Abstract
This retrospective study compares the efficacy and safety of transurethral resection of the prostate (TURP), green-light photoselective vaporization of the prostate (PVP), and holmium laser enucleation of the prostate (HoLEP) in treating small-volume benign prostatic hyperplasia (BPH). Data from 645 patients with small-volume BPH (2012–2022, Zhejiang Provincial People’s Hospital) were analyzed. Baseline characteristics, surgical details, complications, and follow-up outcomes were compared. Logistic regression identified risk factors for urinary incontinence (UI) and bladder neck contracture (BNC). TURP was associated with a longer operative duration (53.15 ± 21.96 min) and catheterization time (5.29 ± 1.31 days) compared to PVP (48.53 ± 22.38 min, 4.84 ± 1.05 days) and HoLEP (45.00 ± 19.04 min, 4.79 ± 0.96 days). The incidence of BNC was significantly higher in the TURP group (9.4%) than in the PVP (4.8%) and HoLEP (5.7%) groups. Within 1 month postoperatively, the TURP group had a significantly higher proportion of patients with urinary incontinence. Between 1 and 3 months post-surgery, only UI with need for drug use (UIWD) remained significantly higher in the TURP group (8.2%). Preoperative indwelling catheterization, detrusor underactivity, severely elevated detrusor pressure, and undergoing TURP were identified as independent risk factors for UI. Green-light PVP was found to be a protective factor against BNC (OR = 0.40, P = 0.043). Green-light PVP and HoLEP showed similar efficacy and safety, with PVP offering the shortest operative time. TURP was associated with higher rates of BNC and UI. Laser techniques are preferable for high-risk patients.
Similar content being viewed by others
Introduction
Benign prostatic hyperplasia (BPH) is a common condition in aging men, which is characterized by the proliferation of smooth muscle, connective tissue, and epithelial cells in the transition zone of the prostate1,2. Prostate volume (PV) serves as an essential reference indicator for formulating treatment strategies for BPH. Small-volume BPH, which is typically defined as a PV of ≤ 30 mL, presents unique clinical challenges3. In small-volume BPH, the severity of lower urinary tract symptoms (LUTS) does not invariably correlate strongly with PV4,5. This suggests that LUTS may arise from factors beyond anatomical enlargement, such as increased smooth muscle tone, bladder dysfunction, and local tissue remodeling6. Among these, bladder outlet obstruction (BOO), which refers to increased resistance to urinary flow at the bladder neck or prostatic urethra, plays a central role, even in small-volume BPH. As a result, surgical interventions, such as transurethral resection of the prostate (TURP), holmium laser enucleation (HoLEP), and green-light photoselective vaporization (PVP), remain key options for symptom relief in patients with BOO7.
TURP has long been regarded as the “gold standard” for treating BPH8. In small-volume BPH, the limited surgical space makes precise resection more challenging; also, the use of electrocautery may increase the risk of thermal injury to surrounding tissue, leading to complications such as bleeding and urethral stricture9. Reich et al.4conducted a multicenter prospective study, reporting the perioperative complications of TURP in patients with small-volume BPH, including postoperative bleeding, transurethral resection syndrome, urethral stricture, and so on. HoLEP, which mimics open surgical enucleation, enables the complete gland removal and is commonly used in patients with large prostates10. Porto et al.11 performed a retrospective study on HoLEP in patients with varying prostate volumes. They found that small-volume BPH (≤ 40 mL) was at a relatively higher risk of developing transient urinary retention after the surgery. Kim et al.12 compared HoLEP and green-light PVP in small-volume BPH and discovered no significant differences in postoperative complications or key outcomes, including International Prostate Symptom Score (IPSS), quality of life (QoL), maximum urinary flow rate (Qmax), and post-void residual urine (PVR). Currently, evidence regarding the safety and efficacy of HoLEP in patients with small-volume BPH (≤ 30 mL) remains limited.
Our study aimed to analyze the applications of TURP, green-light PVP with green laser, and HoLEP in small-volume BPH. We compared the differences among the three in terms of efficacy, safety, recovery, and impact on QoL, thereby providing a basis for clinicians to select the optimal treatment plan.
Methods
Study design
The study was conducted at the Department of Urology, Zhejiang Provincial People’s Hospital, People’s Hospital of Hangzhou Medical College, Hangzhou, Zhejiang, China. All patients with LUTS due to BPH were assessed at our institution from January 1, 2012, to December 31, 2022. All study participants were informed about the planned procedure and asked to sign the informed consent form. The study was approved by the ethics committee of Zhejiang Provincial People’s Hospital. All procedures were conducted in accordance with the Declaration of Helsinki and its amendments.
The inclusion criteria were as follows: prostate size ≤ 30 mL, previous failure of medication therapy (alpha-blockers and 5-alpha reductase inhibitors), or the symptoms significantly impacting the patient’s QoL, coupled with the patient’s strong inclination towards undergoing surgery. The evaluation of all patients included assessments of age, weight, height, hypertension, diabetes mellitus, heart disease, smoking history, drinking history, preoperative indwelling catheterization (≥ 2 weeks), PV, PVR, Qmax, detrusor pressure at Qmax (PedtQmax), cystometric capacity, IPSS, QoL, preoperative prostate-specific antigen (PSA) levels, bladder contractility index, BOO index, detrusor underactivity, detrusor overactivity, and postoperative complications. The postoperative complications were systematically recorded and categorized, including urethrostenosis, neurogenic bladder, bladder neck contracture (BNC), and urinary incontinence (UI). UI was further classified as urinary incontinence with need for drug use (UIND) and urinary incontinence without need for drug use (UIWND).
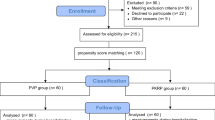
The exclusion criteria were as follows: prostate size > 30 mL, history of prior lower urinary tract surgery, confirmed or suspected prostate cancer, presence of bladder stones or significant bladder diverticula, uncontrolled coagulopathy or inability to discontinue anticoagulant therapy, severe cardiopulmonary impairment precluding safe anesthesia, and incomplete baseline or 3 month follow-up data. Figure 1 presents the flowchart for patient selection, including all exclusions. Patients lacking any baseline laboratory or imaging data were removed from the study cohort in accordance with CONSORT reporting standards. If only 3-month follow-up variables were absent, the study staff attempted telephone or SMS retrieval; when this failed, the case was coded as lost to follow-up.
Surgeon experience and learning curve
In our department, two dedicated surgical teams are responsible for all BPH procedures. Prior to allocating cases to this study, each team completed the required institutional training and surpassed a predefined learning curve (at least 30 independent cases) for TURP, greenlight PVP, and HoLEP. This ensured that all surgeons were fully proficient, minimizing any bias from earlycase inexperience.
Therapeutic regimen
After admission, we completed preoperative assessments (prostate ultrasound, urodynamics, PSA, and blood tests). The anesthesiologists and urologists jointly evaluated comorbidities. Once deemed suitable, patients and urologists engaged in shared decision-making: The benefits and potential complications of all surgical options (TURP, green‑light PVP, and HoLEP) were explained to the patients, after which they signed the informed consent form. Postoperatively, a catheter was inserted and removed following bladder irrigation and a 1-day clamp test. The urinary control, complications, IPSS, and QoL were evaluated during a 3-month follow-up.
Statistical analysis
Descriptive statistical methods were employed to thoroughly analyze the demographic characteristics, clinical features, and postoperative complications of patients undergoing different surgical procedures. Meanwhile, a logistic regression model was used to precisely analyze the risk factors for the occurrence of postoperative UI and BNC. The missing data were assessed and handled accordingly: variables with minimal missingness were included using the pairwise deletion method; variables with substantial missingness were excluded from the regression model to avoid bias. The statistical analysis was accomplished using SPSS 25.0 software (IBM, NY, USA) and the R 4.1.1 programming language.
Results
Demographic characteristics of patients
This study included 645 newly diagnosed patients with BPH (≤ 30mL) at the Zhejiang Provincial People’s Hospital from January 1, 2012, to December 31, 2022. Among these, 85 patients underwent TURP, 417 patients received green-light PVP, and the remaining 143 patients had HoLEP.
Table 1 compares the baseline parameters between the three groups. The Qmax in the TURP group was significantly lower than that in the other two groups. The use of 5α-reductase inhibitors was considerably less in the green-light PVP group than in the TURP group. Significant differences were found in PSA levels and cystometric capacity among the three groups. Decreased PV by TRUS was significantly greater in the HoLEP group compared with the TURP and green-light laser groups. No significant differences were observed in the remaining variables, indicating that the baselines were comparable.
Surgical data and intraoperative/perioperative complications
The data on intraoperative and perioperative complications are presented in Table 2. The surgical and catheter durations were longer in the TURP group compared with the other two groups (P < 0.05). The operative time in the green-light PVP group was longer than that in the HoLEP group. No significant difference was observed in the catheter duration between these two groups. Additionally, no significant difference was observed in perioperative complications among the three groups, with the majority being Clavien–Dindo Grade I.
Postoperative complications and follow-up
The postoperative complications and follow-up data according to the Clavien–Dindo classification are listed in Table 3. The incidence of urethral stricture was higher in the TURP group (7.0%) compared with the green-light PVP (2.6%) and the HoLEP groups (2.8%); however, no significant difference was observed among the three groups. Similarly, the incidence of BNC was higher in the TURP group (9.4%) than in the green-light PVP (4.8%) and the HoLEP groups (5.7%); however, no statistically significant difference was found among three groups.
The number of patients experiencing UI within 3 months after TURP was higher compared with that in the other groups. Specifically, the number of patients with UIWD (14.1%) and UIWND (16.4%) within 1 month after surgery was significantly higher than that in the TURP group. Within 1–3 months after surgery, only the UIWD group had a higher proportion of patients (7.1%) compared with the other two groups. Moreover, the IPSS scores of patients in the TURP group were higher than those in the other two groups during the 3-month postoperative follow-up.
Influential factors of UI and BNC
We conducted a logistic regression analysis to further explore the influencing factors for UI and BNC. Patients with preoperative indwelling urinary catheters were more likely to develop UI after surgery [odds ratio (OR) = 2.44, P = 0.003, Table 4]. In addition, green-light PVP and HoLEP were better at preserving the urinary continence function in patients, resulting in a lower incidence of UI. Compared with patients suffering from detrusor weakness (PdetQmax ≤ 30), those with normal PdetQmax (30 < PdetQmax ≤ 60, OR = 0.44, P = 0.012) or mildly elevated PdetQmax (60 < PdetQmax ≤ 80, OR = 0.49, P = 0.033) had a lower risk of developing UI.
Diabetes (OR = 2.16, P = 0.026) and hematuria/clot retention (OR = 2.51, P = 0.047) were all high-risk factors for the occurrence of BNC(Table 5). Green-light PVP (OR = 0.40, P = 0.034) served as a protective factor for the occurrence of BNC. Although no significant difference in BNC incidence was found between the TURP and green-light PVP groups, the logistic regression still suggested green-light PVP as a protective factor for BNC.
Discussion
BPH is a clinically progressive disorder. The hyperplastic prostate tissue can trigger BOO, which leads to LUTS, exerting a substantial impact on patients’ QoL13. Clinically, drug therapy is initially recommended for small-volume BPH with prominent LUTS, but the compressive effect of the prostate on the urethra is not the dominant factor. Instead, the development of micturition disorders is related to dynamic obstruction, mechanical obstruction, and other factors. Some studies have revealed that there are even more crucial factors such as bladder neck and functional dysregulation, and the efficacy of drug treatment for small-volume BPH is often suboptimal14,15. When drug therapy fails to control the symptoms, surgical intervention is necessary16,17. Currently, the relatively common surgical methods mainly include TURP, green-light PVP, and HoLEP14.
Risk factors for BNC
TURP demonstrates enduring efficacy in enhancing the functionality of small-volume BPH. However, this procedure is associated with surgery-related and postoperative complications, including blood loss, dilutional hyponatremia, hypervolemia, BNC, urethral stricture, retrograde ejaculation, and UI18. Chen et al.19 identified TURP as an independent risk factor for BNC in small-volume prostates, consistent with our findings. Additionally, the inability of TURP to effectively manage certain anatomical factors, such as high tension of the circular fibers at the bladder neck, bladder neck sclerosis, or elevation, further contributes to the occurrence of BNC20,21. The potential mechanisms by which TURP may induce BNC include thermal injury leading to localized tissue necrosis and subsequent inflammatory responses, which can result in fibrosis22. Aberrant collagen deposition during the postoperative healing process may also contribute to the development of BNC23. In contrast, laser-based techniques, including HoLEP and green-light PVP offer more precise tissue ablation with minimal collateral thermal damage, thus potentially reducing the risk of fibrotic complications and preserving the integrity of the bladder neck18,24.
Additionally, postoperative hematuria or clot retention emerged as significant risk factors for BNC in our study. Blood clots exert compressive pressure on local tissue, inducing ischemia and hypoxia. The latter may also act as foreign bodies, triggering an inflammatory cascade and promoting fibrotic proliferation25ultimately leading to contracture. Although Nicholson et al.26 suggested that systemic comorbidities such as hypertension, diabetes, and cardiovascular disease might increase BNC risk, only hypertension was identified as a significant predictor in our cohort.
Risk factors for UI
UI is one of the complications causing maximum worry among patients before surgery and of maximum concern among urologists. Although the mechanism underlying UI remains unclear. At present, the prevailing view is that any damage to the urethral sphincter during the surgical procedure can give rise to sphincter incompetence, thereby triggering the onset of postoperative stress UI27. Regarding the pathogenesis of postoperative urge UI, Zhao et al.28 demonstrated that patients with preoperative terminal detrusor overactivity not only had significantly higher baseline overactive bladder symptom scores (11.0 vs. 8.1 for phasic or no detrusor overactivity, P < 0.05) but were also more likely to report persistent urge UI in three months (42.9% vs. 7.7%, P = 0.037). In this study, the incidence of transient UI, as well as UIND within 3 months after surgery, was higher in the TURP group compared with the green-light PVP or HoLEP group. Although the long-term incidence of UI showed no significant difference among the three procedures, the short-term advantage of PVP and HoLEP in terms of UI prevention highlights their potential value in reducing early-stage complications, thus warranting more in-depth exploration to optimize surgical choices for patients.
As a pivotal determinant governing bladder micturition function, detrusor pressure is intricately and closely related to postoperative UI. Cornwell et al.29, in a single-surgeon HoLEP series, found that a higher preoperative PdetQmax was significantly associated with UI at 6-week follow-up (mean PdetQmax 95 cmH2O in patients with no UI vs. 60 cm H2O in patients with UI, P < 0.01), although this pressure effect diminished by 12 months. In our study, patients presenting with normal or mildly elevated detrusor pressure had a significantly lower risk of postoperative UI compared with those with detrusor weakness. Thus, both our findings and those of Cornwell emphasize that detrusor hemodynamics, whether elevated or diminished, play a crucial role in the development and resolution of early postoperative UI. Patients with detrusor weakness, have difficulty effectively emptying the bladder, leading to an increase in residual urine volume in the bladder and a rise in intravesical pressure, thus triggering overflow UI30. The long-term high-pressure state impairs and destabilizes the function of the bladder detrusor muscle in patients with severely elevated detrusor pressure. After surgery, the detrusor muscle is prone to involuntary strong contractions, with an abnormal urethral sphincter, which results in urge or mixed UI.
Comparison of surgical techniques
The widespread application of medical lasers has led to the rapid adoption of green-light PVP and HoLEP in the treatment of small-volume BPH. A series of studies compared on the application of TURP individually with green-light PVP and HoLEP in the treatment of small-volume BPH9,31,32. In these comparative analyses, both PVP and HoLEP have demonstrated more favorable intraoperative performance; also, the incidence of postoperative complications such as UI and urethral stricture is also lower. However, at present, only one retrospective study has compared the efficacy and safety of PVP and HoLEP in small-volume BPH (< 40 mL), and the high-quality evidence is also lacking12. Our study revealed that green-light PVP and HoLEP yielded similar results in terms of improvements in both subjective and objective parameters.The only difference was in the surgical duration, where HoLEP had an edge. Compared with TURP, HoLEP is not a protective factor for the occurrence of BNC. The incidence of BNC in the HoLEP group was lower than that in the TURP group. However, no significant difference was observed between the two groups, which might be due to the small sample size of the two patient groups. Hypertension, diabetes, and heart disease all could increase the risk of BNC. However, only hypertension was identified as a risk factor for BNC in this study.
Study limitations
The present study had several limitations. First, the relatively small sample sizes in both the TURP and HoLEP groups might have limited the statistical power to detect significant differences between groups, potentially leading to type II errors. Second, the limited follow-up duration restricted our ability to comprehensively observe and evaluate long-term complications, thereby underestimating their true incidence. Third, the retrospective design introduced inherent biases and confounding factors impacting the internal validity of the study. These limitations should be considered when interpreting the generalizability of our findings. Also, future prospective studies with larger cohorts and longer follow-up are warranted to confirm our results.
In summary, although TURP is an effective treatment for small-volume BPH, its association with higher rates of postoperative BNC and short-term UI highlights potential drawbacks compared with minimally invasive laser techniques such as green-light PVP and HoLEP. The varying mechanisms of tissue injury and healing between these approaches, along with patient-related factors such as diabetes, hematuria, detrusor dysfunction, and prolonged catheterization, emphasize the importance of individualized surgical planning. These findings support the use of laser-based procedures as a preferable option for patients at higher risk of complications, thereby facilitating more personalized and safer clinical decision-making. Importantly, integrating shared decision-making into the clinical workflow allows patients to weigh the trade-offs of different surgical techniques based on personalized risk profiles, recovery expectations, and long-term functional outcomes. This patient-centered approach not only improves satisfaction and adherence but also aligns treatment strategies with individual values and preferences. However, further studies are warranted to assess long-term outcomes and compare these established methods with emerging modalities such as aquablation and Rezum water vapor therapy, which may offer additional benefits in managing small-volume BPH.
Conclusions
Greenlight PVP and HoLEP provide comparable symptom relief and improvements in urinary flow for patients with small-volume BPH, with PVP having the shortest operative time. However, TURP is associated with higher rates of BNC and early UI. Detrusor dysfunction, prolonged catheterization, diabetes, and hematuria/clot retention have emerged as key predictors of these complications. Accordingly, laser-based approaches are preferable for patients with small prostates and the aforementioned risk factors. Prospective, long-term studies, ideally including newer options such as aquablation and Rezum, are needed to confirm these findings.
Data availability
The databases used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Enikeev, D. et al. EAU, AUA and NICE guidelines on surgical and minimally invasive treatment of benign prostate hyperplasia: A critical appraisal of the guidelines using the AGREE-II tool. Urol. Int. 106, 1–10. https://doi.org/10.1159/000517675 (2022).
Xiao, N. et al. Small prostate associated with higher incidence of detrusor underactivity and tendency of combination with bladder stone in patients with bladder outlet obstruction. Med. (Baltim). 103, e40451. https://doi.org/10.1097/MD.0000000000040451 (2024).
Lerner, L. B. et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA GUIDELINE PART II-Surgical evaluation and treatment. J. Urol. 206, 818–826. https://doi.org/10.1097/JU.0000000000002184 (2021).
Reich, O. et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J. Urol. 180, 246–249. https://doi.org/10.1016/j.juro.2008.03.058 (2008).
Foo, K. T. What is a disease? What is the disease clinical benign prostatic hyperplasia (BPH)? World J. Urol. 37, 1293–1296. https://doi.org/10.1007/s00345-019-02691-0 (2019).
Kang, M., Kim, M., Choo, M. S., Paick, J. S. & Oh, S. J. Urodynamic features and significant predictors of bladder outlet obstruction in patients with lower urinary tract symptoms/benign prostatic hyperplasia and small prostate volume. Urology 89, 96–102. https://doi.org/10.1016/j.urology.2015.11.027 (2016).
Lee, H. J., Lee, A., Huang, H. H., Sundaram, P. & Foo, K. T. Patients with small prostates and low-grade intravesical prostatic protrusion - A urodynamic evaluation. Asian J. Urol. 4, 247–252. https://doi.org/10.1016/j.ajur.2017.03.003 (2017).
Sandhu, J. S. et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia (BPH): AUA guideline amendment 2023. J. Urol. 211, 11–19. https://doi.org/10.1097/JU.0000000000003698 (2024).
Zhong, J., Feng, Z., Peng, Y., Liang, H. A. & Systematic Review Meta-analysis of efficacy and safety following holmium laser enucleation of prostate and transurethral resection of prostate for benign prostatic hyperplasia. Urology 131, 14–20. https://doi.org/10.1016/j.urology.2019.03.034 (2019).
Yin, L., Teng, J., Huang, C. J., Zhang, X. & Xu, D. Holmium laser enucleation of the prostate versus transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. J. Endourol. 27, 604–611. https://doi.org/10.1089/end.2012.0505 (2013).
Porto, J. G. et al. Is holmium laser enucleation of the prostate truly Size-Independent? A critical evaluation at the extreme ends of the spectrum. Urology 182, 204–210. https://doi.org/10.1016/j.urology.2023.09.002 (2023).
Kim, K. S. et al. Comparison of photoselective vaporization versus holmium laser enucleation for treatment of benign prostate hyperplasia in a small prostate volume. PLoS One. 11, e0156133. https://doi.org/10.1371/journal.pone.0156133 (2016).
Collaborators, G. B. D. B. P. H. The global, regional, and National burden of benign prostatic hyperplasia in 204 countries and territories from 2000 to 2019: a systematic analysis for the global burden of disease study 2019. Lancet Healthy Longev. 3, e754–e776. https://doi.org/10.1016/S2666-7568(22)00213-6 (2022).
Kaplan, S. A. et al. Combination therapy with Doxazosin and finasteride for benign prostatic hyperplasia in patients with lower urinary tract symptoms and a baseline total prostate volume of 25 ml or greater. J. Urol. 175, 217–220. https://doi.org/10.1016/S0022-5347(05)00041-8 (2006). discussion 220 – 211.
McConnell, J. D. et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl. J. Med. 349, 2387–2398. https://doi.org/10.1056/NEJMoa030656 (2003).
Miernik, A. & Gratzke, C. Current treatment for benign prostatic hyperplasia. Dtsch. Arztebl Int. 117, 843–854. https://doi.org/10.3238/arztebl.2020.0843 (2020).
Baboudjian, M. et al. Summary paper on underactive bladder from the European association of urology guidelines on Non-neurogenic male lower urinary tract symptoms. Eur. Urol. 86, 213–220. https://doi.org/10.1016/j.eururo.2024.04.004 (2024).
Elsaqa, M. et al. The incidence of urethral stricture and bladder neck contracture with transurethral resection vs. holmium laser enucleation of prostate: A matched, dual-center study. Can. Urol. Assoc. J. 17, E35–E38. https://doi.org/10.5489/cuaj.7967 (2023).
Chen, Y. H. et al. Risk factors for the postoperative bladder neck contracture in patients with small-volume prostatic hyperplasia. Asian J. Surg. 46, 373–379. https://doi.org/10.1016/j.asjsur.2022.04.076 (2023).
Rosenbaum, C. M. et al. Contemporary outcomes after transurethral procedures for bladder neck contracture following endoscopic treatment of benign prostatic hyperplasia. J. Clin. Med. 10(13), 2884 (2021).
Wu, M. H. et al. Bladder neck contracture following transurethral surgery of prostate: a retrospective single-center study. World J. Urol. 42, 14. https://doi.org/10.1007/s00345-023-04715-2 (2024).
Gao, J. et al. Combined clinical characteristics and multiparametric MRI parameters for prediction of cribriform morphology in intermediate-risk prostate cancer patients. Urol. Oncol. 38, 216–224. https://doi.org/10.1016/j.urolonc.2019.09.002 (2020).
Chung, P. H., Spigner, S., Swaminathan, V., Teplitsky, S. & Frasso, R. Perspectives and experiences of transgender and Non-binary individuals on seeking urological care. Urology 148, 47–52. https://doi.org/10.1016/j.urology.2020.10.026 (2021).
Castellani, D. et al. GreenLight laser photovaporization versus transurethral resection of the prostate: A systematic review and Meta-Analysis. Res. Rep. Urol. 13, 263–271. https://doi.org/10.2147/RRU.S277482 (2021).
Simhan, J., Ramirez, D., Hudak, S. J. & Morey, A. F. J. T Urol. Bladder Neck Contracture 2014 3, 214–220 (2014).
Nicholson, H. L., Al-Hakeem, Y., Maldonado, J. J. & Tse, V. Management of bladder neck stenosis and urethral stricture and stenosis following treatment for prostate cancer. Transl Androl. Urol. 6, S92–S102. https://doi.org/10.21037/tau.2017.04.33 (2017).
Kobayashi, S., Yano, M., Nakayama, T. & Kitahara, S. Predictive risk factors of postoperative urinary incontinence following holmium laser enucleation of the prostate during the initial learning period. Int. Braz J. Urol. 42, 740–746. https://doi.org/10.1590/S1677-5538.IBJU.2015.0477 (2016).
Zhao, Y. R. et al. Predictors of short-term overactive bladder symptom improvement after transurethral resection of prostate in men with benign prostatic obstruction. Int. J. Urol. 21, 1035–1040. https://doi.org/10.1111/iju.12482 (2014).
Cornwell, L. B., Smith, G. E. & Paonessa, J. E. Predictors of postoperative urinary incontinence after holmium laser enucleation of the prostate: 12 months Follow-Up. Urology 124, 213–217. https://doi.org/10.1016/j.urology.2018.11.032 (2019).
Kranzbuhler, B. [Male Incontinence - An overview and its relationship to benign prostatic enlargement]. Ther. Umsch. 80, 133–139. https://doi.org/10.1024/0040-5930/a001426 (2023).
Liu, S. et al. A systematic review and meta-analysis of efficacy and safety comparing greenlight laser vaporization with transurethral resection of the prostate for benign prostatic hyperplasia with prostate volume less than 80 ml. Lasers Med. Sci. 38, 133. https://doi.org/10.1007/s10103-023-03794-2 (2023).
Nguyen, D. D. et al. Operative time comparison of aquablation, greenlight PVP, thulep, greenlep, and holep. World J. Urol. 38, 3227–3233. https://doi.org/10.1007/s00345-020-03137-8 (2020).
Acknowledgements
This study was funded by Medical Scientific Research Foundation of Zhejiang Province (2021KY449) and Zhejiang Medical Association Clinical Research Fund Project (Grant No. 2022ZYC-A01). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Funding
This study was funded by Zhejiang Medical Scientific Research Foundation (Grant No. 2021KY449, to HBW) and Zhejiang Medical Association Clinical Research Fund Project (Grant No. 2022ZYC-A01, to HBW).
Author information
Authors and Affiliations
Contributions
XHH and JM conceived the study, participated in the investigation, and drafted the manuscript. KHX and YKY carried out the data curation and helped to draft the manuscript. XYZ and YFW participated in the data analysis. LQ performed data visualization and validation. DHZ and HBW carried out supervision and writing - review & editing. HBW provided funder for this study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committee of Zhejiang Provincial People’s Hospital. All patients signed informed consent prior to treatment. All procedures were conducted in accordance with the Declaration of Helsinki and its amendments.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hu, X., Miao, J., Xie, K. et al. Clinical comparison of TURP, PVP and holep for small volume BPH. Sci Rep 15, 34751 (2025). https://doi.org/10.1038/s41598-025-18395-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-18395-y