Abstract
Low birth weight (LBW) is a critical public health concern in Pakistan, significantly contributing to neonatal mortality and long-term health disparities. Consanguineous marriages, highly prevalent in the region, are associated with adverse birth outcomes. While antenatal care (ANC) visits are crucial for improving maternal and child health, their role in mediating the relationship between consanguinity and LBW remains underexplored. This study investigates whether ANC visits mediate the association between consanguineous marriage and LBW in Pakistan. This cross-sectional study utilized data from the 2017–18 Pakistan Demographic and Health Survey (PDHS), analyzing 14,465 live births. Consanguineous marriage was the independent variable, ANC visits (categorized as ≥ 8 vs. <8) served as the mediating variable, and LBW (< 2500 g vs. ≥2500 g) was the dependent variable. Generalized Structural Equation Modeling (GSEM) with 2000 bootstrap replications was employed to estimate direct and indirect effects, adjusting for maternal age, region, residence, household wealth, and working status. Consanguineous marriage was significantly associated with a reduction in the likelihood of adequate ANC visits (β=−0.015, p < 0.001). ANC visits, in turn, showed a strong and statistically significant negative association with LBW (β=−0.403, p < 0.001). The lmediation analysis revealed a statistically significant indirect effect of consanguineous marriage on LBW through reduced ANC utilization (β = 0.0062, p = 0.001; 95% CI: 0.0026 to 0.0098). A significant direct positive association between consanguineous marriage and LBW also persisted (β = 0.0173, p = 0.035; 95% CI: 0.0012 to 0.0335), confirming a partial mediation effect. Our findings indicate that consanguineous marriage increases the risk of LBW in Pakistan, partially mediated by reduced antenatal care utilization. This suggests that both behavioral (reduced ANC uptake) and potentially biological (genetic) pathways contribute to adverse birth outcomes in consanguineous unions. Targeted interventions are needed to increase ANC access and utilization, particularly in rural and low-income consanguineous communities, alongside promoting women’s healthcare autonomy and genetic counseling to mitigate the burden of LBW.
Similar content being viewed by others
Introduction
Low birth weight (LBW) is defined as a birth weight of less than 2,500 g regardless of gestational age—is a significant public health challenge linked to increased neonatal mortality, developmental delays, and chronic diseases later in life. Globally, LBW affects approximately 16% of live births, with higher prevalence in developing countries (19%) compared to developed nations (7%)1,2.In Pakistan, the prevalence ranges from 19% in urban areas to as high as 32% in rural settings, contributing substantially to under-five mortality, stunting, and long-term health disparities3,4One factor receiving increasing attention in relation to LBW is consanguineous marriage, unions between biologically related individuals, particularly first cousins. These marriages remain common in Pakistan and other South Asian and Middle Eastern countries due to cultural, economic, and familial preferences5,6,7,8,9Prior studies suggest a link between consanguinity and adverse birth outcomes, including LBW, due to both genetic factors (increased homozygosity and recessive disorders) and social factors such as lower maternal autonomy and limited healthcare access10,11,12,13,14.
Antenatal care (ANC) visits are widely recognized as an effective intervention for improving maternal and neonatal health. The World Health Organization (WHO) recommends a minimum of eight ANC visits to identify and manage risks during pregnancy, ensure timely interventions, and promote positive health-seeking behaviors15,16. Studies show that inadequate ANC is strongly associated with higher LBW risk2,15,16,17. Yet, the role of ANC in mediating the relationship between consanguinity and LBW remains underexplored. Given that consanguineous unions are often embedded in patriarchal family systems, women in such marriages may face sociocultural and logistical barriers to accessing ANC services, including restricted mobility, low autonomy, and reduced decision-making power18. These mechanisms suggest that ANC use could vary significantly by consanguinity status and may act as a mediating pathway influencing LBW.
To address this gap, the present study investigates whether ANC visits mediate the association between consanguineous marriage and low birth weight in Pakistan, using nationally representative data and a generalized structural equation modeling (GSEM) approach. By exploring both direct and indirect effects, this study contributes to a more nuanced understanding of how consanguinity influences neonatal health. This study is grounded in Andersen’s Behavioral Model of Health Services Use19, which posits that healthcare utilization is influenced by individual, contextual, and enabling factors. Consanguineous marriage may act as a predisposing factor that shapes healthcare behaviors through sociocultural norms, gender roles, and household decision-making dynamics. In particular, women in consanguineous unions may experience greater social control from extended family networks, limiting their autonomy to seek timely and adequate ANC.
Furthermore, Life Course Theory (LCT)20 suggests that early-life exposures such as maternal health behaviors and structural disadvantages accumulate to affect child health outcomes. From this perspective, consanguinity can be seen as both a biological and a structural determinant of LBW, with ANC visits serving as a potential buffer or protective factor.
Based on the literature and theoretical framing, we propose the following hypotheses:
-
H1: Consanguineous marriage is positively associated with low birth weight.
-
H2: Antenatal care visits are negatively associated with low birth weight.
-
H3: Consanguineous marriage is negatively associated with antenatal care utilization.
-
H4: Antenatal care visits mediate the relationship between consanguineous marriage and low birth weight.
According to Andersen’s Behavioral Model, healthcare utilization is shaped by predisposing, enabling, and need-based factors19. Consanguineous marriage can be conceptualized as a predisposing factor, reflecting entrenched cultural norms and kinship structures that influence maternal autonomy and decision-making. These sociocultural constraints often reduce women’s ability to seek timely and adequate ANC services, thereby creating a behavioral pathway from consanguinity to ANC utilization. The empirical model captures this mechanism in the negative association between consanguineous marriage and ANC visits.
Life Course Theory (LCT) emphasizes how early exposures and structural disadvantages accumulate to affect health trajectories across time20. In this study, consanguinity represents a structural exposure that can influence neonatal health through two channels: (1) behavioral, by reducing maternal ANC utilization; and (2) biological, by increasing homozygosity for recessive alleles associated with fetal growth restriction10,21,22. ANC visits function as a buffering mechanism in this framework, mitigating some of the adverse effects of consanguinity on birth outcomes. This dual pathway, behavioral (reduced ANC) and biological (genetic risks) is consistent with the partial mediation observed in our empirical analysis, where consanguinity predicted both lower ANC utilization and directly increased the likelihood of low birth weight.
Literature review
Low birth weight remains a major contributor to neonatal mortality and morbidity globally, accounting for 80% of neonatal deaths23,24,25,26. In Pakistan, the burden is disproportionately high due to poor maternal health, malnutrition, and inadequate healthcare access. Risk factors for LBW include preterm birth, maternal undernutrition, infection, and insufficient antenatal care15,17,27. While several population-based studies have documented LBW prevalence in Pakistan, there is limited research exploring the role of socio-cultural practices such as consanguinity.
Multiple studies across South Asia and the Middle East have found a significant association between consanguineous marriage and LBW10,11,21,28. A meta-analysis of 24 studies concluded that consanguinity, particularly first-cousin unions, is linked to lower birth weight and higher rates of genetic disorders21. In Pakistan, where consanguinity rates are among the highest globally, studies have reported similar associations29,30. Biological mechanisms such as increased expression of autosomal recessive genes, along with social factors like reduced maternal autonomy and lower healthcare access, are believed to underlie this relationship31,32 .
ANC visits are shown to reduce the risk of LBW by enabling early detection of pregnancy complications, promoting maternal nutrition, and facilitating timely interventions15,16. Research also indicates that lower maternal education and restricted autonomy often prevalent in consanguineous marriages, are associated with fewer ANC visits18,33. Some studies have explored ANC as a mediator between women’s empowerment or education and birth outcomes34,35, but few have examined its role in the context of consanguinity.
Emerging evidence suggests that cultural norms embedded in consanguineous family structures can discourage healthcare-seeking behaviors. Women in such marriages may lack decision-making authority, face restrictions on mobility, or prioritize traditional over biomedical care, all of which reduce ANC utilization18 This makes ANC a theoretically grounded and empirically testable mediator in the relationship between consanguinity and LBW.
Based on the literature above we can expect that antenatal care visits play a significant impact on the children’s low birth weight, therefore in Fig. 1. we propose the following conceptual framework.
Data and study design
This study utilizes cross-sectional data from the 2017–18 Pakistan Demographic and Health Survey (PDHS), a nationally representative survey conducted every five years by the National Institute of Population Studies (NIPS) with technical support from the United States Agency for International Development (USAID) and other partners. The survey employed a stratified two-stage sampling design, selecting 580 clusters from all provinces and regions of Pakistan—including Azad Jammu and Kashmir (AJK), Gilgit Baltistan (GB), and the former Federally Administered Tribal Areas (FATA). In each cluster, 28 households were systematically chosen, resulting in a total sample of approximately 16,240 households. Ever-married women aged 15–49 were interviewed in all selected households, while data on men, children, and selected health indicators were collected in one-third of households. Due to security concerns, 19 clusters were excluded from the final sample. To ensure national and subnational representativeness, sampling weights were applied to adjust for non-proportional allocation. This study specifically draws on the individual record (IR) dataset, which provides detailed birth histories for all live births reported by women aged 15–49. Each observation in the IR file represents a single live birth, allowing for robust child-level analysis. The dataset includes comprehensive information on maternal, child, household, and contextual characteristics relevant to birth outcomes, antenatal care visits and consanguineous marriages.
Study population and sample
A total of 15,778 ever-married women aged 15–49 were interviewed. Among these, around 63.8% reported being in consanguineous marriages. Additionally, a total of 12,708 children were born in the five years preceding the survey.
Dependent variable
The dependent variable is weight at birth dichotomized as low birth weight (< 2500 g) and average birth weight (≥2500 g). If the birth weight is less than 2500 g we categorized it as low birth weight and coded it as “1”, and if the birth weight is equal or more than 2500 g we categorized it as average birth weight and coded it as “0”. Data collectors, who underwent training, requested detailed birth histories from each respondent (i.e., mothers) for children born in the last five years. The survey encompassed inquiries about antenatal, delivery, and postnatal complications. Birth weights were documented in grams based on birth records36 We incorporated birth weight records due to their greater reliability compared to birth weights reported by mothers. This approach aimed to minimize the potential for introducing recall bias in the study37. Only information about the latest-born child was considered. Data from mothers who experienced stillbirths were omitted from the analysis.
Independent variable
The independent variable is consanguineous marriages. In the survey, women were asked whether they had a blood relationship with their husbands. If the answer is yes, we categorized it as “1”, or if there is no relationship, we categorized it as “0”.
While the PDHS dataset provides information on degrees of relatedness (e.g., first cousin, second cousin, other relatives), for this study we operationalized consanguinity as a binary variable (yes/no). This decision was made to (i) maintain comparability with prior studies in Pakistan and South Asia that predominantly use binary measures12,30, and (ii) preserve statistical power by avoiding small cell sizes when stratifying by multiple degrees of kinship.
Mediating variable
The mediating variable is the “Number of antenatal care (ANC) visits.” This variable was derived from the DHS by this question, “How many times did you receive ANC during this pregnancy?” The response was then categorized as “0” if the number of visits is less than 8, or “1” otherwise, aligning with the WHO-recommended eight-visit ANC model established in 201615. While WHO recommends ≥ 8 ANC visits, we also examined ≥ 4 visits given evidence from Pakistan and similar LMICs that even intermediate ANC frequency reduces LBW risk14,29,30. This dual-threshold approach balances global benchmarks with local feasibility.
Covariates
The study controlled for key socio-demographic variables, including respondent age (grouped in 5-year intervals from 15 to 49), region (Punjab, Sindh, Khyber Pakhtunkhwa, Balochistan, Gilgit-Baltistan, Azad Jammu and Kashmir, FATA, and Islamabad), place of residence (urban/rural), household wealth quintile, and working status. The household wealth index was constructed using principal component analysis (PCA), based on housing characteristics, access to utilities, and asset ownership. Households were categorized into five wealth quintiles: poorest (1) to richest (5), each representing 20% of the population. Table 1 presents details on the variable measurements.
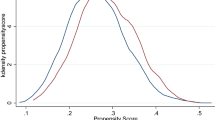
Analytical strategy
This study employed a multi-stage analytical approach to investigate the relationship between consanguineous marriages and low birth weight (LBW), with antenatal care (ANC) visits examined as a potential mediating factor. Initially, descriptive statistics were used to summarize the characteristics of the study population. Bivariate associations were assessed using Spearman’s rank correlation. Subsequently, Generalized Structural Equation Modeling (GSEM) was utilized to estimate both direct and indirect effects, given its suitability for modeling binary outcomes and capturing complex mediation pathways. Model adequacy was assessed through multicollinearity diagnostics, with all variance inflation factors (VIFs) remaining below 3, indicating no significant multicollinearity. Furthermore, a likelihood ratio test demonstrated that the mediation model provided a significantly better fit compared to the base model (χ²(1) = 713.24, p < 0.001). To ensure the robustness of findings, a series of sensitivity analyses were conducted, including: (1) alternative model specifications using probit and logit link functions, (2) stratified analyses by urban and rural residence and confounding. All observations included in the analysis had complete data on these variables. Therefore, no imputation or case-wise deletion was necessary, and the results reflect a complete-case analysis. All analyses were performed using Stata version 18.0, with sampling weights applied to ensure representativeness of the national population.
Results
Table S1 (see supplementary file). presents the summary statistics of variables with respect to low birth weight. Out of 14,465 births, 45.9% were classified as low birth weight (LBW). A higher proportion of LBW cases occurred among children born to women in consanguineous marriages (62.7%) and those with fewer than eight antenatal care (ANC) visits (98.6%). LBW was more prevalent among older mothers (35 + years), urban residents, and those from both the richest (24.5%) and poorest (15.2%) wealth quintiles. Women who were not working made up the majority of the sample, though working women accounted for a slightly higher share among LBW births (14.8%).
Table 2. presents the spearman correlation results indicate that consanguineous marriage is significantly and negatively associated with antenatal care (ANC) visits (ρ = − 0.047, p < 0.01), suggesting reduced ANC utilization among women in consanguineous unions. ANC visits are, in turn, negatively correlated with low birth weight (ρ = − 0.210, p < 0.01), highlighting their protective role. However, the direct correlation between consanguineous marriage and low birth weight is weak and non-significant (ρ = 0.003, p = 0.737), implying that the impact of consanguinity on birth weight may be mediated through ANC access rather than a direct effect.
Table 3 presents the results of the Generalized Structural Equation Modeling (GSEM) assessing the direct and indirect relationships between consanguineous marriages, antenatal care (ANC) visits, and low birth weight (LBW), adjusting for socioeconomic and demographic factors.
In the first equation (Outcome 1: ANC visits), consanguineous marriage was significantly associated with a reduction in the likelihood of attending adequate ANC visits (β = -0.015, p < 0.001), suggesting that women in consanguineous unions were less likely to receive recommended antenatal care. Wealth index was positively associated with ANC visits (β = 0.036, p < 0.001), indicating that higher economic status increases access to care. Age also showed a significant negative association (β = -0.017, p < 0.001), implying that older women were less likely to receive ANC. Region, residence, and working status were not statistically significant predictors in this equation.
In the second equation (Outcome 2: Low birth weight), ANC visits had a strong and statistically significant negative association with LBW (β = -0.403, p < 0.001), confirming the protective effect of adequate antenatal care on birth outcomes. Consanguineous marriage showed a small but significant positive association with LBW (β = 0.017, p = 0.028), indicating an increased risk of LBW among children born from consanguineous unions. Wealth index was positively associated with birth weight (β = 0.050, p < 0.001), while maternal age was also positively related to birth weight (β = 0.090, p < 0.001). Region, residence, and working status did not exhibit significant associations with LBW in this model, except working status, which showed a modest but significant positive effect (β = 0.035, p = 0.002).
These findings suggest a partial mediation effect, where consanguineous marriage negatively affects ANC visits, which in turn increases the risk of low birth weight. Additionally, consanguineous marriage retains a direct positive association with LBW, even after adjusting for ANC and other covariates.
Results from GSEM of antenatal care visits 4 and more
Table S2 (see supplementary file) presents the results indicate that women in consanguineous marriages were significantly less likely to receive at least four antenatal care (ANC) visits (β = − 0.020, SE = 0.007, z = − 2.69, p = 0.007). Household wealth was a strong positive predictor of ANC utilization (β = 0.074, SE = 0.003, z = 25.30, p < 0.001), while increasing maternal age was associated with substantially lower ANC use (β = − 0.061, SE = 0.002, z = − 28.42, p < 0.001). Region (β = − 0.002, p = 0.315), residence (β = − 0.013, p = 0.118), and maternal working status (β = 0.002, p = 0.818) were not statistically significant predictors of ANC visits.
In terms of birth outcomes, having at least four ANC visits was strongly protective against low birth weight (LBW), with a large negative effect (β = − 0.551, SE = 0.008, z = − 69.81, p < 0.001). Consanguineous marriage showed a positive but only marginally significant association with LBW (β = 0.013, SE = 0.007, z = 1.81, p = 0.070). Wealth remained a strong protective factor (β = 0.077, SE = 0.003, z = 26.90, p < 0.001), while maternal age was also positively associated with higher LBW risk (β = 0.064, SE = 0.002, z = 30.64, p < 0.001). Regional variation was marginal (β = − 0.003, p = 0.072), and rural residence was modestly protective compared to urban residence (β = − 0.015, SE = 0.008, z = − 1.98, p = 0.048). Maternal working status was significantly associated with an increased likelihood of LBW (β = 0.034, SE = 0.010, z = 3.38, p = 0.001).
Figure 2. Shows that consanguineous marriage was significantly associated with a reduction in the likelihood of attending adequate ANC visits (β = -0.015, p < 0.001), whereas ANC visits had a strong and statistically significant negative association with LBW (β = -0.403, p < 0.001), furthermore consanguineous marriage showed a small but significant positive association with LBW (β = 0.017, p = 0.028),
Rural-Urban senstivity analysis
Tables S3 and S4 (see supplementary file) report separate generalized structural equation models (GSEM) for urban and rural subsamples in supplementary file. The results show that consanguineous marriage significantly reduced the likelihood of attending adequate antenatal care (ANC) visits in both contexts, though the effect was slightly stronger in urban areas (β = −0.250, p = 0.002) compared to rural areas (β = −0.240, p = 0.038). Household wealth index was a consistently strong positive predictor of ANC attendance across both samples, while maternal age showed a significant negative association. Regional variation was evident only in rural areas (β = −0.065, p = 0.038).
For the outcome of low birth weight (LBW), ANC visits exerted a large and statistically significant protective effect in both settings (urban: β = −2.560, p < 0.001; rural: β = −2.275, p < 0.001). This confirms the robustness of ANC as a determinant of healthier birth outcomes regardless of place of residence.
The key divergence arose in the direct association between consanguineous marriage and LBW. In urban areas, consanguinity was not associated with LBW (β = 0.004, p = 0.944), while in rural areas, it showed a statistically significant positive effect (β = 0.155, p = 0.004). This rural–urban difference (Δβ = 0.151) suggests that the adverse effect of consanguineous unions on low birth weight is context-dependent, being more pronounced in rural environments where structural barriers to maternal health services are greater.
Other predictors behaved consistently across residence groups. Wealth index was positively associated with higher birth weight in both rural (β = 0.237, p < 0.001) and urban (β = 0.238, p < 0.001) settings, with virtually identical magnitudes. Maternal age showed a stronger positive effect on LBW outcomes in urban areas (β = 0.487, p < 0.001) compared to rural (β = 0.354, p < 0.001). Working status was significant only in rural areas (β = 0.191, p = 0.010).
Mediation analysis of the effect of consanguineous marriage on low birth weight via ANC visits
To assess the mediating role of antenatal care (ANC) visits in the relationship between consanguineous marriage and low birth weight (LBW), we conducted a mediation analysis using 2000 bootstrap replications. Table 5, revealed a statistically significant indirect effect of consanguineous marriage on LBW through ANC visits (β = 0.0062, p = 0.001; 95% CI: 0.0026 to 0.0098), indicating that reduced ANC utilization partially mediates the effect of consanguineous unions on adverse birth outcomes. The direct effect of consanguineous marriage on LBW, independent of ANC, also remained significant (β = 0.0173, p = 0.035; 95% CI: 0.0012 to 0.0335). The total effect combining both pathways was significant (β = 0.0236, p = 0.005; 95% CI: 0.0070 to 0.0401).These findings confirm a partial mediation.
Predicted probabilities and public health relevance
Using the overall prevalence of low birth weight in the sample (45.9%) as the baseline, children whose mothers achieved eight or more antenatal care (ANC) visits had a predicted probability of 36.2% of being born with LBW, compared to 45.9% among those with fewer than eight visits. This corresponds to an absolute risk reduction of 9.7% points and an odds ratio of 0.67. In practical terms, approximately 10–11 additional women would need to complete the recommended ANC schedule to prevent one case of LBW.
By contrast, the direct association between consanguineous marriage and LBW was modest. Infants born in consanguineous unions had a predicted LBW probability of 46.3%, only slightly higher than the 45.9% baseline, reflecting an absolute risk increase of about 0.4% points (OR = 1.02). Despite this small effect at the individual level, the high prevalence of consanguineous marriages in Pakistan of 64% implies that even marginal increases in risk translate into a substantial number of additional LBW cases at the population level.
Discussion
This study provides new insights into the complex relationship between consanguineous marriage and low birth weight (LBW), emphasizing the mediating role of antenatal care (ANC) utilization. Our findings indicate that women in consanguineous unions are significantly less likely to receive the recommended number of ANC visits, and this reduced utilization partially mediates the increased risk of LBW observed in such marriages.
The inverse relationship between consanguinity and ANC visits (β = − 0.015, p < 0.001) may reflect a mix of cultural, social, and structural barriers. In highly consanguineous communities, family networks are often tightly knit and patriarchal, which can limit women’s autonomy in seeking healthcare18. Previous studies in Pakistan and the Middle East have found that women in such unions are more likely to experience limited decision-making power, lower health literacy, and increased dependence on male relatives for mobility and healthcare access32,33.These dynamics explain the significantly lower ANC utilization rates among consanguineous couples in our sample.
Moreover, the indirect effect of consanguinity on LBW through ANC visits (β = 0.0062, p = 0.001) underscores ANC’s role as a protective factor. ANC provides critical services including fetal growth monitoring, nutritional counseling, and early detection of complications all of which reduce LBW risk15,17,38. In our model, ANC was strongly associated with reduced odds of LBW (β = − 0.403, p < 0.001), confirming findings from earlier studies in Pakistan, India, and other LMICs, which estimate that adequate ANC can reduce LBW risk by up to 40% in high-risk pregnancies33,39,40,41. Interestingly, we also observed a direct positive association between consanguineous marriage and LBW (β = 0.017, p = 0.028), independent of ANC use. This suggests that biological and genetic mechanisms may also contribute to adverse birth outcomes. Prior research indicates that consanguineous unions increase the likelihood of homozygosity for harmful recessive genes, thereby raising the risk of fetal growth restriction and congenital disorders10,21,29,42. The persistence of the direct effect in our adjusted model supports the hypothesis that consanguinity influences LBW through both behavioral (reduced ANC) and biological (genetic) pathways.
Subgroup and sensitivity analyses reinforced these conclusions. The negative effect of consanguinity on ANC was more pronounced in rural areas (β = − 0.203) than urban areas (β = − 0.148, not significant), suggesting that geographic disparities in access to care may amplify the health risks associated with consanguineous unions. Additionally, the consistency of results across logit and probit models further supports the robustness of our findings.
These results align with Life Course Theory (LCT), which posits that health trajectories are shaped by cumulative exposures and structural conditions across time20. In our case, consanguinity represents a culturally rooted exposure that influences healthcare utilization and child health outcomes. Our findings also support Andersen’s Health Care Utilization Model19 which emphasizes how enabling factors (e.g., household wealth, geography) and predisposing factors (e.g., cultural norms) shape care-seeking behavior.
Limitation and future research
This study has several limitations that should be acknowledged. First, although the analysis is based on nationally representative data, it remains observational, which limits causal inference despite the use of advanced methods such as generalized structural equation modeling (GSEM) and mediation analysis. Unobserved confounding may still influence the associations observed, particularly in the relationship between consanguineous marriage, ANC utilization, and birth outcomes.Second, the possibility of selection bias cannot be ruled out. While the dataset is robust, women who did not survive pregnancy or who were excluded due to missing data on key variables (though minimal in our final sample) may differ systematically in ways that affect the results.Third, recall bias may be present, especially in self-reported measures such as the number of antenatal care visits and birth weight. Although birth weight data are collected close to the time of delivery, inaccuracies due to memory lapses or social desirability bias could affect validity.Fourth, despite controlling for several socio-demographic factors, we could not include certain clinical and genetic variables such as parental health history, nutritional status, or detailed measures of consanguinity (e.g., degree of relatedness) which may confound the observed relationships. Finally, the analysis was limited to the variables available in the Pakistan Demographic and Health Survey, which constrained the ability to explore cultural or psychosocial mechanisms underlying care-seeking behavior.Future research should aim to incorporate longitudinal or prospective designs to better capture causal pathways and reduce recall error. Incorporating qualitative methods could also help unpack cultural beliefs and family dynamics influencing ANC utilization in consanguineous settings. Additionally, studies examining genetic markers and biological pathways could complement behavioral and epidemiological analyses, offering a more holistic understanding of how consanguineous marriage affects child health.
Policy and economic perspective
The findings of this study also carry significant policy and economic implications. Although the direct effect of consanguinity on low birth weight (LBW) was small at the individual level, the population-level burden is substantial given that nearly two-thirds of marriages in Pakistan are consanguineous. Improving antenatal care (ANC) coverage therefore represents a highly cost-effective intervention in this high-risk group. Our predicted probability estimates suggest that achieving the recommended ≥ 8 ANC visits reduces the risk of LBW by approximately 9.7% points (from 45.9% to 36.2%). At the national level, with nearly 5.6 million live births annually in Pakistan, this reduction would translate into roughly 540,000 fewer LBW cases each year if ANC coverage were universally achieved. Even focusing only on consanguineous unions, where around 64% of births occur, scaling up ANC utilization could prevent an estimated 345,000 LBW cases annually. From an economic standpoint, the cost of providing adequate ANC is modest compared to the downstream costs of LBW. Evidence from low- and middle-income countries shows that each LBW case adds significant expenditure in neonatal intensive care, prolonged hospitalization, and long-term developmental support. The World Health Organization (WHO) estimates that the cost of a full ANC package in South Asia is approximately US$40–60 per pregnancy, while the direct medical costs of managing a single LBW infant can exceed US$300–500 in the neonatal period alone. When longer-term consequences such as impaired cognitive development, reduced educational attainment, and lost productivity are factored in, the economic burden becomes several times higher.
Thus, even modest investments in strengthening ANC utilization through targeted subsidies, community health worker outreach, and culturally tailored interventions in consanguineous communities are likely to yield substantial cost savings for the health system. More importantly, they would deliver large public health gains in terms of reducing neonatal mortality, preventing stunting and undernutrition, and improving life-course outcomes. These findings align with global evidence that ANC is among the most cost-effective maternal health interventions and highlight the urgency of prioritizing ANC scale-up in high-consanguinity populations.
Conclusion
This study investigated the association between consanguineous marriages and low birth weight, emphasizing the mediating role of antenatal care (ANC) visits. Using cross-sectional data from the Pakistan Demographic and Health Survey and applying a generalized structural equation model, we found that both consanguineous marriage and ANC visits are significantly associated with low birth weight. Importantly, ANC visits partially mediated the relationship, highlighting their protective role in mitigating the adverse effects of consanguinity on birth outcomes. Based on these insights, we recommend targeted policy interventions, community education programs, and improved access to ANC services, particularly in high-risk and underserved populations.However, the study is subject to certain limitations, including its cross-sectional design, which limits causal inference. Future research should employ longitudinal designs to better understand the causal pathways linking consanguinity, healthcare utilization, and birth outcomes over time.
Data availability
The data utilized in this manuscript can also be obtained from corresponding author on reasonable request.
References
UNICEF. UNICEF data: monitoring the situation of children and women available from Apr, (2017). https://webcache.googleusercontent.com/search?q=cache: xLTqZdN1qEIJ: https://data.unicef.org/topimaternal-health/antenatal-care/+ &cd = 1&hl = om&ct = clnk≷ = et. Updated.
Azhar, M. et al. Nutritional management of low birth weight and preterm infants in low-and low middle-income countries. Neonatology 122 (Suppl. 1), 209–223 (2025).
Class, Q. A. et al. Birth weight, physical morbidity, and mortality: a population-based sibling-comparison study. Am. J. Epidemiol. 179 (5), 550–558 (2014).
Olusanya, B. O. & Ofovwe, G. E. Predictors of preterm births and low birthweight in an inner-city hospital in sub-Saharan Africa. Matern. Child Health J. 14, 978–986 (2010).
Bittles, A. H. et al. Reproductive behavior and health in consanguineous marriages. Science 252 (5007), 789–794 (1991).
Bittles, A. H. A Background Summary of Consanguineous Marriage (Center for Human Genetics, Edith Cowan University, 2001).
Islam, M. M. The practice of consanguineous marriage in oman: prevalence, trends and determinants. J. Biosoc. Sci. 44 (5), 571–594 (2012).
Popescu, G. et al. Social and demographic determinants of consanguineous marriage: insights from a literature review. Genealogy 9 (3), 69 (2025).
Saleem, M. U. et al. Consanguineous marriages and child ever Born—The moderating role of working women. Am. J. Hum. Biology. 37 (5), e70043 (2025).
Bittles, A. H. Consanguinity in Context63 (Cambridge University Press, 2012).
Shawky, R. M. et al. Consanguineous matings among Egyptian population. Egypt. J. Med. Hum. Genet. 12 (2), 157–163 (2011).
Hussain, R. & Bittles, A. H. The prevalence and demographic characteristics of consanguineous marriages in Pakistan. J. Biosoc. Sci. 30 (2), 261–275 (1998).
Tunçbilek, E. & Koç, İ. Consanguineous marriage in Turkey and its impact on fertility and mortality. Ann. Hum. Genet. 58 (4), 321–329 (1994).
Amadou, C. et al. Long-term health in individuals born preterm or with low birth weight: A cohort study. Pediatr. Res. 97 (2), 577–585 (2025).
Organization, W. H. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience (World Health Organization, 2016).
Goldenberg, R. L. et al. Epidemiology and causes of preterm birth. Lancet 371 (9606), 75–84 (2008).
Lattof, S. R. et al. Implementation of the new WHO antenatal care model for a positive pregnancy experience: a monitoring framework. BMJ Global Health. 5 (6), e002605 (2020).
Sahin, E., İnciser Paşalak, Ş. & Seven, M. Consanguineous marriage and its effect on reproductive behavior and uptake of prenatal screening. J. Genet. Couns. 29 (5), 849–856 (2020).
Kabir, M. R. Adopting andersen’s behavior model to identify factors influencing maternal healthcare service utilization in Bangladesh. PloS One. 16 (11), e0260502 (2021).
Jones, N. L. et al. Life course approaches to the causes of health disparities. Am. J. Public Health. 109 (S1), S48–S55 (2019).
Mumtaz, G. et al. Effect of consanguinity on birth weight for gestational age in a developing country. Am. J. Epidemiol. 165 (7), 742–752 (2007).
Wong, M. K. Y. et al. Fertility of adults born very preterm or with very low birth weight. JAMA Netw. Open. 8 (3), e251164–e251164 (2025).
Lee, A. C. et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Global Health. 1 (1), e26–e36 (2013).
Lawn, J. E. et al. Every newborn: progress, priorities, and potential beyond survival. Lancet 384 (9938), 189–205 (2014).
Blencowe, H. et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379 (9832), 2162–2172 (2012).
Nawaz, R. et al. Association between antenatal care visits and under-five mortality: an analysis of the Pakistan demographic and health surveys. PloS One. 20 (4), e0318668 (2025).
Kim, H. et al. Incomplete antenatal care despite high coverage: geographic and. Front. Public. Health. 13, 1625379 (2025).
Adam, H. et al. Impact of major congenital anomalies on preterm birth and low birth weight. Sci. Rep. 15 (1), 24872 (2025).
Bittles, A. H. Consanguinity and its relevance to clinical genetics. Clin. Genet. 60 (2), 89–98 (2001).
Iqbal, S. et al. Consanguineous marriages and their association with women’s reproductive health and fertility behavior in pakistan: secondary data analysis from demographic and health Surveys, 1990–2018. BMC Women’s Health. 22 (1), 118 (2022).
Latif, A. et al. Association between consanguineous marriage and still birth: evidence from district Nankana Sahib Pakistan. Rawal Med. J., 48(1). (2023).
Tariq, J. et al. Factors associated with undernutrition in children under the age of two years: secondary data analysis based on the Pakistan demographic and health survey 2012–2013. Nutrients 10 (6), 676 (2018).
Bellizzi, S. & Padrini, S. Quality utilization of antenatal care and low birth weight: evidence from 18 demographic health surveys. East. Mediterr. Health J. 26 (11), 1381–1387 (2020).
Morón-Duarte, L. S. et al. Quality of antenatal care and its sociodemographic determinants: results of the 2015 Pelotas birth cohort, Brazil. BMC Health Serv. Res. 21, 1–14 (2021).
Abedin, S. & Arunachalam, D. Maternal autonomy and high-risk pregnancy in bangladesh: the mediating influences of childbearing practices and antenatal care. BMC Pregnancy Childbirth. 20, 1–8 (2020).
Kayode, G. A. et al. Contextual risk factors for low birth weight: a multilevel analysis. PloS One. 9 (10), e109333 (2014).
Channon, A. A., Padmadas, S. S. & McDonald, J. W. Measuring birth weight in developing countries: does the method of reporting in retrospective surveys matter? Matern. Child Health J. 15, 12–18 (2011).
Aga, M. A. & Woldeamanuel, B. T. Nutritional and prenatal care factors associated with low birth weight among full-term infants in public hospitals of addis Ababa, Ethiopia. BMJ Paediatrics Open. 9 (1), e003732 (2025).
Florey, C. V. & Taylor, D. J. The relation between antenatal care and birth weight. Rev. Epidemiol. Sante Publique. 42 3, 191–197 (1994).
Banik, M. et al. Low birth weight and associated factors among newborn babies-A comparative cross-sectional study. Asian J. Med. Health. 21 (4), 32–41 (2023).
Abdal Qader, M. A. et al. Influence of antenatal care on birth weight: a cross sectional study in Baghdad City, Iraq. BMC Public. Health. 12, A38–A38 (2012).
Shaikh, A. A. et al. A survey to analyze the need of genetic counseling among doctors in Lahore, Pakistan. J. Genetic Counseling, 34(2): p. e1990. (2025).
Acknowledgements
The author would like to thank Xi’an Jiao tong University for all the support and assistance to conduct this research.
Author information
Authors and Affiliations
Contributions
The authors’ contributions to this work are as follows: Muhammad Usman Saleem conceived the study, Muhammad Usman Saleem and Abdul Ghani Khatir collected and analyzed data, Muhammad Usman Saleem, Abdul Ghani Khatir, drafted the manuscript, and Ambreen Saleem reviewed and Muhmmad Fazel Akbary help in revising the article. All authors approved the final version and are collectively accountable for the research’s content and integrity.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Saleem, M.U., Saleem, A., Khatir, A.G. et al. Consanguineous marriages and low birth weight mediating role of antenatal care visits. Sci Rep 15, 40614 (2025). https://doi.org/10.1038/s41598-025-24261-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-24261-8