Abstract
In recent years, antibody-drug conjugates have become clinically significant in oncology therapeutics. Results from the POLARIX trial revealed that polatuzumab vedotin in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone (Pola-R-CHP) versus rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) reported a 7.7% improvement in the 3-year progression-free survival (PFS), with no difference in overall survival (OS). This study aimed to assess the cost-effectiveness of polatuzumab vedotin in the first-line treatment of diffuse large B-cell lymphoma (DLBCL) from the perspective of the Chinese healthcare system. We constructed a 3-state partitioned survival model and a 10-year horizon to estimate the cost and utility associated with DLBCL treatment. The survival data, direct medical costs, and utilities were obtained from the POLARIX trial, YAOZHI database, and published literature. The outputs of the model include total costs, quality-adjusted life-years (QALYs), and incremental cost-effectiveness ratios (ICERs). Uncertainty was explored through one-way, probabilistic sensitivity and scenario analyses. Over a 10-year horizon, Pola-R-CHP provided an additional 0.29 QALYs versus R-CHOP, while incurring incremental costs of $31,804 and an ICER of $110,594/QALY. One-way sensitivity analysis suggested that the model was most sensitive to the utility of PFS and the cost of polatuzumab vedotin. Probabilistic sensitivity analysis showed that at the willingness-to-pay (WTP) threshold ($38,043), Pola-R-CHP was not considered cost-effective. Scenario analyses indicated that Pola-R-CHP could be a cost-effective therapeutic alternative for patients achieving long-term survival. The threshold analysis demonstrated that a 61% price reduction for polatuzumab vedotin would achieve cost-effectiveness at the WTP threshold. In the first-line treatment of DLBCL, Pola-R-CHP provides an additional health benefit over R-CHOP, but is unlikely to be cost-effective at currently published prices.
Similar content being viewed by others
Introduction
DLBCL is an aggressive lymphoma, accounting for approximately 30% of non-Hodgkin lymphomas (NHL)1. Approximately 150,000 people worldwide are estimated to be diagnosed with DLBCL each year2. According to the Global Burden of Diseases, Injuries, and Risk Factors Study 2019, the number and age-standardized rate of disability-adjusted life-years (DALYs) attributable to NHL are 6,991,329 and 90.36, respectively, while the age-standardized incidence and mortality rates per 100,000 population are 5.91 and 3.29, respectively3. Based on the Burden of Lymphoma in China 2019, there were an estimated 91,954 new cases and 44,310 deaths due to NHL4. R-CHOP has been the unshakeable gold standard for the treatment of untreated DLBCL; even after this standard treatment, approximately 30%~40% of patients will still relapse and progress5,6. Improving the efficacy of first-line therapy for patients with DLBCL is a current research hotspot. Currently, there are limited treatment options for patients who are insensitive to second-line therapies. Once the disease relapses, it progresses rapidly and affects various tissues and organs. Unfortunately, none of the new drugs introduced in previous studies have achieved positive results7,8,9. Therefore, new and innovative treatments are urgently needed.
Polatuzumab vedotin is an antibody-drug conjugate that selectively acts on CD79b in B-cell receptors and releases the small molecule cytotoxic drug monomethyl auristatin E (MMAE). Polatuzumab vedotin binds to CD79b and releases MMAE through an endocytosis mechanism, which binds to microtubules and kills dividing cells by inhibiting cell division and inducing apoptosis10. Polatuzumab vedotin has shown favorable efficacy and manageable toxicity as a single agent or in combination for the treatment of relapsed/refractory DLBCL in several previous studies11,12,13. In a phase 1b-2 trial, polatuzumab vedotin was used as the first-line treatment for DLBCL, with 89% of patients achieving an overall response with a manageable safety profile14. Based on the results of the POLARIX study (NCT03274492), which showed a 6.5% improvement in the 2-year progression-free survival (PFS), with no difference in overall survival (OS) or side effects, Pola-R-CHP was approved for use in patients with previously untreated DLCBL15. Polatuzumab vedotin was launched in China on January 10, 2023; however, the drug is currently not in the health insurance catalog and can only be paid for by patients, which means that patients need to bear a huge financial burden. To our knowledge, its cost-effectiveness has not been evaluated in China. The healthcare resources of China are scarce compared to those of developed countries; thus, economic evaluation is important to help clinicians and policy makers optimize resource allocation.
The objective of our study was to estimate the cost-effectiveness of Pola-R-CHP as a first-line treatment for DLCBL patients on the basis of the POLARIX trial under the Chinese healthcare system.
Methods
Study populations and interventions
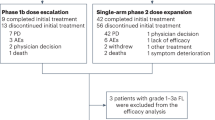
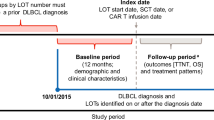
This study complied with the updated Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) guidelines (Supplementary Table 1). The POLARIX trial is an international phase 3 trial with 216 locations. The patient model was consistent with the POLARIX trial patients, where 879 patients with previously untreated DLBCL were randomly assigned to receive pola-R-CHP (n = 440) and R-CHOP (n = 439). The baseline demographic and disease characteristics were comparable between groups, as detailed in Supplementary Table 2. Eight 21-day cycles of treatment were planned. In the first six cycles, the patients received either pola-R-CHP or R-CHOP. All the patients received cyclophosphamide (750 mg per square meter), doxorubicin (50 mg per square meter) and oral prednisone at a dose of 100 mg once daily on days 1 through 5 of each of the first six cycles. The difference between the two groups was that the pola-R-CHP group received polatuzumab vedotin (1.8 mg per kilogram of body weight) and the R-CHOP group received vincristine at a dose of 1.4 mg per square meter of body-surface area (maximum of 2 mg), plus intravenous doses of rituximab (375 mg per square meter). During cycles 7 and 8, patients in both groups received rituximab monotherapy.
Model structure
The study developed a partitioned survival model in TreeAge Pro Software to compare the cost-effectiveness of Pola-R-CHP versus R-CHOP for untreated DLCBL under the Chinese healthcare system and consists of different health states: PFS, PD, and death (Fig. 1). Based on the updated POLARIX trial, which had a median follow-up of 39.7 months, the proportion of patients who survived was estimated by the area under the OS curve, and the proportion of patients who survived on PFS was estimated by the area under the PFS curve. With regard to the PD state, we calculated the proportion of the difference between the PFS and OS curves. IPDfromKM was used to extract the OS and PFS data from the curves16. R software was used for additional statistical analyses to identify the best-fitting parameter distributions of the survival curve from Weibull, Exponential, Gamma, Log-logistic distributions, based on the Akaike and Bayesian information criteria (AIC and BIC), as well as visual inspection (Supplementary Figs. 1 and Supplementary Table 3).
PD, progression disease; PFS, progression-free survival.
In this model, a 10-year horizon was used, and the cycle length was 3 weeks (21 days), which is consistent with the administration cycles of POLARIX. The results of the model were used to calculate the incremental cost-effectiveness ratio (ICER) for each strategy, which reflects the cost for each additional quality-adjusted life year (QALY) gained due to treatment in 2023 US dollars (1$=7.0467 CNY)17. Referring to the China Guidelines for Pharmacoeconomic Evaluations (2020), the WTP threshold ($38,043) was three times China’s per capita GDP ($12,681), and both costs and utilities were discounted at a rate of 5% annually18.
Costs
This analysis was conducted from the perspective of the Chinese healthcare system. The costs mainly included drug acquisition, prophylaxis against neutropenia, laboratory tests, radiographic examinations, pathologic diagnosis, AEs, subsequent treatment, and terminal care(Table 1). Drug prices were sourced from the YAOZHI Database (https://db.yaozh.com), which provides the most up-to-date pricing data across China19. Consistent with the POLARIX regimen, the dosage for Chinese patients was calculated based on a body surface area of approximately 1.72m2 and a body weight of 65 kg20.
Each group, the frequency of prophylaxis against neutropenia, laboratory work, and radiographic examinations were referred to the POLARIX trial and Chinese guidelines of hematological malignancies. The cost of the pathological examination was calculated only in the first cycle. The cost of adverse events only considered grade 3 and higher AEs with an incidence of ≥ 5% in the trial. AEs were assumed to occur in the first cycle and were calculated as a weighted average of the number of adverse reactions reported in clinical trial, including neutropenia, leukopenia, febrile neutropenia, anemia, platelet count decreased, and pneumonia.
Once the patient has progressed, subsequent treatment consistent with the study POLARIX showed that 22.5% of patients in the Pola-R-CHP arm and 30.3% of patients in the R-CHOP arm received ≥ 1 subsequent antilymphoma therapy. In the Pola-R-CHP group, 9.3% of patients received radiotherapy and 17.0% received systemic therapy. In the R-CHOP group, 13.0% of patients received radiotherapy and 23.5% received systemic therapy. Systemic therapies include autologous stem-cell transplantation(ASCT) and chimeric antigen receptor T-cell therapy (CAR-T). Terminal care costs were included as a once-off cost when entering a state of death21. We did not include costs of productivity losses. All of these costs were retrieved from previously published literature and local hospital22.
Utilities
Each health state was assigned a health utility preference between 0 and 1, where 0 represented death and 1 represented perfect health. Since the POLARIX trial did not disclose quality-of-life data, the National Institute of Health and Care Excellence (NICE) accepted source for DLBCL utilities from the GOYA trial, which had a longer follow up than POLARIX, and clinicians had confirmed that the GOYA utility values were more representative of DLBCL than the POLARIX utility values23. The PFS and PD utility values in the GOYA study were 0.82 and 0.74, respectively, using inverse propensity score weighting, which matched the utility values in the POLARIX study24. The disutility values for AEs were derived from published literature25,26,27.
Sensitivity analyses
Sensitivity analyses were conducted to evaluate the robustness of our model. One-way sensitivity analyses were conducted by varying the key model parameters to determine the impact on the ICER. The 95% CI was usually used to limit the range of the parameter, but if no 95% CI was available, ± 20% of the reference value was used as the value of the change. The discount rate in one-way analyses ranged from 0 to 8%. One-way sensitivity analyses were presented by a tornado diagram to show the impact of the different parameters variation on the ICER.
Probabilistic sensitivity analyses (PSA) were performed 1000 Monte Carlo simulations, each time randomly sampling from the prespecified distributions. Costs were distributed according to gamma distributions, and probabilities and utilities were distributed according to beta distributions. An ICER scatter plot and cost-effectiveness acceptability curve (CEAC) were generated to show the results of the PSA.
Scenario analyses
In addition to the sensitivity analyses, scenario analyses were conducted to test model assumptions. We performed several scenario analyses using different time horizons (15, 20 years) or decreased price by 50% of polatuzumab vedotin. We also used different utility estimates taken from the literature on patients with DLCBL for scenario analyses28. In the meantime, a scenario analysis was conducted under the assumption that the included population was Asian29.
Threshold analysis
A threshold analysis was used to estimate the price discount, i.e., how much polatuzumab vedotin would need to be reduced to meet the cost-effectiveness thresholds between one and three times the GDP per capita ($12,681 to $38,043).
Results
Base-case analyses
Compared with R-CHOP, Pola-R-CHP was associated with an incremental cost of $31,804 and an incremental QALYs of 0.29, with a resulting ICER of $110,594/QALY (Table 2). According to the base-case analysis, Pola-R-CHP was much higher than the specified WTP threshold ($38,043).
Sensitivity analyses
The one-way sensitivity analyses showed that the parameters with the largest impact on the ICERs were the utility of PFS, the cost of polatuzumab vedotin, the probability of pneumonia, and the utility of PD (Fig. 2). As the parameters varied between the lower and upper bounds, the ICER remained greater than the WTP threshold.
Results of PSA were presented as an ICER scatter plot and a CEAC (Fig. 3 ~ 4). According to the scatter plot, compared with R-CHOP, almost all scatter points of Pola-R-CHP were located in the north-east quadrant of the cost-effectiveness plane and above the WTP threshold. The CEAC revealed that, compared to R-CHOP, at a WTP threshold of approximately $105,031 per QALY, the probability of Pola-R-CHP being a cost-effective treatment was 50%.
Tornado diagrams of one-way sensitivity analyses of Pola-R-CHP vs. R-CHOP. Abbreviations: ICER, incremental cost-effectiveness ratios; PFS, progressionfree survival; PD, progressive disease; Pola-R-CHP, polatuzumab vedotin in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone; R-CHOP, rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone.
A probabilistic scatter plot of the ICER between Pola-R-CHP and R-CHOP. Abbreviations: WTP, willingness-to-pay; QALY, quality-adjusted life-year; Pola-R-CHP, polatuzumab vedotin in combination with rituximab, cyclophosphamide, doxorubicin, and prednisone; R-CHOP, rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone.
Scenario analyses
Scenario analyses showed large differences in possible ICERs. All scenarios produced ICERs lower than the base case estimate (Table 3). When the time horizon of the model was extended to 15 or 20 years, the ICER decreased significantly. Over the 20-year time horizon, ICERs declined considerably below the WTP threshold. When the price of polatuzumab vedotin was decreased by 50%, Pola-R-CHP resulted in the ICERs of $51,107. One of the scenarios used a different utility of DLCBL, resulted in a slightly lower ICER than the base case. In another scenario, we applied an analysis of survival data from the Asian subpopulation of the POLARIX trial, which resulted in an ICER of $47,105.
Threshold analysis
The threshold analysis demonstrated that a discounted polatuzumab vedotin price of 82%, from $1475.87 per 30 mg vial to $261.26, met the $12,681 per QALY threshold. A discounted price of 61% to $575.87 met the $38,043 per QALY threshold. Achieving cost-effectiveness at the given thresholds would require drug discounts of 82% and 61%, respectively.
Discussion
To our knowledge, this is the first cost-effectiveness study comparing Pola-R-CHP versus R-CHOP for the first-line treatment of DLCBL in China. In this study, we aimed to evaluate the cost-effectiveness of polatuzumab vedotin for DLCBL. Based on the result of the POLARIX clinical trial, we found that Pola-R-CHP has an incremental cost of $31,804 and incremental QALYs of 0.29, resulting in a base case ICER of $110,594 per QALY, which is well above the current WTP threshold for China. From the perspective of health services in China, the results of our study showed that polatuzumab vedotin was not cost effective for Chinese patients. The results of one-way sensitivity analyses and PSA were generally robust.
Although the ICERs for the scenario analyses were lower than those for the base analysis, only scenarios with a 20-year horizon were lower than the WTP threshold. In the scenario with a 15-year time horizon, Pola-R-CHP had an ICER of $38,640 per QALY, which was very close to the WTP threshold ($38,043). Scenario analyses indicate that Pola-R-CHP could be a cost-effective therapeutic alternative for patients achieving long-term survival. The NCCN-IPI showed markedly better 5-year OS in low-risk patients (96%) compared to high-risk patients (33%)30. However, in the subgroup analysis of the POLARIX study, pola-R-CHP demonstrated no clear PFS benefit in patient subgroups aged ≤ 60 years, with bulky disease, or with low IPI scores, and OS benefit was not reported. DLBCL patients who are alive without progression at 24 months from the onset of initial therapy have excellent survival, which is similar to the age- and sex-matched general population31,32. The updated data from the POLARIX study showed that PFS was better for Pola-R-CHP than for R-CHOP, implying improved quality of life for patients and a significant reduction in the overall treatment burden for DLBCL33. The Asian population appeared more likely to benefit than the global population, with incremental QALYs of 0.67 for Pola-R-CHP under this scenario.
We assumed that the price of polatuzumab vedotin would be lower. Brentuximab vedotin is a CD30-directed antibody and microtubule inhibitor conjugate indicated for the treatment of classical Hodgkin lymphoma and anaplastic large cell lymphoma34, and cut price by more than 50% in less than two years since it was first marketed in China. Considering the decrease in drug prices, we assumed that polatuzumab vedotin would drop in price by 50% in a short period of time, and we found a significant decrease in the ICER during scenario analysis. China has implemented combined medication price negotiation and mandatory reimbursement policies for targeted anti-cancer medications since 201735, which could further improve the accessibility and affordability of expensive anti-cancer targeted drugs by lowering the unit cost of the drugs and increasing the utilization rate, benefiting many patients. The results of the threshold analysis showed that Pola-R-CHP was cost-effective when the price reduction of polatuzumab vedotin reached 61%. This trend of price reductions for drugs was in line with the current Chinese health insurance policies, which led to a marked decrease in prices through price negotiations36.
Based on the pivotal data from the POLARIX study, more than 50 countries have approved Pola-R-CHP for the treatment of adult patients with previously untreated DLBCL, including China. A partitioned survival analysis model was developed in Japan under the public health insurance system, and the results showed that Pola-R-CHP was cost-effective with an ICER of ¥2,710,238/QALY, which was below the WTP threshold of ¥7.5 million per QALY28. One economic study under German perspective indicated that pola-R-CHP was a cost-effective treatment at a WTP of €80 000/QALY compared with R-CHOP, assuming a 5-year PFS of 69.6% for pola-R-CHP versus 62.6% for R-CHOP37. Another analysis in the United States concluded that pola-R-CHP was cost-effective at a WTP of $150,000/QALY from both a societal and payer perspectives24. This finding is consistent with the results of Japanese and German studies. These results are inconsistent with our conclusions. These studies used a mixture-cure model, which is different from our model. Since we have the relatively longer follow-up period, we did not use a mixture-cure model. In the US, the WTP threshold is not the per capita GDP. Perhaps differences in modeling and WTP across countries can explain our inconsistencies. New drugs that are cost-effective according to WTP standards in developed countries may exceed WTP thresholds in China or other developing countries, thereby challenging the generalizability of the results of cost-effectiveness studies.
The study by Vijenthira et al. (2023) indicated that Pola-R-CHP was not cost-effective from the perspective of US and Canadian payers38. Several factors in this study appeared to contribute to higher ICERs, most notably the high cost of second-line therapies including CAR-T and ASCT. Additionally, the cost of granulocyte colony-stimulating factor for prophylactic use was included.
A major strength of our analysis was that we used updated data from the phase III POLARIX study. To the best of our knowledge, this study had the longest follow-up of 39.7 months compared with other cost-effectiveness analyses, and no new safety signals were identified. In addition, some of the scenario analysis results were very close to the WTP, which may provide ideas for polatuzumab vedotin to win the Chinese market. For polatuzumab vedotin, price reduction may represent an effective short-term strategy to rapidly gain market share. Furthermore, the subsequent treatment in our study was consistent with the POLARIX trial, which had a lower proportion of patients receiving CAR-T and ASCT. This proportion was in line with the trend of Chinese patients choosing post-relapse treatment options. At the time of the study’s primary analysis, CAR-T was commercially unavailable in China and not broadly available in other regions of Asia. Currently, both ASCT and CAR-T are available in China. However, their high prices greatly limit their use, especially for CAR-T, which costs nearly $170,000.
There are several limitations that need to be noted in this study. First, the utility of PFS and PD was retrieved from the literature, which may have led to deviations in our conclusion. Second, all patients enrolled in the POLARIX trial were from all over the world and therefore may have some individual differences, such as racial differences, from the Chinese patients. Third, an immaturity of the follow-up data from the trial required extrapolation, which introduces uncertainty about the long-term outcomes. Although this study has the longest published follow-up, the results of the long-term outcomes are still immature. Future studies with longer trial follow-up and more mature survival data may help to confirm the longer-term cost benefits of polatuzumab vedotin. Fourth, not all adverse reactions were included in the model, and we only considered adverse reactions of grade 3 or higher. Therefore, we may have overestimated the advantages and underestimated the costs.
Conclusion
In summary, the results of this cost-effectiveness model indicated that Pola-R-CHP was not a cost-effective option in China at currently published prices, when compared with R-CHOP for previously untreated DLBCL at a WTP threshold of $38,043 per QALY.
Data availability
The data presented in this study are available on request from the corresponding author.
References
Al-Hamadani, M. et al. Non-Hodgkin lymphoma subtype distribution, geodemographic patterns, and survival in the US: A longitudinal analysis of the National cancer data base from 1998 to 2011. Am. J. Hematol. 90, 790–795 (2015).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Diseases, G. B. D. & Injuries, C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396, 1204–1222 (2020).
Liu, W. et al. Burden of lymphoma in china, 1990–2019: an analysis of the global burden of diseases, injuries, and risk factors study 2019. Aging (Albany NY). 14, 3175–3190 (2022).
Coiffier, B. et al. Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the groupe d’etudes des lymphomes de l’adulte. Blood 116, 2040–2045 (2010).
Sehn, L. H. et al. The revised international prognostic index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood 109, 1857–1861 (2007).
Leonard, J. P. et al. Randomized phase II study of R-CHOP with or without bortezomib in previously untreated patients with Non-Germinal center B-Cell-Like diffuse large B-Cell lymphoma. J. Clin. Oncol. 35, 3538–3546 (2017).
Younes, A. et al. Randomized phase III trial of ibrutinib and rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone in Non-Germinal center B-Cell diffuse large B-Cell lymphoma. J. Clin. Oncol. 37, 1285–1295 (2019).
Vitolo, U. et al. ROBUST: first report of phase III randomized study of lenalidomide/R-CHOP (R2‐CHOP) vs placebo/R‐CHOP in previously untreated ABC‐type diffuse large B‐cell lymphoma. Hematol. Oncol. 37, 36-37 (2019).
US Food and Drug Administration. POLIVYVR US Prescribing Information. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761121s000lbl.pdf (Accessed 14 December 2023).
Palanca-Wessels, M. C. et al. Safety and activity of the anti-CD79B antibody-drug conjugate polatuzumab Vedotin in relapsed or refractory B-cell non-Hodgkin lymphoma and chronic lymphocytic leukaemia: a phase 1 study. Lancet Oncol. 16, 704–715 (2015).
Sehn, L. H. et al. Polatuzumab Vedotin in relapsed or refractory diffuse large B-Cell lymphoma. J. Clin. Oncol. 38, 155–165 (2020).
Terui, Y. et al. A phase 2 study of polatuzumab vedotin + bendamustine + rituximab in relapsed/refractory diffuse large B-cell lymphoma. Cancer Sci. 112, 2845–2854 (2021).
Tilly, H. et al. Polatuzumab Vedotin in combination with immunochemotherapy in patients with previously untreated diffuse large B-cell lymphoma: an open-label, non-randomised, phase 1b-2 study. Lancet Oncol. 20, 998–1010 (2019).
Tilly, H. et al. Polatuzumab Vedotin in previously untreated diffuse large B-Cell lymphoma. N Engl. J. Med. 386, 351–363 (2022).
Liu, N., Zhou, Y. & Lee, J. J. IPDfromKM: reconstruct individual patient data from published Kaplan-Meier survival curves. BMC Med. Res. Methodol. 21, 111 (2021).
China Foreign Exchange Trade System & National Interbank Funding Center. March (2024). Available at: https://www.chinamoney.com.cn/chinese/bkccpr/ (Accessed 2.
Liu, G. E. Guidelines for pharmacoeconomic evaluation in China Beijing: China Market Publishing House (2020). (2020).
Yao, Z. H. The big data service platform for china’s health industry: information query of drug bid winning (2024). Available at: https://db.yaozh.com (Accessed 15 March 2024).
Zhu, Y., Liu, K., Ding, D., Zhou, Y. & Peng, L. Pembrolizumab plus chemotherapy as First-Line treatment for advanced esophageal cancer: A Cost-Effectiveness analysis. Adv. Ther. 39, 2614–2629 (2022).
Li, N. et al. Cost-effectiveness analysis of Axicabtagene Ciloleucel vs. salvage chemotherapy for relapsed or refractory adult diffuse large B-cell lymphoma in China. Support. Care Cancer. 30, 6113–6121 (2022).
Ma, J. et al. Cost-effectiveness of obinutuzumab plus Bendamustine in Chinese patients with relapse and refractory follicular lymphoma. J. Comp. Eff. Res. 12, e230073 (2023).
National Institute for Health and Care Excellence. Polatuzumab vedotin in combination for untreated diffuse large B-cell lymphoma. Available at: https://www.nice.org.uk/guidance/ta874 (Accessed 15 December 2023).
24 et al. US cost-effectiveness analysis of polatuzumab Vedotin in previously untreated diffuse large B-cell lymphoma. J. Med. Econ. 26, 1134–1144 (2023).
Munir, T. et al. Cost-effectiveness of acalabrutinib regimens in treatment-naive chronic lymphocytic leukemia in the united States. Expert Rev. Pharmacoecon Outcomes Res. 23, 579–589 (2023).
Zhu, Y., Liu, K., Wang, M., Wang, K. & Zhu, H. Trastuzumab Deruxtecan versus trastuzumab emtansine for patients with human epidermal growth factor receptor 2-positive metastatic breast cancer: A cost-effectiveness analysis. Breast 66, 191–198 (2022).
Beusterien, K. M. et al. Population preference values for treatment outcomes in chronic lymphocytic leukaemia: a cross-sectional utility study. Health Qual. Life Outcomes. 8, 50 (2010).
Mizuoka, T. et al. Cost-effectiveness of combination therapy of polatuzumab Vedotin plus rituximab, cyclophosphamide, doxorubicin, and prednisolone for previously untreated diffuse large B-cell lymphoma in Japan. J. Med. Econ. 26, 1122–1133 (2023).
Song, Y. et al. Polatuzumab Vedotin in previously untreated DLBCL: an Asia subpopulation analysis from the phase 3 POLARIX trial. Blood 141, 1971–1981 (2023).
Zhou, Z. et al. An enhanced international prognostic index (NCCN-IPI) for patients with diffuse large B-cell lymphoma treated in the rituximab era. Blood 123, 837–842 (2014).
Maurer, M. J. et al. Event-free survival at 24 months is a robust end point for disease-related outcome in diffuse large B-cell lymphoma treated with immunochemotherapy. J. Clin. Oncol. 32, 1066–1073 (2014).
Jakobsen, L. H. et al. Minimal loss of lifetime for patients with diffuse large B-Cell lymphoma in remission and event free 24 months after treatment: A Danish Population-Based study. J. Clin. Oncol. 35, 778–784 (2017).
Roche Company. Roche presents new and updated data for Polivy in previously untreated diffuse large B-cell lymphoma at ASH (2022). Available at: https://www.globenewswire.com/news-release/2022/12/12/2571491/0/en/Roche-presents-new-and-updated-data-for-Polivy-in-previously-untreated-diffuse-large-B-cell-lymphoma-at-ASH-2022.html (Accessed 28 November 2023).
Horwitz, S. et al. Brentuximab Vedotin with chemotherapy for CD30-positive peripheral T-cell lymphoma (ECHELON-2): a global, double-blind, randomised, phase 3 trial. Lancet 393, 229–240 (2019).
Zhang, Y. et al. The impacts of government reimbursement negotiation on targeted anticancer medication price, volume and spending in China. BMJ Glob Health 6, 1-11 (2021).
Mingge, X., Jingyu, W., Qi, L., Zhe, Z. & Qing, R. Promoting access to innovative anticancer medicines: A review of drug price and National reimbursement negotiation in China. Inquiry 60, 469580231170729 (2023).
Kambhampati, S. et al. Cost-effectiveness of polatuzumab Vedotin in combination with chemoimmunotherapy (pola-R-CHP) in previously untreated diffuse large B-cell lymphoma in Germany. Br. J. Haematol. 202, 771–775 (2023).
Vijenthira, A., Kuruvilla, J., Crump, M., Jain, M. & Prica, A. Cost-Effectiveness analysis of frontline Polatuzumab-Rituximab, cyclophosphamide, doxorubicin, and prednisone and/or Second-Line chimeric antigen receptor T-Cell therapy versus standard of care for treatment of patients with Intermediate- to High-Risk diffuse large B-Cell lymphoma. J. Clin. Oncol. 41, 1577–1589 (2023).
Funding
This study was supported by research funding from the Doctoral Research Initiation Fund of the Affiliated Hospital of the Southwest Medical University. This study was supported by research funding from the 2022 University-level Research Projects of the Southwest Medical University(No.2022QN006).
Author information
Authors and Affiliations
Contributions
Mengya Li: Formal analysis; Funding acquisition; Writing-original draft. Qian Li: Formal analysis; Writing-original draft. Yinhui Zhang: Data curation; Software. Changjing Xu: Data curation; Investigation. Zhu Chen: Investigation; Supervision Yilan Huang: Supervision; Writing-review &editing. Longyang Jiang: Software; Funding acquisition; Writing-review &editing. Final approval of the manuscript was obtained from all authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
No human participants or animals presented in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, M., Li, Q., Zhang, Y. et al. Cost-effectiveness of polatuzumab vedotin plus chemoimmunotherapy for untreated diffuse large B-cell lymphoma in China. Sci Rep 15, 29752 (2025). https://doi.org/10.1038/s41598-025-15477-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15477-9