Abstract
This study assessed the efficacy of 60% CPP-ACP to remineralise white spot lesions (WSLs) in enamel and to occlude patent dentinal tubules in a double-blind, randomized, cross-over, in situ study. Human enamel specimens with subsurface lesions (WSLs) and root dentine specimens with open dentinal tubules were prepared and inserted into intra-oral appliances worn by volunteers. Participants wore the appliances 24 h a day for four 14-consecutive day treatment periods with a 7-day washout period between treatments. Four treatments applied with a micro-brush once daily were 60% CPP-ACP with and without 1100ppm F as SnF2, 1100ppm F as SnF2 alone and a placebo as negative control. Mineral content was measured using transverse microradiography and dentine tubules were examined using scanning electron microscopy (SEM). The data were analysed using a repeated measures ANOVA with a Sidak adjustment for multiple comparisons. Once daily application of 60% CPP-ACP with or without SnF2 produced 36.6 ± 1.6% and 28.8 ± 1.5% remineralisation of the WSLs respectively, and both were significantly higher (p < 0.0001) than that for treatment by SnF2 alone (8.8 ± 0.7%) or placebo control (2.3 ± 0.4%). SEM analysis of the dentine samples showed that daily application of 60% CPP-ACP with or without SnF2 produced near complete dentinal tubule occlusion.
Similar content being viewed by others
Introduction
Dental caries, a prevalent oral disease resulting from the demineralisation of tooth enamel to form enamel subsurface lesions known as White Spot Lesions (WSLs) before enamel breakdown occurs, remains a significant global public health issue1,2. Despite advances in preventive dentistry, dental caries continues to challenge public health, especially among vulnerable groups such as children/adolescents undergoing fixed orthodontic therapy (Fig. 1). Orthodontic therapy with fixed appliances frequently leads to peribracket WSLs, which pose aesthetic concerns upon debanding3. A 2015 meta-analysis of 14 clinical studies investigating WSLs associated with orthodontic therapy indicated that new WSLs developed in 45.8% of cases4. Most WSLs do not regress and may worsen over time. Enamel remineralisation, the natural process of restoring lost minerals to tooth structure, is crucial for halting and reversing early-stage carious lesions (WSLs), thus preserving tooth integrity and function5. However, management of WSLs on labial surfaces of upper anterior teeth post-orthodontic therapy is a challenge and requires professional intervention with innovative technologies. Recent research has increasingly focused on enhancing enamel remineralisation to swiftly and effectively regress demineralised enamel lesions6. This surge in research is largely driven by advances in materials science, nanotechnology, and our understanding of enamel mineralisation7. Non-invasive methods, such as high-concentration fluorides, can remineralise the surface layer but do not fully mask the lesions3,8, due to fluoride ion’s high reactivity and concomitant calcium requirement, thereby limiting subsurface lesion remineralisation9. Micro-invasive techniques like Icon (DMB, USA), which use resin infiltration, are costly and can lead to long-term aesthetic issues10.
Treatment of white spot lesions with a 60% CPP-ACP formulation. (A) White spot lesions (WSLs) caused by plaque accumulation around orthodontic brackets and (B) demineralisation of the underlying enamel shown on debanding and removal of the brackets. (C) Simulation of white spot lesions on human tooth enamel in vitro with the enamel block containing the WSLs cut in half and one half (left side) painted with 60% CPP-ACP using a microbrush.
A key strategy in WSL remineralisation involves using nanosized biomaterials, such as bioavailable casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) nanocomplexes11. CPP-ACP nanocomplexes have been shown to regress early caries in enamel12,13,14,15,16,17, and when combined with fluoride, CPP-AC(F)P is more effective in remineralising early caries than fluoride or CPP-ACP alone16. Dental creams containing 5–10% CPP-ACP can reverse WSLs, but this process is slow and takes several months3,18. Combining 5–10% CPP-ACP with fluoride ions expedites remineralisation, but still requires several months14,19,20,21. Thus, there is a need for an improved remineralisation technology to produce a rapid, effective, non-invasive treatment for WSLs.
Various methods aimed at improving the efficacy of CPP-AC(F)P to repair incipient caries lesions have recently been tested. Initial laboratory tests have shown that topical application of an innovative product containing high concentrations (60% w/w) of CPP-ACP painted onto the surface of enamel WSLs with a microbrush promptly masked the WSLs (Fig. 1C) and significantly improved the white spot remineralisation in vitro. The high concentration CPP-ACP forms a layer of amorphous calcium phosphate with or without fluoride on the lesion surface and is potentially an ideal and efficient approach to mask and remineralise WSLs post-orthodontic therapy. However, the effectiveness of the high concentration CPP-ACP to remineralise WSLs in situ has yet to be investigated. Furthermore, a recent study has shown some calcium phosphate-based technologies, although forming a deposit on the enamel surface, do not result in significant subsurface lesion (WSL) remineralisation22. Hence, it is imperative to test any purported remineralisation technology for its ability to remineralise enamel subsurface lesions in an in situ clinical trial.
Remineralisation technologies may also be utilised for management of dentinal hypersensitivity. Tooth dentine is often exposed in the mouth such as when the enamel is eroded or if exposed tooth roots are abraded due to over-zealous toothbrushing. This leads to exposure of microscopic dentinal tubules that, if patent and exposed to hot, cold or acidic foods or beverages in the oral cavity, can lead to pain (dentinal hypersensitivity) generated by movement of fluid in the tubules23. Dentinal hypersensitivity is often very difficult to treat and there is no current treatment that consistently eliminates its symptoms. However, the severity of these symptoms can be reduced or eliminated when dentinal tubules are physically occluded such as following topical applications of fluoride24, which leads to coverage of exposed dentinal tubules by calcium fluoride deposits25. Hence, one of the main objectives of treatment of dentinal hypersensitivity is to physically occlude the openings of these tubules with calcium and phosphate based materials to promote secondary dentine formation. The efficacy of oral health care products to reduce or eliminate dentinal hypersensitivity appears, at least partly, to depend on their fluoride and calcium levels. It has been shown that application of low concentrations of bioavailable CPP-ACP up to 10% in a tooth crème or dentifrice with or without fluoride can occlude dentinal tubules in vitro26,27 and provide relief from the symptoms of dentinal hypersensitivity clinically28. However, this treatment has the potential to be similarly enhanced and made more efficient if the treatment was targeted to the sensitive tooth with a 60% CPP-ACP(F) product rather than routinely using a low-concentration tooth crème or dentifrice as the vehicle.
To investigate these hypotheses, this present pilot study was designed to evaluate two experimental formulations of 60% CPP-ACP, one with and one without SnF2, for their therapeutic effect when applied directly to the surface of human enamel WSLs and dentine once per day using an in situ model. The primary objective of the study was to compare the improvement in remineralisation of enamel subsurface lesions after topical application of two formulations containing 60% CPP-ACP, one with stannous fluoride and one without, as well as a stannous fluoride alone treatment and a placebo control treatment. The secondary objective of the study was to compare the occlusion of open dentinal tubules after topical applications of the same treatments by observation using scanning electron microscopy (SEM).
Results
Participants and adverse events
All participants completed the cross-over in situ clinical study with 100% reported compliance. No adverse events were reported in the clinical study. The mean participant age was 46.3 years (range 36 58 years) with 1 female and 3 males. The mean unstimulated and stimulated saliva flow rates of the participants were 1.03 ± 0.23 mL/min and 3.22 ± 0.76 mL/min, respectively.
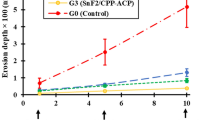
Enamel subsurface lesion remineralisation
On obtaining the complete data set, the randomization code was released and the decoded data for the variables measured from the TMR analysis and the enamel subsurface lesion remineralisation after each treatment in situ are presented in Table 1, and representative microradiographs of treated enamel subsurface lesions are shown in Fig. 2. No significant differences were observed between the initial baseline lesions used for the in situ study as shown by the LDd and ΔZd values (ANOVA, p > 0.05) for the four groups (Table 1).
Significant differences were observed in the subsurface remineralisation (%R, primary outcome variable) and the change in mineral content (ΔZd-ΔZr, secondary outcome variable) after the different treatments (Table 1). The order of remineralisation from the highest to the lowest was: (1) CPP-ACP/SnF2, (2) CPP-ACP, (3) SnF2 and (4) Placebo. Daily application of 60% CPP-ACP with and without SnF2 produced 36.61 ± 1.58% and 28.82 ± 1.53% remineralisation in the enamel subsurface lesions in situ respectively, significantly higher (p < 0.0001) than that for treatment by SnF2 alone (8.86 ± 0.71%) and placebo (2.30 ± 0.43%). Subsurface lesions treated with CPP-ACP/SnF2 showed 313% more remineralisation when compared with subsurface lesions treated with just SnF2 (P < 0.0001), and 27% more remineralisation than those treated with CPP-ACP ((P < 0.0001), highlighting the superior efficacy of CPP-ACP + SnF2 formulation in enhancing mineral deposition within demineralised dental tissues.
There were also significant differences (p < 0.001) in lesion depth changes (LDd – LDr, secondary outcome variable) following the treatments (Table 1). Subsurface lesions treated with CPP-ACP + SnF2 had significantly greater lesion depth reductions (LDd – LDr) than both SnF2 (P = 0.0054) and placebo (P = 0.0011). No significant difference in LDd – LDr was found between the subsurface lesions treated with CPP-ACP + SnF2 and CPP-ACP (P = 0.37). Furthermore, no significant difference was found between those treated with the SnF2 and placebo (P = 0.42). Hence, the order of efficacy was: CPP-ACP/SnF2 = CPP-ACP > SnF2 = Placebo.
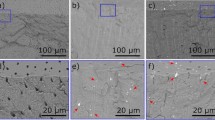
Dentine surface interaction and dental tubule occlusion
Human dentine specimens with exposed tubules were treated the same as the enamel slabs in situ and subsequently analysed using SEM. Representative SEM images of dentinal tubule occlusion after treatment of daily application of 60% CPP-ACP with and without SnF2 compared with SnF2 and placebo control are shown in Fig. 3. The data from enumeration of patent (not occluded) and partially occluded tubules in the dentine specimens for each of the four treatments is presented in Table 2. The three treatments SnF2, CPP-ACP and CPP-ACP/SnF2 all significantly reduced the number of open tubules compared with the placebo control. Patent tubules were not observed in the two CPP-ACP treatments with the combination of CPP-ACP and SnF2 providing the greatest reduction in numbers of partially occluded tubules. Visually the SEM examination provided further insights into the structural changes induced by the treatments. Treatment with 60% CPP-ACP + SnF2 demonstrated a surface covering with robust occlusion of dentinal tubules, indicative of substantial mineral infiltration and surface sealing. This suggests an effective barrier against further demineralisation and potential restoration of tooth integrity. Treatment with 60% CPP-ACP formulation without SnF2 also exhibited significant tubule occlusion, albeit to a slightly lesser extent compared to the combined CPP-ACP/SnF2 formulation. This underscores the intrinsic remineralising capacity of CPP-ACP in the absence of fluoride, albeit with potentially reduced effectiveness. Thus, SEM analysis of dentinal samples after each treatment showed that daily application of 60% CPP-ACP/SnF2 in situ produced superior dentinal tubule occlusion compared with SnF2 alone (Fig. 3; Table 2).
SEM images of dental tubule occlusions after daily application of 60% CPP-ACP formulations with and without SnF2 compared with SnF2 and placebo control. Images of representative regions were captured at 3000x magnification with a FEI ESEM Quanta 600 FEG in low vacuum mode using a solid-state backscattered electron detector at 10 kV, spot size 4.0.
Discussion
The results of this clinical in situ study demonstrates the efficacy of once daily application of high concentration (60%) CPP-ACP products for remineralisation of enamel subsurface lesions (WSLs) and occlusion of patent dentinal tubules.
Enamel subsurface lesion remineralisation
The enhanced remineralisation observed with daily single application of 60% CPP-ACP can be attributed to their unique ability to deliver bioavailable calcium and phosphate ions directly to the tooth surface. Casein phosphopeptides (CPP) stabilize amorphous calcium phosphate (ACP), preventing its precipitation and even in a high concentration form applied directly to the enamel surface the CPP still released calcium and phosphate ions in a controlled manner to produce substantial subsurface remineralisation while at the same time aesthetically masking the WSLs. These ions in the subsurface lesion promote the formation of hydroxyapatite and fluorhydroxyapatite within demineralised enamel and dentine lesions29.
To better understand the effect of the delivery mode of CPP-ACP, the level and rate of remineralisation achieved with the once per day direct application of the 60% CPP-ACP formulation was compared with a previous in situ clinical study46 of four times daily application of a 10% CPP-ACP tooth crème using a similar protocol (Table 3). A single daily application of 143 mg of CPP-ACP delivered in the 60% formulation produced a similar level of enamel subsurface lesion remineralisation in situ as four times daily application of 400 mg of CPP-ACP in a tooth crème (Table 3). This comparison demonstrates the substantial increase in remineralisation efficiency by targeted application of the remineralising high-concentration CPP-ACP technology directly to the WSL.
The inclusion of SnF2 in the 60% CPP-ACP formulation enhanced remineralisation of the enamel subsurface lesions in this clinical study. This result corroborates those of a previous study demonstrating a positive interaction between CPP-ACP and SnF2 when using a lower concentration CPP-ACP product30,31. SnF2 has been shown previously to enhance the uptake of fluoride ions into enamel, promoting the formation of fluorhydroxyapatite32,33. Fluoride is widely recognised for its anticariogenic properties in dental care34, and stannous ions (Sn2+) derived from SnF2 offer additional benefits for periodontal health as well as for caries, erosion and sensitivity prevention35. However, the efficacy of SnF2 in dentifrices hinges on its stabilisation to counteract challenges such as Sn2+ complexation and oxidative degradation over time36. Historically, sodium fluoride (NaF) and sodium monofluorophosphate (NaMFP) have been favoured in dentifrices due to the inherent instability associated with SnF2. Recent advances in stabilisation technologies have enabled the development of SnF2-containing dentifrices that exhibit enhanced clinical effectiveness, notably through increased bioavailability of Sn2+ ions.30,31 Interestingly, it has been recently demonstrated that the casein phosphopeptides (CPP) of the CPP-ACP nanotechnology are very effective at stabilising stannous ions and delivering them intra-orally with full bioactivity to significantly remineralise and harden softened enamel30,31.
The synergistic action of CPP-ACP and SnF2 in this study underscores their complementary roles in promoting effective remineralisation. CPP-ACP provides the necessary calcium and phosphate ions for crystal growth in the subsurface lesion37, while SnF2 enhances the delivery, uptake and retention of these ions through increased cross-linking and stability of CPP-ACP nanocomplexes30, leading to accelerated enamel subsurface lesion remineralisation and increased lesion remineralisation percentages (%R) as observed in this current clinical study.
Dentinal occlusion
The significant occlusion of exposed dentinal tubules by both high concentration CPP-ACP formulations under SEM was unsurprising given the surface visual effect produced with 60% CPP-ACP which completely masked the WSLs (Fig. 1). The addition of SnF2 to the 60% CPP-ACP formulation would be expected to enhance dentinal occlusion in a similar way to the mechanism of enhanced enamel subsurface remineralisation as described above and in other recent publications30,31.
The SEM findings of effective tubule occlusion are crucial in clinical practice, as open dentinal tubules are pathways for external stimuli to reach the pulp, causing pain and discomfort. By occluding these tubules with reparative dentine, CPP-ACP formulations can effectively reduce sensitivity and improve patient comfort38. Furthermore, the preventive potential of these treatments in inhibiting further tubule exposure by creating a protective barrier against demineralisation and abrasion highlights their potential long-term benefits in dental health maintenance.
Dentine hypersensitivity, characterized by sharp, transient pain in response to external stimuli, poses a significant challenge in dental practice and impacts the quality of life of affected individuals. It arises from the exposure of dentinal tubules, which transmit external stimuli to the nerve endings within the dental pulp39. Various factors, including gingival recession, enamel erosion, and periodontal diseases, contribute to dentine tubule exposure, exacerbating sensitivity40. Over the years, researchers and clinicians have focused on developing strategies to alleviate dentine hypersensitivity by occluding or sealing the exposed dentinal tubules. These efforts aim to block the passage of external stimuli to the nerve endings, thereby reducing or eliminating sensitivity. Hence the effective occlusion of dentinal tubules by once per day application of the 60% CPP-ACP formulation in situ as demonstrated in this current clinical study may offer a promising strategy for long-term relief from tooth sensitivity.
Clinical relevance
These findings may have significant implications for clinical practice, particularly in the management of incipient dental caries, erosion and dentinal hypersensitivity. Dental caries, characterised by demineralisation of enamel and dentine, can be effectively managed and even reversed in its early stages by promoting remineralisation. High concentration CPP-ACP formulations, especially when combined with SnF2, offer an innovative and non-invasive therapeutic/preventive option for masking and remineralising subsurface lesions. The ability of these formulations to deliver bioactive ions into the body of subsurface lesions as demonstrated by TMR and onto the surface of exposed dentine as demonstrated by SEM in our in situ study, supports their role in remineralising enamel WSLs and sealing exposed dentinal tubules to reduce dentinal hypersensitivity41,42.
Conclusion
In conclusion, this study underscores the substantial potential of high concentration (60%) CPP-ACP formulations, particularly in combination with SnF2, for treating enamel subsurface lesions through effective remineralisation and dentinal tubule occlusion. The synergistic effects observed in our study resulted in significant remineralisation and superior clinical outcomes compared to treatments with SnF2 alone or placebo control. These findings emphasise the potential clinical relevance of CPP-ACP/SnF2 formulations in enhancing dental health outcomes by promoting remineralisation and reducing dentinal hypersensitivity. Based on these in situ results a larger in vivo clinical trial of the technology is warranted to confirm efficacy of remineralisation of peri-bracket white spot lesions post-orthodontic therapy.
Materials and methods
Human ethics approval and participant recruitment
The study was approved by the University of Melbourne Human Research Ethics Committee (Ethics ID No. 14357) and was registered with the Australian New Zealand Clinical Trial Registry (Registration No. ACTRN12621000591853, Date registered 18/05/2021). All methods were performed in accordance with the relevant guidelines and regulations. Healthy participants were recruited from staff and students at the University of Melbourne and informed consent was obtained from all the participants. This was provided in writing prior to participation in the study. The study commenced on 31/05/2021 and the final treatment period ended on 16/08/2021. Study inclusion criteria were: males and females, aged 18 to 75 years; at least 22 natural teeth; stimulated whole salivary flow rate ≥ 1.0 ml/minute and unstimulated whole salivary flow rate ≥ 0.2 ml/minute. Study exclusion criteria were: current use of antibiotics or medications that affect salivary flow rates; history of severe oral disease; pregnancy, planned to become pregnant or lactating during the study period; existing dental work which would prevent the participant wearing the trial appliance (such as crowns, orthodontic appliances or removable dentures); treatment with antibiotics or anti-inflammatory medicines in the month prior to starting the study; history of allergic or other adverse reactions to milk, milk product or tin.
Sample size calculations
Four healthy participants were recruited for this study. The required sample size was calculated using a repeated measured ANOVA model with G*Power 3.143 using estimates from previous studies and predicted amounts of remineralisation following use of the 60% CPP-ACP formulation based on in vitro studies. Assuming a 90% probability of detecting a true significant difference between the effects of the four treatments (power) and, conversely, a α = 5% probability of falsely detecting a difference, a correlation coefficient (ρ) of 0.7 and a non-sphericity correction (ε) of 0.5, an effect size of 2.89 and a sample size of three were calculated. The effect size is the smallest detectable difference, Δ, between any pair of treatment means, and is given as multiples of the error standard deviation, σ. To compensate for errors in estimates of the standard deviations and potential participant attrition, a sample size of four was deemed sufficient for the purposes of this study.
Study design and test products
This randomised controlled study used a double-blind, four-way crossover design to assess the effects of three formulations and a placebo treatment to remineralise white spots on enamel surfaces and occlude patent dentinal tubules on dentine surfaces using an intra-oral remineralisation model. The treatments were:
A: 60% (w/w) CPP-ACP at pH 7.0 and 1100 ppm fluoride as SnF2,
B: 60% (w/w) CPP-ACP at pH 7.0 and no fluoride,
C: 1100 ppm fluoride as SnF2 at pH 4.0,
D: Placebo.
The formulations were prepared by the research team and stored in a secure refrigerator in the research department at 4 °C.
Participants were randomly allocated to each of the four treatment sequences: ABDC, BCAD, CDBA and DACB (Fig. 4) by the trial statistician (GGA). These sequences were based on a size 4 Williams (1949) design44 and ensured that each experimental product followed the other experimental products the same number of times, thus allowing any carry-over effects to be balanced. During each 14 consecutive-day treatment period, participants wore a palatal appliance for 24 h a day. The participants rested from the study for one week between each treatment period (washout period) (Fig. 5).
Intra-oral appliances and enamel subsurface lesions
A palatal appliance for each participant was prepared by taking alginate impressions of upper and lower dental arches from which study models were produced and articulated as described in previous studies45. Removable palatal acrylic appliances covering the first premolars to the last tooth in the arch were fabricated for each participant. The palatal appliance consisted of a palatal plate that was retained in the mouth by four stainless steel clasps. Troughs on each side of the palatal appliance adjacent to the palatal surface of maxillary premolar/molar teeth each accommodated two pre-sterilised enamel half-slabs containing demineralised subsurface lesions and one pre-sterilised dentine half-slab. Therefore, each appliance contained four enamel half-slabs and two dentine half-slabs.
Extracted third molars were obtained from oral surgeons and general practitioners in private practice. Any attached soft tissues were removed, and the teeth were stored in 10% (v/v) neutral buffered formalin at room temperature for at least two weeks. Enamel slabs were cut and subsurface lesions created as described in previous studies46,47. Dentine slabs were prepared by sawing dentine from the root surfaces of pre-sterilised extracted teeth. The slabs were then be immersed in 15% (w/v) EDTA for two minutes to remove the smear layer and then rinsed thoroughly with MilliQ™ water for five seconds and blotted dry. The slabs were then cut into two 4 × 4 mm half-slabs (test half-slab and control half-slab).
One half of each enamel and dentine slab was retained as the demineralisation control (control half-slab) and stored in labelled 0.5 mL microcentrifuge tubes together with a drop of MilliQ™ water, thereby creating a humidified environment. The other half of the enamel and dentine slabs (test half-slab) was inset into the intraoral appliance using dental wax for the remineralisation protocol. Each appliance contained four enamel half-slabs and two dentine test half-slabs. Care was taken not to cover the artificial lesions with wax. The enamel and dentine test half-slabs were removed and replaced with new pre-sterilised enamel and dentine half-slabs at the beginning of every new treatment period, thus bringing the total number of enamel and dentine half-slabs used in this study to 64 and 32, respectively. After every treatment period each test enamel half-slab was then paired with its control half-slab and then processed for microradiography and image analysis. Similarly, after each treatment period, the dentine test half-slabs were also paired with their control half-slabs and processed for SEM. Figure 6 summarises the steps in the processing of the appliances.
In situ study protocol
Participants wore their appliances for 24 h a day for each of four 14 consecutive-day treatment periods. There was a one-week washout period between each treatment period during which time participants rested from the study. Participants only removed their appliances when eating, drinking (except water), brushing their teeth, cleaning their appliances, participating in sporting activities, and when the formulations were applied to the surfaces of the enamel and dentine slabs on their appliance once each day.
Participants presented to the research department once on each weekday during the four two-week treatment periods where they were allocated to treatments. The research team painted the formulation allocated to that participant for that treatment period on the surface of the enamel and dentine slabs on their appliance, with the appliance out of the mouth. At the same time, the research team heated the film painted on the slabs by shining a curing light used in dental practice to the surface for 40 s with the appliance still out of the mouth. The slabs were allowed to cool to body temperature before the research team gave the appliance back to the participant who then immediately inserted their appliance into the mouth.
On Fridays during these treatment periods, the research team gave each participant enough formulation allocated to the participant for that treatment period for the participant to apply to the enamel and dentine slabs on their appliances once a day at home during the subsequent weekend. On these Fridays the research team also provided participants with microbrushes used in clinical dental practice to apply the formulations to the slabs. On weekends participants stored the formulations in a refrigerator at home when not being used. The research team instructed the participants how to paint the formulation on the slabs at home over the weekend. Once a day on these weekends, participants removed a tube containing the allocated formulation from the refrigerator and allowed it to warm to room temperature. They then removed their appliance, briefly rinsed the slabs with MilliQ™ water, and then gently painted all the formulation in the tube onto the surfaces of each of the enamel and dentine slabs with the microbrush over a 30 s period. No more than 1 mL of formulation was painted on all six slabs each day. After the formulation was applied, participants inserted the appliance in their mouths again and were instructed not to drink or eat while wearing the appliance in the mouth for the following 40 min.
During the entire study period (treatment and washout periods), participants cleaned their teeth once in the morning and once at night using a 1450 ppm fluoride toothpaste and toothbrush (both supplied). During the entire study period, participants otherwise continued with normal oral hygiene practices such as using floss or interdental sticks/brushes (with their appliance out of the mouth) but were requested not to rinse their mouths with any mouthwash solutions during the treatment periods.
Participants cleaned their appliance once in the morning and once at night. They were instructed to gently brush both surfaces of the appliances with a fluoride-free toothpaste and toothbrush (both supplied) but avoid brushing the troughs containing the enamel and dentine slabs. They were then instructed to gently rinse the two surfaces of the appliance including the trough areas with the enamel and dentine slabs with MilliQ™ water (supplied). Participants stored their appliances, when not being worn, at room temperature in a sealed plastic bag with a few drops of MilliQ™ water (both supplied).
Participants rested for at least one week between treatment periods during which time the enamel and dentine slabs on the appliances were replaced with new pre-sterilised enamel and dentine slabs. They repeated the exercise with a different treatment during each treatment period so that each participant completed the four treatments.
The participants returned to the clinical site with their appliances, and diary at the conclusion of each 14-day treatment period. After each treatment period each enamel test half-slab was paired with its control half-slab and embedded, sectioned and analysed by transverse microradiography to determine mineral content as described previously46. Likewise, at the end of the treatment period, each dentine test half-slab and its control half slab were then desiccated with silica gel for 72 h and then mounted on sample holders, gold sputter-coated (2 nm), and examined with an Everhart-Thornley detector in a FEI Quanta FEG 200 scanning electron microscope at 10 kV under high vacuum (Bio21 Advanced Microscopy Facility, Victoria, Australia). Using the scanning electron microscope, each dentine test half-slab and its paired control half-slab were examined for qualitative and quantitative differences in the degree of occlusion of the exposed dentinal tubules. Tubules that could be observed as patent (not occluded) or partially occluded were enumerated and expressed per mm2. Trial staff involved in the analysis of the TMR images of the enamel blocks and the SEM of the dentine blocks were blinded to the allocated treatment.
Data analysis and statistical considerations
The primary analysis set was all participants who completed the trial without significant protocol violations. The identification of which participants were excluded for significant protocol variations and which enamel/dentine samples were unable to be processed was done during the blind review of the data, prior to the treatment code being broken.
The percent mineral profile of each enamel slab’s demineralised and remineralised lesions was compared with the median sound enamel percent mineral profile of the same section. The difference between the areas under the densitometric profile of the demineralised lesion and the median sound enamel, calculated by trapezoidal integration, is represented by ΔZd. The difference between the areas under the densitometric profile of the remineralised lesion and the median sound enamel, calculated by trapezoidal integration, is represented by ΔZr. The primary outcome measure from the microradiography was the percentage change in mineral content values relative to the baseline, %R, calculated as
Descriptive statistics (mean, standard deviation and range) was calculated for all continuous outcome variables and frequencies for all qualitative variables and tabulated by treatment. The experimental unit was the participant. The outcome measures were determined for each participant-treatment combination and the resultant values averaged by treatment. The primary and secondary outcome measures were compared across treatments using a repeated measures analysis of variance with factors for treatment, treatment period and participant. Also, initial mineral loss (ΔZd) was included as a covariate in the analysis of variance model for mineral content change (ΔZd-ΔZr). Post hoc comparisons of treatment differences were performed on the marginal means using the Sidak adjustment for multiple comparisons. Assumptions for the models chosen were checked using standardised residual and normal probability plots. The Stata command, robvar, a robust test for equality of variances, was used to check the homogeneity of variance assumption. All statistical tests were two-sided. The Kruskal-Wallis test in IBM SPSS Statistics (version 30, IBM Corp, Armonk, NY, USA) was used for the comparison of patent tubules between groups, with a Bonferroni adjustment used post hoc comparisons of treatment differences. All other analyses were conducted using Stata/MP 18.0 (StataCorp LLC, College Station, TX, USA) statistical software.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Selwitz, R. H., Ismail, A. I. & Pitts, N. B. Dental caries. Lancet 369, 51–59. https://doi.org/10.1016/S0140-6736(07)60031-2 (2007).
Uribe, S. E., Innes, N. & Maldupa, I. The global prevalence of early childhood caries: A systematic review with meta-analysis using the WHO diagnostic criteria. Int. J. Paediatr. Dent. 31, 817–830. https://doi.org/10.1111/ipd.12783 (2021).
Bailey, D. L. et al. Regression of post-orthodontic lesions by a remineralizing cream. J. Dent. Res. 88, 1148–1153. https://doi.org/10.1177/0022034509347168 (2009).
Sundararaj, D., Venkatachalapathy, S., Tandon, A. & Pereira, A. Critical evaluation of incidence and prevalence of white spot lesions during fixed orthodontic appliance treatment: A meta-analysis. J. Int. Soc. Prev. Community Dent. 5, 433–439. https://doi.org/10.4103/2231-0762.167719 (2015).
Fejerskov, O., Kidd, E. & Nyvad, B. Dental Caries: the Disease and its Clinical Management (Wiley, 2015).
Xiao, Z. H. et al. Rapid biomimetic remineralization of the demineralized enamel surface using nano-particles of amorphous calcium phosphate guided by chimaeric peptides. Dent. Mater. 33, 1217–1228. https://doi.org/10.1016/j.dental.2017.07.015 (2017).
Dorozhkin, S. V. Nanosized and nanocrystalline calcium orthophosphates. Acta Biomater. 6, 715–734. https://doi.org/10.1016/j.actbio.2009.10.031 (2010).
Andersson, A., Skold-Larsson, K., Hallgren, A., Petersson, L. G. & Twetman, S. Effect of a dental cream containing amorphous cream phosphate complexes on white spot lesion regression assessed by laser fluorescence. Oral Health Prev. Dent. 5, 229–233 (2007).
Shen, P. et al. Importance of bioavailable calcium in fluoride dentifrices for enamel remineralization. J. Dent. 78, 59–64. https://doi.org/10.1016/j.jdent.2018.08.005 (2018).
Alqahtani, S., Abusaq, A., Alghamdi, M., Shokair, N. & Albounni, R. Colour stability of resin infiltrated white spot lesion after exposure to stain-causing drinks. Saudi J. Biol. Sci. 29, 1079–1084. https://doi.org/10.1016/j.sjbs.2021.09.063 (2022).
Morgan, M. V. et al. The anticariogenic effect of sugar-free gum containing CPP-ACP nanocomplexes on approximal caries determined using digital bitewing radiography. Caries Res. 42, 171–184. https://doi.org/10.1159/000128561 (2008).
Degli Esposti, L. et al. Composite materials of amorphous calcium phosphate and bioactive glass nanoparticles for preventive dentistry. Ceram. Int. 50, 593–602. https://doi.org/10.1016/j.ceramint.2023.10.137 (2024).
Bartlett, J. D. Dental enamel development: proteinases and their enamel matrix substrates. ISRN Dent. 2013 (684607). https://doi.org/10.1155/2013/684607 (2013).
Bakdach, W. M. M. & Hadad, R. Effectiveness of different adjunctive interventions in the management of orthodontically induced white spot lesions: A systematic review of systematic reviews and meta-analyses. Dent. Med. Probl. 57, 305–325. https://doi.org/10.17219/dmp/118330 (2020).
Rajendran, R. et al. Effect of remineralization agents on white spot lesions: A systematic review. J. Pharm. Bioallied Sci. 14, S7–S12. https://doi.org/10.4103/jpbs.jpbs_836_21 (2022).
Reynolds, E. C. et al. Fluoride and casein phosphopeptide-amorphous calcium phosphate. J. Dent. Res. 87, 344–348. https://doi.org/10.1177/154405910808700420 (2008).
Reynolds, E. C. Casein phosphopeptide-amorphous calcium phosphate: the scientific evidence. Adv. Dent. Res. 21, 25–29. https://doi.org/10.1177/0895937409335619 (2009).
Robertson, M. A. et al. MI paste plus to prevent demineralization in orthodontic patients: a prospective randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 140, 660–668. https://doi.org/10.1016/j.ajodo.2010.10.025 (2011).
Rahmath Meeral, P., Doraikannan, S. & Indiran, M. A. Efficiency of casein phosphopeptide amorphous calcium phosphate versus topical fluorides on remineralizing early enamel carious lesions - A systematic review and meta analysis. Saudi Dent. J. 36, 521–527. https://doi.org/10.1016/j.sdentj.2024.01.014 (2024).
Singal, K. et al. Effectiveness-of calcium phosphate derivative agents on the prevention and remineralization of caries among children- A systematic review & meta-analysis of randomized controlled trials. J. Evid. Based Dent. Pract. 22, 101746. https://doi.org/10.1016/j.jebdp.2022.101746 (2022).
Imani, M. M. et al. Efficacy of CPP-ACP and CPP-ACPF for prevention and remineralization of white spot lesions in orthodontic patients: a systematic review of randomized controlled clinical trials. Acta Inf. Med. 27, 199–204. https://doi.org/10.5455/aim.2019.27.199-204 (2019).
Fernando, J. R. et al. Comparison of calcium-based technologies to remineralise enamel subsurface lesions using microradiography and microhardness. Sci. Rep. 12, 9888. https://doi.org/10.1038/s41598-022-13905-8 (2022).
Bartold, P. M. Dentinal hypersensitivity: a review. Aust. Dent. J. (2006).
Gillam, D. G. & Orchardson, R. Advances in the treatment of root dentine sensitivity: mechanisms and treatment principles. Endo Topic. 13, 13–33 (2006).
Mantzourani, M. & Sharma, D. Dentine sensitivity: past, present and future. J. Dent. 41 (Suppl 4), 3–17. https://doi.org/10.1016/S0300-5712(13)70002-2 (2013).
Mathew, M. G. et al. Efficacy of remineralizing agents to occlude dentinal tubules in primary teeth subjected to dentin hypersensitivity in vitro: SEM study. J. Family Med. Prim. Care. 9, 354–358. https://doi.org/10.4103/jfmpc.jfmpc_853_19 (2020).
Shah, R. & Bajaj, M. Comparative analysis of CPP-ACP, tricalcium phosphate, and hydroxyapatite on assessment of dentinal tubule occlusion on primary enamel using SEM: an in vitro study. Int. J. Clin. Pediatr. Dent. 12, 371–374. https://doi.org/10.5005/jp-journals-10005-1680 (2019).
Mahesuti, A., Duan, Y. L., Wang, G., Cheng, X. R. & Matis, B. A. Short-term efficacy of agents containing KNO3 or CPP-ACP in treatment of dentin hypersensitivity. Chin. J. Dent. Res. 17, 43–47 (2014).
Reynolds, E. C. Remineralization of enamel subsurface lesions by casein phosphopeptide-stabilized calcium phosphate solutions. J. Dent. Res. 76, 1587–1595. https://doi.org/10.1177/00220345970760091101 (1997).
Fernando, J. R. et al. Self-assembly of dental surface nanofilaments and remineralisation by SnF2 and CPP-ACP nanocomplexes. Sci. Rep. 9, 1285. https://doi.org/10.1038/s41598-018-37580-w (2019).
Fernando, J. R. et al. Remineralisation of enamel and dentine with stabilised stannous fluoride dentifrices in a randomised cross-over in situ trial. J. Dent. 143, 104895. https://doi.org/10.1016/j.jdent.2024.104895 (2024).
Ganss, C., Schlueter, N., Hardt, M., von Hinckeldey, J. & Klimek, J. Effects of toothbrushing on eroded dentine. Eur. J. Oral Sci. 115, 390–396. https://doi.org/10.1111/j.1600-0722.2007.00466.x (2007).
Ten Cate, J. M. Fluorides in caries prevention and control: empiricism or science. Caries Res. 38, 254–257. https://doi.org/10.1159/000077763 (2004).
Wong, M. C. et al. Cochrane reviews on the benefits/risks of fluoride toothpastes. J. Dent. Res. 90, 573–579. https://doi.org/10.1177/0022034510393346 (2011).
Clark-Perry, D. & Levin, L. Comparison of new formulas of stannous fluoride toothpastes with other commercially available fluoridated toothpastes: A systematic review and meta-analysis of randomised controlled trials. Int. Dent. J. 70, 418–426. https://doi.org/10.1111/idj.12588 (2020).
White, D. J. A return to stannous fluoride dentifrices. J. Clin. Dent. 6, 29–36 (1995).
Sudjalim, T. R., Woods, M. G., Manton, D. J. & Reynolds, E. C. Prevention of demineralization around orthodontic brackets in vitro. Am. J. Orthod. Dentofac. Orthop. 131, 705e701–705e709. https://doi.org/10.1016/j.ajodo.2006.09.043 (2007).
Yassin, O. & Milly, H. Effect of CPP-ACP on efficacy and postoperative sensitivity associated with at-home vital tooth bleaching using 20% carbamide peroxide. Clin. Oral Investig. 23, 1555–1559. https://doi.org/10.1007/s00784-018-2574-z (2019).
Addy, M. Dentine hypersensitivity: new perspectives on an old problem. Int. Dent. J. 52 (5), 367–375 (2002).
Haneet, R. K. & Vandana, L. K. Prevalence of dentinal hypersensitivity and study of associated factors: a cross-sectional study based on the general dental population of davangere, karnataka, India. Int. Dent. J. 66, 49–57. https://doi.org/10.1111/idj.12206 (2016).
Cochrane, N. J., Cai, F., Huq, N. L., Burrow, M. F. & Reynolds, E. C. New approaches to enhanced remineralization of tooth enamel. J. Dent. Res. 89, 1187–1197. https://doi.org/10.1177/0022034510376046 (2010).
Konradsson, K. et al. Stabilized stannous fluoride dentifrice in relation to dental caries, dental erosion and dentin hypersensitivity: A systematic review. Am. J. Dent. 33, 95–105 (2020).
Faul, F., Erdfelder, E., Lang, A. G. & Buchner, A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods. 39, 175–191. https://doi.org/10.3758/bf03193146 (2007).
Williams, E. J. Experimental design balanced for the Estimation of residual effects of treatments. Aust J. Sci. Res. A. 2, 149–168 (1949).
Iijima, Y. et al. Acid resistance of enamel subsurface lesions remineralized by a sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phosphate. Caries Res. 38, 551–556. https://doi.org/10.1159/000080585 (2004).
Shen, P. et al. Effect of added calcium phosphate on enamel remineralization by fluoride in a randomized controlled in situ trial. J. Dent. 39, 518–525. https://doi.org/10.1016/j.jdent.2011.05.002 (2011).
Cochrane, N. J. et al. Remineralisation by chewing sugar-free gums in a randomised, controlled in situ trial including dietary intake and gauze to promote plaque formation. Caries Res. 46, 147–155. https://doi.org/10.1159/000337240 (2012).
Acknowledgements
This work was supported by a competitive grant from the Australian National Health and Medical Research Council #2000088 to ECR.
Author information
Authors and Affiliations
Contributions
P.S., J.R.F. and E.C.R. conceived and designed the study. J.R.F. collected the clinical data. Y.Y., C.R. supervised the in situ component. Y.Y. created the in situ appliances. Y.Y., C.R. prepared the enamel and dentine blocks, processed the blocks and obtained the TMR images of the enamel blocks. P.S. analysed the TMR images of the enamel blocks. J.R.F. performed the S.E.M. analysis of the dentine blocks. G.G.A. and P.S. conducted data analyses. E.C.R. supervised the study. P.S., J.R.F., G.G.A. E.C.R. wrote the manuscript, which all authors edited and approved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shen, P., Fernando, J.R., Yuan, Y. et al. Efficient enamel subsurface lesion remineralisation and dentine tubule occlusion by high concentration CPP-ACP: a randomised, cross-over in situ study. Sci Rep 15, 28263 (2025). https://doi.org/10.1038/s41598-025-14005-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-14005-z