Abstract
The pathogenesis of the coronavirus disease 2019 (COVID-19) involves a complex group of cytokines and is significantly influenced by genetic and epigenetic factors. The current study aims to assess the association of COVID-19 severity and mortality with the relative expression of MicroRNA-155 (miR-155) and its association with serum levels of interleukin (IL)-6, IL-10, and their derived ratio. This pilot case-control study included 75 COVID-19 patients and 25 healthy controls. Serum levels of cytokines were analyzed by enzyme-linked immunosorbent assay (ELISA), and assessment of miR-155 relative expression level was done using quantitative real-time PCR in all participants. We found that IL-6, IL-10, IL-6/IL-10 ratio, and miR-155 expression levels were significantly higher in COVID-19 patients than in healthy controls (p-values < 0.001). The expression level of miR-155 showed significant differences between all severity categories of COVID-19, reaching its highest levels in the severe group. It was also significantly higher in ICU-admitted patients (p-value < 0.001) and those who died during their hospital stay (p-value = 0.001). It showed a significant negative correlation with serum IL-10 (r=-0.249, p-value = 0.031) and a significant positive correlation with IL-6/IL-10 ratio (r = 0.234, p-value = 0.043). It was also the only independent risk factor for COVID-19 severity by regression analysis and the best predictor for COVID-19 severity by ROC curve analysis. This study reported elevation of cytokines and miR-155 expression in COVID-19 patients. The level of miR-155 expression was associated with COVID-19 severity, mortality, and ICU admission, indicating its potential utility as a biomarker for monitoring the progression of COVID-19 and guiding patient follow-up.
Similar content being viewed by others
Introduction
Three serious pandemics, the coronavirus disease 2019 (COVID-19), the Middle East respiratory disease (MERS) in 2012, and the severe acute respiratory syndrome (SARS) in 2003, were linked to coronaviruses1,2. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) caused the highly contagious COVID-19 infection2. Despite quarantine regulations, the virus spread fast over the world and there were no specific, effective treatments3. COVID-19 has caused a global health crisis with wide variations in disease severity, ranging from asymptomatic infection to critical illness and death. Vaccination programs have played an essential role in reducing disease spread and severity4. While most COVID-19 patients have mild symptoms and a favorable prognosis, some may experience serious fatal consequences due to hyperinflammation caused by cytokine storms5. Excessive cytokine production during the cytokine storm can trigger an uncontrolled immune response and result in lung tissue damage and multiorgan failure6. Therefore, to avoid and treat the cytokine storm early and lower mortality in patients with severe COVID-19, it is important to understand the underlying mechanisms and predisposing factors for it.
Moreover, the outcome of COVID-19 infection is significantly influenced by genetic and epigenetic factors. MicroRNAs, or miRNAs, are a significant component of the epigenetic factors that control many immune cell and viral behaviors7. Of all the miRNAs, miRNA-155 (miR-155) which has been reported to have significant regulatory effects on the immune system and inflammatory response following viral infections8,9. Many previous studies demonstrated that following viral infection, miR-155 rises with the degree of lung inflammation, disease severity, and mortality rate10,11. In addition, the inhibition of this miRNA was reported to reduce lung inflammation and mortality in models of respiratory viral infections9.
The current study aims to assess the association of COVID-19 severity and mortality with the relative expression of miR-155 and its association with serum levels of the pro-inflammatory cytokine interleukin (IL)−6, the anti-inflammatory cytokine IL-10, and their derived ratio as indicators for the cytokine storm.
Methodology
Study settings and subjects
The current pilot case-control study was conducted on 75 confirmed COVID-19 patients recruited from Ain Shams University Hospitals from September 2021 to August 2022. COVID-19 infection was routinely confirmed in all patients by the hospital’s Clinical Pathology Department using real-time reverse transcription-polymerase chain reaction (RT-PCR) (VIASURE, Bio-Rad) from respiratory specimens, according to WHO guidelines12. The study excluded participants with immunological disorders and other active illnesses, those undergoing chemotherapy or radiation therapy, and pregnant women. Twenty-five age- and sex-matched healthy controls were also included. They were selected from relatives of the patients, had no history of COVID-19 infection, and were clinically free from acute or chronic illnesses. Based on the severity of their disease, COVID-19 participants were divided equally (25 participants in each group) into three groups (mild, moderate, and severe) in accordance with the Ain Shams University Hospital Consensus Report for handling adult COVID-19 patients13. All COVID-19 participants were followed up for their outcome either in-hospital death, or discharge from the hospital and the duration of hospital stay was determined for each patient.
Clinical evaluation and sample collection
On admission, a complete medical history, clinical examination, and radiological evaluation were performed on each subject. All blood samples for biomarker assessment were collected upon admission, before the initiation of any COVID-19–related treatment, to ensure baseline measurement and avoid potential drug-related bias.
Assessment of IL-6 and IL-10
From a 3 ml serum sample that was withdrawn from each participant, serum levels of IL-6 and IL-10 were determined by enzyme-linked immunosorbent assay (ELISA) technique using commercially available human kits (BT Laboratory, Shanghai, China, Catalog Numbers: E0090Hu and E0102Hu, respectively). The sensitivity of the IL-6 kit was 1.03 pg/mL and the IL-10 kit was 2.59 pg/mL.
Assessment of miR-155 relative expression
From a 3 mL whole blood sample on an EDTA vacutainer tube that was also withdrawn from each participant, miR-155 relative expression was assessed by PCR analysis. Within an hour of the EDTA sample collection, double centrifugation was carried out. After a first centrifugation that lasted for ten minutes at 1900 ×g, the resulting plasma supernatant was carefully transferred into a separate, sterile tube and centrifuged again for ten minutes at 16,000 ×g. Until the extraction of miRNA, plasma was kept frozen at −80 °C. Plasma was selected instead of serum to avoid artificial contamination of circulating miRNAs that can occur due to the release of platelet-derived and intracellular miRNAs during the coagulation process.
MiRNA extraction, reverse transcription (RT) reaction
By the instructions of miRNeasy serum/plasma Kit (Qiagen, Germany), extraction of total miRNA from 200 µL plasma was performed. The concentration of the extracted total RNA was assesed by Qubit RNA HS assay kit on Qubit 3.0 fluorometer (Thermofisher Scientific, USA). A 5 µL of the RNA extract, containing 1–10 ng was used in the RT reaction mixture as recommended by the manufacturer. The extracted miRNA was used for further complementary DNA (cDNA) reaction using a specific stem-loop RT-primer from the MicroRNA TaqMan® assay and TaqMan® MicroRNA Reverse Transcription Kit (Applied Biosystems, USA) according to the manufacturer’s instructions. The prepared 10 µL RT-reaction was then incubated for 30 min at 16 °C and 42 °C, respectively, followed by a stop reaction of 5 min at 85 °C.
Real-Time quantitative polymerase chain reaction (RT-qPCR)
The resultant cDNA was then amplified using TaqMan Universal Master Mix and MicroRNA TaqMan® assay (ipu-miR-155 assay, cat no. 4440886, test ID: 467534_mat) and the U6 snRNA (cat no. 4427975, test ID: 001973). In brief, five microliters of RT products were used as templates in 20 µL PCR reactions containing assays of miR-155 and U6 snRNA according to the manufacturer’s handbook. The amplification mix was incubated on the Applied Biosystems 7500 Real-Time PCR Detection System with the following conditions: initial activation at 95 °C for 10 min followed by 35 cycles of denaturation at 95 °C for 15 s and annealing/extension at 60 °C for 60 s.
MiR-155 expression was normalized to U6 snRNA expression, which was selected as an endogenous control based on its consistent detection and Ct stability across all study samples. Although U6 is a commonly used reference for cellular RNA, several previous studies have validated its applicability and stability in plasma miRNA profiling, including in COVID-19 patients and other inflammatory conditions14,15,16. Relative quantification in each sample was calculated using the delta-delta Ct (2−ΔΔCT) method.
Statistical methods
Statistical presentation and analysis of the present study were conducted using the median and interquartile range (IQR) for quantitative data and number and percentage for qualitative data by the Statistical Package for Social Science (SPSS) V26 (IBM Corp., USA). The normality of quantitative data was assessed using the Shapiro–Wilk test. As most variables were not normally distributed, nonparametric tests were applied. Comparisons were done using the Mann-Whitney, Kruskal-Wallis, and Chi-square tests. For multiple group comparisons, pairwise Mann–Whitney tests were used as post-hoc analyses following the Kruskal–Wallis test. Spearman’s coefficient was used for the detection of the correlation between variables. Risk factors for COVID-19 severity were identified using logistic regression analysis by odds ratios (ORs) and 95% confidence intervals (CIs). The predicting ability for COVID-19 severity and mortality was evaluated by the receiver operating characteristic (ROC) curve analysis. Significant p-values are < 0.05.
Results
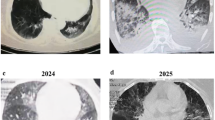
The current study included 75 COVID-19 patients, 42 (56%) males and 33 (44%) females. Their median (IQR) age was 64 (54–69.5.5) years and ranged from 29 to 88 years. Of them, 38 (50.67%) required intensive care unit (ICU) admission. Fifty-four (72%) patients were discharged alive, while 21 (28%) patients died during their hospital stay. Hypertension (52/75, 69.33%) and diabetes (38/75, 50.67%) were the most associated comorbid conditions. Regarding chest CT scan findings of the included COVID-19 patients, 6.67% (5/75) were free and 93.33% (70/75) showed bilateral ground-glass opacity (GGO). The median (IQR) of hospital stay of the COVID-19 patients was 12 (8 −15.5) days and ranged from 3 to 36 days.
Compared to the control group, COVID-19 patients showed significantly higher levels of IL-6, IL-10, IL6/IL-10 ratio, and miR-155 relative expression (p-values < 0.001) (Table 1).
When laboratory data were compared according to COVID-19 severity, IL-6, IL-6/IL-10 ratio, and miR-155 expression showed the highest values in the severe group while serum IL-10 reached its lowest level in the severe group. Serum IL-6 and IL-10 showed significant differences between mild and severe patients only (p-values = 0.003, < 0.001, respectively). IL-6/IL-10 ratio showed significant differences between mild and severe patients (p-value = 0.003) and between moderate and severe patients (p-value < 0.001). On the other hand, miR-155 expression showed significant differences between all the severity groups with p-values of < 0.001 (Table 2).
Compared to the cured and discharged COVID-19 patients (n = 54), expression levels of miR-155 and IL-6/IL-10 ratio were significantly higher in patients who died (n = 21) (p-values = 0.001), while serum level of IL-10 was significantly lower (p-value < 0.001). On the other hand, serum IL-6 did not show any significant differences between cured patients and those who died (p-value = 0.240) (Table 3).
When ICU-admitted patients (n = 38) were compared to those who were not admitted to the ICU (n = 37), serum IL-6 and IL-6/IL-10 ratio did not show any significant differences (p-value = 0.937, 0.330, respectively). On the other hand, serum IL-10 significantly decreased in ICU-admitted patients (p-value = 0.024), while miR-155 expression significantly increased (p-value < 0.001) (Table 4).
Spearman correlation study was performed and showed that miR-155 expression level was significantly negatively correlated with IL-10 (r=−0.249, p-value = 0.031) and significantly positively correlated with IL-6/IL-10 ratio (r = 0.234, p-value = 0.043) but showed no significant correlation with serum IL-6 levels (r = 0.130, p-value = 0.268). No other statistically significant correlations were observed (p-values > 0.05) (Figs. 1 and 2).
When logistic regression analysis was performed after adjustment, miR-155 expression level remained a significant (p-value = 0.014) independent risk factor for severe COVID-19, with an OR of 2.537 and a 95% CI of 1.090–4.169 (Table 5).
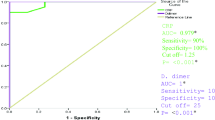
IL-6, IL-10, IL-6/IL-10 ratio, and miR-155 expression were evaluated by ROC curve analyses for prediction ability for COVID-19 severity and mortality. At a cut-off of > 15.61, miR-155 expression was the best predictor for COVID-19 severity. Its area under the curve (AUC) was 0.945, with the best diagnostic specificity (96%) and positive predictive value (91.3%) (Fig. 3).
On the other hand, serum IL-10 at a cut-off of ≤ 36 pg/mL was the best predictor for COVID-19 mortality. Its AUC was 0.846, with the best diagnostic sensitivity (85.71%) and negative predictive value (93.2%) (Fig. 4).
Discussion
The current study aimed to spotlight the interplay between miR-155 expression levels and inflammatory cytokines IL-6 and IL-10 with their derived ratio in the context of COVID-19 severity and mortality. We found that miR-155 expression levels were significantly higher in COVID-19 patients than in healthy controls. Furthermore, miR-155 was the only marker that showed significant differences between all severity categories of COVID-19, reaching its highest levels in the severe group. It was also significantly higher in ICU-admitted patients and those who died during their hospital stay. Also, it was the only independent risk factor for COVID-19 severity by regression analysis. These findings underline the potential clinical value of miR-155 as a non-invasive biomarker for disease progression and outcome prediction in COVID-19.
MiR-155 is encoded by the MIRHG155 gene, originally identified as the B-cell Integration Cluster (BIC) gene, on chromosome 2117,18. It has been extensively studied in relation to host-pathogen dynamics in human viral infections and has been linked to immune modulation19. Expression of miR-155 occurs in B cells, T cells, dendritic cells, and macrophages and is essential for cell-mediated immune responses20. In response to inflammatory stimuli, miR-155 expression was reported to be elevated within hours and is associated with pro-inflammatory transcription20.
Our results extend this understanding by demonstrating that circulating miR-155 levels are not only elevated in COVID-19 patients but also progressively increase with disease severity, reflecting its potential role as a molecular marker of hyperinflammation.
Although our study does not provide direct mechanistic evidence, previous studies have suggested that miR-155 may influence inflammatory pathways, such as SHIP1/SOCS1 and NF-κB signaling, which regulate cytokine production. For instance, miR-155 has been shown to promote IL-6 production by downregulating SHIP1 and SOCS1, negative regulators of the JAK/STAT signaling pathway18,20, and to potentiate inflammation by promoting NF-κB activity in macrophages through Toll-like receptor signaling21. Moreover, several previous studies reported that knocking out of miR-155 in mice has resulted in a decreased lung inflammatory response with fast recovery22,23. Furthermore, Koranteng et al., 200424 reported that the inflammatory response could be effectively reduced by inhibiting the miR-155/NF-kB axis. These mechanisms, reported in experimental models, may partly explain the observed associations in our study and should be further investigated in future research.
In accordance with our results, Haroun et al., 202218demonstrated that the miR-155 expression level was higher in their included COVID-19 patients than in controls and in severe COVID-19 cases than in the moderate ones. They also reported that miR-155 expression increased in non-survivals compared to survivals. Similar results were reported by Gedikbasi et al.20, and Keikha et al., 202325. They found that the relative expression of miR-155 was significantly increased with the increase in COVID-19 severity. Furthermore, Garg et al., 202126, reported that miR-155 expression levels were significantly higher in COVID-19 patients than in healthy controls and patients with influenza-associated acute respiratory distress syndrome.
By confirming and extending these observations, our data reinforce the reproducibility of miR-155 upregulation in COVID-19 and further establish its association with clinical severity and mortality, highlighting its prognostic relevance.
On the other hand, Kassif-Lerner et al., 202227 found a significant decrease in miR-155 expression levels in COVID-19 patients than controls as mild patients had 2.5-fold less miR-155 and severe patients had 5-fold less miR-155 with no significant difference in miR-155 expression between mild and severe COVID-19 patients. They also reported that patients who died had significantly less miR-155 than patients who survived. These discrepancies from our findings may not only be attributed to their relatively small sample size (37 patients) but also to several methodological and biological factors. Differences in patient demographics and clinical characteristics, including age, comorbidities, and disease stage at sampling, could have influenced miRNA expression. Additionally, variations in the timing of sample collection relative to infection onset, differences in RNA extraction protocols, and the choice of internal reference or normalization strategy for miRNA quantification may have contributed to the contrasting results. Together, these factors highlight the complexity of comparing miRNA expression studies across heterogeneous cohorts.
Additionally, miR-155 expression in the current study was the best predictor for COVID-19 severity with a diagnostic sensitivity of 84% and diagnostic specificity of 96% at a cut-off of > 15.61. This high discriminative power suggests that miR-155 could be clinically valuable for early risk stratification of COVID-19 patients. Haroun et al., 202218 found that the AUC for miR-155 expression was 0.75 with 76% sensitivity and specificity for the prediction of COVID-19 severity. Also, Garg et al., 202126 found that miR-155 had a strong discriminative power between COVID-19 and influenza-associated acute respiratory distress syndrome with an AUC of 1.00. Our results thus bridge the gap between studies, positioning miR-155 as a promising yet context-dependent biomarker that warrants validation in larger, multicentric cohorts.
Due to interindividual variability in serum IL-6 levels according to the time of the same day and variations in the associated immune-metabolic comorbidities like obesity, we evaluated the IL-6/IL-10 ratio since serum IL-6 levels alone may not be an accurate indication of COVID-associated hyperinflammation28. McElvaney et al., 202028 used the changes in the IL-6/IL-10 ratio to derive a scoring system and found that each 1-point increase in the score was associated with an increased risk for a more severe outcome by 5.6 times. In the current study, we found that serum IL-6, IL-10, and IL-6/IL-10 ratio were significantly higher in COVID-19 patients than controls. Serum IL-6 and IL-6/IL-10 ratio reached their highest levels in the severe group, while serum IL-10 reached the lowest levels in the severe group.
The pathogenesis of COVID-19 involves a complex group of mediators, including IL-6 and IL-1029. Several studies reported elevation of serum IL-6 and IL-10 in COVID-19 patients, and this elevation was dramatic with severe COVID-19 due to hyperactivation of the humoral immune system29,30,31,32. The discrepancy between our study and the other research regarding IL-10 levels could be attributed to the differences in sample sizes and techniques used in cytokine identification with different sensitivities. Also, we did not study the molecular background and regulatory mechanisms on the cellular level that may impact this cytokines’ expression level.
Moreover, in the current study, miR-155 expression had a negative correlation with serum IL-10 and a positive correlation with IL-6/IL-10 ratio. However, these correlations were weak despite reaching statistical significance and therefore should be interpreted with caution. They suggest a potential but not definitive relationship between miR-155 and cytokine balance in COVID-19. In addition, miR-155 expression showed no significant correlation with serum IL-6 alone. According to Mahesh et al., 201933, IL-10 can suppress the transcription factor Ets2, which reduces miR-155 expression. Additionally, it has been found that inhibiting miR-155 reduces IL-6 expression by 31%34. This is because miR-155 induces the IL-6 signaling pathway through the transcription factor C/EBPβ, which in turn stimulates the production of the IL-6 gene35. This study is the first to evaluate the association between miR-155 expression levels and the IL-6/IL-10 ratio as a more stable marker for COVID-associated hyperinflammation.
However, several limitations should be acknowledged. First, the sample size was limited, particularly after subdividing COVID-19 patients based on disease severity, which may have impacted the statistical power of our findings. Additionally, the study did not account for comorbid conditions or other potential confounding factors that could have influenced the results. Furthermore, as this was a single-center study conducted in Egypt, the findings may not be fully generalizable to other populations or healthcare settings. Another limitation is the limited number of cytokines analyzed, as only IL-6 and IL-10 were measured, which may not fully reflect the complexity of the immune-inflammatory response in COVID-19. Moreover, the study lacked long-term follow-up of discharged patients, which would have provided valuable insights into the sustained impact of miR-155 and cytokine levels. The limited sample size also imposed certain statistical constraints, particularly after stratification by disease severity.
Future studies are recommended to include larger, multi-center, and more ethnically diverse cohorts to enhance the generalizability of the findings. Incorporating a broader panel of cytokines and microRNAs, along with detailed clinical and immunological profiling, would provide a more comprehensive understanding of the immune-inflammatory landscape in COVID-19. Longitudinal studies with extended follow-up are also encouraged to evaluate the prognostic and therapeutic potential of miR-155 and related biomarkers over time. Moreover, adjustment for common comorbidities and treatment regimens in multivariate models will help clarify their independent contributions to disease severity and outcomes.
Conclusions
In conclusion, our study contributes to the growing evidence highlighting the elevation of inflammatory cytokines with their derived ratio (IL-6/IL-10) and miR-155 expression in COVID-19 patients. Importantly, our findings suggest that miR-155 expression holds significant prognostic value being associated with COVID-19 severity, mortality, and ICU admission, indicating its potential utility as a biomarker for monitoring the progression of COVID-19 and guiding patient follow-up. The prognostic relevance of miR-155 underscores its potential role in improving clinical outcomes by enabling more precise risk stratification and targeted interventions in COVID-19 management. Taken together, our clinical findings, in line with previous experimental reports, indicate a possible role of miR-155 in modulating inflammatory responses. However, this remains a hypothesis-generating observation that requires validation through mechanistic studies. These insights pave the way for further research into the interplay between miR-155 and inflammatory cytokines in the context of COVID-19, with implications for both clinical practice and therapeutic development.
Data availability
All the data needed to support the current findings will be available upon request.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- MERS:
-
The Middle East respiratory disease
- SARS:
-
The severe acute respiratory syndrome
- SARS-CoV-2:
-
The severe acute respiratory syndrome coronavirus 2
- IL:
-
Interleukin
- RT-PCR:
-
Real-time reverse transcription-polymerase-chain reaction
- ELISA:
-
Enzyme-linked immunosorbent assay
- ICU:
-
Intensive care unit
- GGO:
-
Ground-glass opacity
References
Peiris, M. & Poon, L. L. M. Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) (Coronaviridae). Encyclopedia of Virology. :814–24. (2021). https://doi.org/10.1016/B978-0-12-814515-9.00138-7. Epub 2021 Mar 1. PMCID: PMC7837069.
Gorbalenya, A. et al. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 5 (4), 536–544. https://doi.org/10.1038/s41564-020-0695-z (2020). Epub 2020 Mar 2. PMID: 32123347; PMCID: PMC7095448.
Jiang, Y. et al. Cytokine storm in COVID-19: from viral infection to immune responses, diagnosis and therapy. Int. J. Biol. Sci. 18 (2), 459–472. https://doi.org/10.7150/ijbs.59272 (2022). PMID: 35002503; PMCID: PMC8741849.
Kandeel, A. et al. COVID-19 vaccination coverage in egypt: a large-scale National survey - to help achieving vaccination target, March-May, 2022. BMC Public. Health. 23 (1), 397. https://doi.org/10.1186/s12889-023-15283-w (2023). PMID: 36849954; PMCID: PMC9969364.
Elessawy, S. M., Shehab, A., Soliman, D. A., Eldeeb, M. A. & Taha, S. I. Interferon-Induced Transmembrane Protein-3 Rs12252-G Variant Increases COVID-19 Mortality Potential in Egyptian Population. Viral Immunol. 37(4):186–193. (2024). https://doi.org/10.1089/vim.2024.0015. PMID: 38717821.
Jose, R. J. & Manuel, A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med. ;8(6):e46-e47. doi: 10.1016/S2213-2600(20)30216-2. Epub 2020 Apr 27. PMID: 32353251; PMCID: PMC7185942. (2020).
Asadpour-Behzadi, A., Kariminik, A. & Kheirkhah, B. MicroRNA-155 is a main part of proinflammatory puzzle during severe coronavirus disease 2019 (COVID-19). Allergol Immunopathol (Madr). 51(2):115–119. (2023). https://doi.org/10.15586/aei.v51i2.698. PMID: 36916095.
Lind, E. F. & Ohashi, P. S. Mir-155, a central modulator of T-cell responses. Eur J Immunol. ;44(1):11 – 5. (2014). https://doi.org/10.1002/eji.201343962. PMID: 24571026.
Soltani-Zangbar, M. S. et al. SARS-CoV2 infection induce miR-155 expression and skewed Th17/Treg balance by changing SOCS1 level: A clinical study. Cytokine 169, 156248 (2023). Epub 2023 Jun 8. PMID: 37307689; PMCID: PMC10247889.
Arroyo, M. et al. Airway mir-155 responses are associated with TH1 cytokine polarization in young children with viral respiratory infections. PLoS One. 15 (5), e0233352. https://doi.org/10.1371/journal.pone.0233352 (2020). PMID: 32442188; PMCID: PMC7244143.
Natekar, J. P., Rothan, H. A., Arora, K., Strate, P. G. & Kumar, M. Cellular microRNA-155 regulates virus-Induced inflammatory response and protects against lethal West nile virus infection. Viruses 12 (1), 9. https://doi.org/10.3390/v12010009 (2019). PMID: 31861621; PMCID: PMC7019255.
World Health Organization. Coronavirus disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. (2021). Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situationreports [Last accessed November 22, 2021].
Abdelfattah, E. et al. Hospital response to COVID-19 A consensus report on Ain Shams university hospital strategy. ScienceOpen Preprints. https://doi.org/10.14293/S2199-1006.1.SOR-.PPD4QZX.v1 (2020).
Belete, M. A. et al. The potential of Circulating MicroRNAs as novel diagnostic biomarkers of COVID-19: a systematic review and meta-analysis. BMC Infect. Dis. 24 (1), 1011. https://doi.org/10.1186/s12879-024-09915-8 (2024). PMID: 39300343; PMCID: PMC11414062.
Pollet, K. et al. Host MiRNAs as biomarkers of SARS-CoV-2 infection: a critical review. Sens. Diagnostics. 2 (1), 12–35. https://doi.org/10.1039/d2sd00140c (2023).
de Santana Silva, Í. T. S. et al. Identification of SnRNA U6 as an endogenous reference gene for normalization of MiRNA expression data in COVID-19 patients. Sci. Rep. 15 (1), 26636. https://doi.org/10.1038/s41598-025-04062-9 (2025). PMID: 40695852; PMCID: PMC12284167.
Hu, J. et al. miR-155: an important role in inflammation response. J. Immunol. Res. 2022, 7437281. https://doi.org/10.1155/2022/7437281 (2022). PMID: 35434143; PMCID: PMC9007653.
Haroun, R. A. et al. Circulating plasma miR-155 is a potential biomarker for the detection of SARS-CoV-2 infection. Pathology 54 (1), 104–110. https://doi.org/10.1016/j.pathol.2021.09.006 (2022). Epub 2021 Nov 6. PMID: 34838331; PMCID: PMC8570980.
Li, Y. & Kowdley, K. V. MicroRNAs in common human diseases. Genomics Proteom. Bioinf. 10 (5), 246–253. https://doi.org/10.1016/j.gpb.2012.07.005 (2012). Epub 2012 Sep 29. PMID: 23200134; PMCID: PMC3611977.
Gedikbasi, A. et al. The effect of host MiRNAs on prognosis in COVID-19: miRNA-155 May promote severity via targeting suppressor of cytokine signaling 1 (SOCS1) gene. Genes (Basel). 13 (7), 1146. https://doi.org/10.3390/genes13071146 (2022). PMID: 35885930; PMCID: PMC9320261.
Mann, M. et al. An NF-κB-microRNA regulatory network tunes macrophage inflammatory responses. Nat Commun. 8(1):851. (2017). https://doi.org/10.1038/s41467-017-00972-z. Erratum in: Nat Commun. 2018; 9(1):3338. DOI: 10.1038/s41467-018-05720-5. PMID: 29021573; PMCID: PMC5636846.
Pociask, D. A. et al. Epigenetic and transcriptomic regulation of lung repair during recovery from influenza infection. Am. J. Pathol. 187 (4), 851–863 (2017). Epub 2017 Feb 10. PMID: 28193481; PMCID: PMC5397680.
De Smet, E. G. et al. The role of miR-155 in cigarette smoke-induced pulmonary inflammation and COPD. Mucosal Immunol. 13 (3), 423–436. https://doi.org/10.1038/s41385-019-0241-6 (2020). Epub 2019 Dec 9. PMID: 31819170.
Koranteng, R. D. et al. Differential regulation of mast cell cytokines by both dexamethasone and the p38 mitogen-activated protein kinase (MAPK) inhibitor SB203580. Clin. Exp. Immunol. 137 (1), 81–87. https://doi.org/10.1111/j.1365-2249.2004.02510.x (2004). PMID: 15196247; PMCID: PMC1809098.
Keikha, R., Hashemi-Shahri, S. M. & Jebali, A. The MiRNA neuroinflammatory biomarkers in COVID-19 patients with different severity of illness. Neurologia 38 (6), e41–e51. https://doi.org/10.1016/j.nrl.2021.06.005 (2023 Jul-Aug). Epub 2021 Jul 16. PMID: 34305233; PMCID: PMC8282440.
Garg, A. et al. Circulating cardiovascular MicroRNAs in critically ill COVID-19 patients. Eur. J. Heart Fail. 23 (3), 468–475 (2021). Epub 2021 Mar 5. PMID: 33421274; PMCID: PMC8014268.
Kassif-Lerner, R. et al. miR-155: A potential biomarker for predicting mortality in COVID-19 patients. J. Pers. Med. 12 (2), 324. https://doi.org/10.3390/jpm12020324 (2022). PMID: 35207812; PMCID: PMC8877479.
McElvaney, O. J. et al. A linear prognostic score based on the ratio of interleukin-6 to interleukin-10 predicts outcomes in COVID-19. EBioMedicine. 61: 103026. DOI: 10.1016/j.ebiom.2020.103026. Epub 2020 Oct 8. Erratum in: EBioMedicine. 2020; 62: 103116. (2020). https://doi.org/10.1016/j.ebiom.2020.103116. PMID: 33039714; PMCID: PMC7543971.
Han, H. et al. Profiling serum cytokines in COVID-19 patients reveals IL-6 and IL-10 are disease severity predictors. Emerg. Microbes Infect. 9 (1), 1123–1130 (2020). PMID: 32475230; PMCID: PMC7473317.
Zhao, Y. et al. Longitudinal COVID-19 profiling associates IL-1RA and IL-10 with disease severity and RANTES with mild disease. JCI Insight. 5 (13), e139834. https://doi.org/10.1172/jci.insight.139834 (2020). PMID: 32501293; PMCID: PMC7406242.
Wang, F. et al. The laboratory tests and host immunity of COVID-19 patients with different severity of illness. JCI Insight. 5 (10), e137799. https://doi.org/10.1172/jci.insight.137799 (2020). PMID: 32324595; PMCID: PMC7259533.
Coomes, E. A. & Haghbayan, H. Interleukin-6 in Covid-19: A systematic review and meta-analysis. Rev. Med. Virol. 30 (6), 1–9. https://doi.org/10.1002/rmv.2141 (2020). Epub 2020 Aug 26. PMID: 32845568; PMCID: PMC7460877.
Mahesh, G. & Biswas, R. MicroRNA-155: A master regulator of inflammation. J. Interferon Cytokine Res. 39 (6), 321–330. https://doi.org/10.1089/jir.2018.0155 (2019). Epub 2019 Mar 20. PMID: 30998423; PMCID: PMC6591773.
Pfeiffer, D., Roßmanith, E., Lang, I. & Falkenhagen, D. miR-146a, miR-146b, and miR-155 increase expression of IL-6 and IL-8 and support HSP10 in an in vitro sepsis model. PLoS One. 12 (6), e0179850. https://doi.org/10.1371/journal.pone.0179850 (2017). PMID: 28662100; PMCID: PMC5491059.
Ceppi, M. et al. MicroRNA-155 modulates the interleukin-1 signaling pathway in activated human monocyte-derived dendritic cells. Proc. Natl. Acad. Sci. U S A. 106 (8), 2735–2740. https://doi.org/10.1073/pnas.0811073106 (2009). Epub 2009 Feb 4. PMID: 19193853; PMCID: PMC2650335.
Acknowledgements
None.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The authors received no financial support for the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Contributions
The study design was done by all authors. SIT and RAG did the investigations and wrote the manuscript. SHF, MMM, AO, and DHHE shared in clinical evaluation and sample collection and reviewed the manuscript.EME and MH shared in the investigations and reviewed the manuscript.BO and RAA did the formal analysis and edited and reviewed the manuscript.All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Not applicable.
Ethical approval and consent to participate
The Ain Shams University Faculty of Medicine’s Research Ethics Committee (REC) authorized the current study protocol (# FMASU R 156/2021). Before they could take part in the study, we gave each participant an explanation of the procedures and got their written informed consent. This research complies with the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Taha, S.I., Fouad, S.H., El-Sehsah, E.M. et al. Role of immune-inflammatory biomarkers and their derived ratio in predicting COVID-19 severity and mortality. Sci Rep 15, 39003 (2025). https://doi.org/10.1038/s41598-025-24173-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-24173-7