxicol. 36, 12–17. https://doi.org/10.1016/j.reprotox.2012.11.007 (2013).
Lin, T. Y., Chang, H. C. & Hsu, K. H. Areca nut chewing is associated with common mental disorders: a population-based study. Soc. Psychiatry Psychiatr Epidemiol. 53 (4), 393–401. https://doi.org/10.1007/s00127-017-1460-3 (2018).
Boruah, N., Singh, C. S., Swargiary, P., Dkhar, H. & Chatterjee, A. Securin overexpression correlates with the activated Rb/E2F1 pathway and histone H3 epigenetic modifications in Raw areca nut-induced carcinogenesis in mice. Cancer Cell. Int. 22 (1), 30. https://doi.org/10.1186/s12935-022-02442-z (2022).
Warnakulasuriya, S. & Chen, T. H. Areca nut and oral cancer: evidence from studies conducted in humans. J. Dent. Res. 101 (10), 1139–1146 (2022).
Rizwi, F. A. et al. Janus kinase-signal transducer and activator of transcription inhibitors for the treatment and management of cancer. J. Environ. Pathol. Toxicol. Oncol. 42 (4), 15–29. https://doi.org/10.1615/JEnvironPatholToxicolOncol.2023045403 (2023).
Bhat, A. A. et al. Pivotal modulators of TGF-β signalling in cancer pathogenesis. Noncoding RNA Res. 9 (2), 277–287 (2024).
De Rubis, G. et al. Involvement of osteopontin, EpCAM, estrogen receptor-alpha, and carbonic anhydrase IX protein in managing lung cancer via berberine-loaded liquid crystalline nanoparticles. Pathol. Res. Pract. 253 154971. https://doi.org/10.1016/j.prp.2023.154971 (2024).
Mukherjee, S. et al. Unlocking Exosome-Based theragnostic signatures: Deciphering secrets of ovarian Cancer metastasis. ACS Omega. 8 (40), 36614–36627. https://doi.org/10.1021/acsomega.3c02837 (2023).
Acknowledgements
The authors extend their sincere gratitude to all patients or their family members who participated in this study. Additionally, authors acknowledge NECHRI for sharing the patient registry. The authors also appreciate Assam down town University (AdtU) and the Institute of Advanced Study in Science and Technology (IASST), Guwahati, Assam, for providing essential laboratory infrastructure support. SKS and MPS gladly acknowledge AdtU’s Seed grant (AdtU/DRA-II/2023-24/137), which was used in part to fund the work.
Author information
Authors and Affiliations
Contributions
DD, GA, DC, DDey, and SC collected data from patients, while MPS, MNB, IL, and SKS collaborated on compiling the patient registry from NECHRI. DD and SKS accumulated and analyzed the data, while SD conducted specific analyses using MATLAB. SKS drafted the initial version of the paper, which NCT and all others co-authors have subsequently finalized. SKS has conceptualized and supervised the entire study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Deka, D., Sarma, M.P., Das, S. et al. Correlation of specific addictions with cancer sites identified among patients in Northeast India. Sci Rep 15, 27598 (2025). https://doi.org/10.1038/s41598-025-12939-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-12939-y