Abstract
This study aimed to examine the association between the triglyceride-glucose (TyG) index, TyG-BMI index, and gallbladder disease (GBD) among Uyghurs in the Xinjiang Production and Construction Corps (XPCC), offering insights for GBD prevention and management. A prospective cohort design was utilized, enrolling 12,794 Uyghur participants from XPCC. The cumulative GBD incidence across quartiles of TyG, TyG-BMI, and BMI categories was estimated using the Kaplan-Meier method. The Cox proportional hazard regression model assessed the association between TyG, TyG-BMI, and GBD incidence, while mediation analysis investigated TyG’s potential mediating role in the relationship between BMI and GBD. Participants had a mean age of 37.68 ± 13.96 years, with 51.30% being male. Over a median follow-up of 6.00 years, 466 new GBD cases were identified, yielding a cumulative incidence of 4.3% and an incidence density of 7.68 per 1000 person-years. Women exhibited a higher cumulative incidence of GBD than men. The incidence of GBD gradually rises in both men and women with the increase of age. When the age exceeds 40, the incidence of GBD increases significantly. Following adjustments for gender, age, educational level, exercise frequency, diabetes, HDL-C, and LDL-C levels, individuals in the Q4 TyG index group demonstrated a significantly elevated GBD risk relative to the Q1 group (HR = 1.34, 95% CI:1.01–1.77). Similarly, GBD risk rose progressively across the Q2, Q3, and Q4 TyG-BMI index groups (HR = 1.97, 95% CI:1.23–3.16), (HR = 2.67, 95% CI:1.70–4.19), and (HR = 4.47, 95% CI:2.88–6.93), respectively. Overweight and obesity were also linked to a markedly greater GBD risk compared to normal weight (HR = 1.52, 95% CI:1.09–2.12) and (HR = 3.01, 95% CI:2.22–4.09). Among Uyghurs in the XPCC, elevated TyG and TyG-BMI indices were strongly associated with GBD risk, with TyG-BMI demonstrating the most pronounced association. Early TyG-BMI monitoring may aid in identifying individuals at high risk of developing GBD.
Similar content being viewed by others
Introduction
Gallbladder disease (GBD) is a prevalent digestive disorder with a significant global incidence, affecting 10% to 15% of adults in certain regions1. Common types of GBD include gallstones, cholecystitis, and gallbladder polyps. With improved living standards and dietary shifts, its incidence has shown a continuous upward trend, contributing to increasing disease burden and healthcare costs. Identifying and managing risk factors at an early stage is essential for effective prevention and treatment.
Insulin resistance (IR) is characterized by reduced insulin sensitivity and/or diminished insulin responsiveness2, leading to metabolic disturbances such as dyslipidemia, hyperglycemia, and hypertension—factors that may elevate GBD risk3,4,5. The hyperinsulinemic-euglycemic clamp technique has been employed in prior studies to assess IR, but its complexity and cost limit its feasibility in large-scale epidemiological research. In 2008, Simental-Mendia et al. introduced the TyG index as a practical surrogate for IR, offering a straightforward and accessible calculation method6,7. Its validity as an alternative marker for IR has been widely recognized8,9. BMI is commonly used to assess overall obesity, and the combination of TyG and BMI has primarily been applied in metabolic and cardiovascular disease research, with limited exploration in the context of GBD.
The prevalence of GBD in the Xinjiang Uyghur population exceeds that observed in the Han ethnic group, exhibiting distinct ethnic disparities10. This study prospectively examined the association of TyG and TyG-BMI indices with GBD risk, offering insights to inform preventive and therapeutic strategies.
Participants and methods
Participants
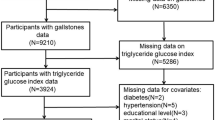
The study employed a representative sampling method to select the 51 st Regiment of the Third Division of the XPCC, a region with a high concentration of Uyghur residents, as the survey site. A total of 12,794 Uyghurs aged ≥ 18 years who had resided in the 51 st Regiment for at least one year were randomly selected as survey participants. The baseline survey was conducted between August and September 2016, followed by four subsequent assessments in August to September 2019, August to September 2020, August to September 2021, and August to September 2022. The final outcome survey took place from August to September 2022, ensuring consistency across all assessment phases. Outcome events were systematically collected and evaluated at each follow-up stage. Among the 12,794 initial participants, 858 were excluded due to missing data, severe illness, loss of consciousness, inability to cooperate, unwillingness to participate, migration, or pregnancy. An additional 785 individuals were excluded due to GBD or post-cholecystectomy status. The loss to follow-up rate was 2.60% (n = 331). (Fig. 1)
Data collection
(1) Questionnaire survey: A standardized training team administered a structured questionnaire to participants, including basic information, lifestyle habits, and personal and familial medical histories. (2) Physical examination: Anthropometric and physiological assessments adhered to standardized protocols, including measurements of height, weight, waist circumference, hip circumference, and blood pressure. Height and weight were obtained using a calibrated measuring instrument, while waist circumference was recorded with a flexible measuring tape. Blood pressure was assessed three times with an electronic sphygmomanometer [HBP-9020, Omron (China) Co., Ltd.], and the mean value was calculated. (3) For laboratory analyses, a 5 ml fasting venous blood sample was drawn from the antecubital vein in the morning, and biochemical markers such as FPG, TG, TC, LDL-C, and HDL-C were quantified using an OLYMPUS 2007 fully automated biochemical analyzer.
Diagnostic criteria for GBD
Diagnostic criteria for gallstones
According to the 2016 EASL Clinical Practice Guidelines11, routine abdominal B-ultrasound identified gallstones based on three characteristic findings: (1) a stable, hyperechoic mass within the gallbladder lumen; (2) a well-defined acoustic shadow posterior to the hyperechoic mass; (3) positional mobility of the hyperechoic mass, shifting according to gravitational changes. In cases where cholecystectomy was performed due to gallstones, the surgical report should explicitly state “cholecystectomy for gallstones.”
Diagnostic criteria for cholecystitis
According to the Consensus on Diagnosis and Treatment of Chronic Cholecystitis and Gallstones in China (2018)12, routine abdominal B-ultrasound examination identified characteristic features indicative of cholecystitis. (1) Acute cholecystitis: The gallbladder appeared enlarged with indistinct contours. The gallbladder wall exhibited diffuse thickening, characterized by hyperechoic bands interspersed with hypoechoic bands, producing a distinctive “double-sided shadow” effect. In cases of pus accumulation, the lumen contained sparse, or dense variably sized echogenic spots without acoustic shadowing or sedimentation bands. (2) Chronic cholecystitis: The gallbladder was enlarged, with a coarsely thickened wall and widened echogenic bands. Contractile function was impaired, and in severe cases, significant wall thickening was observed, along with mucosal cavity reduction, gallbladder atrophy, and filled stones. These features corresponded to the “wall-echo-shadow (WES) sign.”
Diagnostic criteria for gallbladder polyps
The 2017 European Multi-Society Joint Guidelines defined diagnostic criteria based on routine abdominal B-ultrasound imaging13. Characteristic features included an elevated lesion arising from the gallbladder wall and extending into the lumen, devoid of acoustic shadowing, and demonstrating no positional mobility. The echogenicity predominantly appeared as medium to low, with an absence of posterior acoustic shadowing. The lesion may present with a pedunculated morphology or exhibit no pedunculated characteristics.
Definition of related indicators
(1) Hypertension14: Defined as SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg, a documented history of hypertension, or antihypertensive use within the past two weeks.
(2) Smoking15: A smoking habit of at least one cigarette per day, either continuously or cumulatively, for six months or longer.
(3) Alcohol Consumption16: Alcohol consumption at a frequency of at least once per week, either continuously or cumulatively, for a minimum of six months.
(4) BMI Classification (kg/m²)17: Categories include underweight (< 18.5), normal weight (18.5–23.9), overweight (24.0–27.9), and obesity (≥ 28.0).
(5) Exercise Frequency : Classified as regular exercise (≥ 3 sessions per week, ≥ 30 min per session), occasional exercise (< 3 sessions per week, < 30 min per session), or minimal exercise (< 1 session per week).
(6) Type 2 Diabetes18: Diagnosis based on medical records, insurance data, or physical examination findings, including FPG ≥ 7.0 mmol/L.
(7) Dyslipidemia19: HDL-C < 1.00 mmol/L or LDL-C ≥ 3.40 mmol/L.
Calculation of related indicators
(1) BMI = weight (kg)/height (m2).
(2) TyG Index = ln [TG (mg/dL) × FPG (mg/dL)/2]
(3) TyG-BMI Index = TyG × BMI.
Statistical analysis
Data analysis was conducted using SPSS 26.0 and R 4.4.2. Continuous variables were presented as mean ± standard deviation and compared using the independent sample t-test, while categorical variables were expressed as frequency and constituent ratio, with inter-group comparisons performed using the test. BMI was categorized into four groups based on the quartiles of the TyG index and TyG-BMI index: <18.5 (underweight), 18.5- (normal weight), 24.0- (overweight), and ≥ 28.0 (obese). The Kaplan-Meier method estimated the cumulative incidence of GBD events across these index groups, and the Log-rank test assessed differences in cumulative GBD incidence among quartile groups. The Cox proportional hazards regression model evaluated associations between index groups and GBD risk, yielding HR and 95% CI. Covariates and traditional risk factors with P < 0.05 in the univariate analysis were incorporated into the multivariate Cox model.
The mediation effect of the TyG index on the relationship between BMI and GBD was assessed using the causal mediation analysis method developed by Imai et al.20.Incorporating adjustments for confounding variables, including age, gender, educational level, exercise frequency, hypertension, HDL-C, and LDL-C. A statistically significant mediation effect (P < 0.05) indicated the TyG index functioned as a mediating variable in the BMI-GBD association. Statistical significance was defined as P < 0.05 across all analyses.
Results
Baseline characteristics
The study comprised 10,820 participants (mean age: 37.68 ± 13.96 years), of whom 51.3% were male. Significant differences were observed between the GBD and non-GBD groups concerning educational level, exercise frequency, smoking status, diabetes, hypertension, HDL-C, LDL-C, BMI, TyG index, TyG-BMI index, and BMI classification (P < 0.001). No statistically significant association was identified between GBD incidence and alcohol consumption history, family history of cardiovascular disease, or diabetes (P > 0.05) (Table 1).
Incidence of GBD
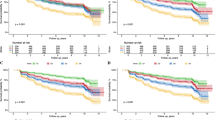
The median follow-up duration was 6.00 years, during which 466 individuals experienced their first GBD event. The cumulative incidence reached 4.3%, with an incidence density of 7.68 per 1,000 person-years. Women exhibited a higher cumulative incidence of GBD than men. (Fig. 2). The incidence of GBD gradually rises in both men and women with the increase of age. When the age exceeds 40, the incidence of GBD increases significantly. (Fig. 2). A progressive rise in cumulative GBD incidence was observed across TyG and TyG-BMI quartiles. Specifically, the incidence rates across TyG quartiles (Q1–Q4) were 3.1%, 2.9%, 3.8%, and 7.52%, respectively, with an upward trend from Q3 onward. Similarly, TyG-BMI quartile (Q1–Q4) analysis revealed cumulative incidence rates of 0.9%, 2.5%, 4.3%, and 9.5%, demonstrating a consistent increase.Among different BMI categories (underweight, normal weight, overweight, obese), the cumulative incidences of GBD are 0.88%, 1.44%, 3.31%, and 8.81% respectively. (Fig. 3)
Association of TyG and TyG-BMI indices with the risk of GBD
The Cox regression model was employed to assess the link between both indices and GBD risk, stratified by quartiles and BMI categories. Univariate Cox analysis identified gender, age, educational level, exercise frequency, diabetes, HDL-C, LDL-C, TyG index, overweight, obesity, and TyG-BMI index as significant factors associated with GBD. Multivariate Cox proportional hazard regression analysis, adjusted for gender, age, educational level, exercise frequency, diabetes, HDL-C, and LDL-C, revealed a markedly elevated GBD risk in the TyG index Q4 compared to Q1. A progressive increase in GBD risk was observed across the Q2, Q3, and Q4 TyG-BMI index groups. Additionally, overweight and obesity were associated with a significantly higher GBD risk relative to normal weight (Table 2).
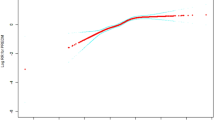
Mediation effect of TyG index on the association between BMI and GBD
After adjusting for age, gender, educational level, exercise frequency, hypertension, HDL-C, and LDL-C, analysis indicated that the TyG index served as a potential mediating variable in this association, accounting for 13.70% of the total effect (Table 3).
Discussion
This study represents the first prospective cohort analysis examining the association between TyG index, TyG-BMI index, and GBD in the Uyghur population within the XPCC in China. Multivariate Cox regression analysis identified TyG index and TyG-BMI index as independent risk factors for GBD. Compared with the Q1 group, the TyG index Q4 group exhibited a significantly higher risk of GBD. Similarly, an elevated risk of GBD was observed across the Q2, Q3, and Q4 groups of the TyG-BMI index, respectively. Overweight and obese individuals demonstrated a markedly higher risk of GBD compared to those with normal weight. These findings indicate that TyG-BMI may serve as a valuable reference metric for assessing GBD risk in this population.
IR is an independent risk factor for GBD, under IR conditions, hepatic lipid synthesis exhibits hyperactivation21, with fatty acid synthase gene expression increasing by 2.4 to 2.9 times22. SREBP1c activation occurs independently of insulin signaling through ER stress, mTORC1, and FoxO1, leading to enhanced lipid synthesis23 and a marked rise in hepatic plasma fatty acids and triglycerides. Excessive lipid accumulation in the liver activates specific protein kinases, which impair insulin receptor function and further aggravate IR24. IR represents a significant risk factor for GBD, contributing to compensatory hyperinsulinemia, excessive lipid synthesis, obesity, dysregulated lipid metabolism, inflammation, oxidative stress, and alterations in gut microbiota25. Among these, lipid metabolism disorders promote gallstone formation by disrupting cholesterol metabolism, while chronic inflammation and oxidative stress26 compromise gallbladder epithelial integrity, inducing or exacerbating gallbladder inflammation. Gut microbiota imbalances may interfere with bile acid metabolism, further contributing to GBD pathogenesis27. Previously, the hyperinsulinemic-euglycemic clamp technique had been employed for IR diagnosis; however, its high cost and time-consuming nature limit its application to specialized research rather than large-scale epidemiological studies. In contrast, the TyG index offers a practical alternative, characterized by simplicity, low cost, and accessibility, making it well-suited for clinical assessments and extensive epidemiological investigations7. A multicenter cross-sectional study involving a health examination cohort of over 500,000 participants identified a significant association between the TyG index and GBD risk28. Each unit increase in the TyG index corresponded to a 1.25-fold rise in GBD risk (95% CI: 1.13–1.37), while a standard deviation change was linked to a 1.24-fold increase (95% CI: 1.16–1.32). A similar cross-sectional study in the US reported a significant link between elevated TyG index levels and higher GBD prevalence29. Additionally, Chang Fu et al.30 demonstrated a strong positive relationship between TyG-BMI, TyG-WC, and TyG-WHtR and GBD in the American adult population. A cohort study utilizing a public database further corroborated that a progressive rise in the TyG index was associated with an incremental increase in GBD risk31. This study represents the first prospective cohort analysis to establish a significant link between the TyG index, TyG-BMI index, and GBD risk in the rural Uyghur population of Xinjiang.
The findings of this study revealed a significantly higher cumulative incidence of GBD among adult females in the Uyghur rural population of Xinjiang compared to males. Extensive research, both domestically and internationally, has consistently demonstrated a greater susceptibility to GBD in females than in males32,33,34, suggesting that gender disparities in GBD prevalence are independent of racial or geographical factors. Prior studies have attributed this pattern to the physiological influence of estrogen in women35. Estrogen levels exhibit considerable fluctuations due to age, menstrual cycle variations, and different physiological states36. Notably, pregnancy induces a sharp rise in estrogen levels, whereas menopause leads to a substantial decline. Evidence indicates that estrogen receptors are definitely expressed in the bile duct, with both estrogen receptor α and estrogen receptor β present in biliary cells37. Estrogen modulates cholesterol metabolism by activating estrogen receptor α and estrogen receptor β38, inhibiting cholesterol 7-alpha hydroxylase (CYP7A1) expression through multiple signaling pathways39,40,41, and reducing bile acid synthesis. This process lowers cholesterol solubility in bile, increases cholesterol saturation42, and contributes to GBD onset. Additionally, estrogen elevates the cholesterol-to-phospholipid ratio in liver and gallbladder cell membranes, diminishing membrane fluidity and obstructing bile outflow35, leading to cholestasis and further promoting GBD development. Its influence on gallbladder motility43 further delays gallbladder emptying and weakens contraction function, impairing bile excretion and causing cholesterol stone formation. Furthermore, the high fertility rate among Uyghur women in Xinjiang is associated with an elevated GBD risk, as multiparity has been linked to increased susceptibility. The data in this study corroborate this association, demonstrating a significantly higher GBD incidence in women compared to men.
Prior research has demonstrated a marked increase in GBD incidence with advancing age44, highlighting a distinct age-related risk pattern. The findings of this study align with those observed in previous investigations.
Obesity has been identified as a significant risk factor for GBD, with a well-established association between obesity and GBD onset44. IR contributes to weight gain through secondary hyperinsulinemia and serves as a fundamental mechanism underlying obesity-related disorders45. In this study, 63.5% of individuals with GBD were classified as obese. TyG demonstrated a partial mediation effect in the relationship between obesity and GBD, indicating that obesity elevates GBD risk by inducing IR, lipid metabolism disturbances, and chronic inflammation46. Epidemiological data highlight a concerning trend of increasing obesity rates in Xinjiang47. Greater attention should be directed toward obesity management, emphasizing early health education, structured dietary habits, proactive weight control, and preventive strategies to mitigate GBD onset and progression.
A key strength of this study lies in its large prospective cohort design, enabling the examination of the time-dependent relationship between TyG index, TyG-BMI index, and GBD. Additionally, this is the first investigation of the association between both indices and GBD within the Uyghur population of Xinjiang. However, several limitations should be acknowledged. The broad definition of GBD prevents a separate analysis of the association and relative strength of the links between gallstones, cholecystitis, and gallbladder polyps these indices. Moreover, the early diagnosis of GBD remains challenging due to its prolonged insidious onset and complex etiology. Extending the follow-up period is necessary to further validate these results. Furthermore, this study primarily focuses on the Uyghur population residing in rural areas of the XPCC. Variations in genetic background, diet, lifestyle, and cultural practices across different regions and populations may limit the generalizability of the findings.
Conclusions
In summary, both the TyG index and TyG-BMI index exhibit significant associations with GBD risk in the Uyghur population of the XPCC. Compared to the TyG index, the TyG-BMI index demonstrates a stronger correlation with GBD. In large-scale epidemiological investigations, assessing the TyG-BMI index holds substantial value for the early identification of individuals at high risk for GBD.
Data availability
The dataset used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sun, H. et al. Factors influencing gallstone formation: A review of the literature. Biomolecules 12, 550 (2022).
Gu, Q., Zhou, G. & Xu, T. Risk factors for gallstone disease in Shanghai. Medicine 99(3), e18754 (2020).
Qing, S. & Li, Z. Insulin resistance: history, mechanisms and management. Chin. J. Diabetes Mellitus. 1, 6–13 (2023).
González-Castillo, A. M. et al. Mortality risk estimation in acute calculous cholecystitis: beyond the Tokyo Guidelines. World J. Emerg. Surgery 16(1), 24 (2021).
Dhamnetiya, D., Goel, M. K., Dhiman, B. & Pathania, O. P. Gallstone disease and quantitative analysis of independent biochemical parameters: study in a tertiary care hospital of India. J. Lab. Physicians. 10, 448–452 (2020).
Sánchez-Íñigo, L., Navarro‐González, D., Fernández‐Montero, A., Pastrana‐Delgado, J. & Martínez, J. A. The TyG index May predict the development of cardiovascular events. Eur. J. Clin. Invest. 46, 189–197 (2016).
Navarro-González, D., Sánchez-Íñigo, L., Pastrana-Delgado, J., Fernández-Montero, A. & Martinez, J. A. Triglyceride–glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: the Vascular-Metabolic CUN cohort. Prev. Med. 86, 99–105 (2016).
Simental-Mendía, L. E., Rodríguez-Morán, M. & Guerrero-Romero, F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab. Syndr. Relat. Disord. 6, 299–304 (2008).
Lee, S. B. et al. Association between triglyceride glucose index and arterial stiffness in Korean adults. Cardiovascular Diabetology 17(1), 41 (2018).
Wang, H. et al. Risk factors for postoperative stone recurrence after cholecystolithotomy in Xinjiang Han nationality and Uygur nationality patients. Chin. Archives Gen. Surgery(Electronic Edition). 12, 388–392 (2018).
(EASL). EAftSotL, easloffice@easloffice.eu. Ea: EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J. Hepatol. 65, 146–181 (2016).
Digestion & EBoCJo Gastroenterology cgohdocso: consensus on diagnosis and treatment of chronic cholecystitis and gallstones in China (2018). Chin. J. Digestion. 39, 73–79 (2019).
Foley, K. G. et al. Management and follow-up of gallbladder polyps: updated joint guidelines between the ESGAR, EAES, EFISDS and ESGE. Eur. Radiol. 32, 3358–3368 (2021).
Hypertension RCoCGftPaTo, Alliance, H., Care HBoCIEaPAfMaH, S., Care, H. B. C. G. & HBoCAoGaH, Association, C. S. National center for chronic and noncommunicable disease control and prevention CCfDCaP, Jiguang W: Chinese guidelines for the prevention and treatment of hypertension (Revised 2024 Edition). Chin. J. Hypertens. 32, 603–700 (2024).
Bai, R. et al. Gallbladder disease is associated with the risk of cardiovascular disease among Uyghurs in Xinjiang: a prospective cohort study. BMC Public. Health 23(1), 242 (2023).
Sun, K. et al. Alcohol consumption and risk of metabolic syndrome: A meta-analysis of prospective studies. Clin. Nutr. 33, 596–602 (2014).
Care NaMMBoCIEaPAfMaH, Society, C. N. B. C. N., Society, C. D., Nutrition & CSfPaE Association ccncocmd: guidelines for medical nutrition treatment of overweight/obesity in China (2021). Asia Pac. J. Clin. Nutr. 31, 450–482 (2022).
Society, C. D. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin. J. Endocrinol. Metabolism. 37, 311–398 (2021).
Management JCotCGfL Chinese guidelines for lipid management (2023). Chin. J. Cardiol. 38, 237–271 (2023).
Imai, K., Keele, L. & Tingley, D. A general approach to causal mediation analysis. Psychol. Methods. 15, 309–334 (2010).
Sanders, F. W. B. & Griffin, J. L. De novolipogenesis in the liver in health and disease: more than just a shunting yard for glucose. Biol. Rev. 91, 452–468 (2015).
Eissing, L. et al. De novo lipogenesis in human fat and liver is linked to ChREBP-β and metabolic health. Nature Communications 4(1), 1528 (2013).
Matsuzaka, T. et al. Hepatocyte ELOVL fatty acid elongase 6 determines ceramide Acyl-Chain length and hepatic insulin sensitivity in mice. Hepatology 71, 1609–1625 (2020).
Lyu, K. et al. A Membrane-Bound Diacylglycerol species induces PKCϵ-Mediated hepatic insulin resistance. Cell Metabol. 32, 654–664e655 (2020).
Society, C. D. Expert consensus on insulin resistance (2022 edition). Chin. J. Diabetes. 14, 1368–1379 (2022).
LiNa, Y. & Yuan, C. Research progress in mechanism of inflammation and autophagy and their interaction in insulin resistance. J. Jilin Univ. (Medicine Edition). 45, 742–746 (2019).
Kim, J.-Y., Choi, Y., Leem, J. & Song, J. E. Heme Oxygenase-1 Induction by Cobalt Protoporphyrin Ameliorates Cholestatic Liver Disease in a Xenobiotic-Induced Murine Model. International J. Mol. Sciences 22(15), 8253 (2021).
Chun-yan, L. et al. The association between TyG-index and the risk of gallstone disease: a multicenter study. Mod. Prev. Med. 50, 775–780 (2023).
Feng, X., Wu, S., Ke, B. & Liang, Y. Elevated TyG index associated with increased prevalence of gallstones in a United States cross-sectional study. Frontiers Public. Health 12, 1351884 (2024).
Fu, C. et al. Association between triglyceride glucose index-related indices with gallstone disease among US adults. Lipids Health Disease 23(1), 203 (2024).
Liao, Q., Chen, Y., Peng, Q. & Li, C. Relationship between triglyceride-glucose index and gallstones risk: a population-based study. Frontiers Endocrinology 15, 1420999 (2024).
Collins, S. L., Stine, J. G., Bisanz, J. E., Okafor, C. D. & Patterson, A. D. Bile acids and the gut microbiota: metabolic interactions and impacts on disease. Nat. Rev. Microbiol. 21, 236–247 (2022).
Roa, J. C. et al. Gallbladder cancer. Nature Reviews Disease Primers 8(1), 69 (2022).
Kang, Q. et al. Relationship of Gallbladder Diseases with Sociodemographic Characteristics, Lifestyle, and Chronic Diseases in Northeastern China. International J. Environ. Res. Public. Health 15(11), 2596 (2018).
Jackson, S. S., Graubard, B. I., Gabbi, C. & Koshiol, J. Association with menopausal hormone therapy and asymptomatic gallstones in US women in the third National Health and Nutrition Examination Study. Scientific Reports 14(1), 191 (2024).
Kundakovic, M. & Rocks, D. Sex hormone fluctuation and increased female risk for depression and anxiety disorders: From clinical evidence to molecular mechanisms. Frontiers Neuroendocrinology 66, 101010 (2022).
Cheng, Y. et al. Research advances in effects of hormonal changes during the menstrual cycle on Neu-rological diseases. Adv. Clin. Med. 12, 10312–10317 (2022).
A, D. A. & AF, G. Regulation and deregulation of cholangiocyte proliferation. J. Hepatol. 33, 333–340 (2000).
Lu, L. & Yuyou, J. Shushu l: research progress on the mechanism of action of sex hormones and their receptors in liver lipid metabolism. Chin. J. Endocrinol. Metabolism. 36, 267–272 (2020).
Yu Cai Lim, M. & Kiat Ho, H. Pharmacological modulation of cholesterol 7α-hydroxylase (CYP7A1) as a therapeutic strategy for hypercholesterolemia. Biochemical Pharmacology 220, 115985 (2024).
Chiang, J. Y. L. & Ferrell, J. M. Up to date on cholesterol 7 alpha-hydroxylase (CYP7A1) in bile acid synthesis. Liver Res. 4, 47–63 (2020).
Zu, Y., Yang, J., Zhang, C. & Liu, D. The Pathological Mechanisms of Estrogen-Induced Cholestasis: Current Perspectives. Frontiers Pharmacology 12, 761255 (2021).
Xiao, J. et al. Bile acids-mediated intracellular cholesterol transport promotes intestinal cholesterol absorption and NPC1L1 recycling. Nature Communications 14(1), 6469 (2023).
Song, Y. et al. Age, gender, geographic and clinical differences for gallstones in china: a nationwide study. Annals Translational Med. 10, 735–735 (2022).
Parra-Landazury Nela, M., Cordova-Gallardo, J. & Méndez-Sánchez, N. Obesity and gallstones. Visc. Med. 37, 394–402 (2021).
Barber, T. M., Kyrou, I., Randeva, H. S. & Weickert, M. O. Mechanisms of Insulin Resistance at the Crossroad of Obesity with Associated Metabolic Abnormalities and Cognitive Dysfunction. International J. Mol. Sciences 22(2), 546 (2021).
Jia, H. et al. Epidemiological study on overweight and obesity among rural adult residents in Hazakh, Uygur and Han populations in Xinjiang. Chin. J. Epidemiol. 34, 1164–1168 (2013).
Acknowledgements
We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Funding
This study was funded by the Xinjiang Production and Construction Corps Key Areas Science and Technology Research Project (2018AB022).
Author information
Authors and Affiliations
Contributions
MHZ: Investigation, Conceptualization, Data curation, Methodology, Software, Visualization, Writing-original draft.JG: Conceptualization, Data curation, Investigation, Writing-original draft. JS: Conceptualization, Data curation, Investigation, Writing-original draft. ZHH: Conceptualization, Data curation, Investigation, Writing-review & editing.SLL: Conceptualization, Data curation, Investigation, Writing-review & editing.SJZ: Investigation, Methodology, Resources, Writing-review & editing.WHZ: Conceptualization, Data curation, Investigation, Writing-review & editing.JL: Conceptualization, Datacuration, Investigation, Writing-review & editing.JY: Conceptualization, Data curation, Investigation, Writing-review & editing.WXW: Conceptualization, Methodology, Supervision, Writing-review & editing.SXG: Investigation, Supervision, Writing-review & editing.XYP: Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing-review & editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Review Board (IERB) of the First Affiliated Hospital of Shihezi University School of Medicine (IERB no.: SHZ2010LL01). Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, M., Sun, J., Guo, J. et al. Association between triglyceride glucose index-related indices with gallbladder disease: a prospective cohort study in rural China. Sci Rep 15, 40680 (2025). https://doi.org/10.1038/s41598-025-21073-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-21073-8