Abstract
The securement of centrally inserted central venous catheters is crucial for their safe use. However, a standardized approach to centrally inserted central venous catheters securement has not been established, and securement methods remain controversial. This study is aimed to compare the safety and efficacy of integrated securement device with suture securement for centrally inserted central venous catheters, analyzing the differences in the incidence rates of catheter-related complications between the two methods, thereby providing evidence to inform clinical decision-making regarding centrally inserted central venous catheter securement strategies. From May to June 2025, 271 hospitalized patients with indwelling centrally inserted central venous catheters at a tertiary hospital in Zhejiang, China, were enrolled in this study. Demographic characteristics and catheter insertion details were collected for all participants on the day of catheter placement. Comfort scores were assessed within 48–72 h post-insertion, and patients were monitored daily until catheter removal for complications including catheter dislodgement (complete or partial), catheter-associated skin injury, and catheter-related bloodstream infection. Chi-square tests and Mann-Whitney U test were used, as appropriate, to compare complication rates between patients managed with the two different securement methods. The enrolled patients had a mean age of 63.46 ± 14.13 years, with a slightly higher proportion of males (57.6%) than females. The majority of catheters were placed in surgical patients (84.5%), with double-lumen catheters predominating (93.4%). Right-sided insertion was the most common approach(97.8%). The mean catheter dwell time was 9.01 ± 4.62 days. No significant differences were observed between the suture cohort and the integrated securement device cohort regarding complete catheter dislodgement, partial catheter dislodgement, or catheter-associated skin injury. Neither cohort experienced catheter-related bloodstream infections. However, the integrated securement device cohort demonstrated higher comfort scores and longer average maintenance intervals compared to the suture cohort, with both differences being statistically significant. The integrated securement device could be suggested as a “safe alternative” to suture securement for centrally inserted central venous catheters stabilization, and simultaneously improves patient comfort, extends maintenance intervals, may reduces nursing workload.
Similar content being viewed by others
Background
Centrally inserted central venous catheters (CICCs) are indwelling devices inserted via the subclavian, jugular, or femoral veins, with the catheter tip positioned within the superior or inferior vena cava1. As an indispensable vascular access tool in clinical practice, CICCs are extensively utilized in critical care and surgical settings for hemodynamic monitoring, chemotherapy administration, parenteral nutrition support, and prolonged antibiotic therapy2,3. The use of CICCs effectively reduces the need for repeated venipuncture and vascular damage. According to 2025 market projections, the global CICC market is poised for substantial growth, with an estimated compound annual growth rate of 6.6%. The market value is anticipated to rise from USD 3.09 billion in 2025 to nearly USD 5.86 billion by 2035, primarily driven by demand in intensive care unit (ICU), oncology wards, and emergency departments4. However, the frequent use of CICCs is accompanied by complications, among which catheter dislodgement is a commonly reported adverse event. Studies have consistently identified CICCs as having the highest dislodgement rate compared to other central venous access devices, such as peripherally inserted central catheters, both in pediatric oncology patients and hospitalized adults5,6. Inadequate securement can lead to catheter accidental dislodgement, causing treatment interruptions, the need for catheter reinsertion, and associated complications. Such incidents not only compromise the quality of healthcare and increase medical costs but also impose unnecessary operational burdens on clinical staff. More critically, they pose life-threatening risks to patients and may trigger medical disputes. Therefore, implementing appropriate securement methods to maintain CICC stability should not be neglected in clinical practice, ensuring safe catheter retention and utilization.
In the selection of securement methods, suture has been regarded as the ‘gold standard’ for CICCs. In China, suture-based securement remains the predominant clinical practice for CICC stabilization. A nationwide survey revealed that 66.51% of ICU in Chinese tertiary hospitals utilize suture securement7. Moreover, data from secondary and tertiary hospitals at the provincial level demonstrated an even higher adoption rate of 98%8. Previous studies have explored various suture securement techniques to enhance catheter stability and safety9,10. However, the associated risks demand critical attention, including needlestick injuries, biofilm formation, infection, skin integrity compromise, and patient discomfort11. Suture securement may disrupt the local cutaneous microenvironment. Moreover, this technique necessitates securing the catheter by suturing through the wings of a butterfly fixation device to the skin, creating a concealed interface beneath the clamp that compromises disinfectant penetration during antisepsis procedures. This may lead to bacterial colonization, thereby elevating the risk of catheter-related bloodstream infections (CRBSI). Additionally, suture breakage caused by patient movement may also weaken the securement effect and increase the difficulty and time of the nurse’s operation when removing the catheter9.
Within this context, the Infusion Nursing Society (INS) Standards of Practice for Infusion Therapy recommend supplemental securement methods as alternatives to suture securement, such as adhesive securement device (ASD), subcutaneous anchor securement system (SASS), sutureless securement devices (SSD), or tissue adhesive (TA)11. Each securement method exhibits distinct advantages and limitations. TA significantly enhances dressing durability compared to SSD, reducing dressing change frequency and patient discomfort12. However, the use of TA may increase the risk of skin irritation or damage and the rate of failed catheter securement12,13. Besides, a study conducted in patients with peripherally inserted central catheters(PICCs) demonstrated that ASD demonstrate higher CRBSI incidence versus SASS14. The Integrated Securement Device (ISD), recommended by the INS standard, combines dressing and securement functions. It features a transparent, semipermeable window and a bordered fabric collar with built-in securement technology, such as chlorhexidine gluconate (CHG) dressings11. A pilot randomized controlled trial conducted in adult ICU demonstrated that ISD achieved the lowest securement failure rate compared to SSD, standard care, and TA groups15. Although these sutureless securement methods offer advantages in reducing tissue trauma and enhancing procedural efficiency, concerns regarding their long-term stability persist among clinicians. Inadequate adhesive strength may result in catheter dislodgement due to patient movement, perspiration, or skin sebum production. Furthermore, evidence comparing the efficacy and complication rates of various securement methods remains limited, preventing consensus on optimal CICC stabilization strategies. This prospective cohort study investigates the incidence of catheter dislodgement and other related complications in CICCs secured by suture securement versus ISD. The findings aim to establish clinical evidence for CICC stabilization strategies, while also expected to provide partly complication incidences information for different securement techniques.
Methods
A prospective cohort study was conducted at a tertiary hospital in Zhejiang, China, between May and June 2025, to compare the incidence of complications associated with different CICC securement methods. Two cohorts were recruited: one comprised patients whose CICCs were inserted and secured by anesthesiologists using subcutaneous sutures combined with sterile transparent dressings, while the other consisted of patients whose CICCs were inserted and secured by the Vascular Access Specialist Team (VAST) using ISD (CHG dressings).There are 10 VAST members and 12 anesthesiologists who perform this procedure.
Participants
Participants were recruited using convenience sampling from hospitalized patients with indwelling CICCs. Inclusion criteria were as follows: ①Age ≥ 18 years; ②Hospitalized patient with an indwelling CICC; ③Intact skin at the intended catheter insertion site prior to placement; ④Voluntary participation with signed informed consent. Exclusion criteria were:① CICC inserted via the femoral vein; ②Known allergy to CHG or sterile transparent dressings; ③Patients with cognitive impairment. Withdrawal criteria included:①Participant voluntarily withdrew from the study; ②CICC dwell time < 3 days; ③Development of altered cognitive function (e.g., delirium, agitation) during catheterization due to changes in clinical status.
Sample size
The sample size for this study was calculated using the formula for comparing two independent proportions. With the significance level (α) set at 0.05 and the power (1-β) at 80% (β = 0.2), baseline complication rates were derived from the literature: p₁ = 2% (intervention group) and p₂ = 12% (control group)16. The initial calculation indicated a required sample size of 99 participants per group. To accommodate the study design and an anticipated attrition rate of 20%, the target sample size was increased to 119 participants per cohort, resulting in a total sample size of 238 participants.
Variables
Socio-demographic variables
Age, gender, education level, and marital status.
Catheter insertion variables
History of catheterization, intended use of the catheter, insertion site, number of lumens, length of the inserted catheter, and catheter dwell time.
Primary outcome
Dislodgement: Complete dislodgement means CICC completely leaves the vein, and partial dislodgement refers to CICC migrating outward from its original position by 1 centimeter or more15,17.
Secondary outcomes
CRBSI Diagnosed if the same organism is isolated from a blood culture and the tip culture and the quantity of organisms isolated from the tip is greater than 15 colony forming units11.
Catheter-associated skin injury(CASI): An abnormality including, but not limited to, erythema, vesicle, bulla, erosion or tear, at a peripheral or central vascular access device (VAD) site that is noted in the area of the device dressing and/or securement device and that is observable for 30 min or more after dressing/securement removal11.
Comfort score: Assessed at 48–72 hours post-catheterization using a 10-cm Visual Analogue Scale. Patients marked a vertical Line on the 10-cm VAS ruler anchored by ‘worst imaginable discomfort’ (0 cm) and ‘complete comfort’ (10 cm), with higher scores indicating greater comfort.
Average maintenance intervals: Calculated by dividing the catheter dwell time by the number of maintenance procedures performed during the indwelling period.
Data collection
The research team underwent training to ensure clarity on the study’s purpose and to standardize the definitions of complications. Data collection began at the time of catheter insertion and continued daily by designated research team members until participants’ CICCs were removed. Comfort scores were specifically collected at 48-72h post-insertion.
Quality control
Before the study began, all operators responsible for CICC insertions completed training on standard operating procedures and underwent competency assessments in catheter securement techniques, ensuring procedural consistency among all participants. Concurrently, surgical ward nurses who might manage CICC patients received training on dressing change protocols and criteria for assessing complications to standardize catheter maintenance throughout the dwell time. The standard procedure for dressing change was every 7 days, with immediate replacement required upon detection of exudate or bleeding. Additionally, two trained research assistants conducted daily follow-ups. The pre-study training provided them with definitions and criteria for recognizing catheter-related complications, a follow-up schedule, and data collection protocols (including daily monitoring for complications, and recording of catheter maintenance time, removal time, and removal reasons). We conducted calibration exercises to ensure at least 90% inter-rater agreement in the identification of complications. The principal investigator performed systematic daily verification of all recorded data to ensure its completeness and accuracy.
Statistical analysis
Data entry and statistical analyses were performed using Excel and IBM SPSS Statistics software (version 26.0). Categorical data are presented as frequencies and percentages, whereas continuous data are expressed as means and standard deviations (SDs). The chi-square test was used to compare complication rates, comfort scores and average maintenance intervals between the two cohorts. A p-value of less than 0.05 was considered significant differences.
Results
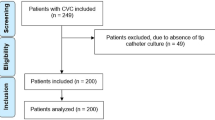
A total of 299 participants were initially enrolled, with 156 in the ISD cohort and 143 in the suture-securement cohort. During the study period, 28 participants were withdrawn: 26 due to a catheter dwell time of ≤ 2 days, and 2 due to the development of delirium following clinical deterioration. Consequently, 271 participants completed the study and were included in the final analysis (Fig. 1).
Socio-demographic and catheter insertion characteristics
The mean age of the participants was 63.46 ± 14.13 years; males (57.6%) slightly outnumbered females; a history of catheterization was present in 11.1% of the participants; the majority of catheters (84.5%) were placed for surgical patients; double-lumen CICCs constituted the predominant type (93.4%), and the right side was the most common insertion site (97.8%); the mean catheter dwell time was 9.01 ± 4.62 days. Significant differences (p < 0.05) were observed between the two groups regarding intended catheter use, number of lumens, inserted catheter length, and catheter dwell time (Table 1).
Primary outcome analysis
During the catheter indwelling period, the rate of complete dislodgement was 1.6% in the suture cohort, with no cases of partial dislodgement. In the ISD cohort, the rates of complete and partial dislodgement were 2.1% and 0.7%, respectively. The Chi-square test results indicated no significant difference between the two cohorts (Table 2).
Secondary outcomes analysis
No CRBSI occurred in either cohort, and no CASI occurred in the suture cohort, while the CASI incidence in the ISD cohort was 1.4%. The Chi-square test results indicated no significant difference in CASI incidence between the cohorts. Comfort scores were 9.22 ± 1.247 for the suture cohort and 9.64 ± 0.662 for the ISD cohort. Average maintenance intervals were 3.53 ± 1.80 days and 5.21 ± 1.99 days, respectively. The Chi-square test revealed significant differences between the two cohorts for both comfort scores and average maintenance intervals (Table 2).
Discussion
ISD demonstrates comparable safety to suture securement, with no increased risk of catheter dislodgement
Catheter dislodgement is a recognized complication associated with CICCs. It not only compromises the security of the line but also subjects patients to the distress of reinsertion and potential further trauma at the insertion site, constituting a secondary injury. Furthermore, it hampers the overall treatment progress and, in severe cases, can lead to life-threatening consequences. Therefore, selecting securement devices requires careful consideration of their efficacy. Current practices for catheter securement exhibit significant global variation. Polyurethane dressings with ISD are more prevalent in high-income countries, while sterile gauze and tape dressings, alongside chlorhexidine-impregnated dressings, are more commonly utilized in middle-income countries18. However, comparative research on the effectiveness of suture securement versus ISD is limited. A pilot randomized controlled trial conducted by Marion et al.15 suggested that suture securement might be more effective than ISD in reducing dislodgement rates. Nevertheless, this study was constrained by a small sample size of only 30 participants per group, rendering it insufficiently powered to test statistical hypotheses. Suture securement has been regarded as the cornerstone for preventing catheter dislodgement in China due to its physical anchoring effect, and it remains the predominant securement method19. Our study, leveraging a substantially larger and adequately powered sample, demonstrates that well-engineered ISD can achieve stability equivalent to that of sutures. This finding holds significant promise for transforming clinical securement practices. Transitioning to sutureless securement methods could eliminate inherent risks associated with sutures, including needlestick injuries, suture-related infections, and patient discomfort or pain. Furthermore, sutureless securement is considerably simpler and faster to perform, saving time for the operator. Therefore, when equivalent securement efficacy is assured, sutureless securement represents a safer and more efficient approach.
ISD enhances patient comfort, extends maintenance intervals
ISD provided significantly greater patient comfort than suture securement in this study, as evidenced by higher comfort scores. Given the high mobility of the neck region, sutures used in traditional securement are prone to tension during movement, causing discomfort (pain and a foreign body sensation) that compromises daily activities and rest. The ISD used in this study mitigated these problems through improved skin conformity, substantially reducing tension-related discomfort. This advantage in comfort was especially pronounced among patients requiring frequent maintenance or prolonged catheterization.
Furthermore, ISD exhibited superior performance in decreasing the necessity for additional dressing changes. This is likely due to its exudate absorption and anti-infection properties, indicating that replacement is only required when blood or fluid seepage reaches a certain level. For nursing staff, ISD reduces the frequency of dressing changes and prolongs catheter maintenance intervals. This decreases the risk of local contamination at the puncture site and potential skin damage associated with frequent manipulation, thereby lowering infection risk and further enhancing patient safety20. Furthermore, the elimination of suture removal during catheter removal simplifies the removal process, reducing the nursing workload. These improvements in maintenance schedules and procedural workflows allow nursing staff to allocate more time and resources to other critical aspects of patient care. Simultaneously, from an economic perspective, reduced consumable usage and labor costs promote the rational allocation and utilization of healthcare resources. Although our study did not conduct a formal cost analysis and cannot provide specific cost-saving figures, existing evidence supports potential economic benefits. For instance, a cost modeling assessment of Tegaderm™ CHG dressing conducted by the UK National Institute for Health and Care Excellence Medical Technologies Advisory Committee demonstrated savings of £77.26 per patient compared to standard dressings, representing a 98.5% cost reduction21. Similarly, a cost-benefit analysis conducted by Maunoury et al.22, which utilized a health economic model, found that CHG dressings are more cost-effective than transparent dressings. Future research specifically evaluating the costs associated with these devices is warranted to quantify their precise economic contribution and provide robust data to inform optimal healthcare resource allocation.
No significant difference was observed in the rates of CRBSI and CASI between suture securement and ISD securement
CRBSI is a serious complication of CICC. A study conducted across 41 countries in Asia, Africa, Eastern Europe, Latin America, and the Middle East over 24 years reported a pooled Central Line–Associated Blood Stream Infections (CLABSI) rate of 4.82 per 1000 catheter-days23. CLABSI associated with CICC not only compromises the utility of the catheter but also increases the healthcare burden and can lead to patient mortality. A multicenter study in Australia found a CLABSI rate of 5.3% for CICCs, identifying it as a primary cause of catheter failure6. Singhal et al.24 revealed that the mortality rate among adult ICU patients with CLABSI in India could be as high as 45%. In China, studies indicate that the average hospitalization cost for patients with CLABSI in the ICU was $67,923, nearly double that of the control group25. In non-ICU wards, total healthcare expenditures were 76% higher for CLABSI patients compared to those without CLABSI and after controlling for relevant risk factors, CLABSI was associated with a 2.27-fold increased risk of death26. In this study, five catheters from the suture securement cohort and six from the ISD securement cohort were removed due to fever, with all corresponding blood and catheter tip cultures yielded negative results. Our study demonstrated no significant difference in CLABSI rates between suture securement and ISD securement, despite previous studies have suggested that suture securement may increase the risk of CLABSI27,28. However, it’s worth noting the ISD securement cohort exhibited longer catheter dwell time than the suture securement cohort. The catheter dwelling time is a recognized risk factor for CLABSI29,30, with a study indicating a 4% increased risk per additional catheter-day23. This observation, when considered alongside CLABSI rates, suggests that chlorhexidine gluconate (CHG) dressings may play a beneficial role in reducing infection risk, which is consistent with previous studies31,32,33.
While some studies report an association between CHG dressings and an increased risk of skin injury21, our study observed a low incidence of such events. This discrepancy may be attributable to our limited sample size. Furthermore, chlorhexidine gluconate is an antiseptic agent, and prolonged exposure can lead to dermatitis, meaning long-term use may increase the risk of dermatitis and related skin injuries34. Our inclusion criterion, which restricts enrollment to patients with CICCs that have a Limited dwelling time of no more than 1 month, and patients involved in this study only had a mean dwelling time of 9.50 ± 4.10 days, potentially reducing the detection rate for skin injuries. Compared with other central venous access devices, the duration of local skin exposure in CICCs was relatively short, possibly contributing to the lower observed rate of skin complications. Based on the demonstrated infection prevention benefits and the manageable skin risk profile observed in this cohort with typical CICC dwelling times, CHG dressings could be considered a standard practice for CICC securement.
Study limitations
Naturally, this study has limitations. First, as a single-center investigation, the results should be interpreted with caution regarding generalizability; future multi-center studies with larger samples are warranted for further validation. Second, the influence of individual patient factors (e.g., severe obesity, profuse sweating, poor skin condition) on securement efficacy requires deeper investigation within larger cohorts. Future research should further explore the applicability of ISD in complex clinical scenarios (e.g., agitated ICU patients) and conduct cost-effectiveness analyses comparing ISD with suturing.
Conclusion
As a prospective cohort study conducted in a real-world setting, this research enrolled a diverse patient population—including individuals with varying ages and BMIs—to compare the impact of ISD securement versus conventional suturing on CICCs dislodgement rates. This design enhances the generalizability and external validity of our findings. Our data suggest ISD may be a safer option and that ISD could be suggested as a “safe alternative” to suture. This challenges the traditional paradigm that “sutures are the gold standard for preventing catheter dislodgement,” providing crucial evidence-based support for clinical practice.
Data availability
All data and materials are included in this published article.
Abbreviations
- CICCs:
-
Centrally inserted central venous catheters
- ICU:
-
Intensive Care Unit
- CRBSI:
-
Catheter-related Bloodstream Infections
- INS:
-
Infusion Nursing Society
- ASD:
-
Adhesive Securement Device
- SASS:
-
Subcutaneous Anchor Securement System
- SSD:
-
Sutureless Securement Devices
- TA:
-
Tissue Adhesive
- ISD:
-
Integrated Securement Device
- CHG:
-
Chlorhexidine Gluconate
- CASI:
-
Catheter-associated Skin Injury
- SD:
-
Standard Deviation
References
Kolikof, J., Peterson, K., Williams, C. & Baker, A. M. Central Venous Catheter Insertion. (2025).
Boulet, N., Muller, L., Rickard, C. M., Lefrant, J. Y. & Roger, C. How to improve the efficiency and the safety of real-time ultrasound-guided central venous catheterization in 2023: a narrative review. Ann. Intensive Care 13(1), 46 (2023).
Chinese Abdominal Intensive Care Association ASOE. Chinese expert consensus on management of central venous catheters for critically ill patients (2022 edition). Chin. J. Dig. Surg. 21 (3), 313–322 (2022).
Insights, F. M. Central Venous Catheter Market Size and Share Forecast Outlook 2025 to 2035 (2025).
Nunn, J. L. et al. Central venous access device adverse events in pediatric patients with cancer: a systematic review and meta-analysis. Support Care Cancer 32(10), 662 (2024).
Corley, A. et al. Incidence and risk factors for central venous access device failure in hospitalized adults: A multivariable analysis of 1892 catheters. J. Hosp. Med. 19(10), 905–917 (2024).
Fei, P., Yangyang, L., Fang, W., Yao, J. & Meng, C. The nursing prevention and control of central Line-Associated blood stream infections in ICUs of tertiary grade A hospitals. Chin. Nurs. Manage. 24 (1), 24–29 (2024).
Yang, S. et al. Prevention and control status of central line-associated bloodstream infection in intensive care unit in Shandong province: a cross-sectional survey analysis. Chin. Crit. Care Med. 36 (12), 1315–1320 (2025).
Ahmad, S. S., Hajela, K. & Mammen, A. M. Securing central venous catheters: PT fixation technique. Ann. Card Anaesth. 25(2), 244–246 (2022).
Khavanin, Z. M. et al. Skin fold technique for central venous catheter fixation; comparison with conventional method for postopration infections. Med. J. Islam Repub. Iran. 30, 419 (2016).
Nickel, B. et al. Infusion Therapy Standards of Practice, 9th edition. J Infus Murs 47(1S Suppl 1), S1–S285 (2024).
Xu, H. et al. The effectiveness of dressings and securement devices to prevent central venous catheter-associated complications: A systematic review and meta-analysis. Int. J. Nurs. Stud. 149, 104620 (2024).
Hawes, M. L., McCormick, C. A. & Gilbert, G. E. A retrospective study of subcutaneous anchor securement systems in oncology patients. J. Vasc Access. 25(6), 1848–1852 (2024).
Rowe, M. S., Arnold, K. & Spencer, T. R. Catheter securement impact on PICC-related CLABSI: A university hospital perspective. Am. J. Infect. Control 48(12), 1497–1500 (2020).
Mitchell, M. L. et al. Central venous access device securement and dressing effectiveness: the CASCADE pilot randomised controlled trial in the adult intensive care. Aust Crit. Care 33(5), 441–451 (2020).
Li, Q., Cheng, H. & Hui, D. Comparative study of two in vitro fixation methods for central venous catheterization (CVC). J. Chin. Res. Hosp. 6 (5), 48–51 (2019).
Fitzsimons, K. M. et al. An observational study of the securement of central venous access devices with a subcutaneous anchor device in a paediatric population at a tertiary level hospital. J. Vasc. Access. 21 (6), 959–962 (2020).
Hyun, A. et al. Central venous access device management for children undergoing treatment for blood disorders and cancer: a descriptive international cross-sectional survey. Support Care Cancer 33(3), 179 (2025).
Miaomiao, Y. et al. Usage and management of central venous vascular access in hematology departments of 48 hospitals. Chin. J. Nurs. 59 (11), 1310–1318 (2024).
Medicine, C. S. O. C. Practice guideline on the prevention and treatment of central line associated bloodstream infection in 2025. Chin. Crit. Care Med. 37 (3), 193–220 (2025).
Jenks, M. et al. Tegaderm CHG IV securement dressing for central venous and arterial catheter insertion sites: A NICE medical technology guidance. Appl. Health Econ. HEA 14(2), 135–149 (2016).
Maunoury, F. et al. Cost-Effectiveness analysis of a transparent antimicrobial dressing for managing central venous and arterial catheters in intensive care units. PLOS ONE. 10 (6), e130439 (2015).
Rosenthal, V. D. et al. Multinational prospective study of incidence and risk factors for central-line-associated bloodstream infections in 728 intensive care units of 41 Asian, African, Eastern European, Latin American, and middle Eastern countries over 24 years. Infect Cont. Hosp. EP: 1–11 (2023).
Singhal, T., Shah, S., Thakkar, P. & Naik, R. The incidence, aetiology and antimicrobial susceptibility of central line-associated bloodstream infections in intensive care unit patients at a private tertiary care hospital in mumbai, India. Indian J. Med. Microbi 37(4), 521–526 (2019).
Zhang, Y. et al. Incidence rate, pathogens and economic burden of Catheter-Related bloodstream infection: A Single-Center, retrospective Case-Control study. Infect. Drug Resist. 16, 3551–3560 (2023).
Stevens, V. et al. Inpatient costs, mortality and 30-day re-admission in patients with central-line-associated bloodstream infections. Clin. Microbiol. Infec 20(5), O318–O324 (2014).
Yamamoto, A. J. et al. Sutureless securement device reduces complications of peripherally inserted central venous catheters. J. Vasc Interv Radiol. 13(1), 77–81 (2002).
Molina-Mazón, C. S., Martín-Cerezo, X., Domene-Nieves, D. L. V. G., Asensio-Flores, S. & Adamuz-Tomás, J. Comparative study on fixation of central venous catheter by suture versus adhesive device. Enferm Intensiva (Engl Ed). 29 (3), 103–112 (2018).
Moriyama, K. et al. Risk factors associated with increased incidences of catheter-related bloodstream infection. Medicine 101(42), e31160 (2022).
Lafuente, C. E. et al. Risk factors of catheter- associated bloodstream infection: systematic review and meta-analysis. PLOS ONE. 18 (3), e282290 (2023).
Xu, H., Zhu, M., Xu, S. & Bian, L. Improving central venous catheter care with chlorhexidine gluconate dressings: evidence from a systematic review and Meta-analysis. J. Health Popul. Nutr. 43(1), 177 (2024).
Puig-Asensio, M. et al. Effectiveness of chlorhexidine dressings to prevent catheter-related bloodstream infections. Does one size fit all? A systematic literature review and meta-analysis. Infect. Cont. Hosp. EP 41(12), 1388–1395 (2020).
Yueliang, C. et al. Meta-Analysis on the effectiveness of chlorhexidine gluconate dressing for preventing Catheter-Related bloodstream infections in adult ICU patients. Chin. J. Emerg. Med. 26 (12), 1461–1464 (2017).
Liippo, J., Kousa, P. & Lammintausta, K. The relevance of chlorhexidine contact allergy. Contact Dermat. 64 (4), 229–234 (2011).
Acknowledgements
We sincerely thank all patients participated in the study, and all members of our study team.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Yilin Chen: Designed the experiments and wrote the manuscript; Xianghua Chen: Data collection; Xianghong Jin: Data collection; Xufen Zeng: Analyse the data; Xiuzhu Cao: Quality control; Linfang Zhao: Project management and revised the paper. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
Prior to commencement, this study received ethical approval (Approval No. 20250401) from the Sir Run Run Shaw Hospital Ethics Committee. Before the study began, all of the participants were informed about the purpose and process of the study, and their participation was voluntary. The guidelines of the Declaration of Helsinki (World Medical Association, 2013) were followed throughout this study. Written informed consent was obtained from all of the included participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, Y., Chen, X., Jin, X. et al. Compare the safety and efficacy of integrated securement device versus suture securement for centrally inserted central venous catheters: a prospective cohort study. Sci Rep 15, 34907 (2025). https://doi.org/10.1038/s41598-025-18777-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-18777-2