Abstract
The gastrointestinal tract is regarded as vulnerable due to frequent exposure to a variety of foods. Diarrhea, ulcers, constipation, and parasitic infections are considered to be the most prevalent disorders worldwide. The present study was conducted in the District Sahiwal to appraise the local flora for the treatment of a diverse range of gastrointestinal disorders (GIDs) for the first time. The interviews of 125 respondents were conducted during August 2021–January 2022 via a semi-structured questionnaire. Floristic analysis yielded a total of 73 plant species in 65 genera and 35 families. Fabaceae (n = 9), Cucurbitaceae (n = 5), Apiaceae (n = 5), Malvaceae (n = 5), and Moraceae (n = 5) were observed as the most prominent ethnomedicinal families. The gastrointestinal disorders were categorized into diarrhea, dysentery, stomach burn, abdominal pain, constipation, ulcer, intestinal problems, indigestion and stomachache. The maximum times reported gastrointestinal category was indigestion and stomachache (Informant Consensus Factor = 0.69.). Most of the plants were herbs (50%) and wildly (52%) available in this region. Local people prefer to use their leaves (43%) in the form of decoction or powder (37%). Quantitative data analysis reported Cymbopogon citrates and Musa paradisiaca most utilized medicinal taxa (Used value = 2.25). Furthermore, the study documented two new medicinal species i.e. Alstonia scholaris and Gardenia jasminoides, that were never been identified GID ethnopharmacology. These medicinal plants play a vital role in the development of our pharmaceutical industry for the better livelihoods of future generations. Documenting medicinal flora that was used in the treatment of gastrointestinal disorders in district Sahiwal would be helpful in the development of low-cost, effective, safe, and appropriate medications against gastrointestinal disorders.
Similar content being viewed by others
Introduction
Gastrointestinal disorders (GIDs) are the most prevailing disorders in the world1. World health organization (WHO), estimates GIDs caused nearly 1 million adult deaths worldwide during 2019 where diarrhea alone was responsible for 370,000 deaths in children under the age of 5 years2. According to last reports a major percentage (40%) of entire world is suffering in some kind of GIDs. It is more prevalent in women rather men3 and also spread over to infants (27%), toddlers (40.5%), children (9.9%), and adolescents (27.5%)4. The prevalence rate in United States of America reaches to 11 percent for chronic GIDs, whereas in geriatric population it extents to 35 percent3 and in children up to 23.1 percent5. In United Kingdom 81% of population have at least one of GIDs. Flatulence is most commonly reported issue6 along with abdominal pain and gut disorders in 25% of the infant and child population7. Its prevalence is much higher in the countries of Middle East i.e. 30.4 prevalence among children and adolescents (between 4–18 years age group)8. Data from India show 10 percent prevalence of GIDs in the people aged between 10–17 years9. In Pakistan, according to the last reports of Pakistan institute of medical sciences (PIMS), the number of patients with GIDs climbed by 30% over the between June 2016 and June 201710.
Ethnomedicine is considered to be a cultural and spiritual mode of medication11. This area of traditional medicine examines how different civilizations see health, illness, and fitness as well as how to seek treatment and alternative healing modalities12. Since ages ago, plants have been used medicinally because of their abundant and variety of biologically active compounds13. Based on the statistics, utilization of ethnomedicine is prominent in multiple developed nations. For instance, in China between 30–50 percent of all therapeutic usage is made up of herbal remedies and in India, out of the 15,000 herbaceous plants, 6000 have been employed as herbal medications14. According to a report seventy percent of HIV/AIDS patients in South Africa, London, and San Francisco use ethnomedicinal therapies for survival15. Moreover, especially in underdeveloped countries like Ghana, Mali, Nigeria, and Zambia ethnomedicine serves as the preliminary source of treatment. As per World Health Organization, 80% of the world’s population receives their main medical treatment from traditional medicine, including ethnomedicines16. Likewise for other ailments, ethnomedicines are also proven helpful to cure GIDs. Aleo vera, Withania somnifera, Morus nigra, Achyranthes aspera, Azadirachta indica, Mentha spicata, Syzygium cumini, Psidium guajava, Trachyspermum ammi and Foeniculum vulgare were repeatedly reported plants that were utilized in the treatment of gastrointestinal disorders. Low cost, easy availability, and instant relief are some of the certain reasons for the higher number of people’s dependence on local plant-based treatment for GIDs17,18. Additionally, in Asian cultures, many of the GIDs are considered as taboos e.g. piles, irritable bowel syndrome and gas etc. People never feel comfortable of sharing such GIDS with an unknown or non-native (most of the cases) physician19,20. Consequently, the trust of indigenous people on traditional remedies for GIDs is exceptionally high. Conversely, in various remote areas of third world countries including Pakistan, plant-based therapies are the only choice for rural communities.
There were many surveys and researches conducted in all-over the world that identified and described different therapeutic plants that used to cure GIDs21,22,23,24,25,26. In 2017, a research survey was conducted on ethnomedicinal treatment of GIDs in Romania. This study reported 78 plants potentially useful plants for the treatment of GIDs27. Similarly in Nigeria, a study on medicinal plants used for the treatment of gastrointestinal disorders reported 33 medicinally important plants species for GIDs28. In Pakistan as well limited ethnomedicinal surveys focusing on GIDs were conducted in past few years29,30. A GIDs specific ethnomedicinal evaluation was undertaken at the five major remote areas (Dera Ismail Khan, Bannu, Lakki Marwat, and Karak and Kohat) of Khyber Pakhtunkhwa province of Pakistan and reported total 52 medicinal plants species that were used for the treatment of gastrointestinal disorders31. In another digestive disorders oriented ethnomedicinal survey at the Laspur valley, Chitral, documented 44 medicinal plants27. Recently, efficacies of 69 medicinal plants against GIDs were reported from North Waziristan, Pakistan32. However, these GIDs specific ethnomedicinal studies are encompassing to northern flora mostly. Therefore, a comprehensive ethnomedicinal study specific for GIDs is required from other regions of Pakistan as well. Moreover, without a proper documentation this traditional knowledge wealth is at the verge of being threatened due to modernization and urbanization33. Hence, the basic purpose of this study was to document and preserved the GIDs specific ethnomedicinal knowledge of Sahiwal, Pakistan. The specific research questions were; (1) which medicinal flora used against GIDs by the people of the study area? (2) Which part of plant has medicinal potential, along with its basic drug formulation recipe and mode of administration? (3) What is the cultural relevance and agreement in the use of medicinal plants against certain GIDs? (4) Which plants are most trusted by the local people for GIDs cure? (5) What the statistical association between reported species and their identified attributes e.g. life form, growth habit etc.? (6) What are the similarities and differences between the GIDs associated traditional knowledge of aligned areas? Ethnobotanical indices were applied to answer the last three research questions. This data could be than subjected to further pharmacological and phytochemical investigation.
Results
Socio-demographic features of informants
A total of 125 people were interviewed during the survey among which, 62% of participants were men and 38% were women and the majority (49%) of them were between 40–60 years. Four ethnic groups were prominently identified in the study area i.e. Siyal, Arain, Rajput, and Baloch. However, Arain (48%) was dominant, and Rajput (14%) was the subservient ethnic group of the study area. Concerning education, the maximum participants were educated i.e. (70%) and most of them possessed post-graduation or higher qualifications (26%). Demographic data showed that housewives (29%) were well aware of the utilization of medicinal flora for GIDs (Table 1). Whereas herbalists (14%), gardener (13%), farmers (18%), and other job holders (26%), also well contributed to the data collection (Table 1).
Taxonomic diversity
In this study total of 74 plants that were associated with 65 genera and 35 families were reported for GIDs. Fabaceae was mentioned as the top-represented family in terms of species number (n = 9), followed by Cucurbitaceae (n = 5), and Apiaceae, Malvaceae, Moraceae (n = 5). Amaranthaceae, Poaceae, and Solanaceae are represented with 4 species in each family. Asteraceae represent 3 species. Brassicaceae, Convolvulaceae and Myrtaceae represent 2 species (Table 2), while the remaining 23 families were monotypic. Results showed that the majority of collected plants were grown as wild (52%), however, substantial number is regarded as cultivated (24%), or both wild and cultivated (24%) in the study area (Fig. 1a). Reported flora was most abundant in summers (41%), followed by winter (22%), spring–summer (21%), and spring (7%) (Fig. 1b).
Growth form, part used, and remedy of medicinal plants
Among the reported species growth habit was observed as, herbaceous plants 33, trees 20, shrubs 9, climbers 7, and grasses 4. Overall, predominantly, for the treatment of gastrointestinal disorders, leaves were the most frequently utilized plant part across 29 species, succeeded by fruit (18 species), seed (15 species), root (11 species), bark (10 species), flower (8 species), whole plant (6 species), stem (3 species), and bulb (2 species). The part utilization data showed variation as per type of habit. For example herbaceous plants predominantly employed for leaves (31%), Whereas, among shrubs, fruit and flower were the most utilized parts (33%).Trees predominantly utilized for bark (34%), and leaves (28%). (Fig. 2a, b) (Table 2).
(a) The percentage of different plant parts in various growth form categories of medicinal flora used for gastrointestinal disorders. (b) Chord diagram depicting the plant part and species used against gastrointestinal disorders. The degree of taxa diversity is shown by the width of each block, while the tendency of the outlines shows which species are associated with which part is used. For full species names see Table 2.
Mode of administration
The investigation into the preparation methods of remedies derived from the 73 recorded plant species involved categorization according to their application in medicinal formulations. The findings indicated that overall decoction was the prevailing technique employed by the local population, encompassing 47 species, followed closely by powder (45 species). Additionally, juice was utilized in 12 species, while raw preparations were noted in 8 species. Paste and cooked forms were employed in 4 species each, whereas oil-based preparations were found in only 2 species. Figure 3a, b represented a closer look for relationship between mode of preparation and plant part. The plant part bulb is predominately used in the form of decoction and powder (43%) followed by paste (10%), and juice (05%). The flower part is mostly used in the form of decoction (46%), powder (31%), juice (15%), and paste (08%). The leaves were used in the form of decoction in the form of decoction (44%), followed by powder (37%), juice (07%), paste (06%), cooked (04%), and raw (2%). Fruit is predominantly used as powder (33%), followed by decoction (31%), juice and raw (14%), cooked (06%), and paste (03%) (Fig. 3a, b).
(a) The percentage of different modes of administration of various plant parts of medicinal flora used for gastrointestinal disorders. (b) Chord diagram depicting the mode of administration and species used against gastrointestinal disorders. The degree of taxa diversity is shown by the width of each block, while the tendency of the outlines shows which species are associated with which part is used. For full species names see Table 2.
Ethnomedicinal data analysis
Informant Consensus Factor (ICF) categorized GIDs into 8 categories i.e. diarrhea, dysentery, ulcer, constipation, stomach burn, abdominal pain, intestinal problems, indigestion & stomach pain. In this research survey, the values of ICF placed in between the range of 0.38–0.69. The ailment category with the highest ICF value 0.69 was indigestion and stomach pain with the maximum number of reported medicinal plants (Table 3) (Fig. 4). The least consensus was reported for abdominal pain (ICF 0.38) (Table 3).
The analysis of collected data reflected that the highest reported utilized plant part was leaves for all kinds of GIDs i.e. 43% for diarrhea, 43% for dysentery, 55% for ulcers, 45%, for constipation, 33% for stomach burn, 35% for abdominal pain, 36% for intestinal problems, 34% for indigestion and stomach. The majority of plant species form drugs against GID by using decoction and powder methods with a count of 37%. Significant disparities were observed in the utilization of plant species across various GIDs, as illustrated by axis 1 in the accompanying Fig. 4. Principal Component Analysis (PCA) unveiled noteworthy distinctions among the different disorders. PC1 and PC2, delineating the presence and absence of plant species respectively, collectively explained 57.1% of the variance in species distribution within the biplot (Fig. 5).
Research observations of Use Value (UV) of plant species placed between the range of 1 (Solanum virginianum, Rosa indica, Zea mays, Azadirachta indica, Ficus palmata, Syzygium cumini, Hibiscus rosa-sinensis, Grewia asiatica, Malva parviflora, Abutilon indicum, Cyamopsis tetragonoloba, Digera muricata and some others) to 2.25 (Cymbopogon citratus and Musa paradisiaca) (Table 2).
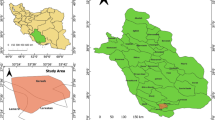
Similarity with previous work
By calculating the value of the Jaccard index (JI), results showed that the value of JI ranges between 41.32 and 9.09. The maximum similarity index (JI) was documented from the areas of Wazirabad, Kharian, Gujranwala, and Gujrat i.e. ≥ 30.36. The lowest JI was determined from the area of Cholistan i.e. 9.09 (Fig. 6) (Table 4). By comparing the data with align areas (20 published research literatures of aligned areas); it was found that Alstonia scholaris and Gardenia jasminioides had never been reported for their utilization against GIDs. Trachyspermum ammi were reported in only ethnomedicinal literatures from Chichawatni, Wazirabad and Sialkot but with dissimilar use. While eight plants species Daucus carota, Luffa acutangula, Leucaena leucocephala, Asperagus racemosus, Ficus palmate, Tinospora cordifolia, Musa paradisiacal and Phyla nodiflora that were reported in only published ethnomedicinal literature of Wazirabad with similar use (Table 2).
Discussions
It was observed that participation of men in the survey is greater than women. This is due to the social limitations of research area that women were hesitant to engage in conversation with random strangers46,54. However, during survey it was observed that female informants contain substantial traditional knowledge in comparison to men because most of the drug formulation recipes were reported by them. This is due the fact that most of the women were housewives and they play more effective role in sustenance and healthcare of their families in case of an illness. These results were in accordance to the previously published ethnobotanical literature from Pakistan55,56,57,58. The largest number of participants belonged to age group between 40 and 60 years because below this age group young people were usually not interested or mistrusted the traditional therapeutic ways and above 60 years although people possessed significant traditional knowledge (as they reported greater number of plants in comparison to other age groups) but smaller number of them were able to communicate due to multiple health issues. Hence, it indicates the threat of loss of traditional knowledge. At present, the traditional medical knowledge transmitted from generation to generation is in danger, because transmission between old people and younger generations is not always assured59. Results showed most people of this area were literate. This is because of the higher literacy rate of the area (https://www.pbs.gov.pk/census-2017-district-wise/results/061). Although the smaller numbers of informants have not attended school at all (27%) shared more information about traditional use of medicinal plant species in comparison to literate ones. This is due the fact that formal education affects the lifestyle patterns and usually people shift on allopathic medicine rather traditional medicines. Similar findings have also been reported from other ethnobotanical studies60,61.
Results reported that indigestion and stomach pain as most significant GID, as most of the medicinal taxa have been used against this category (highest ICF). This shows that this is prevailing disease of the study area and should be investigated for its causes of occurrence and effects62. The majority of collected plants were present in herbaceous form, it seems that local people more preferably use the herbaceous flora because of its availability and accessibility ease in study area. The predominant utilization of leaves as medicinal part for all GIDs is well supported by other ethnomedicinal studies of Pakistan34,37,40,41,48,49,50. This study also advocated decoction as most preferred mode of preparation. The frequent use of the decoction can be explained by the fact that the decoction makes it possible to collect the most active ingredients and attenuates or cancels out the toxic effect of certain recipes. Ethnobotanical research surveys conducted somewhere else in Pakistan showed the majority of the informants prepared their traditional medicines by decoction method59,63,64,65. This confirms that there is a perpetual exchange of information on the use of medicinal plants across the communities of Pakistan. Decoction mentioned as the major method of preparation at the continental level66,67,68. This study also accounted for substantial use of cultivated plant resource such Allium cepa, Mangifera indica, Piper nigrum, and Zea mays to cure common GIDs. One of the reasons is easy availability and accessibility of these plants. Another reason possibly could be the unfamiliarity with use of wild plant resources. This shows that traditional knowledge associated with wild plants is declining day by the day. Due to modernization and urbanization, people are getting more familiar with cultivated plants rather wild. Hence preservation of traditional knowledge associated with wild plants needed to be more cautiously preserved.
Quantitative indices applied in this study helped to identify the homogeneity among the reported data69. Nearly all plants showed good utilization values (UV ≥ 1). This reflected that all the plants popular and trusted by the local com-munities59,70. However, Musa x paradisiaca, Cymbopogon citratus, Alstonia scholaris, Gardenia jasminoides and Phyla nodiflora were most trustworthy by the local community for GIDs because of their comparatively higher relative significance (UV ≥ 2). From the literature survey (Supplementary Table) it was found that these medicinal plants contain valuable bioactive compounds which provide definite physiological action on the human body for particular GIDs71. Previously reported phytochemical studies of these plants documented the presence of alkaloids, flavonoids, tannins, glycosides, saponins, terpenoids, fatty acids, steroids and phenols. All of these phytochemicals somehow play role in curing GIDs. Tannins and flavonoids are thought to be responsible for antidiarrhoeal activity by increasing colonic water and electrolyte reabsorption72,73,74. Alkaloids are well-known for having analgesic, antispasmodic and antimicrobial effects75. Similarly glycosides are notable antimicrobial and laxative properties76. Phenols are recognized for their antioxidant and antimicrobial activities77. Saponins offer antifungal, antiviral, anticancer and antispasmodic properties78. Steroids are anti-inflammatory in nature79. Terpenoids show antispasmodic properties80.
The largest JI value reflected that the floral types of these areas have similarity due to homogenous climate, geographical and cultural situations. The lowest JI value reflected that the floral types of these areas have no similarity due to the variations in climate, geographical, cultural situations and the utilization pattern of the plants of this area was changed from the utilization pattern of present study. Bibi et al.69, and Farooq et al.81, also advocated that similarities and differences in ethnomedicinal data arise due to the ecological, historical, and organoleptic across the areas. Moreover it was found that Alstonia scholaris and Gardenia jasminioides had never been reported for their utilization against GIDs in the align areas. Compared to previous ethnomedicinal surveys in nearby areas such as Wazirabad49, Sialkot35, and Bahawalnagar41, our study reveals both overlapping and distinct uses of medicinal flora. For instance, Musa paradisiaca and Cymbopogon citratus were also cited in Wazirabad but were assigned broader uses in our study, particularly with higher use values. In contrast, Alstonia scholaris and Gardenia jasminoides were uniquely reported in our study for treating gastrointestinal disorders, representing novel ethnomedicinal knowledge. The variation in reported species and their application may be attributed to ecological differences, informant traditions, or methodological approaches.
Conclusions
It can be concluded that plants a significant role in primary health care system of district Sahiwal, Pakistan. This study for the very first time provides documented data about the ethnomedicinal plants of district Sahiwal, Pakistan particularly used for GIDs. The study reported 74 plants belonging to 35 families with the predominant herbaceous habit and leaves as the most reliable ethnomedicinal part. Furthermore, majorities were prepared drugs through decoction and ingest from oral route. Indigestion and stomach pain were regarded as the most significant GID, as most of the medicinal taxa have been used against these categories. Almost all plants showed good utilization values (UV ≥ 1). However, Musa x paradisiaca, Cymbopogon citratus, Alstonia scholaris, Gardenia jasminoides and Phyla nodiflora showed comparatively higher relative significance (UV ≥ 2). By comparing the data with align areas Alstonia scholaris and Gardenia jasminioides were reported as novel species for their utilization against GIDs. These findings not only preserve the traditional wealth of ethnomedicinal knowledge but also serve as the baseline data for drug discoveries. Further studies are required to identify the endemic ethnomedicinal species due to over exploitation which could be of significant value for conservation and sustainable management of these ethnomedicinal species.
Materials and methods
Study area
Ethno-medicinal field surveys were conducted in district Sahiwal Punjab Pakistan. Sahiwal is located between Lahore and Mul-tan (http://www.mcsahiwal.lgpunjab.org.pk/). district Sahiwal is bordered on the south by district Bahawalnagar, west by district Khanewal, and East by district Okara. On the north side, the Ravi River runs. district Sahiwal covers 3201 square kilometers. Most of the forests in Sahiwal district are irrigated; the Chichawatni Forest, which covers 9000 acres and is the second-largest planned forest in Pakistan, is one of these forests. There are riverine forests beside the Sutlej and Ravi rivers. The region has a 5210 km linear plantation and 11,532 acres of forest. Major crops like sugarcane, maize, and cotton are supported by its fertile soils, which range from sandy loam to clayey loam. The weather of Sahiwal is semi-arid, with long, hot summers and moderate winters. The major flora of the district includes Acacia arabica (kikar), Acacia modesta (phulai), Acacia nilotica (babul), Albezia lebbek (sirin), Azardirachta indica (neem), Bombax cieba (simal or silk) cotton, Capparis aphylla (karir), Cassia fistula (amaltas), Cordia myxa (lasura), Dalbergio sissoo (shisham), Eucalyptus camaldulensis (red gum tree or sufaida), Eucalyptus cineraria (eucalyptus), Ficus benghalensis (bargad or banyan), Ficus racemosa (gulhar), Ficus religiosa (pipal), Grewia optiva (dhamna), Melia azedarach (bakain or Persian lilac), Moringa oleifera (sohanjna), Morus alba (mulberry or toot), Nyctanthes arbor-tristis (night jasmine), Oroxylum indicum (talwar phali), Pithecellobium dulce (jungle jalebi), Pongamia pinnata (sukh chain), Prosopis juliflora (mesquite), Prosopis spicigera (jand), Salvadora oleoides (vann or peelu), Swietenia macrophylla (mahogany), Tamarix articulata (frash), Terminalia arjuna (arjun), and Zizyphus nummularia (ber). Some shrubs grown in the district include Acacia filicoides (leaf acacia), Alhagi maurorum (jawain), Atriplex canescens (lani), Buxus papillosa (boxwood), Caesalpinia bonduc (katkaranj), Cassia occidentalis (kasondi), Sesbania bispinosa (canicha), Leptadenia pyrotechnica (khip), and Ocimum basilicum (niazbo or basil) and Mimosa pudica (touch-me-not). Some of the grasses found in the district include Cenchrus biflorus (Indian Sandbur), Cyperus rotundus (nut grass or mutha), Cynodon dactylon (khabbal), Desmostachya bipinnata (dab), and Panicum turgidum (murat) (Pakistan Almanac 2024; Government of Pakistan 2021) (https://pakistanalmanac.com/punjab-sahiwal, https://bor9.pitb.gov.pk/system/files/Sahiwal.pdf). As per Pakistan Bureau of Statistics reports population of Sahiwal district was 2,513,011 in 2017. Out of which 1,997,327 were residing in rural areas and 515,684 in urban areas. Sahiwal district is divided in 2 tehsils at administrative level. Population of Sahiwal tehsil was 1,488,831 while for Chichawatni tehsil 1,024,180 (Pakistan Bureau of Statistics 2017). In 2023 it was estimated that the population of Sahiwal district reached 2,881,811 with average growth rate of 2.31 (Pakistan Bureau of Statistics 2023 https://www.pbs.gov.pk/sites/default/files/population/2017/results/06101.pdf, https://www.pbs.gov.pk/sites/default/files/population/2023/Punjab.pdf). Ethno-medicinal data was collected from five different sites Kamir, Noorshah, Chichawatni, Harappa, and Qadarabad from the study area for the survey of medicinal plants used for the treatment of gastrointestinal disorders in district Sahiwal (Fig. 6). These sites were rich in floral diversity which is why local inhabitants prefer to adopt herbal remedies than pharmaceutical drugs to cure gastrointestinal problems. Cattle are also kept, and Sahiwal is known for its water, and buffalo milk. Sahiwal district has a hot climate in the summer, with temperatures reaching 47 °C, and a cold climate in the winter, with temperatures dropping to 2 °C. The district Sahiwal’s soil is extremely fertile. The average rainfall is 177 mm34 (https://www.punjab.gov.pk/sahiwal).
Data collection
Well-organized field visits were conducted in 5 different sampling sites of the study area from August 2021 to January 2022. The Participatory Rural Appraisal (PRA), which is based on interactions with local inhabitants and direct field surveying, was used to collect ethno-medical data. International Society of Ethnobiology (ISE) code of Ethics (https://www.ethnobiology.net/what-we-do/coreprograms/ise-ethics-program/ code-of-ethics/), and rules and regulations developed by the ethical review committee of the University of Okara was strictly observed throughout research activities. All methods were performed in accordance with the relevant guidelines and regulations. In addition, individuals’ informed consents were also taken before the interviews. The informants were chosen using a purposive sampling method; this is a non-probability type of sampling that involves knowledgeable experts of study area. In the current study informants were selected that are directly or indirectly involve in utilization of medicinal plants like herbalists, farmers, gardeners or other common people possessed the ethnomedicinal knowledge. All the participants were inquired through semi-structured open-ended interviews and a standard questionnaire (Supplementary Table 1a). The questionnaire compiled data on the respondent’s demographic characteristics, traditional names for plants, sections used, availability, mode of plant administration, mode of preparation, cultivation status, and diseases cured the questionnaire was in both English, Urdu and Punjabi. With the help of medical practitioner, we have prepared a list of symptoms to particular gastrointestinal disorder in the local language of informants (Urdu, Punjabi) (Supplementary File 1). By questioning about the exact symptoms informants encountered in their local language, we were able to obtain information from them. Face-to-face interviews with individual participants, as well as group discussions, were conducted. The interviews were conducted in Punjabi and Urdu according to the comfort of respondents (Supplementary Table 1b). Respondents were chosen mostly based on their knowledge and willingness to share. Following the collection of demographic information, the respondent’s knowledge of herbal remedies was recorded. With the aid of local informants, the mentioned plants were recognized by their common names and collected in the field. The Flora of Pakistan was used to identify the plant species. All collected plants were organized on the sheets of herbarium with their botanical names and family names after their correct identification and submit this herbarium in the laboratory of the botany department of the University of Okara, Pakistan (Supplementary Figs. 1–13).
Ethnomedicinal data analysis tools
Informant consensus factor (ICF)
Informant consensus factor (ICF) for diverse GIDs ailment categories was calculated to test the homogeneity or constancy of the informants’ knowledge about a particular therapy for a particular GIDs ailment. It is used to highlight plants of cultural relevance and agreement in the use of medicinal plants against certain disorders82,83 The ICF value ranges from 0 to 1. A value close to 1 indicates an agreement among respondents in the use of taxa within a particular disease category84,85. The ICF value was calculated using the formula82 i.e.
Nur = total number of uses reported for a specific category of disease. Nt = number of taxa reported for a specific category of disease.
Use value (UV)
The proportional significance of uses of different species of plants is determined by their usage value (UV) by the formula83
UV = usage value of specific species. Ui = number of uses that recorded by informants. N = total number of informants who reported that species.
Jaccard index (JI)
Jaccard index is used to compare the research work with relevant previous research, to examine the differences and resemblances of conventional knowledge between various communities and regions. By using Jaccard indices, it was possible to evaluate the values that show how identical traditional knowledge of different areas84,85,86. JI is calculated by using the subsequent formula i.e.
a = total number of plants species recorded from research area. b = total number of plants species recorded from other published research area. c = number of plants species common in both areas.
Statistical analysis
The data collected through research surveys underwent analysis using IBM SPSS version 25 to derive quantitative and qualitative results, which were subsequently discussed Principal Component Analysis (PCA) was employed to elucidate the consumption of plant components and the uses. The PCA biplot, contribution plot, and eigenvalues corresponding to the variance explained by each principal component were generated using the “fact” function. OriginPro software (version 9.95, free student version; OriginLab Corporation, Northampton, MA, USA; https://www.originlab.com) was used to generate chord diagrams illustrating relationships between plant parts and their modes of preparation, as well as to create a circular cluster heat map visualizing species frequency and usage patterns. The thickness of each bar in the diagram was utilized to discern the association between species and life form, as well as the method of preparation, along with the frequency of each species within each group. Furthermore, a circular cluster heat map was generated using the Origin Pro (version 9.95) program87.
Data availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- GI:
-
Gastrointestinal
- GIDs:
-
Gastrointestinal disorders
- WHO:
-
World health organization
- PRA:
-
Participatory rural appraisal
- ISE:
-
International society of ethnobiology
- ICF:
-
Informant consensus factor
- UV:
-
Usage value
- RI:
-
Relative importance
- FL:
-
Fidelity level
- JI:
-
Jaccard index
- PCA:
-
Principal component analysis
References
Welcome, M. O. Gastrointestinal Physiology: Development, Principles and Mechanisms of Regulation 1st edn. (Cham, Springer Nature, 2018).
Peterson, C. T. Dysfunction of the microbiota-gut-brain axis in neurodegenerative disease: The promise of therapeutic modulation with prebiotics, medicinal herbs, probiotics, and synbiotics. J. Evid. Based Integr. Med. 25, 2515690X20957225 (2020).
Avramidou, M. et al. Epidemiology of gastrointestinal symptoms in young and middle-aged Swiss adults: Prevalences and comorbidities in a longitudinal population cohort over 28 years. BMC Gastroenterol. 18, 1–10. https://doi.org/10.1186/s12876-018-0749-3 (2018).
Robin, S. et al. Prevalence of pediatric functional gastrointestinal disorders utilizing the Rome IV criteria. J. Pediatr. 195, 134–139. https://doi.org/10.1016/j.jpeds.2017.12.012 (2018).
Lewis, M. L., Palsson, O. S., Whitehead, W. E. & van Tilburg, M. A. Prevalence of functional gastrointestinal disorders in children and adolescents. J. Pediatr. 177, 39–43 (2016).
Thomson, C., Edwards, C. & Garcia, A. Digestive symptoms in UK adults and the perceived effect of foods. Curr. Dev. Nutr. 5, 458. https://doi.org/10.1093/cdn/nzab038_070 (2021).
Thapar, N. et al. Paediatric functional abdominal pain disorders. Nat. Rev. Dis. Primers 6, 89. https://doi.org/10.1038/s41572-020-00222-5 (2020).
Ibrahim, A. T., Hamdy, A. M. & Elhodhod, M. A. Prevalence of functional gastrointestinal disorders among school-aged children and adolescents, a multicenter study. QJM Int. J. Med. 113, 063–129. https://doi.org/10.1093/qjmed/hcaa063.029 (2020).
Bhatia, V. et al. Prevalence of functional gastrointestinal disorders among adolescents in Delhi based on Rome III criteria: A school-based survey. Indian J. Gastroenterol. 35, 294–298. https://doi.org/10.1007/s12664-016-0680-x (2016).
Qasim, M. PIMS Registers 87,790 Patients with Digestive Diseases in One Year (The News International, 2018).
Shyma, T. B. & Devi Prasad, A. G. Traditional use of medicinal plants and its status among the tribes in Mananthavady of Wayanad district, Kerala. World Res. J. Med. Arom. Plants 1(2), 22–26 (2012).
Amuthavalluvan, V. Ethno medicinal practices and traditional healing system of Kattunayakan in Tamilnadu: An anthropological study. Int. Multidiscip. Res. J. 1(7), 47 (2011).
Prasad, C. C., Khemchandani, N. V., Bhagat, R. T. & Pimpale, A. D. Ethnomedicinal plant—A review. J. Pharm. Res. Int. 33(29B), 17–30 (2021).
Tripathi, S. Ethnomedicine and future challenges. Global J. Archaeol. Antropol. 10(5), 87–90 (2019).
Sharma, B. K. Ethnomedicine: Study of traditional medicine. Biotech. Artic. 18, 30–31 (2011).
Ramesh, T.C. Ethnomedicinal Plants of Chandi Devi Hills of Haridwar in Perspectives of Ayurveda. 14 (2013).
de Wet, H., Nkwanyana, M. N. & van Vuuren, S. F. Medicinal plants used for the treatment of diarrhoea in northern Maputaland, KwaZulu-Natal province South Africa. J. Ethnopharm. 130(2), 284–289 (2010).
Lokho, A. The folk medicinal plants of the Mao Naga in Manipur, North East India. Int. J. Sci. Res. Pub. 2(6), 1–8 (2012).
Chelvanayagam, S. Stigma, taboos, and altered bowel function. Gastrointest. Nurs. 12(1), 16–22 (2014).
Qin, Y. et al. Dietary and behavioural associations with maternal health among puerperal women in South China. Asia Pac. J. Clin. Nutr. 30(2), 291–302 (2021).
Olajuyigbe, O. & Afolayan, A. Ethnobotanical survey of medicinal plants used in the treatment of gastrointestinal disorders in the Eastern Cape province South Africa. J. Med. Plant. Res. 6(18), 3415–3424 (2012).
Dwivedi, S., Dwivedi, S. & Patel, P. (2006) Medicinal plants used by the tribal and rural people of Satna district, Madhya Pradesh for the treatment of gastrointestinal diseases and disorders. 60–63.
Chanda, R. et al. Medicinal plants used against gastrointestinal tract disorders by the traditional healers of Sikkim Himalayas. Indian J. Tradit. Knowl. 6(4), 606–610 (2007).
Neamsuvan, O. et al. A survey of folk remedies for gastrointestinal tract diseases from Thailand’s three southern border provinces. J. Ethnopharm. 144(1), 11–21 (2012).
Rokaya, M. B. et al. Traditional uses of medicinal plants in gastrointestinal disorders in Nepal. J. Ethnopharm. 158, 221–229 (2014).
Bahmani, M., Zargaran, A. & Rafieian-Kopaei, M. Identification of medicinal plants of Urmia for treatment of gastrointestinal disorders. Rev. Bras. Farmacogn. 24(4), 468–480 (2014).
Papp, N. et al. Ethnomedicinal treatment of gastrointestinal disorders in Transylvania Romania. Acta Ethnographica Hungarica 62(1), 207–220 (2017).
Sulaiman, A. N., Arzai, A. H. & Taura, D. W. Ethnobotanical survey: A comprehensive review of medicinal plants used in treatment of gastrointestinal diseases in Kano state Nigeria. Phytomed. Plus 2(1), 100180 (2022).
Wali, R. et al. Ethnomedicinal appraisal of plants used for the treatment of gastrointestinal complaints by tribal communities living in Diamir district, Western Himalayas Pakistan. PLoS ONE 17(6), e0269445 (2022).
Jamal, Z. et al. Ethnomedicinal plants used for gastrointestinal ailments by the rural communities of Kaghan valley, Mansehra Pakistan. J. Appl. Environ. Biol. Sci. 7(12), 41–48 (2017).
Tariq, A. et al. Ethnomedicinal evaluation of medicinal plants used against gastrointestinal complaints. Biomed. Res. Int. 1, 892947 (2015).
Rehman, S., Iqbal, Z. & Qureshi, R. Ethnomedicinal plants used for the treatment of gastrointestinal disorders in tribal district North Waziristan, Khyber Pakhtunkhwa Pakistan. Ethnobot. Res. Appl. 26, 1–22 (2023).
Ibrar, M., Hussain, F. & Sultan, A. Ethnobotanical studies on plant resources of Ranyal hills, district Shangla Pakistan. Pak. J. Bot. 39(2), 329 (2007).
Qureshi, R. et al. Ethnomedicinal uses of plants by the people of Kadhi areas of Khushab, Punjab Pakistan. Pak. J. Bot. 43, 121–133 (2011).
Arshad, M. et al. Ethnomedicinal flora in district Sialkot, Punjab Pakistan. Middle East J. Sci. Res. 9, 209–214 (2011).
Qureshi, R. et al. Medico-ethnobotanical knowledge of Jhang Saiyidan, Islamabad Pakistan. Arch. Sci. 65, 259–271 (2012).
Mahmood, A. et al. Indigenous knowledge of medicinal plants from Gujranwala district Pakistan. J. Ethnopharmacol. 148, 714–723 (2013).
Ahmed, N. et al. Ethnomedicinal knowledge and relative importance of indigenous medicinal plants of Cholistan desert, Punjab Province Pakistan. J. Ethnopharmacol. 155, 1263–1275 (2014).
Ajaib, M., Ashraf, Z. & Riaz, F. Ethnobotanical studies of some plants of Tehsil Kharian district Gujrat. FUUAST J. Biol. 4, 65–71 (2014).
Ahmed, N. et al. Relative importance of indigenous medicinal plants from Layyah district, Punjab Province Pakistan. J. Ethnopharmacol. 155, 509–523 (2014).
Ahmed, N. et al. Ethnopharmacological relevance of indigenous medicinal plants from district Bahawalnagar, Punjab Pakistan. J. Ethnopharmacol. 175, 109–123 (2015).
Zereen, A., Khan, Z. U. D. & Sardar, A. A. An assessment and documentation of conventional medico-botanical knowledge of indigenous communities around chichawatni plantation reserved forest. Pharm. Chem. J. 2, 27–35 (2015).
Ahmed, N. et al. Ethnopharmacological importance of medicinal flora from the district of Vehari, Punjab province Pakistan. J. Ethnopharmacol. 168, 66–78 (2015).
Khan, I. et al. Importance of ethnomedicinal flora of Sarai Alamgir (boundary side of river Jhelum) district Gujrat, Punjab Pakistan. Med. Aromat. Plants 5, 2167–2412 (2016).
Saleem, J., Jabeen, A. & Butt, A. Ethno-medicinal investigation of floral diversity of Bahawalnagar district, Punjab Pakistan. Middle East J. Bus. 12, 1 (2017).
Umair, M., Altaf, M. & Abbasi, A. M. An ethnobotanical survey of indigenous medicinal plants in Hafizabad district Punjab–Pakistan. PLoS ONE 12, e0177912 (2017).
Noreen, F. et al. Data of ethnomedicinal plants in Wazirabad, district Gujranwala, Punjab Pakistan. J. Pharma Care Health Syst. 5, 2376–2419 (2018).
Umair, M. et al. Ethnomedicinal uses of the local flora in Chenab riverine area, Punjab province Pakistan. J. Ethnobiol. Ethnomed. 15, 1–31 (2019).
Altaf, R. Ethnomedicinal study of Tehsil Wazirabad Gujranwala Punjab Pakistan. Pak. J. Sci. 71, 4 (2019).
Ali, S. S. et al. Ethnobotanical knowledge and folk medicinal significance of the flora of district Gujrat, Punjab Pakistan. Herba Polonica 66, 1 (2020).
Noreen, F. et al. Ethnomedicinal profile of flora of District Sialkot, Punjab Pakistan. New Trends Med. Sci. 1, 65–83 (2020).
Tufail, M. et al. Ethnobotanical survey of important wild medicinal plants of Tehsil Gojra, District Toba Tek Singh, Punjab Pakistan. Ethnobot. Res. Appl. 20, 1–14 (2020).
Mukhtar, A. et al. Ethnoflora of Tehsil Kharian, district Gujrat-Punjab Pakistan. GU J. Phytosci. 1, 133–139 (2021).
Harun, N. et al. Ethnobotanical studies of fodder grass resources for ruminant animals, based on the traditional knowledge of indigenous communities in Central Punjab Pakistan. J. Ethnobiol. Ethnomed. 13, 1–16 (2017).
Hassan, M. et al. Cross-ethnic use of ethnoveterinary medicine in the Kashmir Himalaya—A Northwestern Himalayan region. Acta Ecol. Sin. 43, 617–627 (2023).
Arshad, F. et al. Environmental variables drive medicinal plant composition and distribution in various forest types of the subtropical region in Pakistan. Ecol. Front. 44, 234–246 (2024).
Haq, S. M. et al. Plant cultural indicators of forest resources from the Himalayan high mountains: Implications for improving agricultural resilience, subsistence, and forest restoration. J. Ethnobiol. Ethnomed. 20, 44 (2024).
Awoke, A. et al. Traditionally used phytomedicines and their associated threats in Bita district, southwestern Ethiopia. J. Ethnobiol. Ethnomed. 21(1), 8 (2025).
Jabeen, S. et al. Folk knowledge and perceptions about the use of wild fruits and vegetables—Cross-cultural knowledge in the Pipli Pahar reserved forest of Okara Pakistan. Plants 13, 832 (2024).
Kamanzi Ntakirutimana, G. The impact of urbanization on traditional medicinal plant use in disease management. Health 3, 4 (2025).
Arshad, A. et al. Ethnobotanical assessment of woody flora of district Kasur (Punjab) Pakistan. Ethnobot. Res. Appl. 20, 1–13 (2020).
Wang, C. et al. Gut microbiota‐derived butyric acid regulates calcific aortic valve disease pathogenesis by modulating GAPDH lactylation and butyrylation. IMeta. e70048 (2025).
Murad, W. et al. Ethnobotanical assessment of plant resources of Banda Daud Shah, district Karak Pakistan. J. Ethnobiol. Ethnomed. 9, 1–10 (2013).
Kayani, S. et al. Ethnobotanical uses of medicinal plants for respiratory disorders among the inhabitants of Gallies-Abbottabad Northern Pakistan. J. Ethnopharmacol. 156, 47–60 (2014).
Sher, H. et al. Traditional use of medicinal plants among Kalasha, Ismaeli and sunni groups in Chitral District, Khyber Pakhtunkhwa province Pakistan. J. Ethnopharmacol. 188, 57–69 (2016).
Khoja, A. A., Waheed, M., Haq, S. M. & Bussmann, R. W. The role of plants in traditional medicine and current therapy: A case study from North part of Kashmir Himalaya. Ethnobot. Res. Appl. 27, 1–23 (2024).
Wang, B. et al. Low-friction soft robots for targeted bacterial infection treatment in gastrointestinal tract. Cyborg Bionic Syst. 5, 0138 (2024).
Yetein, M. H. et al. Ethnobotanical study of medicinal plants used for the treatment of malaria in plateau of Allada, Benin (West Africa). J. Ethnopharmacol. 146, 154–163 (2013).
Bibi, F. et al. Indigenous knowledge and quantitative ethnobotany of the Tanawal area, Lesser Western Himalayas Pakistan. PLoS ONE 17, e0263604 (2022).
Zenderland, J. et al. The use of “use value”: Quantifying importance in ethnobotany. Econ. Bot. 73, 293–303 (2019).
Bai, M. et al. Hydrolyzed protein formula improves the nutritional tolerance by increasing intestinal development and altering cecal microbiota in low-birth-weight piglets. Front. Nutr. 11, 1439110 (2024).
Palombo, E. A. Phytochemicals from traditional medicinal plants used in the treatment of diarrhoea: Modes of action and effects on intestinal function. Phytother. Res. 20, 717–724 (2006).
Wang, S. et al. The effects of different extraction methods on physicochemical, functional and physiological properties of soluble and insoluble dietary fiber from Rubus chingii Hu. fruits. J. Funct. Food. 93, 105081 (2022).
Cazarolli, L. H. et al. Mechanism of action of flavonoids in the control of diabetes mellitus. Med. Res. Rev. 28, 529–554 (2008).
Cordell, G.A. & Qin, G.W. Alkaloids: Their structure, biosynthesis, and pharmacological activity. In: The Alkaloids (1990).
Kapoor, L. D. CRC Handbook of Ayurvedic Medicinal Plants (CRC Press, 2018).
Rice-Evans, C., Miller, N. & Paganga, G. Antioxidant properties of phenolic compounds. Trends Plant Sci. 2, 152–159 (1997).
Francis, G. et al. The biological action of saponins in animal systems: A review. Br. J. Nutr. 88, 587–605 (2002).
Gower, D.B. & Ruparelia, B.A. Steroids: A comprehensive review. In Annu. Rev. Pharmacol. Toxicol. (1993).
Thoppil, R. J. & Bishayee, A. Terpenoids as potential chemopreventive and therapeutic agents in liver cancer. World J. Hepatol. 3, 228 (2011).
Farooq, A. et al. Ethnomedicinal knowledge of the rural communities of Dhirkot, Azad Jammu and Kashmir Pakistan. J. Ethnobiol. Ethnomed. 15, 1–30 (2019).
Trotter, R.T. & Logan, M.H. Informant consensus: a new approach for identifying potentially effective medicinal plants. In Plants and Indigenous Medicine and Diet, Redgrave Publishing Company, Bedford Hill, New York, 91-112 (2019).
Abe, R. & Ohtani, K. An ethnobotanical study of medicinal plants and traditional therapies on Batan island, the Philippines. J. Ethnopharmacol. 145, 554–565 (2013).
González-Tejero, M. et al. Medicinal plants in the Mediterranean area: Synthesis of the results of the project Rubia. J. Ethnopharmacol. 116(2), 341–357 (2008).
Asiimwe, S. et al. Ethnobotanical survey of medicinal plant species used by communities around Mabira and Mpanga central forest reserves Uganda. Trop. Med. Health 49, 52 (2021).
Phillips, O. & Gentry, A. H. The useful plants of Tambopata, Peru: I. Statistical hypotheses tests with a new quantitative technique. Econ. Bot. 47, 15–32 (1993).
Jaccard, P. Étude comparative de la distribution florale dans une portion des Alpes et des Jura. Bull. Soc. Vaudoise Sci. Nat. 37, 547–579 (1901).
Acknowledgements
The authors would like to extend their sincere appreciation to Ongoing Research Funding program (ORF-2025-134), King Saud University, Riyadh, Saudi Arabia.
Funding
The authors would like to extend their sincere appreciation to Ongoing Research Funding program (ORF-2025-134), King Saud University, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
Conceptualization, N.H. and S.S.R.; Methodology, M.W; software, M.W. and F.A.; validation, N.H. and M.W.; formal analysis, S.M.H., F.A., and M.A.; investigation, S.S.R.; resources, F.A. and I.B.; Data curation, M.W.; writing—original draft preparation, S.S.R, M.W., I.B; writing—review and editing, M.W., M.S., N.H., S.S.R, S.M.H., I.B., K.F., A.H., A.M.A., E.F.A., R.W.B., M.A., S.M.H., and F.A.; visualization, M.W.; supervision, M.W. and F.A.; project administration, S.S. All authors having substantial contributions in research, read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
For the survey, ethical guidelines of the International Society of Ethnobiology, 1988 (https://www.ethnobiology.net)78 were followed continuously. The survey design was approved by the Ethical Review Committee of the University of Okara (permit no. UOERC#125).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Harun, N., Waheed, M., Rubab, S.S. et al. Ethnomedicinal documentation of plants used for gastrointestinal disorders in Sahiwal District Pakistan. Sci Rep 15, 30683 (2025). https://doi.org/10.1038/s41598-025-15632-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15632-2