Abstract
Mild cognitive impairment (MCI) is a prodromal stage of dementia, and its early detection is critical for improving clinical outcomes. However, current diagnostic tools such as brain magnetic resonance imaging (MRI) and neuropsychological testing have limited accessibility and scalability. Using machine-learning models, we aimed to evaluate whether multimodal physical and behavioral measures, specifically gait characteristics, body mass composition, and sleep parameters, could serve as digital biomarkers for estimating MCI severity. We recruited 80 patients diagnosed with MCI and classified them into early- and late-stage groups based on their Mini-Mental State Examination scores. Participants underwent clinical assessments, including the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet Korean Version, gait analysis using GAITRite, body composition evaluation via dual-energy X-ray absorptiometry, and polysomnography-based sleep assessment. Brain MRI was also performed to obtain structural imaging data. We evaluated the classification performance across various models, including support vector machines, random forest, multilayer perceptron, and convolutional neural network, using unimodal and multimodal datasets. Machine learning models trained on physical and behavioral data alone achieved a high classification accuracy (AUC up to 94%), comparable to that of MRI-based models, in differentiating early- and late-stage MCI. Combining physical and behavioral and MRI features yielded marginal improvements in the prediction performance. Gait velocity, lean body mass, and sleep efficiency were among the top predictors of cognitive function. Multimodal digital biomarkers or multimodal physical and behavioral signals can effectively estimate MCI severity and may offer a scalable, low-cost approach for early detection and monitoring of cognitive decline in real-world settings.
Similar content being viewed by others
Introduction
Mild cognitive impairment (MCI) refers to a stage of cognitive decline that precedes dementia and is characterized by noticeable cognitive impairment while maintaining the ability to perform daily activities1. In clinical practice, the ability of patients with MCI to preserve daily functioning despite cognitive deterioration is closely linked to their quality of life and long-term prognosis. Consequently, the early detection of cognitive decline is essential, as it facilitates timely treatment and improves patient outcomes.
Recent advances in digital technology have enabled the measurement of individualized health data using wearable and mobile devices, thereby facilitating real-time health monitoring. As the interest in preventive healthcare grows, there is increasing research on the use of digital tools to measure health indicators for the assessment and prediction of various health conditions. Standardized neuropsychological tests provide relatively accurate assessments of cognitive function. However, these tests are time intensive, typically requiring 1.5 to 2 h—and are not conducive to continuous or real-time monitoring2.
Given these limitations, there is growing interest in identifying digital biomarkers that allow for simpler and more accessible assessments of cognitive status3. A well-designed health indicator is a critical tool for assessing an individual’s health status, and selecting appropriate indicators based on specific objectives is critical for effective assessment4. Health indicators encompass a wide range of factors, including clinical and physical and behavioral measures, as well as socioeconomic and behavioral components. Among these, physical and behavioral measures that are objective, quantifiable, and easily obtainable in everyday life are particularly promising for digital cognitive assessment.
In this study, we focused on three non-imaging physical and behavioral measures—gait, body composition, and sleep—which have been previously associated with cognitive function5,6,7. Compared to imaging-based markers, which are widely used in research but remain costly and less accessible, these measures offer a practical alternative. Therefore, we aimed to investigate whether these easily measurable health indicators could serve as digital biomarkers for predicting the degree of cognitive decline and reflect structural changes in the brain.
Methods
Participants
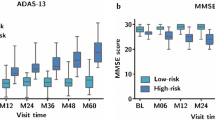
We prospectively recruited 80 patients with MCI at Chuncheon Sacred Heart Hospital between October 2020 and April 2021. The inclusion criteria were as follows: (a) age 40–100 years; (b) patients with MCI met the diagnostic criteria for minor neurocognitive disorder according to the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-V); (c) absence of dementia as assessed by physicians; and (d) a Clinical Dementia Rating (CDR) global score of 0.5, with a memory domain score ≥ 0.5. The exclusion criteria were as follows: (a) severe illness with an anticipated fatal outcome within 3 months, (b) language barrier, (c) deafness or blindness, and (d) inability to provide informed consent. Patients were classified into two groups based on their Mini-Mental State Examination (MMSE) scores: (a) late-stage MCI, defined as performance more than 1.5 standard deviation (SD) below the normative mean; and (b) early-stage MCI, defined as performance ≥ 1.5 SD below the normative mean. Written informed consent was obtained from each participant, and the study protocol was approved by the Institutional Review Board (IRB) of Chuncheon Sacred Heart Hospital (IRB number: Chuncheon 2020–09-005). The study was conducted in accordance with the Declaration of Helsinki, and all methods were performed in accordance with the relevant guidelines and regulations.
Clinical assessment
The demographic data (age, sex, and years of education) and anthropometric measurements (height, weight, and waist circumference) were recorded. Blood pressure was measured and laboratory tests, including fasting glucose and total cholesterol levels, were conducted. Participants completed scales assessing depression (Short Form of Geriatric Depression Scale, SGDS), anxiety (Korean Geriatric Anxiety Inventory, K-GAI), and quality of life (Geriatric Quality of Life Dementia, GQOL-D). Additionally, information of health behaviors and medical comorbidities was obtained using the questionnaire from the Korean National Health and Nutrition Examination Survey (KNHANES). Information on other medical comorbidities was obtained during in-clinic interviews. The comorbidities considered in this study included diabetes mellitus, hypertension, dyslipidaemia, heart disease, stroke, liver disease, depression, kidney disease, pulmonary disease, arthritis, chronic gastrointestinal disease, cancer, and fractures.
Cognitive function assessment
All participants underwent the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet, Korean version (CERAD-K) and the Short Blessed Test (SBT-K)8,9 for cognitive evaluation. The CERAD-K consists of Verbal Fluency, the Boston Naming Test, the Mini-Mental State Examination Korean version (MMSE-KC)10, Word List Memory, Constructional Praxis, Word List Recall, Word List Recognition, Constructional Praxis Recall, and the Trail Making Test (Parts A and B)10,11. All cognitive assessments were conducted during the participant’s two-day hospital stay, either on the same day or within one day before/after the gait, sleep, MRI, and body composition measurements.
Gait assessment
Gait was assessed using GAITRite instrumentation (CIR systems Inc., Havertown, PA, USA), which consists of a 5.6 m long and 0.9 m wide electronic walkway. Each patient was instructed to walk across the walkway at a normal pace without gait aid in a single pass. The study coordinator observed each patient’s gait without any interference. Gait features, including spatial (stride and step length), temporal (gait speed, step count, cadence, and stance time), and spatiotemporal (cadence) parameters, were analyzed.
Body composition assessment
Body composition, including body fat percentage and appendicular skeletal muscle mass, was assessed using dual-energy X-ray absorptiometry (DXA; Lunar, GE Healthcare, Fairfield, CT, USA).
Sleep assessment
Polysomnography (PSG) was performed using the Nox A1 device (Nox Medical, Reykjavik, Iceland). Sleep stage and respiratory events were scored according to the American Academy of Sleep Medicine guidelines12,13. The following sleep parameters were assessed: total sleep time (TST), sleep efficiency (TST/time in bed × 100), sleep stage (N1, N2, N3, and R), oxygen desaturation index (ODI), apnea index (AI), hypopnea index (HI), and apnea–hypopnea index (AHI). Definitions of oxygen desaturation, apnea, and hypopnea followed standard guidelines, and the indices were computed for each participant.
MR imaging techniques
Standardized T2 fluid-attenuated inversion recovery (FLAIR) and three-dimensional (3D) T1-weighted images were acquired using a 3.0 T MRI scanner (Skyra, Siemens Healthineers, Erlangen, Germany) at the Chuncheon Sacred Heart Hospital. T1-weighted structural brain images were obtained using a magnetization-prepared rapid acquisition gradient echo (MPRAGE) sequence with the following parameters: sagittal slice thickness, 1.0 mm (no gap); repetition time (TR), 2300 ms; echo time (TE), 2.98 ms; flip angle, 9°; inversion time (TI), 900 ms. FLAIR images were acquired with an axial slice thickness of 2 mm, TR of 11,000 ms, TE of 125 ms, and a flip angle of 90°.
Gray matter measurements
The total volume and other morphometric features of the grey matter (average cortical thickness [ThickAvg], standard deviation of cortical thickness [ThickStd], mean curvature [MeanCurv], Gaussian curvature [GausCurv], folding index [FoldInd], and curvature index [CurvInd]) were measured using 3D Slicer (version 4.11) and FreeSurfer (version 7.1.1). Cortical parcellation was conducted using the Desikan–Killiany atlas (lh.aparc.annot and rh.aparc.annot for the left and right hemispheres, respectively)14, and each hemisphere was divided into 34 distinct cortical regions (68 regions in total). The subcortical structures were segmented based on 3D T1-weighted MRI data.
White matter hyperintensity measurements
White matter hyperintensities (WMH) were quantified using the Brain Intensity Abnormality Classification Algorithm (BIANCA) software within the FMRIB Software Library (FSL). FLAIR MRI images were used for the segmentation and classification of the WMH. The non-default settings included a lesion model trained using the MICCAI WMH segmentation challenge dataset. Features derived from WMH segmentation included the total WMH volume, periventricular WMH, and deep WMH volumes, which were further categorized by the four lobes of the brain.
Datasets for machine learning
Data on gait characteristics, body composition, sleep, and MRI scans were collected at baseline. The following unimodal datasets were created: (a) Gait Dataset: derived from GAITRite (74 features per participants); (b) Gray Matter Dataset: derived from MRI (476 features per participant); (c) White Matter Dataset: derived from MRI (27 features per participant); (d) Body Composition Dataset: derived from DXA (37 features per participant); (e) Sleep Dataset: derived from polysomnography (12 features per participant). Three multimodal datasets were constructed by combining the following unimodal datasets: Gait + Sleep + Body Composition, Gray Matter + White Matter Hyperintensity, and Gait + Sleep + Body Composition + Gray Matter + White Matter Hyperintensity. Machine learning analyses were conducted on these multimodal datasets.
Statistical analysis
Descriptive statistics were computed for baseline characteristics, with continuous variables presented as mean ± standard deviation (SD) and categorical variables as percentages. Differences between the early and late-stage MCI groups were assessed using Student’s t-tests were applied for normally distributed continuous variables and the Mann–Whitney U test was applied for non-normally distributed continuous variables. Categorical variables were compared using the chi-squared test. Demographic and clinical characteristics were analysed using IBM SPSS Statictics, version 27 (IBM corp., Armonk, NY, USA).
Correlation analysis
Pearson’s correlation coefficient (r) was calculated to examine the linear relationship between the cognitive scores and each lifelog feature. Spearman’s rank correlation coefficient (ρ) was also calculated to assess any potential monotonic associations, particularly for variables that were not normally distributed. Data normality was assessed using the Kolmogorov–Smirnov test, and outliers, defined by Z-scores exceeding ± 3, were excluded. Both correlation coefficients and their corresponding p-values are reported, with p-values adjusted using False Discovery Rate (FDR) correction. The analysis was conducted using the SciPy library in Python 3.8, with the statistical significance set at p < 0.05.
Exploratory data analysis and preprocessing
We conducted exploratory data analysis to assess data completeness, distributional properties, and potential collinearity among features before implementing the independent component analysis (ICA), principal component analysis (PCA), or machine learning algorithms. No missing values were present across the modalities (gait, 74 features; body composition, 37 features; grey matter on MRI, 476 features; and sleep, 12 features). Data normality was assessed using the Kolmogorov–Smirnov test, and variables were standardised using z-score normalisation to account for different scales and distributions. Histograms and density plots were visually inspected for skewness and multimodality. While some skewed distributions were observed, no clear bimodal patterns indicative of latent subgroups were found. Collinearity was addressed implicitly using ICA and PCA, which transformed the correlated variables into orthogonal components.
Machine learning and deep learning analysis
Two unsupervised machine learning (ML) algorithms, independent component analysis (ICA) and principal component analysis (PCA), were used for feature reduction. We tested 20, 40, and 60 reduced features for each of the three multimodal datasets. Supervised ML algorithms—support vector machine (SVM), random forest (RF), multilayer perceptron (MLP), and convolutional neural network (CNN)—were trained for classification using these reduced features. For the CNN, a one-dimensional convolutional neural network (1D CNN) was implemented. Each subject’s feature vector, which was reduced using PCA/ICA, was reshaped into an array of [n_components, 1], before being fed into two Conv1D layers with ReLU activation, followed by dropout, max pooling, a fully connected hidden layer, and a sigmoid output unit for binary classification. The detailed hyperparameters and architectural specifications are summarised in Supplementary Table S1. The dataset was split into 80% training and 20% test sets with tenfold cross-validation for model evaluation. Hyperparameter tuning was performed using 60 variations of each algorithm. The model performance was evaluated based on the area under the receiver operating characteristic curve (AUC), accuracy, recall, precision, and F1 score. The computations were performed on an Ubuntu 18.04 system with an Intel Core i9-9820X CPU (10 cores), a 64 GB memory, and an NVIDIA GTX 1080 Ti GPU.
Network analysis
A multiple regression model was employed to predict the cognitive scores based on independent variables from the multimodal datasets by incorporating features derived from ICA and PCA. The model can be expressed as follows:
where
\(Y_{ik}\) represents the ith cognitive score of the kth multimodal dataset,
\(X_{ij}\) represents the jth feature associated with the ith cognitive score of the kth multimodal dataset,
\(\beta_{0}\) and \(\beta_{j}\) are the intercept and regression coefficients, respectively, indicating the strength of each feature’s effect on the ith cognitive score of the kth multimodal dataset,
\(\varepsilon_{ik}\) is an error term that accounts for the unobserved factors influencing the ith cognitive score of the kth multimodal dataset, and
\(m_{k}\) is the total number of features in the kth multimodal dataset.
Multiple regression analysis was performed using the statsmodels library in R. The regression results were further analyzed in the context of network structure variables, such as centrality and network position, using Cytoscape version 3.9.1. Cytoscape provides advanced tools for visualizing and integrating network data.
Results
Baseline characteristics
Detailed demographic and clinical characteristics of the participants are presented in Table 1. The early-stage MCI group exhibited a higher proportion of females as than the late-stage MCI group. The years of education were shorter in the early than in the late-stage MCI group. Additionally, the early-stage MCI group had more comorbidities than the late-stage MCI group. Body mass index (BMI) was higher in the early than in the late-stage MCI group.
Correlation between physical and behavioral measures and cognitive functions
Figure 1 and Table 2 show the gait, body composition, and sleep parameters most strongly correlated with each cognitive function score. Overall, a longer stride length, faster gait velocity, and greater single support were all positively associated with better cognitive performance, whereas greater variability, increased step count, and longer double support were negatively associated. In Table 2, both Pearson’s r and Spearman’s ρ values are reported for the direct comparison between linear and rank-based correlations. The top five measures most strongly associated with each cognitive score are presented in Supplementary Table S2. Notably, features showing strong correlations also overlapped with the PCA components and ML model importance rankings, indicating consistency across analytic approaches (Supplementary Table S3). For reference, the corresponding Spearman correlation plots are shown in Supplementary Fig. S1.
Heatmaps illustrating the correlation between cognitive function scores and (a) gait parameters, (b) body mass composition, and (c) sleep parameters. Red represents positive correlations, blue represents negative correlations, and the color gradient indicates the strength of the correlation. Asterisks denote statistical significance: p < 0.05 (*), p < 0.01 (**). Abbreviations: MMSE-KC, mini-mental state examination, Korean version; SBT-K, short blessed test, Korean version; CERAD-K, Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet Korean Version; L, Left; R, Right; Supp, Support; GC, Gait Cycle; Std Dev, Standard Deviation; Len, Length; BMC, Bone Mineral Content; BMD, Bone Mineral Density; AHI, Apnea-Hyponea Index; AI, Apnea Index; ESS, Epworth Sleepiness Scale; HI, Hypopnea Index; NREM, Non-Rapid Eye Movement sleep; RDI, Respiratory Disturbance Index; REM, Rapid Eye Movement sleep; RERA, Respiratory Effort-Related Arousal.
Correlation between brain structures and cognitive functions
Figure 2 and Table 3 present the brain MRI parameters that were most strongly correlated with each cognitive function score. Significant correlations were observed among cognitive measures, grey matter morphometry, and white matter hyperintensity burden across multiple regions. Detailed results, including the top five structural features per cognitive domain, are provided in Supplementary Table S4. Both Pearson’s r and Spearman’s ρ values are reported to enable the comparison of linear and rank-based associations. For reference, the corresponding Spearman correlation plots are shown in Supplementary Fig. S2.
Heatmaps illustrating the correlation between cognitive function scores and brain structural features: (a) gray matter parameters and (b) white matter hyperintensity parameters. Red represents positive correlations, blue represents negative correlations, and the color gradient indicates the strength of the correlation. Asterisks denote statistical significance: p < 0.05 (*), p < 0.01 (**). Abbreviations: MMSE-KC, mini-mental state examination, Korean version; SBT-K, short blessed test, Korean version; CERAD-K, Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet Korean Version; lh, left hemisphere; rh, right hemisphere; GrayVol, Gray matter Volume; ThickAvg, Thickness Average; ThickStd, Thickness Standard deviation; MeanCurv, Mean Curvature; GausCurv, Gaussian Curvature; FoldInd, Folding Index; CurvInd, Curvature Index; WMH, White Matter Hyperintensity; LV, Lateral Ventricle.
Predicting late MCI using machine learning and deep learning analyses
The machine learning classifications of the participants are listed in Table 4. Four machine learning algorithms (SVM, RF, MLP, and CNN) were employed to identify the optimal feature pattern for distinguishing late-from early stage MCI. In the health metrics dataset, SVM achieved an AUC of 0.94, ACC of 0.80, recall of 0.86, precision of 0.69, and F1 of 0.75. For the MRI dataset, the CNN achieved an AUC, ACC of 0.86, Recall of 0.94, 0.86, 0.86, 0.79, and F1 of 0.81. In the health metrics and MRI-combined dataset, the MLP achieved an AUC of 0.94, ACC of 0.86, recall of 0.81, precision of 0.83, and an F1 of 0.82. In addition to the classification performance, the top 10 features identified by PCA and ICA for each dataset are provided in Supplementary Table S5. Although the feature sets derived from PCA and ICA did not directly overlap owing to methodological differences, several variables, including gait variability, step length, sleep fragmentation, and regional cortical thickness, consistently emerged as important predictors across different modalities and analytic approaches.
Discussion
Gait, body composition, sleep parameters, and brain structure were associated with cognitive function. In addition to brain MRI information, which is widely used as a predictor of cognitive function levels, health metrics such as gait, body composition, and sleep were also shown to be effective predictors of cognitive function. These health metrics demonstrated predictive accuracy comparable to that of brain MRI for estimating cognitive function levels. Moreover, combining health metrics with brain MRI data improves the prediction of cognitive function.
Previous studies have demonstrated that gait characteristics differ between elderly individuals with normal cognitive function and those with cognitive impairment15,16,17. Furthermore, machine learning models utilizing gait parameters have been successfully employed to differentiate between various degrees of cognitive function impairment18. These findings indicate that gait parameters can serve as reliable biomarkers for assessing the extent of cognitive impairment. The cholinergic system plays a crucial role in both gait and cognitive function, supporting the hypothesis that gait function may indirectly reflect cognitive function. Specifically, the findings on the nucleus basalis of Meynert suggest that the majority of cholinergic input to the cerebral cortex modulates hippocampal activity and cognitive frontoparietal networks19. Additionally, the cholinergic pedunculopontine nucleus (PPN) is thought to play a key role in both cognitive function20 and locomotion21. Dysfunction in specific brain regions and associated network impairments affect both cognitive and gait functions, reinforcing the link between these two domains. Our neuropsychological data suggest that attention and executive function are involved in gait control, particularly in the regulation of gait speed and variability. In this context, frontal cognitive networks are crucial, as they integrate sensory information through cortical sensory association areas, such as the parietal and occipital cortices22. The frontal-visuospatial network, in particular is implicated in controlling both gait velocity and variability, parameters related to dynamic stability23. This network facilitates adaptive motor behavior, especially in response to changes in the environmental context. Additionally, reduced hippocampal volume and decreased metabolism further support the role of memory in gait control. The hippocampal function has been associated with timing or rhythmicity of locomotion24. Gait characteristics also associated with hippocampal metabolism vary depending on the degree of memory impairment24. Taken together, these findings suggest that gait parameters, influenced by neurocognitive mechanisms, can provide valuable insights into cognitive function and serve as potential biomarkers for cognitive impairment.
Previous studies have shown that body composition parameters correlate with cognitive impairment. In midlife, obesity with a body mass index over 30 kg/m2 has been linked to an increased risk of dementia and Alzheimer’s disease (AD), even after adjusting for sociodemographic factors25. MRI-based studies have further shown that individuals with higher BMI exhibit greater brain atrophy in the frontal, temporal, parietal, and occipital lobes26. On the other hand, in individuals over 65 years of age, a higher BMI has paradoxically been associated with a lower risk of dementia27. This discrepancy suggests that BMI alone may not accurately reflect body composition, particularly in the elderly population. With aging, body composition changes as muscle mass decreases and fat mass increases, making BMI an unreliable indicator for assessing obesity in older adults28. Since BMI does not differentiate between fat and muscle mass, it may fail to capture the true metabolic risks associated with body composition changes in the elderly. More precise body composition assessments have demonstrated that increased fat mass and reduced muscle mass are more directly associated with cognitive impairment in older adults29. Additionally, reductions in whole-body soft tissue, particularly lean mass loss, have been linked to cognitive decline30,31. Our study also found a positive correlation between lean mass and cognitive function, which is consistent with previous research demonstrating an association between body composition and cognitive function. Additionally, our findings revealed a positive correlation between bone mineral composition and cognitive function, which is consistent with previous studies reporting that decreased bone mineral density (BMD) is linked to an increased risk of AD and cognitive decline32,33. One proposed mechanism underlying the relationship between BMD and cognitive function is that osteoporosis may induce calcium influx, leading to degenerative changes in the brain32. Additionally, bone mass loss may contribute to cognitive decline by increasing systemic inflammation34.
In the present study, sleep efficiency was positively associated with visuospatial function. Polysomnography defines sleep efficiency as the percentage of time spent asleep while in bed, and reductions in sleep efficiency often reflect difficulties such as prolonged sleep latency or frequent awakening35. Prior studies have reported that sleep efficiency, rather than sleep duration, is more strongly associated with cognitive impairment36. A previous study using PSG evidence showed that disturbed sleep patterns precede the clinical onset of cognitive decline, appearing during the prodromal stage known as MCI37. Patients with MCI exhibit a reduced amount of REM sleep and increased fragmentation of slow-wave sleep compared to cognitively healthy old adults37. Sleep disturbances have been increasingly recognized as both a symptom and a potential contributor to cognitive impairment, particularly in the context of AD. One proposed mechanism is amyloid-beta deposition. Even in the preclinical stage of AD, poor sleep quality has been linked to amyloid-beta accumulation38. As amyloid aggregation disrupts circadian rhythms and reduces the sleep quality, the sleep efficiency declines, which in turn leads to increased neuronal activity and further promotes amyloid deposition, creating a self-perpetuating cycle. Animal studies have demonstrated that sleep–wake cycle disruptions, previously considered a consequence of amyloid deposition, may precede its accumulation. Notably, these disruptions were reversed following amyloid clearance, indicating that impaired sleep could serve as an early marker of amyloid pathology39. Another pathway involves sleep-induced neuroinflammation. Sleep disturbances elevate the levels of proinflammatory cytokines, leading to microglial activation in the hippocampus and impairing memory consolidation40. Neuroinflammation induced by poor sleep may therefore exacerbate cognitive deficits independently or synergistically with amyloid pathology. Finally, structural degeneration of the basal forebrain, a region vulnerable to atrophy in AD and a major source of acetylcholine, plays an essential role in both sleep regulation and cognitive function. This suggests a shared cholinergic mechanism underlying sleep disturbances and cognitive decline41. Together, these mechanisms underscore the complex, bidirectional relationship between sleep quality and cognitive function.
Cognitive assessments are typically required to detect cognitive decline in patients with MCI. However, frequent cognitive testing is often impractical, which makes it difficult to identify early changes in cognitive function. Previous studies have attempted to address this issue by using brain MRI, a modality considered to be one of the most objective indicators of cognitive function, as input for machine learning models to detect MCI and estimate cognitive status42. Nonetheless, brain MRI has limitations in accurately reflecting cognitive function and is not easily accessible due to the high cost and limited availability of imaging equipment. By contrast, gait analysis, body composition measurements, and sleep monitoring can be easily performed in daily life. If cognitive deterioration can be accurately detected using easily accessible physical and behavioral data, it may enable the continuous monitoring of cognitive status and facilitate earlier intervention and treatment.
This study has several limitations. First, the relatively small sample size and single-center design may have limited the generalizability of our results. Second, the cross-sectional nature of the study restricts the interpretation of causal relationships or longitudinal cognitive changes. Third, although we used MMSE-based cut-offs to classify early- and late-stage MCI because the MMSE has been widely applied as a global index of cognitive functioning in prior studies43 and is suitable for staging purposes, reliance on the MMSE alone may not fully capture the clinical complexity of cognitive impairment. Fourth, any differences in educational attainment and comorbidities between early- and late-stage MCI may have influenced MMSE performance as well as behavioural features such as gait and sleep, raising the possibility of residual confounding. Finally, despite the use of cross validation, the complexity of the models relative to a modest sample size may increase the risk of overfitting. This finding underscores the need for external validation in larger multicentre cohorts to confirm the robustness of our findings.
Despite these limitations, this study demonstrated that easily accessible physical and behavioral measures such as gait, body composition, and sleep, can predict cognitive decline with a performance comparable to that of MRI-based models. This suggests a promising and cost-effective approach for early detection and continuous monitoring of cognitive impairment in real-world settings.
Data availability
The datasets generated and analysed during the current study are not publicly available due to privacy or ethical restrictions but are available from the corresponding author on reasonable request.
References
Petersen, R. C. et al. Mild cognitive impairment: a concept in evolution. J. Intern. Med. 275, 214–228. https://doi.org/10.1111/joim.12190 (2014).
Borson, S., Scanlan, J. M., Chen, P. & Ganguli, M. The Mini-Cog as a screen for dementia: Validation in a population-based sample. J. Am. Geriatr. Soc. 51, 1451–1454. https://doi.org/10.1046/j.1532-5415.2003.51465.x (2003).
Ding, Z., Lee, T. L. & Chan, A. S. Digital cognitive biomarker for mild cognitive impairments and dementia: A systematic review. J. Clin. Med. https://doi.org/10.3390/jcm11144191 (2022).
Sokoya, T. et al. Health indicators as measures of individual health status and their public perspectives: Cross-sectional survey study. J. Med. Internet Res. 24, e38099. https://doi.org/10.2196/38099 (2022).
Tolea, M. I. et al. Gait, balance, and physical performance as markers of early Alzheimer’s disease and related dementia risk. J. Alzheimers Dis. https://doi.org/10.1177/13872877241313144 (2024).
Chen, L. et al. Association between cognitive function and body composition in older adults: Data from NHANES (1999–2002). Front. Aging Neurosci. 16, 1372583. https://doi.org/10.3389/fnagi.2024.1372583 (2024).
Zimmerman, M. E. et al. The effects of insufficient sleep and adequate sleep on cognitive function in healthy adults. Sleep Health 10, 229–236. https://doi.org/10.1016/j.sleh.2023.11.011 (2024).
Lee, D.-Y. et al. Reliability and validity of the Korean version of Short Blessed Test (SBT-K) as a dementia screening instrument. J. Korean Neuropsychiatr. Assoc. 38, 1365–1375 (1999).
Kim, J. S. et al. Clinical implications of quantitative electroencephalography and current source density in patients with Alzheimer’s disease. Brain Topogr. 25, 461–474. https://doi.org/10.1007/s10548-012-0234-1 (2012).
Lee, D. Y. et al. A normative study of the CERAD neuropsychological assessment battery in the Korean elderly. J. Int. Neuropsychol. Soc. 10, 72–81. https://doi.org/10.1017/S1355617704101094 (2004).
Lee, J. H. et al. Development of the Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet (CERAD-K): Clinical and neuropsychological assessment batteries. J. Gerontol. B Psychol. Sci. Soc. Sci. 57, P47-53. https://doi.org/10.1093/geronb/57.1.p47 (2002).
Berry, R. B. et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 8, 597–619. https://doi.org/10.5664/jcsm.2172 (2012).
Berry, R. B. et al. AASM scoring manual updates for 2017 (Version 2.4). J. Clin. Sleep Med. 13, 665–666. https://doi.org/10.5664/jcsm.6576 (2017).
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31, 968–980. https://doi.org/10.1016/j.neuroimage.2006.01.021 (2006).
Hao, W. et al. Association of gait with global cognitive function and cognitive domains detected by MoCA-J among community-dwelling older adults: a cross-sectional study. BMC Geriatr 21, 523. https://doi.org/10.1186/s12877-021-02467-5 (2021).
Hoogendijk, E. O. et al. Gait speed as predictor of transition into cognitive impairment: Findings from three longitudinal studies on aging. Exp. Gerontol. 129, 110783. https://doi.org/10.1016/j.exger.2019.110783 (2020).
Seo, K. et al. Association between daily gait speed patterns and cognitive impairment in community-dwelling older adults. Sci. Rep. 13, 2783. https://doi.org/10.1038/s41598-023-29805-4 (2023).
Seifallahi, M., Galvin, J. E. & Ghoraani, B. Detection of mild cognitive impairment using various types of gait tests and machine learning. Front. Neurol. 15, 1354092. https://doi.org/10.3389/fneur.2024.1354092 (2024).
Coyle, J. T., Price, D. L. & DeLong, M. R. Alzheimer’s disease: A disorder of cortical cholinergic innervation. Science 219, 1184–1190. https://doi.org/10.1126/science.6338589 (1983).
Ruan, Y. et al. Cholinergic neurons in the pedunculopontine nucleus guide reversal learning by signaling the changing reward contingency. Cell Rep. 38, 110437. https://doi.org/10.1016/j.celrep.2022.110437 (2022).
Pahapill, P. A. & Lozano, A. M. The pedunculopontine nucleus and Parkinson’s disease. Brain 123(Pt 9), 1767–1783. https://doi.org/10.1093/brain/123.9.1767 (2000).
Haber, S. N., Liu, H., Seidlitz, J. & Bullmore, E. Prefrontal connectomics: From anatomy to human imaging. Neuropsychopharmacology 47, 20–40. https://doi.org/10.1038/s41386-021-01156-6 (2022).
Amboni, M., Barone, P. & Hausdorff, J. M. Cognitive contributions to gait and falls: evidence and implications. Mov. Disord. 28, 1520–1533. https://doi.org/10.1002/mds.25674 (2013).
Zimmerman, M. E., Lipton, R. B., Pan, J. W., Hetherington, H. P. & Verghese, J. MRI- and MRS-derived hippocampal correlates of quantitative locomotor function in older adults. Brain Res. 1291, 73–81. https://doi.org/10.1016/j.brainres.2009.07.043 (2009).
Kivipelto, M. et al. Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch. Neurol. 62, 1556–1560. https://doi.org/10.1001/archneur.62.10.1556 (2005).
Gazdzinski, S., Kornak, J., Weiner, M. W. & Meyerhoff, D. J. Body mass index and magnetic resonance markers of brain integrity in adults. Ann. Neurol. 63, 652–657. https://doi.org/10.1002/ana.21377 (2008).
Hughes, T. F., Borenstein, A. R., Schofield, E., Wu, Y. & Larson, E. B. Association between late-life body mass index and dementia: The Kame Project. Neurology 72, 1741–1746. https://doi.org/10.1212/WNL.0b013e3181a60a58 (2009).
Zamboni, M. et al. Body composition changes in stable-weight elderly subjects: the effect of sex. Aging Clin. Exp. Res. 15, 321–327. https://doi.org/10.1007/BF03324517 (2003).
Papachristou, E. et al. The relationships between body composition characteristics and cognitive functioning in a population-based sample of older British men. BMC Geriatr. 15, 172. https://doi.org/10.1186/s12877-015-0169-y (2015).
Buffa, R., Mereu, R. M., Putzu, P. F., Floris, G. & Marini, E. Bioelectrical impedance vector analysis detects low body cell mass and dehydration in patients with Alzheimer’s disease. J. Nutr. Health Aging 14, 823–827. https://doi.org/10.1007/s12603-010-0115-9 (2010).
Geng, J. et al. Low lean mass and cognitive performance: data from the National Health and nutrition examination surveys. Aging Clin Exp Res 33, 2737–2745. https://doi.org/10.1007/s40520-021-01835-w (2021).
Zhou, R., Deng, J., Zhang, M., Zhou, H. D. & Wang, Y. J. Association between bone mineral density and the risk of Alzheimer’s disease. J. Alzheimers Dis. 24, 101–108. https://doi.org/10.3233/JAD-2010-101467 (2011).
Zhao, Y., Chen, H., Qiu, F., He, J. & Chen, J. Cognitive impairment and risks of osteoporosis: A systematic review and meta-analysis. Arch. Gerontol. Geriatr 106, 104879. https://doi.org/10.1016/j.archger.2022.104879 (2023).
Ershler, W. B. Interleukin-6: a cytokine for gerontologists. J. Am Geriatr. Soc. 41, 176–181. https://doi.org/10.1111/j.1532-5415.1993.tb02054.x (1993).
Shrivastava, D., Jung, S., Saadat, M., Sirohi, R. & Crewson, K. How to interpret the results of a sleep study. J. Comm. Hosp. Intern. Med. Perspect 4, 24983. https://doi.org/10.3402/jchimp.v4.24983 (2014).
Ju, Y. E., Lucey, B. P. & Holtzman, D. M. Sleep and Alzheimer disease pathology–a bidirectional relationship. Nat. Rev. Neurol. 10, 115–119. https://doi.org/10.1038/nrneurol.2013.269 (2014).
Hita-Yanez, E., Atienza, M., Gil-Neciga, E. & Cantero, J. L. Disturbed sleep patterns in elders with mild cognitive impairment: The role of memory decline and ApoE epsilon4 genotype. Curr. Alzheimer Res. 9, 290–297. https://doi.org/10.2174/156720512800107609 (2012).
Ju, Y. E. et al. Sleep quality and preclinical Alzheimer disease. JAMA Neurol. 70, 587–593. https://doi.org/10.1001/jamaneurol.2013.2334 (2013).
Roh, J. H. et al. Disruption of the sleep-wake cycle and diurnal fluctuation of beta-amyloid in mice with Alzheimer’s disease pathology. Sci. Transl. Med 4, 150122. https://doi.org/10.1126/scitranslmed.3004291 (2012).
Zhu, B. et al. Sleep disturbance induces neuroinflammation and impairment of learning and memory. Neurobiol. Dis. 48, 348–355. https://doi.org/10.1016/j.nbd.2012.06.022 (2012).
Hita-Yanez, E., Atienza, M. & Cantero, J. L. Polysomnographic and subjective sleep markers of mild cognitive impairment. Sleep 36, 1327–1334. https://doi.org/10.5665/sleep.2956 (2013).
Zubrikhina, M. O. et al. Machine learning approaches to mild cognitive impairment detection based on structural MRI data and morphometric features. Cogn. Syst. Res. 78, 87–95. https://doi.org/10.1016/j.cogsys.2022.12.005 (2023).
Bergamino, M., McElvogue, M. M. & Stokes, A. M. Distinguishing early mild cognitive impairment from late mild cognitive impairment through free-water diffusion tensor imaging: A comparative analysis. Alzheimer’s Dementia https://doi.org/10.1002/alz.084580 (2025).
Acknowledgements
This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (NRF-2022R1A2C1011286; RS2022NR069669), and Basic Science Research funded by the Korean Government (2020R1F1A1048281; RS202300240976). This study was supported by a grant of from the Korea Health Promotion R&D Project, funded by the Ministry of Health and Welfare, Republic of Korea (Grant No.: HS21C0000). This research was supported by the Regional Innovation System & Education(RISE) Glocal University 30 Project program through the Gangwon RISE Center, funded by the Ministry of Education(MOE) and the Gangwon State(G.S.), Republic of Korea (2025-RISE-10-009). The funder played no role in study design, data collection, analysis and interpretation of data, or the writing of this manuscript. We would like to thank Editage (www.editage.co.kr) for English language editing.
Funding
This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (NRF-2022R1A2C1011286; RS2022NR069669), and Basic Science Research funded by the Korean Government (2020R1F1A1048281; RS202300240976). This study was supported by a grant of from the Korea Health Promotion R&D Project, funded by the Ministry of Health and Welfare, Republic of Korea (Grant No.: HS21C0000). This research was supported by the Regional Innovation System & Education (RISE) Glocal University 30 Project program through the Gangwon RISE Center, funded by the Ministry of Education(MOE) and the Gangwon State(G.S.), Republic of Korea. (2025-RISE-10-009). The funder played no role in study design, data collection, analysis and interpretation of data, or the writing of this manuscript.
Author information
Authors and Affiliations
Contributions
Ingyu Park and Unjoo Lee analyzed the data and created visualizations. Sang-Kyu Lee, Hui-Chul Choi, Moo-Eob Ahn, Ohk-Hyun Ryu, Yong Soon Park, and Dong-Kyu Kim collected data and contributed to the review and editing of the manuscript. Yeo Jin Kim collected data and drafted the original manuscript. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Park, I., Lee, SK., Choi, HC. et al. Machine learning-based estimation of the mild cognitive impairment stage using multimodal physical and behavioral measures. Sci Rep 15, 35369 (2025). https://doi.org/10.1038/s41598-025-19364-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-19364-1




