Abstract
Hajj, the annual pilgrimage to Makkah, Saudi Arabia, attracts around two million Muslims from across the globe, making it one of the world’s largest mass gatherings. This event is associated with different public health challenges due to the scale of participation, the diversity of attendees, the complexity of the rituals, and the extreme physical and environmental conditions individuals encounter on their pilgrimage. This study employed the Haddon Matrix and Combined Model frameworks to categorize risk factors into pre-event, during-event, and post-event phases. A comprehensive literature review was conducted, and data were extracted from peer-reviewed articles on health outcomes associated with Hajj. Factors across human, environmental, and agent domains were analyzed, and the effectiveness of various public health strategies to reduce adverse outcomes during Hajj was assessed. This study comprehensively examined the factors contributing to morbidity and adverse outcomes during Hajj. Cardiovascular diseases, respiratory infections, and heat-related illnesses were identified as the primary causes of morbidity, and older adults and individuals with pre-existing conditions were more affected.
Similar content being viewed by others
Introduction
Hajj, the annual pilgrimage to Makkah, Saudi Arabia, attracts over two million Muslims from across the globe, making it one of the world’s largest mass gatherings (MGs). This event is associated with different public health challenges, which are attributable to the scale of participation, the diversity of attendees, and the severe physical and environmental conditions pilgrims encounter1. The pilgrims move to the Holy Site of Mina on 8th of Dhul-Hijja for Hajj ritual days; they spend the day of the 9th of Dhul-Hijja in Arafat before a short stay in the Muzdalifah area, where around two million pilgrims perform the physically demanding Hajj rituals across these sites every year2. This MG in a complex, highly dense crowd in high-temperature environments poses significant public health risks, including the transmission of infectious diseases, exacerbating pre-existing health conditions, trauma, and environment-related health problems3. The Saudi government employs a well-coordinated, inter-sectoral approach to managing Hajj-related public health challenges, including the increased demand for health services. Pilgrims receive free healthcare through numerous permanent and seasonal hospitals, healthcare centers in Makkah and Madinah, and medical teams accompanying pilgrims cohorts4. Despite the availability of healthcare access, Hajj pilgrims encounter various health challenges. Cardiovascular diseases are a leading cause of death among pilgrims, especially in individuals with pre-existing conditions, such as hypertension, diabetes, and obesity5. Pilgrims also experience respiratory infections; community-acquired pneumonia has been identified as one of the leading causes of morbidity and adverse outcomes, especially among pilgrims over 65 and those with chronic conditions (e.g., asthma and chronic obstructive pulmonary disease)3,6. In addition, heat-related illnesses (HRIs), where long walks in an arid climate, present a significant risk to individuals with pre-existing health conditions and those without adequate knowledge to mitigate HRIs7.
This study assessed the determinants of morbidity and adverse outcomes during Hajj using two analysis tools: the Haddon Matrix and the Combined Model. The Haddon Matrix categorizes factors into pre-event, during-event, and post-event phases across human, agent, and environmental domains, and the Combined Model evaluates the effectiveness of interventions by mapping public health strategies to each phase8,9. Using these models, this study intends to determine critical intervention points and propose a comprehensive plan to decrease adverse outcomes during Hajj.
Methodology
This study applied a mixed-methods approach using theoretical frameworks and data analysis to evaluate the factors contributing to morbidity and adverse outcomes during Hajj. Data were systematically extracted from peer-reviewed articles focusing on Hajj-related health outcomes (i.e., cardiovascular diseases, respiratory infections, and HRIs). The Haddon Matrix was used to classify the contributing factors into pre-event, during-event, and post-event, considering human, agent, and environmental domains. Moreover, the Combined Model (Fig. 1) was used to assess public health strategies in each phase and provide a structured evaluation of intervention effectiveness. This study was based on secondary data from peer-reviewed sources and emphasized empirical outcomes and their relevance to the research objectives. The research did not directly involve human participants, so ethical approval was not required. The study acknowledged the limitations of this type of research, such as potential biases in the original datasets and the challenges of analyzing and interpreting diverse data sources.
Key determinants affecting morbidity and adverse outcomes during Hajj
The analysis was structured using the Haddon Matrix, categorizing factors into the pre-event, during-event, and post-event phases. These were further examined across the human (host), agent, physical environment, and socio-cultural environment domains. The detailed breakdown is presented in Table 1.
Pre-event factors
Older pilgrims and age-related health issues
Older pilgrims (especially those over 60 years old) are more vulnerable to health issues during Hajj because they are more likely to have pre-existing cardiovascular diseases, decreased physical endurance, and increased susceptibility to infections compared with younger pilgrims10. Previous studies have indicated that the mean age of hospitalized pilgrims is approximately 60 years, and cardiovascular and respiratory diseases are the leading causes of in-patient adverse outcomes11,12. Also, as older adults are also more susceptible to respiratory infections and HRIs, a higher incidence of pneumonia and heat exhaustion has been reported in older pilgrims13,14.
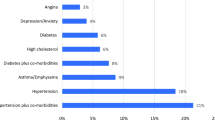
Chronic health conditions
Pilgrims with chronic illnesses, such as cardiovascular diseases, diabetes, and hypertension, might encounter a higher risk of complications due to strenuous physical activities and harsh environmental conditions during Hajj. A study conducted at a tertiary care hospital in Makkah identified a strong link between pre-existing cardiac conditions and increased adverse outcomes12. Similarly, diabetes and hypertension increase health risks during Hajj. Reports from King Abdul Aziz Hospital in Makkah found that these conditions were significant predictors of adverse health outcomes; pilgrims with these health issues were more likely to experience complications, such as acute kidney injury15,16.
Infectious diseases and risks associated with a lack of vaccination
Respiratory diseases also jeopardize pilgrims. A study on Indonesian Hajj pilgrims found that respiratory conditions, especially pneumonia, contributed significantly to adverse outcomes17. Chronic respiratory diseases are common comorbidities in patients admitted to the intensive care unit (ICU) during Hajj and increase the risk of severe sepsis and septic shock18. Furthermore, despite the importance of vaccines, vaccination rates could be suboptimal among pilgrims as many lack awareness and hold misconceptions about vaccine efficacy19 Thus, many pilgrims counter the high risk of contracting preventable diseases like influenza and meningococcal disease. For example, although the seasonal influenza vaccine effectively prevents laboratory-confirmed influenza, vaccination rates varied significantly among Hajj pilgrims20.
Mental health challenges
The physical and mental demands of Hajj can cause substantial mental health challenges, including stress, anxiety, and depression21. If unmanaged, these mental health issues can exacerbate physical health conditions and increase risks. Research has demonstrated that unmanaged mental health conditions contribute to severe physical health outcomes during Hajj22. In an Indian study, stress-related disorders are commonly reported, and psychological stress was identified as a pivotal contributor to morbidity among pilgrims21,23.
During-event factors
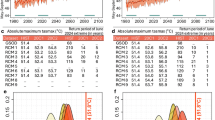
Physical environment and HRIs
Hajj is characterized by extreme heat, which coincides with summer mainly over the years, creating significant health risks, such as heat exhaustion and heat stroke24. Although the weather contributes to most of the overall heat load during Hajj, additional heat is generated by the densely crowded environment and heat contained by the mountainous terrains, asphalt, and concrete buildings9. A cross-sectional study reported a high rate of adverse outcome from heat stroke among affected pilgrims25.
Crowding and infectious disease transmission
Hajj pilgrims experience high-density crowding, which increases the risk of infectious diseases. Studies indicate that crowding during Hajj significantly increases the transmission rates of diseases like upper respiratory tract infections, which was the most common complaint during Hajj season26,27Another significant risk is poor hygiene in crowded conditions, contributing to gastrointestinal infections. In 2011, an outbreak of gastroenteritis among Iranian pilgrims was traced to contaminated food and water, revealing that the communal living conditions during Hajj can facilitate the spread of gastrointestinal pathogens28.
Walking distance and physical exhaustion
Physical exhaustion is critical during Hajj, particularly for older pilgrims and those with pre-existing conditions. The long walks and physically demanding rituals increase the risk of exhaustion, which can lead to cardiac events in individuals with underlying heart conditions. Most of these walks are not required as bus transportation are available, yet many decide to walk despite long walks in harsh conditions to avoid traffic or as a ritual of devotion29,30,31.
Delays in seeking medical attention and adherence to management plan
During the event, pilgrims may delay seeking medical attention to avoid ritual interference. This delay can worsen health outcomes and cause complications for those at high risk. A study on morbidity and health complications among Indian Hajj pilgrims identified delays in accessing medical care due to the overwhelming crowds23. A study conducted at Al Noor Specialist Hospital in Makkah found that delays in medical attention were particularly detrimental to vulnerable groups, including older adults and those with language barriers12. Indeed, managing pre-existing conditions during Hajj is challenging due to the demanding physical activities, extreme weather conditions, and the logistics of medication adherence in MGs settings32,33,34.
Post-event factors
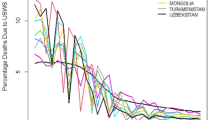
Infectious disease transmission
The risk of infectious disease transmission raises global health concerns, as pilgrims mixing from all over the world can cause the spreading of communicable diseases. The dense crowding and close physical interactions during Hajj increase the pilgrims’ risk of respiratory infections, such as influenza, pneumonia, and tuberculosis, which may then be transmitted to others after the event35. Furthermore, pilgrims may acquire antimicrobial-resistant (AMR) bacteria during Hajj; this presents additional challenges to healthcare systems, particularly among vulnerable populations, such as individuals with compromised immune function36. The large-scale international travel following Hajj leads to considerable potential for the cross-border spread of these pathogens.
Post-traumatic stress disorder (PTSD)
The intense experiences during Hajj can cause psychological trauma for some pilgrims, which can have long-term health consequences and increase the risk of adverse outcomes if they are not addressed37. The causes of this psychological trauma include high physical demands, overcrowding, witnessing or experiencing accidents, and the overall intensity of the pilgrimage experience21. A study on the psychological impact of traumatic events highlighted that trauma could result in different psychological responses, including re-experiencing the traumatic event and acute stress reactions38.
Staff burnout
Healthcare staff and volunteers providing medical services during Hajj are more vulnerable to burnout due to the intense workload, prolonged demand for care, and stress, which present an enormous burden for medical personnel. This demand and the necessity for rapid responses to medical emergencies contribute to physical and emotional exhaustion among healthcare staff. Research has found that healthcare providers working in Hajj are prone to burnout, affecting their well-being and compromising the quality of care they provide to pilgrims39. Furthermore, a study involving healthcare professionals in ICUs during Hajj found that they experience high levels of emotional exhaustion, depersonalization, and impaired personal achievement, implying a need for effective interventions to ameliorate burnout40.
Mitigation strategies for reducing morbidity and adverse outcomes during Hajj using the combined model
The corresponding findings discussed below are presented in Table 2.
Education
Implementing comprehensive educational strategies before, during, and after Hajj is highly effective in mitigating health risks among pilgrims, especially for communicable diseases and heat-related illnesses. For example, previous studies have reported that pre-Hajj educational interventions considerably improve pilgrims’ preparedness for extreme weather conditions26,41. Although these interventions are promising, further research is needed to evaluate their long-term effects, particularly in follow-up care after Hajj and a targeted approach23. Mobile applications and digital platforms have been identified as modern approaches to real-time education, although concerns remain regarding accessibility and engagement, especially among pilgrims who are unfamiliar with or uncomfortable using technology42. Additionally, education provided after Hajj is vital in managing chronic conditions that may have been exacerbated during the pilgrimage43Despite the effectiveness of current strategies, further research is required to optimize these programs and ensure that they are broadly applicable. In conclusion, ongoing evaluation and adaptation are crucial to assuring that these strategies address the rising needs of Hajj population.
Enforcement
Regulatory measures during Hajj, particularly mandatory health screenings and vaccination requirements, must be enforced to reduce the risk of infectious disease outbreaks44,45. For instance, a study conducted in 2016 underlined the importance of enforcing meningococcal vaccination; this measure aligns with broader public health strategies and represents a vital preventive measure specific to Hajj46. Although these measures are effective, their success depends on the consistency of implementation. Comprehensive surveillance and vaccination campaigns are essential, but challenges persist in ensuring that all pilgrims comply with these requirements47. Moreover, during Hajj, ongoing enforcement, such as continuous health monitoring and crowd control, is essential for managing the dense population and preventing health crises. A review supported this approach but highlighted practical challenges and obstacles in controlling large crowds, increasing concerns about the scalability of these measures48. In a particular situation such as a pandemic, pre-event screening, hygienic measures, face masks, good hygiene, social distancing, and utilizing digital technology as contact tracing are practical approaches to mitigate infection transmissions8,49.
Engineering and environmental modifications
Engineering and environmental modifications are necessary to ensure pilgrims’ safety and well-being during Hajj. An environmental impact assessment of Hajj revealed the necessity of providing proper shelters and infrastructure to mitigate heat-related risks, significantly as climate change increases the likelihood of heat stress during the pilgrimage50. This indicates a critical need for engineering solutions to protect pilgrims and decrease the occurrence of HRIs, ensuring safety throughout the event. Previous studies have documented the effectiveness of these interventions, revealing a significant reduction in heat-related health issues when such measures are in place. For example, a study conducted in 2020 assessed the impact of temperature-controlled environments on individuals with chronic conditions, such as diabetes. It demonstrated that these modifications reduce heat-related complications during Hajj51. Additionally, maintaining environmental health during the pilgrimage is essential, as it is directed toward monitoring air quality to prevent environmentally induced health issues52. Similarly, A study conducted in 2019 revealed that improvements in air quality play an essential role in reducing respiratory illnesses53.
Economic incentives
Economic incentives can promote healthy practices and support the development of health-promoting infrastructure. For example, research conducted in 2016 showed that financial incentives, such as subsidized vaccinations, significantly increased vaccination uptake among Australian Hajj pilgrims, contributing to improved health outcomes during the pilgrimage42. Providing financial assistance to pilgrims requiring emergency medical care would be highly beneficial, as would other support initiatives, such as distributing free umbrellas and hand sanitizer. These measures could help reduce the financial burden on pilgrims, promote preventive practices, and facilitate access to imperative healthcare services. Studies have highlighted that the Saudi government provides high-quality medical services to all Hajj pilgrims to ensure they receive necessary care without incurring additional costs. This comprehensive healthcare approach during Hajj spotlights the importance of reducing financial barriers to accessing critical services and preventive measures for pilgrims54. Similarly, continued financial support after the event is essential to addressing long-term health issues that may arise after the pilgrims return home. Thus, ongoing economic support is vital to maintain health improvements during the event23.
Emergency response strategies
Emergency response strategies are integral to managing health crises during Hajj. Before the event, preparation involves establishing rapid response teams trained to handle emergencies such as heat stroke and cardiac and respiratory distress. For example, studies have shown that the strategic placement of emergency medical teams and the preparation of necessary resources during the event are crucial to warranting adequate health security55. A systematic review demonstrates that proper planning and resource allocation are essential to minimizing the impact of health crises at large-scale events56. Another study demonstrated that pre-deploying emergency response units and supplies effectively managed health emergencies during Hajj, promoting pilgrims’ overall safety and well-being57. During Hajj, the Ministry of Health deploys mobile clinics and emergency response units across pilgrimage sites to provide timely medical care, and it sets up temporary shelters and medical stations to address medical needs as they arise4. These measures are components of a broader strategy to ensure that healthcare is readily available throughout the event, minimizing the health impact of emergencies. Effective coordination of these resources is essential to safeguard health during large-scale MGs58. After the event, strengthening the emergency response capacity is critical in addressing delayed health effects that may emerge. Continued preparedness and incident monitoring during and after Hajj are essential for managing potential health crises and ensuring pilgrims’ long-term safety and well-being59. Furthermore, systematic evaluations and preparedness plans are vital in maintaining high emergency readiness so that health issues after the event can be promptly addressed60.
Conclusion
This study comprehensively examined the factors contributing to morbidity and adverse outcomes during Hajj using the Haddon Matrix and Combined Model frameworks to analyze pre-event, during-event, and post-event factors. The findings indicate that cardiovascular diseases, respiratory infections, and HRIs are the primary risks among pilgrims, mainly affecting older pilgrims and those with pre-existing health conditions. This study also underscores that strategic public health interventions, including pre-Hajj medical screenings, continuous health monitoring, and targeted education and enforcement measures, are essential to minimize such risks. Additionally, engineering and environmental modifications, as well as economic incentives and robust emergency response strategies, are critical for managing the health issues posed by the unique and demanding conditions of Hajj. Although these strategies promise to reduce health risks, further robust investigation is required to evaluate their long-term effectiveness, especially regarding follow-up care after Hajj and adapting to evolving challenges, such as climate change and global health threats. Therefore, continual research and adaptive strategies are essential to ensure that interventions are effective and adapt to the changing needs of Hajj pilgrims.
Data availability
Data supporting this study are available from the corresponding author upon reasonable request.
References
Yezli, S. & Khan, A. A. The Jeddah tool: A health risk assessment framework for mass gatherings. Saudi Med. J. 41(2), 121 (2020).
Ministry of Hajj and Umrah [Internet]. [cited 2024 Dec 9]. Ministry of Hajj and Umrah. (2023). Available from: https://www.haj.gov.sa/Haj/Introduction.
Yezli, S., Yassin, Y., Mushi, A., Almuzaini, Y. & Khan, A. Pattern of utilization, disease presentation, and medication prescribing and dispensing at 51 primary healthcare centers during the Hajj mass gathering. BMC Health Serv. Res. 22(1) (2022).
Saudi MOH. Statistical Yearbook 2022 [Internet]. (2022). [cited 2024 Oct 8].Available from:https://www.moh.gov.sa/en/Ministry/Statistics/book/Documents/StatisticalYearbook-2022.pdf.
Al-Ghamdi, S. M., Akbar, H. O., Qari, Y. A., Fathaldin, O. A. & Al-Rashed, R. S. Pattern of admission to hospitals during Muslim pilgrimage (Hajj). Saudi Med. J. 24(10), 1073–1076 (2003).
Madani, T. A. et al. Causes of hospitalization of pilgrims during the Hajj period of the Islamic year 1423 (2003). Ann. Saudi Med. 26 (5), 346–351 (2006).
Khamis, N. K. Epidemiological pattern of diseases and risk behaviors of pilgrims attending Mina hospitals, Hajj 1427 h (2007 g). J. Egypt. Public. Health Assoc. 83(1–2), 15–33 (2008).
Khan, A. et al. A combined model for COVID-19 pandemic control: the application of haddon’s matrix and community risk reduction tools combined. J. Infect. Public. Health 15(2), 261–269 (2022).
Almuzaini, Y. et al. Mitigation strategies for heat-related illness during mass gatherings: Hajj experience. Front. Public. Health 10 (2022).
Murtaza, S., Abu, A. & Yussof, S. Determining the types of diseases and emergency issues in pilgrims during hajj: A literature review. Int. J. Adv. Comput. Sci. Appl. 7(10) (2016).
Ardiana, M., Utami, E. R., Al Farabi, M. J. & Azmi, Y. The impact of classical cardiovascular risk factors on hospitalization and mortality among Hajj pilgrims. Sci. World J. 2023, 1–9 (2023).
Khan, N. A. et al. Pattern of medical diseases and determinants of prognosis of hospitalization during 2005 Muslim pilgrimage Hajj in a tertiary care hospital. A prospective cohort study. Saudi Med. J. 27(9), 1373–1380 (2006).
Shirah, B. H., Zafar, S. H., Alferaidi, O. A. & Sabir, A. M. M. Mass gathering medicine (Hajj pilgrimage in Saudi Arabia): The clinical pattern of pneumonia among pilgrims during Hajj. J. Infect. Public. Health 10(3), 277–286 (2017).
Gautret, P., Soula, G., Delmont, J., Parola, P. & Brouqui, P. Common health hazards in French pilgrims during the Hajj of 2007: A prospective cohort study. J. Travel Med. 16(6), 377–381 (2009).
Yousuf, M., Al-Saudi, D. A., Sheikh, R. A. & Lone, M. S. Pattern of medical problems among Haj pilgrims admitted to King Abdul Aziz Hospital, Madinah Al-Munawarah. Ann. Saudi Med. 15(6), 619–621 (1995).
Elrewihby, W., Hasan, N., Fikry, W. & Wafa, E. Acute kidney injury in hospitalized patients during Muslim pilgrimage (Hajj: 1432). Saudi J. Kidney Dis. Transplantation. 29(5), 1128 (2018).
Pane, M. et al. Indonesian Hajj cohorts and mortality in Saudi Arabia from 2004 to 2011. J. Epidemiol. Glob Health. 9(1), 11 (2019).
Baharoon, S., Al-Jahdali, H., Al Hashmi, J., Memish, Z. A. & Ahmed, Q. A. Severe sepsis and septic shock at the hajj: Etiologies and outcomes. Travel Med. Infect. Dis. 7(4), 247–252 (2009).
Schmid, P., Rauber, D., Betsch, C., Lidolt, G. & Denker, M. L. Barriers of influenza vaccination intention and behavior—a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One. 12(1), e0170550 (2017).
Alqahtani, A. S., Rashid, H. & Heywood, A. E. Vaccinations against respiratory tract infections at Hajj. Clin. Microbiol. Infect. 21(2), 115–127 (2015).
Khan, S., Chauhan, V., Timothy, A., Kalpana, S. & Khanam, S. Mental health in mass gatherings. Ind. Psychiatry J. 25(2), 216 (2016).
Hankir, A., Chariwala, Z., Siddique, U., Carrick, F. R. & Zaman, R. Hajj and the mental health of Muslim pilgrims: A review. Psychiatr Danub. 31(Suppl 3), 290–293 (2019).
Khan, I. D. et al. Morbidity and mortality amongst Indian Hajj pilgrims: A 3-year experience of Indian Hajj medical mission in mass-gathering medicine. J. Infect. Public. Health. 11(2), 165–170 (2018).
Almuzaini, Y. et al. Characteristics and distribution of Heat-Related illnesses during Hajj 2022. Saudi J. Emerg. Med. 141–147 (2024).
Abdelmoety, D. A. et al. Characteristics of heat illness during hajj: A Cross-sectional study. Biomed. Res. Int. 2018, 1–6 (2018).
Ahmed, Q. A., Arabi, Y. M. & Memish, Z. A. Health risks at the Hajj. Lancet 367(9515), 1008–1015 (2006).
Alamri, F. A. et al. Common health complains among pilgrims during Manasik El Hajj; season 1439H (2018). Merit Res. J. Med. Med. Sci. 8, 351–360 (2020).
Emamian, M. H. & Mohammad Mohammadi, G. An outbreak of gastroenteritis among Iranian pilgrims of Hajj during 2011. Iran. Red Crescent Med. J. 15(4), 317–319 (2013).
Al-Hayani, M. M. et al. Trauma and Injuries pattern during Hajj, 1443(2022) : A cross-sectional study. Cureus (2023).
Balog, P. & Konkolÿ Thege, B. The role of vital exhaustion in predicting the recurrence of vascular events: A longitudinal study. Int. J. Clin. Health Psychol. 19(1), 75–79 (2019).
Alsofayan, Y. et al. The impact of preventive measures on acute illnesses among pilgrims during Hajj season. Saudi J. Emerg. Med. 218–224 (2021).
Ibrahim, M. et al. Recommendations for management of diabetes and its complications during Hajj (Muslim Pilgrimage) – 2024 update. Diabetes Res. Clin. Pract. 212, 111647 (2024).
Yezli, S., Yassin, Y., Mushi, A., Balkhi, B. & Khan, A. Insulin knowledge, handling, and storage among diabetic pilgrims during the Hajj mass gathering. J. Diabetes Res. 2021(1), 5596914. https://doi.org/10.1155/2021/5596914 (2021).
Yezli, S. et al. Medication Handling and Storage among Pilgrims during the Hajj Mass Gathering. in Healthcare 626 (MDPI, 2021).
Wilder-Smith, A., Foo, W., Earnest, A. & Paton, N. I. High risk of Mycobacterium tuberculosis infection during the Hajj pilgrimage. Tropical Med. Int. Health. 10 (4), 336–339 (2005).
Alreeme, S., Bokhary, H. & Craig, A. T. Transmission of antimicrobial resistant bacteria at the hajj: A scoping review. Int. J. Environ. Res. Public. Health 19(21), 14134 (2022).
Boscarino, J. Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Ann. Epidemiol. 16(4), 248–256 (2006).
McNally, R. J. Psychological mechanisms in acute response to trauma. Biol. Psychiatry. 53(9), 779–788 (2003).
RAYAN, A., SISAN, M. & Stress, B. A. K. E. R. O. Workplace Violence, and burnout in nurses working in King Abdullah medical City during Al-Hajj season. J. Nurs. Res. 27(3), e26 (2019).
Rugaan, A. et al. Burnout among ICU healthcare workers at two tertiary care hospitals in Makkah during the Hajj season. Saudi J. Med. Med. Sci. 11(1), 54–59 (2023).
Ahmed, Q. A., Barbeschi, M. & Memish, Z. A. The quest for public health security at Hajj: The WHO guidelines on communicable disease alert and response during mass gatherings. Travel Med. Infect. Dis. 7(4), 226–230 (2009).
Alqahtani, A. S. et al. Exploring barriers to and facilitators of preventive measures against infectious diseases among Australian Hajj pilgrims: Cross-sectional studies before and after Hajj. Int. J. Infect. Dis. 47, 53–59 (2016).
Al-Tawfiq, J. A. & Memish, Z. A. Mass gathering medicine: 2014 Hajj and Umra preparation as a leading example. Int. J. Infect. Dis. 27, 26–31 (2014).
Tobaiqy, M. et al. Assessment of preventative measures practice among Umrah pilgrims in Saudi Arabia, 1440H-2019. Int. J. Environ. Res. Public. Health. 18(1), 257 (2020).
Deris, Z. Z., Hasan, H., Sulaiman, S. A., Wahab MSAb, Naing, N. N. & Othman, N. H. The prevalence of acute respiratory symptoms and role of protective measures among Malaysian Hajj pilgrims. J. Travel Med. 17 (2), 82–88 (2010).
Yezli, S., Assiri, A. M., Alhakeem, R. F., Turkistani, A. M. & Alotaibi, B. Meningococcal disease during the Hajj and Umrah mass gatherings. Int. J. Infect. Dis. 47, 60–64 (2016).
Memish, Z. A. et al. Hajj: infectious disease surveillance and control. Lancet 383(9934), 2073–2082 (2014).
Memish, Z. A. et al. Mass gatherings medicine: International cooperation and progress. Lancet 383(9934), 2030–2032 (2014).
Alahmari, A. A. et al. Healthcare policies, precautionary measures and outcomes of mass gathering events in the era of COVID-19 pandemic: expedited review. J. Infect. Public. Health (2023).
Saeed, F., Schleussner, C. F. & Almazroui, M. From Paris to makkah: Heat stress risks for Muslim pilgrims at 1.5°C and 2°C. Environ. Res. Lett. 16(2), 024037 (2021).
Shaikh, S. et al. Diabetescare during Hajj.Hajj Diabetes Ther. 11(12), 2829–2844. (2020).
Siddique, A. Roads to Makkah: Ambient Air Quality and Personal Exposure Assessment During Ritual of Hajj. in Qatar Foundation Annual Research Conference Proceedings Vol. 2016(1). (Hamad bin Khalifa University Press (HBKU Press), 2016).
Liang, L. et al. Associations between daily air quality and hospitalisations for acute exacerbation of chronic obstructive pulmonary disease in Beijing, 2013–17: An ecological analysis. Lancet Planet. Health 3(6), e270–e279 (2019).
Shafi, S., Booy, R., Haworth, E., Rashid, H. & Memish, Z. A. Hajj: Health lessons for mass gatherings. J. Infect. Public. Health 1(1), 27–32 (2008).
Al-Shareef, A. S. et al. The role of emergency medical services providers during mass gathering. Saudi J. Health Sci. 11(1), 17–22 (2022).
Spaepen, K., Lajolo, C., Wang, N., Salio, F. & Hubloue, I. Standards of medical planning and response for emergency medical teams during mass gatherings: A systematic review. Prehosp Disaster Med. 38(S1), s81–s82 (2023).
Khan, I. D. et al. Indian medical mission at Hajj-2016: Mass-gathering medicine perspectives, challenges, and opportunities in a mission posture. Int. J. Travel Med. Glob Health 5(3), 94–101 (2017).
Memish, Z. A., Stephens, G. M., Steffen, R. & Ahmed, Q. A. Emergence of medicine for mass gatherings: Lessons from Hajj. Lancet Infect. Dis. 12(1), 56–65 (2012).
Zafeirakis, A. & Efstathiou, P. Health care challenges at mass gatherings. J. Clin. Med. Kaz. 6(60), 23–28 (2020).
Margalit, G., Rachaminov, O., Levy, Y., Adini, B. & Grinberg, A. Ensuring emergency preparedness through systematic evaluations. Prehosp Disaster Med. 34(s1), s76–s76 (2019).
Funding
There are no funding sources to declare.
Author information
Authors and Affiliations
Contributions
Y.A. was primarily responsible for the study conception and manuscript writing. A.K. and F.A. assisted with writing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This is a narrative review, and thus, ethical approvals were unrequired.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Almuzaini, Y., Alamri, F., Alabdullatif, L. et al. Critical determinants of morbidity and adverse outcomes during the Hajj using the Haddon matrix and the combined model. Sci Rep 15, 39824 (2025). https://doi.org/10.1038/s41598-025-23504-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-23504-y