Abstract
Dopamine transporter (DAT) imaging and electroencephalography (EEG) are recommended biomarkers for diagnosing dementia with Lewy bodies (DLB). However, their interrelationship and independent associations with clinical symptoms remain unclear. We retrospectively analyzed 120 patients with DLB who underwent neuropsychological tests, DAT positron emission tomography, and quantitative EEG analysis. In the first step, partial correlation and univariable logistic regression analyses were conducted to screen for EEG or DAT biomarkers significantly associated with clinical characteristics. In the second step, multivariable regression models were constructed using combinations of the selected EEG and/or DAT variables to identify the best-fitting models. All models were adjusted for age, sex, and education. Lower DAT uptake in the ventral striatum was associated with higher theta power, lower beta power, and higher theta-to-beta ratio (TBR). EEG and DAT imaging biomarkers independently explained clinical symptoms: Fluctuations were best explained by increased temporal theta power and decreased putaminal DAT uptake. While visual hallucinations and rapid eye movement sleep behavior disorder were primarily linked to decreased DAT uptake in the putamen. Cognitive dysfunctions were mainly associated with EEG biomarkers—including lower central-parietal beta power, higher parietal theta power, and higher temporal-parietal TBR—while lower caudate DAT uptake provided additional explanatory value for semantic fluency dysfunction. EEG and DAT biomarkers offer independent and, in some cases complementary information about the clinical features in DLB. These findings support their potential use as multimodal biomarkers for disease monitoring.
Similar content being viewed by others
Background
Dementia with Lewy bodies (DLB) is the second most common cause of degenerative dementia, second only to Alzheimer’s disease (AD). Unlike AD, the diagnosis of which is feasible using biomarkers for amyloid and tau pathologies1, the diagnosis of DLB is based on the presence of clinical features and biomarkers that are not direct representative of Lewy body pathology in vivo. Clinical features are weighted as core or supportive, and biomarkers as indicative or supportive based upon their diagnostic specificity and the volume of good quality evidence available. There are three indicative biomarkers including the reduced striatal dopamine transporter (DAT) uptake on DAT imaging, abnormal uptake on 123iodine-MIBG myocardial scintigraphy, and polysomnography-confirmed rapid eye movement (REM) sleep without atonia. In addition, there are three supportive biomarkers that increase the diagnostic likelihood of DLB but are not themselves disease-specific. Prominent posterior slow-wave activity around the pre-alpha and theta ranges on electroencephalography (EEG) is one of these supportive biomarkers2.
Although the accuracy of DAT3,4,5,6 and EEG7,8,9,10,11,12 biomarkers have been studied for the diagnosis of DLB, there are inconsistencies in the results regarding their correlation with the clinical symptoms of DLB. Regarding biomarker correlation with clinical symptoms, some studies reported a significant correlation between striatal DAT uptake and motor parkinsonism13,14,15,16,17,18, while others did not19. Likewise, some studies reported a significant relationship between striatal DAT uptake and cognitive dysfunction6,20, while others did not14,15,16,17,19. Moreover, although some studies have investigated the correlation between EEG biomarkers and clinical symptoms, including general cognition reflected by the Mini-Mental State Examination (MMSE)21, visual hallucination10,12, and cognitive fluctuation11, the independent associations of DAT imaging and EEG biomarkers with clinical symptoms of DLB have not yet been elucidated.
In this study, we investigated the relationship between quantitative DAT imaging biomarkers, EEG biomarkers, and the clinical symptoms of patients with DLB. The mechanisms underlying EEG changes in DLB include dysfunctional thalamocortical connection21 and cholinergic dysfunction12, which could occur independent of nigrostriatal dopaminergic degeneration. Therefore, we hypothesized that the two biomarkers would exert independent effects on the clinical symptoms of DLB. To test this hypothesis, we analyzed 120 patients with probable DLB who underwent both DAT imaging and EEG. The primary outcomes were (1) the correlation between DAT and EEG biomarkers and (2) their independent associations with the core clinical features of DLB and cognitive dysfunction. Elucidating this relationship could be helpful in identifying the implications of the two biomarkers for monitoring disease severity in patients with DLB.
Methods
Participants
We retrospectively reviewed the medical records of 120 patients with probable DLB who visited the dementia outpatient clinic at Severance Hospital, Yonsei University Health System, from 2018 to 2022 and underwent EEG, DAT positron emission tomography (PET), and 3-Tesla brain magnetic resonance imaging (MRI). The diagnosis of probable DLB was based on the fourth consortium criteria for DLB2. All patients also underwent neurological examination, comprehensive neuropsychological tests, and amyloid PET imaging using florbetaben to evaluate the presence of co-existing β-amyloid pathology. The clinical features of DLB, including parkinsonism, REM sleep behavior disorder (RBD), visual hallucinations, and cognitive fluctuations, were evaluated using semi-structured questionnaires administered to caregivers22. The severity of parkinsonism was assessed based on a modified version of the Movement Disorder Society Unified Parkinson’s Disease Rating Scale part III score (mUPDRS), which included selected motor items assessing masked face, bradykinesia, rigidity, tremor, postural instability, and gait. The modified score included selected items 2,3,4,10,12,15,17 of UPDRS part III score. None of the patients exhibited pure vascular cognitive impairment or other causes of degenerative dementia or other causes of cognitive impairment. This study was approved by the Institutional Review Board of the Yonsei University Severance Hospital (No. 4-2021-0300). Due to the retrospective nature of the study, Institutional Review Board of the Yonsei University Severance Hospital waived the need of obtaining informed consent. All procedures performed in human studies were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Patients with suspected non-DLB pathophysiology were excluded, including (1) pure vascular cognitive impairment; (2) other degenerative dementias (e.g., frontotemporal lobar degeneration, corticobasal degeneration, and progressive supranuclear palsy); (3) drug-induced cognitive impairment; and (4) other conditions that could fully account for cognitive impairment, such as epilepsy, psychiatric disorders, normal pressure hydrocephalus, or structural brain lesion (e.g., tumor or hemorrhage).
Neuropsychological test
All patients underwent detailed neuropsychological tests using the Seoul Neuropsychological Screening Battery23. Standardized z-scores were available for all scorable tests based on age- and education-matched norms. This battery included the digit span backward test, the Korean version of the Boston Naming Test, the copying item of the Rey–Osterrieth Complex Figure Test (RCFT), the 20-min delayed recall item of the RCFT and Seoul Verbal Learning Test, the phonemic Controlled Oral Word Association Test (COWAT), semantic COWAT, and the Stroop color reading test. General cognitive status was measured using the Mini-Mental State Examination (MMSE) and Clinical Dementia Rating-Sum of Boxes (CDR-SOB).
EEG acquisition and analysis
All participants underwent EEG using the international 10–20 system for electrode placement. Nineteen channels were used: FP1, FP2, F7, F3, Fz, F4, F8, T3, C3, Cz, C4, T4, T5, P3, Pz, P4, T6, O1, and O2, with a reference montage. The contact impedance was kept below 10 kΩ during the recording. The sampling rate was 200 Hz. Participants were relaxed and awake, with eyes closed during the recording, and resting state EEG data were recorded for at least 5 min. We selected 3 min of eye-closed and artifact-free data based on visual inspection for further analysis. One epoch was 4 s long, and an average of 45 epochs were analyzed. The EEG data were passed through a notch filter. Thereafter, EEG data were filtered with high-pass offline above 1 Hz, and then low-pass filter below 60 Hz. The EEG data were recomputed to obtain the common average reference. Artifacts were removed in two steps. The first step was the rejection of non-stationary bad epochs, and the second step was to remove stationary bad components related to electromyogram, electrooculogram, cardiac signals such as heartbeat and slow drift wave such as drowsiness were removed to yield cleaned EEG data by independent component analysis24. At the sensor level, the absolute and relative power of EEG data was calculated in the following eight spectral bands using Welch-based discrete Fourier transformation. We used built-in function in MATLAB for performing Welch method (window size: sampling rate * 4 s; overlap: sampling rate * 2 s; window type: hamming window). After the preprocessing of EEG, Sensor-level analysis using the spectopo function in EEGLAB was performed in the following seven spectral bands: delta (1–4 Hz), theta (4–8 Hz), alpha1 (8–10 Hz), alpha2 (10–13 Hz), beta1 (13–20 Hz), beta2 (20–30 Hz), and gamma (30–45 Hz). We calculated the theta-to-beta ratio (TBR), which is obtained by dividing the theta band power density by the beta band power density for each channel. The mean lobar TBR was calculated by averaging the TBR values of the electrodes in each lobe (frontal: FP1, FP2, F3, F4, F7, F8, Fz; central: C3, C4, Cz; temporal: T3, T4, T5, T6; parietal: P3, P4, Pz; occipital: O1, O2). In addition, the EEG relative power densities in the theta, beta1, and beta2 bands in all lobar regions were calculated. A logarithmic transformation was applied considering the right-skewed distribution of the relative power and TBR.
Image processing
Details of MR and 18F-FP-CIT PET image acquisitions are provided in the supplementary material. Images were processed using the Functional Magnetic Resonance Imaging of the Brain (FMRIB) Software Library (FSL, version 6.0.3, http://fsl.fmrib.ox.ac.uk/fsl). T1-weighted images were corrected for intensity inhomogeneity and brain extracted. To prevent white matter lesions from biasing MRI tissue segmentation and reference region mask generation, we incorporated individual white matter hyperintensity (WMH) masks derived from FLAIR MRI using a three-dimensional U-Net convolutional neural network25. First, lesion-induced T1 hypointensities that could confound tissue classification were corrected by filling them with intensities from surrounding normal-appearing tissue on the inhomogeneity-corrected T1, using the WMH mask. Second, the segmented occipital white matter tissue class is further intersected with the WMH mask to obtain a lesion-cleaned reference region. Finally, to reduce partial-volume spill-in, this reference mask was further refined by retaining voxels with white matter tissue probability > 0.99 and applying three-dimensional one-voxel erosion (Supplementary Fig. 1).
Each participant’s 18F-FP-CIT PET image was then linearly co-registered to the individual T1-weighted MR image using a rigid body transformation. Volumes of interest (VOIs) for the ventral striatum (VST), caudate, and putamen were defined from the Oxford striatal structural atlas26 and non-linearly mapped using the high deformable registration (SyN) algorithm implemented in the Advanced Normalization Tools27. Standardized uptake value ratio (SUVR) maps were generated using the occipital white matter reference region28, and median 18F-FP-CIT SUVRs were extracted from the VST, caudate, and putamen. To explore the clinical relevance of the regional distribution of DAT uptake29,30, we additionally computed the caudate to posterior putamen SUVR ratio.
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences version 26.0 (IBM Corp., Armonk, NY, USA). The independent t-test and χ2 test were performed to compare demographics and clinical features across disease groups.
The statistical analysis was performed in two stages. First, we screened candidate predictors among EEG and DAT biomarkers for each dependent variable (clinical symptoms or cognitive test scores). Continuous outcomes, such as cognitive test scores, were analyzed with partial correlation analyses adjusted for age, sex, and education, whereas categorical outcomes, including visual hallucinations and cognitive fluctuations, were analyzed with univariable logistic regression models using the same covariates. To control for multiple testing, we applied a false discovery rate (FDR) correction and retained only those predictors that remained significant after correction (Q < 0.05). Second, we constructed multivariable models with the biomarkers that survived the screening step. For each outcome, every combination of one EEG biomarker and/or one DAT biomarker was evaluated, and the model with the lowest Akaike information criterion (AIC) was selected. This strategy focused on identifying the model that best explained the outcome rather than on retesting the statistical significance of individual predictors. In addition, for all regression models, we examined standard assumptions including linearity, independence of errors, normality, and homoscedasticity. Normality of residuals was assessed using the Kolmogorov-Smirnov test, linearity and homoscedasticity were evaluated by residual plots, and independence was assessed using the Durbin-Watson statistic. Multicollinearity was examined using variance inflation factors (VIF). When violations of homoscedasticity were detected, we repeated the analysis using the robust estimator (Huber-White sandwich method) as a sensitivity analysis.
Results
Demographics and clinical characteristics
The demographic and clinical characteristics of the participants are shown in Table 1. The mean age was 76.8 ± 6.3 and 43.3% were male participants. Half of participants had concomitant AD. Regarding the core neuropsychiatric symptoms of DLB, 60 patients had fluctuations (50%), 27 had visual hallucinations (22.5%), and 32 had RBD (26.7%). The mean mUPDRS score was 27.4 ± 7.6. The mean MMSE score was 20.9 ± 5.2, and mean CDR-SOB score was 4.1 ± 3.2.
Association between DAT and EEG biomarkers
The relationship between regional DAT uptake and EEG biomarkers was assessed using partial correlation analysis (Table 2). VST DAT uptake was weakly associated with the EEG biomarkers. The lower VST DAT uptake was correlated with the higher TBR in all lobes (range of ρ = −0.22–0.24) and relative theta power in the central and parietal lobes. Higher VST DAT uptake was related to greater relative beta1 power in the temporal lobe (ρ = 0.23) and beta2 power in the occipital lobe (ρ = 0.22). There were no significant results in other regional DAT uptake biomarkers.
Univariable association of biomarkers with core clinical features of DLB
The logistic regression analyses for the presence of fluctuation, visual hallucination, or RBD (Table 3) showed that higher TBR [range of odds ratio (OR) = 1.66–1.81], and relative theta power (range of OR = 2.55–3.80) in all lobes except for the frontal lobe and lower relative beta1 power (range of OR = 0.39–0.47) in all lobes except for the central lobe were related to the increased risk of fluctuation. No EEG biomarkers were associated with the risk of visual hallucination and RBD.
Lower regional DAT uptakes in the VST (OR = 0.39, 95% CI = 0.21–0.72, P = 0.003), putamen (OR = 0.52, 95% CI = 0.33–0.81, P = 0.004), and caudate (OR = 0.46, 95% CI = 0.27–0.78, P = 0.004) were associated with the increased risk of fluctuation. Lower DAT uptakes in the VST (OR = 0.42, 95% CI = 0.21–0.81, P = 0.010) and putamen (OR = 0.42, 95% CI = 0.24–0.72, P = 0.002), and higher caudate to posterior putamen DAT uptake ratio (OR = 52.97, 95% CI = 3.36-834.72, P = 0.005, Q = 0.010) were related to the increased risk of visual hallucination. Lower DAT uptake in the putamen (OR = 0.52, 95% CI = 0.32–0.86, P = 0.010, Q = 0.040) and higher caudate to posterior putamen DAT uptake ratio (OR = 16.61, 95% CI = 1.49-185.45, P = 0.022, Q = 0.044) were related to the increased risk of RBD.
Multivariable association of biomarkers with core clinical features of DLB
The multivariable associations of biomarkers with the core features of DLB are presented in Table 4. The multivariable model with the temporal theta power and putamen DAT uptake as predictors was the best-fit model for the presence of fluctuations. Higher relative temporal theta power (OR = 3.34, 95% CI = 1.30–8.57, P = 0.012) and lower putamen DAT uptake (OR = 0.54, 95% CI = 0.34–0.85, P = 0.008) were independently associated with the increased risk of fluctuation. The best-fit multivariable model for the presence of visual hallucinations only included the putamen DAT uptake as predictor. Lower putamen DAT uptake (OR = 0.42, 95% CI = 0.24–0.72, P = 0.002) was associated with an increased risk of visual hallucinations. The best model for the presence of RBD only included the putamen DAT uptake as a predictor (OR = 0.52, 95% CI = 0.32–0.86, P = 0.010).
Partial correlation analyses of biomarkers with cognitive test scores
Cognitive test scores were related to the widespread EEG and some DAT imaging biomarkers (Table 5). The KBNT score was associated with the PDR frequency, TBR and beta1 power in all lobes, theta power in the temporal, parietal, and occipital lobes. The Rey copy score was related to TBR and beta1 power in all lobes, beta2 power and theta power in the parietal lobe. Phonemic COWAT test scores were related to the parietal TBR and theta power in the temporal and parietal lobes. The semantic COWAT test score was related to the TBR in all lobes, theta power in central, temporal, and parietal lobes, beta1 power in all lobes. The Stroop CR score was related to the PDR frequency, TBR in all lobes, theta power in the parietal and occipital lobes, beta1 power in the temporal and parietal lobes and parietal beta2 power. The DSB, SVLT DR, and RCFT DR scores were not related to the any of EEG parameters investigated.
Among the DAT imaging biomarkers VST and caudate DAT uptakes were related to COWAT semantic score. Otherwise, there was no significant result.
Multivariable association of biomarkers with cognitive test scores
The multivariable associations between biomarkers and cognitive test scores were presented in the Table 6. The best-fit models for the KBNT, Rey copy, phonemic COWAT, Stroop CR scores included only EEG biomarker, whereas those for the semantic COWAT score included both EEG and DAT imaging biomarkers. Lower central beta1 power best explained the lower KBNT scores (B = 0.28, P = 0.003). Lower parietal beta1 power (B = 1.38, P < 0.001) best explained the lower Rey copy score. The combination of higher temporal TBR (B = −0.29, P = 0.002) and lower caudate DAT uptake (B = 0.36, P = 0.003) best explained lower COWAT semantic score. Higher parietal theta power (B = −0.69, P = 0.003) best explained lower COWAT phonemic score. Higher parietal TBR (B = −0.41, P = 0.003) best explained lower Stroop CR score. The best-fit models for the DSB, SVLT DR and RCFT DR scores were not made due to lack of significant parameter in the univariable analysis and partial correlation analysis.
For the RCFT copy score analysis, the residuals showed a deviation from normality. (Kolmogorov-Smirnov p-value 0.004). Therefore, we repeated the analysis using the robust estimator (Huber-White sandwich method). The results were consistent with those from the original regression analysis (Supplementary Table 1).
Discussion
In this study, we investigated the relationship between DAT imaging biomarkers, EEG biomarkers, and clinical symptoms in patients with DLB. Our major findings were as follows: First, EEG and DAT imaging biomarkers demonstrated independent and, in some cases, complementary associations with the clinical functions in DLB. Second, the combination of increased temporal theta power and decreased putaminal DAT uptake best predicted fluctuation, while visual hallucination and RBD were primarily explained by decreased DAT uptake in the putamen. Third, cognitive dysfunction was mainly explained by EEG biomarkers—specifically, lower central-parietal beta power, higher parietal theta power, and higher temporal-parietal TBR—while decreased caudate DAT uptake provided additional explanatory value for semantic fluency dysfunction. Forth, EEG biomarkers were associated with lower DAT uptake in the VST.
These findings suggest that EEG and DAT imaging biomarkers contribute independently, and in some cases complementarily, to the clinical features in DLB. For fluctuation, the multivariable model included both EEG and DAT imaging biomarkers, whereas visual hallucination and RBD symptoms were best explained by DAT imaging biomarkers alone. In contrast, cognitive symptoms were primarily associated with EEG biomarkers, while phonemic fluency was best explained by a combination of EEG and DAT imaging biomarkers. These findings highlight that specific neuropsychiatric and cognitive manifestations of DLB may be differently linked to EEG and DAT imaging biomarkers. EEG and DAT imaging biomarker can serve complementary role in characterizing the heterogeneous clinical presentations of DLB.
EEG and DAT imaging biomarkers explained the increased risk of fluctuations. Specifically, higher temporal theta power and lower putamen DAT uptake best explained the increased risk of fluctuation. Prominent posterior slow-wave activity around the pre-alpha and theta ranges on EEG is a supportive biomarker for the diagnosis of DLB2. However, our findings emphasize the relative importance of temporal theta activity over occipital slowing in relation to this core clinical feature. Previous studies also showed a significant association between cognitive fluctuation and slower dominant frequency, not confined to the occipital lobe8,31. Regarding the association between cognitive fluctuations and regional DAT uptake, Lee et al. reported a significant relationship for the ventral striatum but not for the caudate or putamen32. The discrepancy between those findings and the present results may stem from (1) the concurrent inclusion of EEG biomarkers in the present study and (2) the broader cohort analyzed in the previous study, which included patients DLB, AD, and mixed AD/DLB. Taken together, these results indicate that temporal-lobe theta activity and putaminal dopaminergic loss capture distinct yet complementary aspects of the pathophysiology underlying cognitive fluctuations in DLB.
Visual hallucinations in DLB were primarily associated with decreased DAT uptake in the putamen, with no significant contribution from EEG biomarkers in our multivariable model. This finding suggests the nigrostriatal dopaminergic deficits may contribute to the pathophysiology of hallucinations, although previous literature on this association has been inconsistent. While some studies have reported significant correlation between striatal DAT binding and visual hallucinations33, but others that found no significant association19,34,35. Our results support the possibility that nigrostriatal dopaminergic deficits may be involved in the development of visual hallucinations in DLB, although alternative mechanisms, such as concomitant cholinergic dysfunction36 or abnormalities in the visual pathway37,38,39, may also contribute. Regarding EEG biomarkers, although few previous studies suggested an association between visual hallucination and EEG slowing—such as decreased alpha power, increased theta/alpha or theta/beta ratio40,41—no EEG biomarkers survived FDR correction in our analysis. Notably, increased theta power exhibited a marginal association with the risk of visual hallucinations, although this did not reach statistical significance following multiple comparison correction. This trend may suggest a weak contribution of EEG biomarker in the risk of visual hallucination. Taken together, our findings indicate that EEG changes may play a limited role in visual hallucinations compared to dopaminergic deficits, further studies with larger sample sizes are warranted to clarify this relationship.
In the present study, EEG biomarkers were not associated with the risk of RBD, whereas lower putamen DAT uptake explained the increased risk of RBD. These results are consistent with previous studies showing reduced DAT uptake in patients with idiopathic RBD42,43, Parkinson’s disease and RBD44, and cognitively impaired patients with AD or Lewy body disease32. Although previous studies have reported slower occipital dominant frequency rhythm45, higher frontal-temporal-occipital theta power45, lower occipital beta power45, lower central beta power46, and occipital-central alpha-beta power46 in patients with RBD, to the best of our knowledge, the association between RBD and EEG changes has not been evaluated in DLB patients. Our results emphasize the role of brainstem nigrostriatal dopaminergic depletion in the pathogenesis of RBD in patients with DLB.
EEG biomarkers, including lower central-parietal beta power, higher parietal theta power, and higher temporal-parietal TBR, best explained cognitive dysfunction, but DAT biomarkers, especially lower caudate DAT uptake, provided additional information regarding semantic fluency dysfunction. Similar to our results, previous studies have shown a significant association of striatal, especially caudate, DAT uptake and cognitive dysfunction in patients with DLB20,47. Although previous studies have shown that the slowing of dominant frequency is associated with lower MMSE scores in patients with DLB21, and lower median frequency of EEG is associated with attention, memory, fluency, and executive dysfunction in patients with Parkinson’s disease48, the association of EEG changes with domain-specific cognitive dysfunction has not been evaluated in patients with DLB. These results suggest the possibility of using EEG biomarkers for disease monitoring of DLB in terms of cognitive dysfunction.
Previous studies have consistently demonstrated EEG abnormalities in patients with DLB, yet only a limited number of investigations have directly addressed the neural correlates of these abnormalities. Some reports have suggested an association with cholinergic dysfunction, particularly involving the nucleus basalis of Meynert49. Other studies have highlighted alterations in large-scale network dynamics has been associated with a loss of EEG microstate dynamics in Lewy body dementia50. Building upon these findings our study specifically examined whether EEG changes are related to DAT uptake, thereby probing the contribution of dopaminergic dysfunction to the electrophysiological abnormalities observed in DLB. DAT uptake in the VST was associated with EEG slowing patterns, including higher TBR, higher theta power, and lower beta power (Table 2). The VST comprises key regions of the mesolimbic dopaminergic system, such as the medial shell of the nucleus accumbens and the olfactory tubercle51,52, and it receives dopaminergic projections primarily from the ventral tegmental area (VTA)52 rather than from the nigrostriatal pathway. These EEG changes have previously been reported in patients with DLB2,12,53, and because they were not related to DAT uptake in the caudate or putamen—regions innervated by the nigrostriatal system—our findings point to a specific contribution of mesolimbic dopaminergic dysfunction to EEG abnormalities in DLB. Experimental data reinforce this interpretation: in rodents, selective knock-down of DAT in the VTA prolongs mesolimbic dopamine signaling—presumably elevating extracellular dopamine in the VST—and is accompanied by increased beta power and decreased theta power54. Conversely, our patients showed the opposite EEG pattern—decreased beta power and increased theta power—in proportion to VST DAT depletion. Because degeneration of the VTA-VST projection would reduce presynaptic dopamine stores and stimulus-evoked release, the electrophysiological effect observed in our patients can be regarded as the mirror image of the DAT knock-down experiment. Taken together, our findings suggest that dopaminergic dysfunction, particularly within the mesolimbic pathway, may contribute to EEG abnormalities in DLB. However, given prior evidence implicating cholinergic dysfunction and large-scale network alterations, further multimodal studies integrating dopaminergic, cholinergic, and cortical network markers are warranted to disentangle their relative contributions to the pathophysiology of EEG changes in DLB.
This study had several limitations. First, pathological confirmation was not performed to diagnose DLB. However, all of the enrolled patients with DLB satisfied the research criteria for probable DLB2, and the diagnosis was based on the meticulous clinical evaluation including DAT PET analyses. Second, all the patients with DLB were recruited from a single university hospital; as such, our results should be interpreted considering the referral bias. In addition, the relatively low prevalence of RBD (26. 7%) in our patients, which is within the lower range of previously reports rates55,56,57, may be due to several factors; Most patients were evaluated at an early disease stage shortly after diagnosis, and prolonged follow-up (which may increase RBD detection) was not available; RBD was assessed using caregiver-based questionnaires rather than polysomnography, which may underestimate its prevalence. These factors should be considered when interpreting the findings related to RBD. Additionally, although residual normality was satisfied in all but one of the linear regression models, the model predicting Rey copy scores showed a deviation from normality. To address this, we repeated the analysis using the robust estimator, which yielded results consistent with the original regression analysis. This sensitivity analysis indicates that the findings are robust despite the violation of normality.
Conclusions
This study investigated the interrelationship between DAT imaging and EEG biomarkers, and their associations with the clinical symptoms in patients with DLB. Our findings highlight the complementary roles of EEG and DAT imaging biomarker in explaining the clinical manifestations of DLB and support their potential utility as multimodal biomarkers for disease monitoring.
Data availability
The data and code used in this study are available from the corresponding authors upon request.
References
Jack, C. R. Jr. et al. NIA-AA research framework: toward a biological definition of alzheimer’s disease. Alzheimers Dement. 14, 535–562. https://doi.org/10.1016/j.jalz.2018.02.018 (2018).
McKeith, I. G. et al. Diagnosis and management of dementia with lewy bodies: fourth consensus report of the DLB consortium. Neurology 89, 88–100. https://doi.org/10.1212/wnl.0000000000004058 (2017).
Walker, R. W. H. & Walker, Z. Dopamine transporter single photon emission computerized tomography in the diagnosis of dementia with lewy bodies. Mov. Disord. 24, S754–S759 (2009).
O’Brien, J. T. et al. Dopamine transporter loss visualized with FP-CIT SPECT in the differential diagnosis of dementia with lewy bodies. Arch. Neurol. 61, 919–925. https://doi.org/10.1001/archneur.61.6.919 (2004).
McKeith, I. et al. Sensitivity and specificity of dopamine transporter imaging with 123I-FP-CIT SPECT in dementia with lewy bodies: a phase III, multicentre study. Lancet Neurol. 6, 305–313 (2007).
Kang, S. W. et al. Implication of metabolic and dopamine transporter PET in dementia with lewy bodies. Sci. Rep. 11, 14394. https://doi.org/10.1038/s41598-021-93442-y (2021).
Aoki, Y. et al. EEG Resting-State networks in dementia with lewy bodies associated with clinical symptoms. Neuropsychobiology 77, 206–218. https://doi.org/10.1159/000495620 (2019).
Bonanni, L. et al. EEG comparisons in early alzheimer’s disease, dementia with lewy bodies and parkinson’s disease with dementia patients with a 2-year follow-up. Brain 131, 690–705 (2008).
Bonanni, L. et al. EEG markers of dementia with lewy bodies: A multicenter cohort study. J. Alzheimer’s Dis. https://doi.org/10.3233/jad-160435 (2016).
Schumacher, J. et al. Quantitative EEG as a biomarker in mild cognitive impairment with lewy bodies. Alzheimers Res. Ther. 12, 82. https://doi.org/10.1186/s13195-020-00650-1 (2020).
Stylianou, M. et al. Quantitative electroencephalography as a marker of cognitive fluctuations in dementia with lewy bodies and an aid to differential diagnosis. Clin. Neurophysiol. 129, 1209–1220. https://doi.org/10.1016/j.clinph.2018.03.013 (2018).
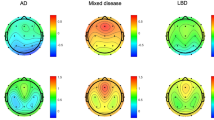
Baik, K. et al. Implication of EEG theta/alpha and theta/beta ratio in alzheimer’s and lewy body disease. Sci. Rep. 12, 18706. https://doi.org/10.1038/s41598-022-21951-5 (2022).
Chen, Q. et al. β-Amyloid PET and 123 I-FP-CIT SPECT in mild cognitive impairment at risk for lewy body dementia. Neurology 96, e1180–e1189. https://doi.org/10.1212/wnl.0000000000011454 (2021).
Kasanuki, K. et al. 123I-FP-CIT SPECT findings and its clinical relevance in prodromal dementia with lewy bodies. Eur. J. Nucl. Med. Mol. Imaging. 44, 358–365. https://doi.org/10.1007/s00259-016-3466-6 (2017).
Roselli, F. et al. Severity of neuropsychiatric symptoms and dopamine transporter levels in dementia with lewy bodies: A 123I-FP‐CIT SPECT study. Mov. Disord. 24, 2097–2103. https://doi.org/10.1002/mds.22702 (2009).
Shimizu, S. et al. Correlation between clinical symptoms and striatal DAT uptake in patients with DLB. Ann. Nucl. Med. 31, 390–398. https://doi.org/10.1007/s12149-017-1166-3 (2017).
Siepel, F. J. et al. Loss of dopamine transporter binding and clinical symptoms in dementia with lewy bodies. Mov. Disord. 31, 118–125. https://doi.org/10.1002/mds.26327 (2016).
Sole, A. D. et al. Correlation between 123I-FP-CIT brain SPECT and parkinsonism in dementia with lewy bodies: caveat for clinical use. Clin. Nucl. Med. 40, 32–35 (2015).
Ziebell, M. et al. Striatal dopamine transporter binding does not correlate with clinical severity in dementia with lewy bodies. J. Nucl. Med. 54, 1072–1076 (2013).
Marquie, M. et al. Striatal and extrastriatal dopamine transporter levels relate to cognition in lewy body diseases: an 11 C altropane positron emission tomography study. Alzheimers Res. Ther. 6, 52. https://doi.org/10.1186/s13195-014-0052-7 (2014).
Franciotti, R. et al. Anterior EEG slowing in dementia with lewy bodies: a multicenter European cohort study. Neurobiol. Aging. 93, 55–60. https://doi.org/10.1016/j.neurobiolaging.2020.04.023 (2020).
Park, M., Baik, K., Sohn, Y. H. & Ye, B. S. Development and validation of a screening questionnaire for dementia with lewy bodies (DLB): the DLB screening questionnaire (DLBSQ). Dement. Neurocognitive Disorders. 23, 11 (2024).
Kang, Y., Na, D. & Hahn, S. Seoul neuropsychological screening battery. (Human brain research & consulting co, 2003).
Delorme, A. & Makeig, S. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J. Neurosci. Methods. 134, 9–21 (2004).
Park, G., Hong, J., Duffy, B. A., Lee, J. M. & Kim, H. White matter hyperintensities segmentation using the ensemble U-Net with multi-scale highlighting foregrounds. NeuroImage 237, 118140. https://doi.org/10.1016/j.neuroimage.2021.118140 (2021).
Tziortzi, A. C. et al. Imaging dopamine receptors in humans with [11C]-(+)-PHNO: Dissection of D3 signal and anatomy. NeuroImage 54, 264–277. https://doi.org/10.1016/j.neuroimage.2010.06.044 (2011).
Avants, B. B. et al. A reproducible evaluation of ants similarity metric performance in brain image registration. Neuroimage 54, 2033–2044. https://doi.org/10.1016/j.neuroimage.2010.09.025 (2011).
Joutsa, J., Johansson, J. & Kaasinen, V. Is occipital cortex a valid reference region in 123I-FP-CIT SPECT imaging? Clin. Nucl. Med. 40, 615–616 (2015).
Joling, M. et al. Lower 123I-FP-CIT binding to the striatal dopamine transporter, but not to the extrastriatal serotonin transporter, in parkinson’s disease compared with dementia with lewy bodies. NeuroImage: Clin. 19, 130–136 (2018).
Walker, Z. et al. Striatal dopamine transporter in dementia with lewy bodies and Parkinson disease: a comparison. Neurology 62, 1568–1572 (2004).
Stylianou, M. et al. Quantitative electroencephalography as a marker of cognitive fluctuations in dementia with lewy bodies and an aid to differential diagnosis. Clin. Neurophysiol. 129, 1209–1220. https://doi.org/10.1016/j.clinph.2018.03.013 (2018).
Lee, Y. G., Jeon, S., Kang, S. W. & Ye, B. S. Effects of amyloid beta and dopaminergic depletion on perfusion and clinical symptoms. Alzheimers Dement. 19, 5719–5729. https://doi.org/10.1002/alz.13379 (2023).
Roselli, F. et al. Severity of neuropsychiatric symptoms and dopamine transporter levels in dementia with lewy bodies: a 123I-FP‐CIT SPECT study. Mov. Disorders: Official J. Mov. Disorder Soc. 24, 2097–2103 (2009).
Shimizu, S. et al. Correlation between clinical symptoms and striatal DAT uptake in patients with DLB. Ann. Nucl. Med. 31, 390–398 (2017).
Siepel, F. J. et al. Loss of D opamine T ransporter B Inding and C Linical S ymptoms in D ementia W Ith L Ewy B odies. Mov. Disord. 31, 118–125 (2016).
Perry, E. K. et al. Evidence of a monoaminergic-cholinergic imbalance related to visual hallucinations in lewy body dementia. J. Neurochem. 55, 1454–1456 (1990).
Pizzi, S. D. et al. Relevance of subcortical visual pathways disruption to visual symptoms in dementia with lewy bodies. Cortex 59, 12–21 (2014).
Heitz, C. et al. Neural correlates of visual hallucinations in dementia with lewy bodies. Alzheimers Res. Ther. 7, 6 (2015).
Iaccarino, L. et al. The brain metabolic signature of visual hallucinations in dementia with lewy bodies. Cortex 108, 13–24 (2018).
Schumacher, J. et al. Quantitative EEG as a biomarker in mild cognitive impairment with lewy bodies. Alzheimers Res. Ther. 12, 1–12 (2020).
Vallesi, A. et al. Resting-state EEG spectral and fractal features in dementia with lewy bodies with and without visual hallucinations. Clin. Neurophysiol. 168, 43–51 (2024).
Eisensehr, I. et al. Reduced striatal dopamine transporters in idiopathic rapid eye movement sleep behaviour disorder: comparison with parkinson’s disease and controls. Brain 123, 1155–1160. https://doi.org/10.1093/brain/123.6.1155 (2000).
Bauckneht, M. et al. Presynaptic dopaminergic neuroimaging in REM sleep behavior disorder: A systematic review and meta-analysis. Sleep Med. Rev. 41, 266–274. https://doi.org/10.1016/j.smrv.2018.04.001 (2018).
Chung, S. J., Lee, Y., Lee, J. J., Lee, P. H. & Sohn, Y. H. Rapid eye movement sleep behaviour disorder and striatal dopamine depletion in patients with parkinson’s disease. Eur. J. Neurol. 24, 1314–1319. https://doi.org/10.1111/ene.13388 (2017).
Fantini, M. L. et al. Slowing of electroencephalogram in rapid eye movement sleep behavior disorder. Ann. Neurol. 53, 774–780. https://doi.org/10.1002/ana.10547 (2003).
Sasai, T., Matsuura, M. & Inoue, Y. Electroencephalographic findings related with mild cognitive impairment in idiopathic rapid eye movement sleep behavior disorder. Sleep 36, 1893–1899. https://doi.org/10.5665/sleep.3224 (2013).
Yoo, H. S. et al. Interrelation of striatal dopamine, brain metabolism and cognition in dementia with lewy bodies. Brain 145, 4448–4458. https://doi.org/10.1093/brain/awac084 (2022).
Zimmermann, R. et al. Correlation of EEG slowing with cognitive domains in nondemented patients with parkinson’s disease. Dement. Geriatr. Cogn. Disord. 39, 207–214. https://doi.org/10.1159/000370110 (2015).
Schumacher, J. et al. EEG alpha reactivity and cholinergic system integrity in lewy body dementia and alzheimer’s disease. Alzheimers Res. Ther. 12, 46 (2020).
Schumacher, J. et al. Dysfunctional brain dynamics and their origin in lewy body dementia. Brain 142, 1767–1782 (2019).
Cansler, H. L., Wright, K. N., Stetzik, L. A. & Wesson, D. W. Neurochemical organization of the ventral striatum’s olfactory tubercle. J. Neurochem. 152, 425–448. https://doi.org/10.1111/jnc.14919 (2020).
Ikemoto, S. Dopamine reward circuitry: two projection systems from the ventral midbrain to the nucleus accumbens-olfactory tubercle complex. Brain Res. Rev. 56, 27–78. https://doi.org/10.1016/j.brainresrev.2007.05.004 (2007).
van der Zande, J. J. et al. Diagnostic and prognostic value of EEG in prodromal dementia with lewy bodies. Neurology 95, e662–e670. https://doi.org/10.1212/wnl.0000000000009977 (2020).
Guo, J. et al. Dopamine transporter in the ventral tegmental area modulates recovery from Propofol anesthesia in rats. J. Chem. Neuroanat. 121, 102083. https://doi.org/10.1016/j.jchemneu.2022.102083 (2022).
Roguski, A., Rayment, D., Whone, A. L., Jones, M. W. & Rolinski, M. A neurologist’s guide to REM sleep behavior disorder. Front. Neurol. 11, 610 (2020).
Elder, G. J., Lazar, A. S., Alfonso-Miller, P. & Taylor, J. P. Sleep disturbances in Lewy body dementia: A systematic review. Int. J. Geriatr. Psychiatry 37, 85 (2022).
Sobreira-Neto, M. A. et al. REM sleep behavior disorder: update on diagnosis and management. Arq. Neuropsiquiatr. 81, 1179–1194 (2023).
Acknowledgements
Not applicable.
Funding
This research was supported by a grant for the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant number: HI14C1324). This research was supported by a faculty research grant of Yonsei University College of Medicine (6-2021-0240) and by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. RS-2022-NR072434).
Author information
Authors and Affiliations
Contributions
KB, MY and BSY designed the study. KB, SJ performed image analysis and interpreted output. KB, SJ and SK performed statistical analysis and interpreted output. YK, KMK and KH collected data. KB, SJ drafted the manuscript. SK, YK, KMK, KH, MY, and BSY revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the Yonsei University Severance Hospital (No. 4-2021-0300), and the need for informed consent was waived because of the retrospective design of the study. All procedures performed in human studies were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Baik, K., Jeon, S., Kang, S. et al. Implication of dopamine transporter and electroencephalography biomarkers in dementia with lewy bodies. Sci Rep 15, 36755 (2025). https://doi.org/10.1038/s41598-025-20587-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-20587-5