Abstract
The rise in antifungal resistance has limited treatment options for serious fungal infections, emphasizing the need for effective combination therapies. However, low-cost and rapid systems to evaluate synergy and antagonism in antifungal combinations are lacking. Here, we introduce a novel in vitro testing method for assessing antifungal interactions in C. albicans, enabling the simultaneous testing of three antifungal agents in a single agar plate with overnight results. This method, validated against the checkerboard assay, provides consistent fractional inhibitory concentration (FICi) measurements with reduced variability and workload. We applied this method in a comprehensive screen of 92 clinical C. albicans isolates for three antifungals—amphotericin B, fluconazole, and anidulafungin—yielding assessments of a total of 276 distinct combinations of antifungals and isolates. Results revealed isolate-specific interaction patterns, with amphotericin B and fluconazole showing synergy in 1% of isolates, anidulafungin and fluconazole in 19.5%, and amphotericin B and anidulafungin in 23.9%. These findings underscore the need for isolate-specific testing in clinical settings. This proposed assay aims to present a solution to that as a scalable high throughput approach to this clinical problem.
Similar content being viewed by others
Introduction
Fungal infections pose a significant health risk, causing life-threatening diseases such as meningitis, pneumonia, and fungaemia, as well as chronic and recurrent conditions like oral and vaginal candidiasis, and asthm1. The growing threat from fungal pathogens is exacerbated by the increasing prevalence of antifungal resistance, which limits both treatment options and efficacy2. During the last decades, several resistant fungal species have emerged, such as N. glabratus, C. parapsilosis, and C. auris, that have very few therapeutic options due to the limited available antifungal arsenal3,4,5,6.
Among human fungal pathogens, Candida albicans is the leading cause of both mucosal and bloodstream candidiasis, accounting for roughly 40–60% of invasive Candida infections worldwide1. First-line therapy for candidemia typically involves an echinocandin (e.g., anidulafungin or caspofungin), with step-down to fluconazole in susceptible isolates; amphotericin B remains a rescue option for refractory or azole-resistant cases2,7. The limited size of this antifungal arsenal underscores the need for reliable combination testing specifically tailored to C. albicans.”
With a limited array of antifungals and the continued rise of resistance, clinicians are increasingly turning to combination therapies to enhance treatment outcomes7. Combination therapy, used either consecutively or sequentially3,8,9 is particularly important in treating immunocompromised patients with underlying comorbidities, where monotherapy may not be sufficient for eradication10.
One antifungal combination, amphotericin B and 5-flucytosine, is already regularly recommended for the treatment of candidiasis11 and several other combinations are also frequently employed to treat infections3,8,9. Combination therapy however is not a simple addition of antimicrobial effects. Administering multiple antifungal drugs can lead to synergistic interactions, where their combined action is greater than the sum of their individual effects, or conversely, antagonistic interactions may occur, reducing the overall effectiveness of treatment11.
Beyond immediate therapeutic gain, combination therapy can also slow the evolution of antifungal resistance. When two agents act on distinct cellular the fungus must acquire multiple, independent mutations to survive, dramatically lowering the probability that a single lineage can evolve high-level resistance. Synergistic combinations further reduce resistance risk by permitting lower individual drug exposures, thereby decreasing dose-dependent selective pressure on each target pathway. In addition, some combinations impose collateral fitness costs hindering the growth of partially resistant mutants. Collectively, these mechanisms make well-chosen combinations a promising strategy to extend the clinical lifespan of existing antifungals.
In cases of synergistic interactions, the required doses of each drug could be lowered, potentially reducing toxic side effects12,13. This is especially beneficial given that several antifungal agents are associated with toxicity or contraindications in high-risk patient populations14. Moreover, the emergence of antifungal resistance could be slowed, preserving the efficacy of available drugs15 particularly with newly introduced antifungals like ibrexafungerp, where prolonging their clinical lifespan is essential16.
The potential benefits of identifying synergistic combinations and avoiding antagonistic ones have led to numerous studies aimed at evaluating antifungal interactions7,17,18,19. However, the field lacks consensus, with some combinations reported to show either synergistic or antagonistic effects depending on the isolate suggesting that the efficacy of antifungal combinations may be isolate specific19,20.
At present, however, combination-susceptibility testing is rarely performed in routine clinical microbiology laboratories. Checkerboard or time-kill assays are generally confined to research settings or to exceptional, drug-refractory cases, largely because they are labour-intensive, take 48–72 h to complete, and suffer from inter-laboratory variability. Consequently, clinicians must often initiate combination therapy empirically, without isolate-specific interaction data. A rapid, standardisable assay would make combination testing feasible on a day-to-day basis, enabling evidence-based selection of synergistic regimens and avoidance of antagonistic pairs during the narrow window in which treatment decisions are made.
In recent years, several high-throughput methods have been developed to predict the combinatorial outcome of antifungal combinations, mainly by utilizing chemogenomic screenings21,22,23. However, in vitro methods for studying isolate-specific antifungal interactions have limitations. The checkerboard assay is the most widely used, but it lacks standardization, resulting in significant variability in both performance and data collection24. Moreover, it is labour-intensive and requires skilled personnel, which may limit its application in resource-constrained settings. Other methods, such as disc diffusion and time-kill assays, are also used but face similar challenges with standardization25. In contrast, recent advances in antibiotic combination studies have introduced innovative approaches that could be adapted for antifungal combinations26,27,28,29.
In this study, we aimed to develop a reliable and user-friendly method for studying antifungal interactions, with the goal of creating a straightforward pipeline that could lead to much-needed standardization in the field.
Our method builds on an in vitro assay previously used for testing antibiotic interactions in bacteria26. The CombiANT interaction method, uses a custom culture plate designed to create defined diffusion gradients of three antimicrobials simultaneously. Each antimicrobial is loaded into separate reservoirs surrounding a triangular interaction area. After overnight incubation, distinct zones of growth inhibition appear, allowing for the rapid quantification of drug interactions. Automated image analysis calculates Fractional Inhibitory Concentration indices (FICis) with high accuracy, enabling precise identification of synergistic, additive, or antagonistic effects between antimicrobial pairs.
Here, we optimized and adapted this method into a novel combination plate for testing antifungal interactions, using C. albicans as a model organism since it remains the dominant species isolated from invasive and mucosal fungal infections in our setting . This plate allows for the simultaneous testing of three antifungal agents in one agar plate, effectively replacing the need for three individual checkerboard assays. We validated the performance of the combination plate against the commonly used checkerboard assay and applied it to screen interclass antifungal combinations (amphotericin B, anidulafungin, and fluconazole) across 92 clinical C. albicans isolates. Through this method validation and its application in the largest screening of clinical C. albicans isolates to date, we aim to provide a valuable tool for antifungal combination testing, generate large-scale data on Candida interactions, and facilitate the development of patient-specific combination therapies.
Results
We adapted a previously established technique for antibiotic interaction testing26,30,31. to develop a plate-based assay for detecting interactions among three antifungal agents simultaneously (Fig. 1). The setup uses a standard petri dish format with three antifungal-loaded reservoirs (A, B, and C) positioned around a triangular interaction zone (Fig. 1a). Agar infused with antifungal agents is added to the reservoirs and allowed to solidify. At this stage, the plate remains inert and can be refrigerated, limited only by the antifungals’ shelf life—allowing advance preparation and consistent reagent handling for large-scale experiments.
Schematic and workflow of the antifungal combination plate assay for interaction testing. The combination plate assay, designed for testing interactions between three antifungal agents, uses a standard petri dish format with antifungal-loaded reservoirs (A, B, and C) surrounding a triangular interaction area (a). Agar infused with antifungal agents is added to the reservoirs, solidified, and refrigerated until use. The assay is activated by adding a 25 mL agar underlay to allow antifungal diffusion (b), followed by inoculating the plate with a low-temperature gelling agarose overlay containing a fungal inoculum (c). After overnight incubation at 30 °C, inhibition zones and growth patterns indicating antifungal interactions are visible (d). Areas of inhibition for individual antifungals appear (marked in pink), while growth inhibition zones due to antifungal interactions are marked in green. Six key points of interest, marked by asterisks, represent the inhibition edges for each antifungal and the internal growth zone edges near each corner of the interaction triangle, used for calculating Fractional Inhibitory Concentration index (FICi) values for each antifungal pair.
The assay is activated by pouring a 25 mL agar layer across the plate, enabling diffusion from the reservoirs (Fig. 1b). Once this layer solidifies, fungal inoculum is applied using low-temperature gelling agarose spread across the surface (Fig. 1c). This step ensures adequate cell density for readable results after overnight incubation, compensating for the slower growth of fungi compared to bacteria.
The diffusion model, numerical solution, and validation experiments underlying these concentration estimates are previously described26 The same open-source code and plate geometry were applied here without modification, ensuring that concentration mapping is fully reproducible.
After incubation at 30 °C, distinct interaction patterns emerge, with visible zones of inhibition and growth (Fig. 1d). Key readout points include the inhibitory concentration points (ICs, marked with asterisks in the pink zones of Fig. 1 right panel), found where individual antifungals alone inhibit growth, and combination inhibitory points (CPs, marked in the green zones), located at corners of triangular growth areas where two-drug combinations act. ICs lie along the outer edge of the interaction zone, directly opposing each antifungal reservoir, while CPs sit inside the triangle, representing combined effects.
Using the previously described analysis algorithm26 , the annotated IC and CP points are aligned with a predefined diffusion model that maps the concentration gradients of the antifungals across the agar. The algorithm estimates the local concentrations of each antifungal at these key points: the ICs (where single drugs act) and the CPs (where drug pairs act). These estimated concentrations are then used to calculate fractional inhibitory concentration index (FICi) values, reflecting the relative inhibitory contribution of each drug alone and in combination, using the following formulae and the extrapolated concentrations of the CP and IC points32:
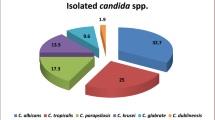
After establishing the protocol, we conducted a large-scale screen for antifungal interactions using a collection of 92 clinical C. albicans isolates (Fig. 2). The screening provided FICi values for combinations of fluconazole (FLC), anidulafungin (ANI), and amphotericin B (AMB)—antifungals chosen as representatives of the three main classes used to treat systemic fungal infections. A FICi value of 1 was used as the threshold between synergistic and antagonistic interactions33,34. Isolates with a mean FICi below 1 were categorized as synergistic, those with FICi above 1 as antagonistic, and values of exactly 1 were considered additive or indifferent. Due to the gradient-based nature of the assay and the use of interpolated values, exact FICi = 1 was not frequently observed in our dataset32,35,36,37,38. Our results showed that the AMB-FLC combination exhibited a synergistic interaction in 1% (1/92) of the strains (Fig. 2). The ANI-FLC combination showed synergy in 19.5% (18/92) of the strains (Fig. 2), and the AMB-ANI combination had a synergistic interaction in 23.9% (22/92) of the strains (Fig. 2).
Screening results of antifungal interactions across clinical Candida albicans isolates. Results from a large-scale screen of 92 C. albicans isolates tested with the combination plate assay for three antifungal pairs,: amphotericin B (AMB) with fluconazole (FLC) , anidulafungin (ANI) with FLC and AMB with ANI, shown in ascending FICi order for every combination . FICi values were used to categorize interactions as synergistic (mean FICi < 1,marked in green) or antagonistic (mean FICi > 1, marked in orange). Grey bars mark SEM for n = 3.
To verify the accuracy of our method, we compared its results with those obtained using checkerboard interaction assays for the same three combinations (AMB-FLC, ANI-FLC, and AMB-ANI). Checkerboards of AMB-FLC, ANI-FLC, and AMB-ANI were performed for ATCC 90,028 C. albicans reference strain. FICi values were calculated32 at 95% growth inhibition for the combinations of AMB-ANI and AMB-FLC and 75% for of ANI-FLC in concordance with the Broth micro dilution (BMD) thresholds for determining the inhibitory effect of each antifungal39 (supplementary protocol 1). FICi values from the combination plate and checkerboard assays were similar (Fig. 3 left), with a paired nonparametric t-test showing no significant differences between the methods.
Validation of combination plate results against checkerboard assay for antifungal interaction testing. Left: FICi values of the ATCC 90,028 C. albicans reference strain with the Combination plate and Checkerboard assay, non-parametric t test shows no significant difference between the two methods. Right: Regression analysis of FICi values obtained from both methods for selected clinical isolates (those with the most synergistic and antagonistic FICi values), regression slope shown in read between 1.066 and 1.317 (95% CI, p = 0.001).
To test the discrepancy between the two methods when applied on clinical strains, we proceeded to checkerboard test the most synergistic and antagonistic clinical strains identified in our screen (Fig. 3 right). Strains DA81057 and DA81040 were most synergistic and antagonistic, respectively, for the combination of AMB-FLC; DA81050 and DA81109 were most synergistic and antagonistic, respectively, for the combination of ANI-FLC; and DA81027 and DA81024 were most synergistic and antagonistic, respectively, for the combination of AMB-ANI. FICi values for the clinical isolates with both methods were plotted against each other and fitted to a linear regression model (Fig. 3 right). The slope of the regression ranged from 1.066 to 1.317 (95% confidence interval, p = 0.001), indicating a strong agreement between the methods, though the combination plate tended to slightly overestimate FICi values compared to the checkerboard assay. Additionally, Bland–Altman analysis showed a low intrinsic bias (0.2) between the two methods, with 95% limits of agreement ranging from − 0.67 to 1.09, further confirming the high level of concordance between results, despite the slight tendency of the combination plate to yield higher FICi values.
Discussion
In this study, we present a new method for studying antifungal interactions. The combination plate allows testing of three antifungal combinations simultaneously and has been developed to provide overnight results. By replacing three checkerboard assays with a single, less labour-intensive, agar-based test, the combination plate provides an easier and faster approach to conducting antifungal interaction screenings, without compromising accuracy. For example, hands-on preparation time for one combination plate is approximately 5–10 min whilst one checkerboard may require upwards of 60min. Additionally, the method can easily be adjusted for the screening of isolates with varying susceptibility levels by simply altering the antifungal concentration in the loading chambers as needed.
Applying the combination plate to determine interactions in susceptible, tolerant or resistant fungal species could be clinically useful. This approach could help identify synergistic combinations against invasive infections, and development of new resistances could potentially be delayed. Of significant concern is the increase in resistance towards echinocandins, found in both C. glabrata and C. auris. Combining empirical echinocandin treatment with other synergistic antifungals could prove to be an effective measure to widespread resistance emerging.
One of the primary goals with using this method was to obtain interaction results within an overnight incubation. Two key steps contributed to achieving this goal. First, we used YPD medium and agar throughout the process instead of RPMI. Even though RPMI medium is most commonly used in regular antifungal susceptibility testing, it has been argued that nutrient deprivation from RPMI medium may lead to artificially low MIC results, as inhibited growth can be misinterpreted as susceptibility40. For this assay, RPMI failed to support sufficient fungal growth for clear interaction patterns after overnight incubation, so YPD medium was used instead. While further standardization and optimization of media formulations for antifungal interaction testing is needed, results from the combination plates on YPD medium were similar to those obtained with RPMI in checkerboard assays, indicating that media choice has low impact on interaction results for this technology. Because YPD differs from the EUCAST/CLSI RPMI medium in buffering, glucose content, and pH, direct MIC comparisons should be interpreted with caution. Nevertheless, the assay’s purpose is rapid interaction mapping rather than MIC determination, and YPD was the only medium that consistently yielded overnight lawn formation. The second step to reaching assay readability quickly was the use of an inoculated agar overlay. Using a suspension of cells in agar instead of streaking a liquid culture onto an agar plate enhanced fungal growth and produced a smooth lawn with distinct inhibition zones, aiding in the analysis of the combination plates.
While the ability to obtain overnight results is one of the major advantages of this method, this benefit currently applies primarily to fast-growing fungi such as C. albicans. The growth-dependent readout of the combination plate relies on the formation of clear inhibition zones after a short incubation period, which may not be feasible for more slowly growing species like Nakaseomyces glabratus , Candida guilliermondii, or members of other genera such as Aspergillus. For such species, longer incubation times and standardized inoculi would be necessary to allow sufficient colony expansion and interaction pattern development. However, the underlying principle and assay workflow remain applicable, making this method adaptable across fungal taxa with modifications to incubation duration or media composition. Further validation studies are needed to systematically assess the performance of the combination plate for non-albicans Candida and other fungal species, but the potential for broader applicability remains strong, particularly in clinical settings where species-specific turnaround times can be planned accordingly.
Future work will test whether extended incubation(48–72 h), higher-nutrient overlays, or temperature adjustments can adapt the assay for slower-growing yeasts and filamentous fungi, but these modifications remain to be empirically validated.
In vitro studies of antifungal interactions have increased in recent years, as combination therapy is increasingly used to treat resistant pathogens. Traditionally, these studies have relied on checkerboard assays and typically involved smaller isolate collections20,41,42,43,44,45,46. Our study was performed on a substantially larger isolate collection, and quantified 3 distinct combinations at once and on the same clinical collection. We observed striking differences between the interaction pattern of echinocandins compared to that of amphotericin and fluconazole.
Specifically, combinations involving an echinocandin displayed a variety of interaction profiles in our study, with close to 20% of strains exhibiting a positive interaction and 80% a negative one. This pattern, studies comprised of fewer isolates may not be able to capture. Indeed, varying responses to the same combinations are evident between studies7,17, which has been posed to arise both due to the non-standardization of methodology and limited isolate collections7. The isolate-specific variability in interaction pattern we observed here, makes a compelling argument for case-to-case testing of antifungal interaction in hospital clinics. Such routine clinical use of interaction testing of antifungals requires an easy to use and affordable test, which we think this combination plate can provide.
The combination of amphotericin B and fluconazole studied here showed, in contrast to the echinocandin combinations, limited variability and was overwhelmingly antagonistic, with all but one strain exhibiting antagonism. This combination is known to show discrepancies between in vivo an in vitro studies. Thus, the combination plate and other in vitro methodologies consistently report this combination as antagonistic44,45,47, despite the favourable effects seen in vivo48. A recent study showed that the difference seen may be due to concentration dependant interactions based on the free-drug levels in plasma49. Deciphering these various physiological factors which may affect drug availability is necessary to help bridge the knowledge between in vitro and in vivo, aiding the tailoring of antifungal combination therapy regimens.
To categorize the interactions quantified in this study, we adhered to the original definition of the FIC index33,34. Interactions with an index above 1 were classified as antagonistic, and those below 1 as synergistic. Some studies use alternative thresholds, such as an upper limit of 0.5 for synergy and a lower limit of 4 for antagonism, to reduce misclassification from the intrinsic variability in checkerboard assays (see below), though these thresholds lack clinical validation. Therefore, we chose to present our findings using a straightforward classification. We hope that large-scale studies enabled by the here proposed and similar technologies will ultimately help define clinically relevant thresholds for synergy and antagonism, though this goal remains a future step in method development.
Checkerboard assays, while common, have inherent difficulties in readability. They rely on serial dilutions, which have a margin of error of one well, leading to potential variability of up to four-fold in the FICi readout due to this inherent ambiguity. In contrast, the combination plate employs a continuous gradient of antifungals rather than serial dilutions, reducing variability as shown in the consistent FICi values from our screening.
Advances in the field of antifungal interaction testing have been made with the invention of several predictive chemogenomic methods21,22,23. These methods hold great strength and can be valuable when exploring new combinations, developing new antifungals or evaluating interactions with other drugs. However, they may miss out on isolate-specific interactions which need to be tested on a case-to-case basis. Here the combination plate can serve as a complement to the in-silico methods to quickly evaluate if predicted synergies are present in clinical isolates, and if interaction profiles vary.
By guiding clinicians toward synergistic regimens and away from antagonistic or indifferent ones, the assay may help optimize drug exposure at infection sites, thereby reducing sub-inhibitory concentrations that drive resistance. Personalized combination selection can also shorten treatment courses and limit the total antifungal burden, both of which lower selective pressure for resistant mutants.
Although the combination plate is less labour-intensive and faster to perform, it maintains accuracy. Our cross-validation of the most synergistic and antagonistic drug-pathogen combinations with checkerboard assays demonstrates that results from this assay are directly comparable to those obtained from checkerboards, which are widely used but significantly more time-consuming to perform and interpret.
One limitation of the combination plate is that it primarily samples the concentration space near the MICs of the individual antifungal agents. Interactions between compounds, however, may vary at different concentrations50,51, which a checkerboard assay could detect. We argue that the reduced inherent variability of the combination plate compensates for this limitation, especially as clinically relevant interactions are likely to occur around inhibitory concentrations, which is precisely where the combination plate operates.
In conclusion, the combination plate method presented here offers reproducible, overnight results when testing antifungal interactions in vitro. It is easily scalable, allowing larger screens as the one presented here which showed isolate-specific interaction profiles to the combinations tested. The current results highlight the need for individual testing prior to implementation of combination treatment, which could both improve the therapeutic outcome and slow down resistance emergence. Due to its simplicity the combination plate could readily be implemented in both clinical and research labs, to further advance the field of antifungal interactions. Although the method uses a single input concentration per antifungal, it generates a continuous gradient of drug concentrations across the agar surface. This allows for high-resolution mapping of interaction zones, in contrast to the stepwise dilutions used in checkerboard assays. However, the method primarily captures interactions occurring near MIC levels. While this may limit detection of interactions that manifest only at extreme concentrations, it aligns well with the clinically relevant range in which treatment decisions are made.This method beyond the scope of this proof of concept also caries potential in investigating interactions involving other pathogens, such as the clinically important, C. auris, C. parapsilosis, and additional antifungal agents, thereby broadening its impact on antifungal research and treatment strategies.
Materials and methods
Fungal isolates and growth conditions
For technical validation and method calibration the C. albicans American Type Culture Collection (ATCC) strain 90,028, obtained from the Department of Clinical Microbiology at Karolinska Institutet, was used. The fungus was grown overnight at 30°C, in liquid cultures using Yeast Peptone Dextrose (YPD) broth (Sigma-Aldrich, Ref. Y1375) in an orbital shaking incubator set at 190 rpm. All clinical C. Albikans isolates (n = 92) were obtained from the Department of Clinical Microbiology of Karolinska Institutet, Huddinge. The isolates tested in this study were sampled from C. albicans bloodstream and vulvovaginal infections collected between 2021–2024 at Karolinska University Hospital, Stockholm, Sweden. Isolates were stored at − 80°C in freezing medium (-Nutrient broth (Oxoid CM0067) 21,25 g/L (2,13%)-Glycerol 85% (VWR 24,384) 184,5 g/L (= 150 mL/L) (12.75%)) until use and subsequently tested. Overnight cultures were prepared by transferring the yeast from frozen vials into 2 ml of YPD broth and incubated at 190 rpm orbital shaking in 30C.
Antifungals
Antifungals were suspended in DMSO or water, according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) recommendation ADDIN ZOTERO_ITEM CSL_CITATION { “citationID” : “G8N4koZU” , “properties” :{ “formattedCitation” :(26)” , “plainCitation” : “(26)” , “noteIndex” :0}, “citationItems” :[{ “id” :565, “uris” :[ “http://zotero.org/users/2448648/items/2YFLKWLX” ], “itemData” :{ “id” :565, “type” : “article-journal” , “abstract” : “Existing methods for identifying efficient combinations of antibiotics are time-consuming and costly, restricting their use in clinics and research. This study describes the novel CombiANT methodology, which uses defined diffusion landscapes of three antibiotics to permit rapid and low-cost synergy quantification between all antibiotic pairs.” , “container-title” : “PLOS Biology” , “DOI” : “https://doi.org/10.1371/journal.pbio.3000856” , “issue” : “9” , “journalAbbreviation” : “PLOS Biology” , “note” : “publisher: Public Library of Science” , “page” : “e3000856” , “title” : “CombiANT: Antibiotic interaction testing made easy” , “volume” : “18” , “author” :[{ “family” : “Fatsis-Kavalopoulos” , “given” : “Nikos” },{ “family” : “Roemhild” , “given” : “Roderich” },{ “family” : “Tang” , “given” : “Po-Cheng” },{ “family” : “Kreuger” , “given” : “Johan” },{ “family” : “Andersson” , “given” : “Dan I.” }], “issued” :{ “date-parts” :[[ “2020” ,9,17]]}}}], “schema” : “https://github.com/citation-style-language/schema/raw/master/csl-citation.json”} (26) E.Def 7.4 to a final concentration of 10 mg/ml, aliquoted in 20 µl, and stored at − 20°C until use. Antifungals used in this study include anidulafungin (Sigma-Aldrich, Ref. SML2288), amphotericin B (ThermoFisher Scientific, Ref. J61491.03), fluconazole (Sigma-Aldrich, Ref. PHR1160).
Broth microdilutions
Minimum inhibitory concentrations (MICs) for the C. albicans ATCC 90,028 reference strain were determined by broth microdilution following EUCAST E.Def 7.4, with the following modification: 100 µL of inoculum was added to 100 µL of each antifungal dilution. RPMI-1640 buffered with 0.165 M HEPES (pH 7.0) was used instead of MOPS; plates were incubated at 30 °C and read visually. Two-fold serial dilutions of each antifungal were prepared in 96-well round-bottom plates at 2 × the final test concentration. Wells then received 100 µL of a 0.5 McFarland yeast suspension in RPMI, giving a final inoculum of 0.5–2.5 × 10^5 CFU mL^− 1.
-
Azoles and echinocandins: MIC = lowest concentration showing ≥ 50% growth inhibition relative to the drug-free control.
-
Amphotericin B: MIC = lowest concentration showing ≥ 90% growth inhibition, per EUCAST recommendations
Optimization of fungal growth conditions
The six laboratory medium tested were:
-
1.
BD BACTO™ Brain Heart Infusion (BHI) broth (Becton Dickinson, Ref. 237,500)
-
2.
BD DIFCO™ Mueller–Hinton (MH) broth (Becton Dickinson, Ref. 275,730)
-
3.
MH-II broth (Becton Dickinson, Ref. 212,322)
-
4.
Lysogeny Broth (LB) (Sigma-Aldrich, Ref. L3522)
-
5.
Yeast Peptone Dextrose (YPD) broth (Sigma-Aldrich, Ref. Y1375)
-
6.
RPMI medium (Gibco, Ref. 130,118,031)
2% D-glucose (w/v) was supplemented to all media, except YPD, and plates were prepared in-house with 1.5% agarose (w/v) (Sigma-Aldrich, Ref. A9639), except for YPD agar which was bought (Sigma-Aldrich, Ref. Y1500).
Three different plating methods were evaluated, namely:
-
1.
Glass beads. 100 µl of undiluted fungal overnight culture was added directly to plates and spread using the beads. An undiluted inoculum was used as this yielded the most consistent growth and clear inhibition zones on the combination plates.
-
2.
Cotton swabbing, performed according to EUCAST guidelines but using undiluted overnight culture52.
-
3.
Inoculating an overlay using low-temperature gelling agarose. Overlay was prepared by mixing equal volumes of 3% (w/v) low-temperature gelling agarose (Sigma-Aldrich, Ref. A4018) with undiluted overnight culture, yielding a 1:2 dilution of the overnight. The low temperature gelling agarose was homogenized in a water bath set at 55°C.
Combination plate calibration
Prior to the screening of clinical isolates, the concentrations of the antifungals to be used on the assay were calibrated using the ATCC type strain. MIC values obtained from the BMDs lay the basis for the calibration which was done for every antifungal. Optimal assay concentration was defined as the concentration where clear inhibition zones with defined edges formed as this aids the annotation of the key points during data analysis. During calibration, the three antifungal-loading reservoirs in a plate contained the same antifungal, but at different concentrations. Concentrations up to 600 times the MIC of each antifungal was tested, using an increment of either 10 (between 10-100X the MIC) or 100 (between 100-600X the MIC).
Protocol validation and ATCC strain
After optimal growth conditions and antifungal concentrations were established for the assay, the developed protocol (supplementary protocol 2) was evaluated using the ATCC type strain. The strain was tested for the pairwise combination of ANI, AMB, and FLC in technical triplicates.
The antifungal-loading chambers were loaded with YPD agar containing one of the three antifungals. After the agar solidified, the assays were kept at 4°C for a minimum of 45 min, after which an underlay of 25 ml YPD agar was added. The agar was left the rest and solidify at room temperature for at least 2h before plating. Plating was done by using an inoculated agar overlay which was prepared by mixing equal volumes of a 3% low-temperature gelling agarose with a dense fungal overnight culture diluted 1:50 in fresh YPD medium, resulting in a final 1:100 dilution of the overnight culture. Methylene blue was added to the 3% agarose solution at a concentration of 1 μg/mL for a final concentration of 0.5 μg/ml.
Screening of clinical isolates
All clinical isolates (n = 92) were screened for the pairwise combination of ANI, AMB, and FLC. Isolates were tested in technical triplicates of biological duplicates. Isolates were grown overnight as described and subsequently screened using the developed protocol (Supplementary protocol 2). The incubation temperature for the combination plates was set to 30°C, as this consistently supported overnight growth for all clinical isolates in our panel. During assay development, we found that several strains failed to produce sufficient growth at 35°C within the 16–20 h incubation period required for next-day readout. Therefore, 30°C was selected to ensure reliable and uniform growth across all tested strains.
Checkerboard technique
Checkerboard assays were performed for the ATCC 90,028 C. albicans reference strain and the most synergistic and antagonistic clinical strains identified in the screen to verify the results. The checkerboard protocol used here was modified from the protocol published by Vitale et.al53 and a step-by-step protocol is available in Supplementary protocol 1. Checkerboards were performed using 96-well round bottom microtiter plates in biological triplicates. The antifungal stocks prepared previously were suspended in RPMI medium at 4X the highest concentration to be used. The suspensions was twofold serially diluted and 50 μl of each antifungal, at 4X the final concentration, was added to their corresponding well. 100 μl of fungal suspension prepared at 0.5 McFarland was added to all experimental wells. RPMI medium served as a sterility control. After an overnight static incubation at 30°C the wells were resuspended and the optical density (OD) was measured at 450 nm using a Thermo Fisher Scientific Multiscan FC Type 357. For analyses, the OD values of the sterility control were subtracted from all experimental wells and the growth inhibition was calculated as a percentage by dividing the experimental wells with the growth control. To obtain the MIC values for the antifungals when used in combinations, points of theoretical additivity were picked. Based on the EUCAST method of MIC determination of yeasts in BMDs, the theoretical additivity is at 95% growth inhibition for the combinations of AMB-ANI and AMB-FLC whilst for the combination of ANI-FLC it is at 75% growth inhibition.
Statistical analysis
Statistical analyses were performed using Graphpad Prism version 9, significance levels are noted at p = 0.05 probability unless otherwise stated.
Data availability
All data generated or analysed during this study are included in this published article.
References
Perlin, D. S., Rautemaa-Richardson, R. & Alastruey-Izquierdo, A. The global problem of antifungal resistance: Prevalence, mechanisms, and management. Lancet Infect. Dis. 17(12), e383–e392 (2017).
Hendrickson, J. A., Hu, C., Aitken, S. L. & Beyda, N. Antifungal resistance: A concerning trend for the present and future. Curr. Infect. Dis. Rep. 21(12), 47 (2019).
Pfaller, M. et al. Epidemiology and outcomes of candidemia in 3648 patients: Data from the prospective antifungal therapy (PATH Alliance®) registry, 2004–2008. Diagn. Microbiol. Infect. Dis. 74(4), 323–331 (2012).
Chakrabarti, A. & Sood, P. On the emergence, spread and resistance of Candida auris: Host, pathogen and environmental tipping points. J. Med. Microbiol. 70(3), 001318 (2021).
Daneshnia, F. et al. Worldwide emergence of fluconazole-resistant Candida parapsilosis: Current framework and future research roadmap. Lancet Microbe 4(6), e470–e480 (2023).
Kaur, R., Dhakad, M. S., Goyal, R. & Kumar, R. Emergence of non-albicans Candida species and antifungal resistance in intensive care unit patients. Asian Pac. J. Trop. Biomed. 6(5), 455–460 (2016).
Fioriti, S. et al. Antifungal combinations against candida species: From bench to bedside. J. Fungi 8(10), 1077 (2022).
Qiu, K. Y. et al. Combination antifungal treatment for invasive fungal disease after hematopoietic stem cell transplantation in children with hematological disorders. Transpl. Infect. Dis. 21(3), e13066 (2019).
Haider, S., Rotstein, C., Horn, D., Laverdiere, M. & Azie, N. The Prospective antifungal therapy alliance® registry: A two-centre Canadian experience. Can. J. Infect. Dis. Med. Microbiol. 25(1), 17 (2014).
Campitelli, M., Zeineddine, N., Samaha, G. & Maslak, S. Combination antifungal therapy: A review of current data. J. Clin. Med. Res. 9(6), 451 (2017).
Pappas, P. G. et al. Clinical Practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of America. Clin. Infect. Dis. 62(4), e1-50 (2016).
Johnson, M. D. & Perfect, J. R. Use of antifungal combination therapy: Agents, order, and timing. Curr. Fungal Infect. Rep. 4(2), 87 (2010).
Shrestha, S. K., Fosso, M. Y. & Garneau-Tsodikova, S. A combination approach to treating fungal infections. Sci. Rep. 5(1), 17070 (2015).
McKeny, P. T., Nessel, T. A. & Zito, P. M. Antifungal Antibiotics (StatPearls, 2024).
Fuentefria, A. M., Pippi, B., Dalla Lana, D. F., Donato, K. K. & de Andrade, S. F. Antifungals discovery: An insight into new strategies to combat antifungal resistance. Lett. Appl. Microbiol. 66(1), 2–13 (2018).
El Ayoubi, L. W., Allaw, F., Moussa, E. & Kanj, S. S. Ibrexafungerp: A narrative overview. Curr. Res. Microb. Sci. 1(6), 100245 (2024).
Wake, R. M. et al. Optimizing the treatment of invasive candidiasis—A case for combination therapy. Open Forum Infect. Dis. 11(6), ofae072 (2024).
O’Brien, B., Liang, J., Chaturvedi, S., Jacobs, J. L. & Chaturvedi, V. Pan-resistant Candida auris: New York subcluster susceptible to antifungal combinations. Lancet Microbe 1(5), e193–e194 (2020).
Jacobs, S. E. et al. Candida auris pan-drug-resistant to four classes of antifungal agents. Antimicrob. Agents Chemother. 66(7), e00053-e122 (2022).
O’Brien, B., Chaturvedi, S. & Chaturvedi, V. In vitro evaluation of antifungal drug combinations against multidrug-resistant candida auris isolates from New York outbreak. Antimicrob. Agents Chemother. https://doi.org/10.1128/aac.02195-19 (2020).
Gaikani, H., Smith, A. M., Lee, A. Y., Giaever, G. & Nislow, C. Systematic prediction of antifungal drug synergy by chemogenomic screening in saccharomyces cerevisiae. Front. Fungal. Biol. https://doi.org/10.3389/ffunb.2021.683414/full (2021).
Jansen, G. et al. Chemogenomic profiling predicts antifungal synergies. Mol. Syst. Biol. 5(1), 338 (2009).
Wambaugh, M. A. et al. Synergistic and antagonistic drug interactions in the treatment of systemic fungal infections. Elife 9, e54160 (2020).
Chaturvedi, V. et al. Multilaboratory Testing of two-drug combinations of antifungals against Candida albicans, Candida glabrata, and Candida parapsilosis. Antimicrob. Agents Chemother. 55(4), 1543 (2011).
Bidaud, A. L., Schwarz, P., Herbreteau, G. & Dannaoui, E. Techniques for the assessment of in vitro and in vivo antifungal combinations. J Fungi. 7(2), 113 (2021).
Fatsis-Kavalopoulos, N., Roemhild, R., Tang, P. C., Kreuger, J. & Andersson, D. I. CombiANT: Antibiotic interaction testing made easy. PLOS Biol. 18(9), e3000856 (2020).
Lee, W. B. et al. An integrated microfluidic system for antimicrobial susceptibility testing with antibiotic combination. Lab Chip 19(16), 2699–2708 (2019).
Shao, F. et al. Automated and miniaturized screening of antibiotic combinations via robotic-printed combinatorial droplet platform. Acta Pharm. Sin. B 14(4), 1801–1813 (2024).
Cacace, E. et al. Systematic analysis of drug combinations against Gram-positive bacteria. Nat Microbiol. 8, 1–17 (2023).
Fatsis-Kavalopoulos, N., Roelofs, L. & Andersson, D. I. Potential risks of treating bacterial infections with a combination of β-lactam and aminoglycoside antibiotics: A systematic quantification of antibiotic interactions in E. coli blood stream infection isolates. EBioMedicine 78, 103979 (2022).
Tang, P. C., Sánchez-Hevia, D. L., Westhoff, S., Fatsis-Kavalopoulos, N. & Andersson, D. I. Within-species variability of antibiotic interactions in Gram-negative bacteria. MBio 15(3), e0019624 (2024).
Fatsis-Kavalopoulos, N., Sánchez-Hevia, D. L. & Andersson, D. I. Beyond the FIC index: The extended information from fractional inhibitory concentrations (FICs). J. Antimicrob. Chemother. 79(9), 2394–2396 (2024).
Hall, M. J., Middleton, R. F. & Westmacott, D. The fractional inhibitory concentration (FIC) index as a measure of synergy. J. Antimicrob. Chemother. 11(5), 427–433 (1983).
Loewe, S. The problem of synergism and antagonism of combined drugs. Arzneimittelforschung 3(6), 285–290 (1953).
Meletiadis, J., Pournaras, S., Roilides, E. & Walsh, T. J. Defining fractional inhibitory concentration index cutoffs for additive interactions based on self-drug additive combinations, Monte Carlo simulation analysis, and in vitro-in vivo correlation data for antifungal drug combinations against Aspergillus fumigatus. Antimicrob. Agents Chemother. 54(2), 602–609 (2010).
Te Dorsthorst, D. T. A. et al. In vitro interaction of flucytosine combined with amphotericin B or fluconazole against thirty-five yeast isolates determined by both the fractional inhibitory concentration index and the response surface approach. Antimicrob. Agents Chemother. 46(9), 2982–2989 (2002).
Deng, S. et al. Combination of amphotericin B and terbinafine against melanized fungi associated with chromoblastomycosis. Antimicrob. Agents Chemother. 62(6), e00270-e318 (2018).
Marchetti, O., Moreillon, P., Glauser, M. P., Bille, J. & Sanglard, D. Potent synergism of the combination of fluconazole and cyclosporine in Candida albicans. Antimicrob. Agents Chemother. 44(9), 2373–2381 (2000).
Guinea, J., Meletiadis, J., Arikan-Akdagli, S., Giske, C., Muehlethaler, K., Arendrup, M. C. and the, Subcommittee on Antifungal Susceptibility Testing (AFST) of the ESCMID European Committee for, et al. Method for the determination of broth dilution minimum inhibitory concentrations of antifungal agents for yeasts (EUCAST, 2023). https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/AFST/Files/EUCAST_E.Def_7.4_Yeast_definitive_revised_2023.pdf
Vahedi-Shahandashti, R., Stubenböck, M. M. & Lass-Flörl, C. The influence of medium composition on EUCAST and Etest antifungal susceptibility testing. J. Fungi 9(10), 973 (2023).
Tobudic, S., Kratzer, C., Lassnigg, A., Graninger, W. & Presterl, E. In vitro activity of antifungal combinations against Candida albicans biofilms. J. Antimicrob. Chemother. 65(2), 271–274 (2010).
Nagy, F. et al. In vitro and in vivo interaction of caspofungin with isavuconazole against Candida auris planktonic cells and biofilms. Med. Mycol. 59(10), 1015 (2021).
Bidaud, A. L., Botterel, F., Chowdhary, A. & Dannaoui, E. In Vitro antifungal combination of flucytosine with Amphotericin B, voriconazole, or micafungin against Candida auris shows no antagonism. Antimicrob Agents Chemother. 63(12), e01393 (2019).
Katragkou, A. et al. In vitro combination therapy with isavuconazole against Candida spp. Med Mycol. 55(8), 859–868 (2017).
Vazquez, J. A., Arganoza, M. T., Vaishampayan, J. K. & Akins, R. A. In vitro interaction between amphotericin B and azoles in Candida albicans. Antimicrob. Agents Chemother. 40(11), 2511 (1996).
Yang, Q. et al. In vitro synergistic antifungal activities of caspofungin in combination with fluconazole or voriconazole against candida species determined by the Etest method. Int. J. Infect. Dis. 1(122), 982–990 (2022).
Lewis, R. E., Lund, B. C., Klepser, M. E., Ernst, E. J. & Pfaller, M. A. Assessment of antifungal activities of fluconazole and amphotericin B administered alone and in combination against Candida albicans by using a dynamic in vitro mycotic infection model. Antimicrob. Agents Chemother. 42(6), 1382–1386 (1998).
Rex, J. H. et al. A randomized and blinded multicenter trial of high-dose fluconazole plus placebo versus fluconazole plus amphotericin B as therapy for candidemia and its consequences in nonneutropenic subjects. Clin. Infect. Dis. 36(10), 1221–1228 (2003).
Meletiadis, J., Beredaki, M. I., Elefanti, A., Pournaras, S. & Muller, A. In vitro–in vivo correlation of posaconazole–amphotericin B combination against Candida albicans: In vitro interacting concentrations are associated with in vivo free drug levels. J. Fungi 9(4), 434 (2023).
Drusano, G. L. Antimicrobial pharmacodynamics: Critical interactions of “bug and drug”. Nat. Rev. Microbiol. 2(4), 289–300 (2004).
Bollenbach, T. Antimicrobial interactions: Mechanisms and implications for drug discovery and resistance evolution. Curr. Opin. Microbiol. 27, 1–9 (2015).
Matuschek, E., Brown, D. F. J. & Kahlmeter, G. Development of the EUCAST disk diffusion antimicrobial susceptibility testing method and its implementation in routine microbiology laboratories. Clin. Microbiol. Infect. 20(4), O255–O266 (2014).
Vitale, R. G., Afeltra, J. & Dannaoui, E. Antifungal Combinations. In Antifungal Agents: Methods and Protocols (eds Ernst, E. J. & Rogers, P. D.) 143–152 (Humana Press, 2005). https://doi.org/10.1385/1-59259-943-5:143.
Funding
Open access funding provided by Uppsala University. Funding was provided by grants awarded to VÖ and DIA by the Swedish Foundation for Strategic Research. Funders had no input in the investigation, analysis or decision to publish.
Author information
Authors and Affiliations
Contributions
Conceptualization: NFK, DA, VÖ, TUA Formal analysis: NFK, HL Funding acquisition: DA, VÖ Investigation: NFK, HL, RS Methodology: NFK, HL Writing—original draft: NFK, HL Writing—review and editing: all authors.
Corresponding authors
Ethics declarations
Competing interests
Authors NFK and DIA hold shares and have decision making capacity in Rx Dynamics AB. All the remaining authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lundvik, H., Santini, R., Altintop, T.U. et al. Fast detection of synergy and antagonism in antifungal combinations used against Candida albicans clinical isolates. Sci Rep 15, 36103 (2025). https://doi.org/10.1038/s41598-025-22870-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-22870-x