Abstract
The beneficial effects of albumin use have been suggested in various clinical settings including critically ill patients. However, the association between intraoperative albumin administration and acute kidney injury (AKI) after noncardiac surgery is unclear. This is a retrospective, hospital registry-based study including 39,336 adult patients who underwent intermediate to high risk noncardiac surgery between January 2011 and June 2019 at single tertiary hospital. The patients were divided into two groups based on exposure to 5% albumin during intraoperative period. The primary outcome was the incidence of AKI within seven days after surgery. Among 39,336 patients, 1725 (4.4%) patients were administered 5% albumin during the intraoperative period. The incidence of AKI was 3.4% (1285/37,611) in the albumin non-exposure group and 13.0% (225/1725) in the albumin exposure group. After 1:3 propensity score matching, 5221 patients (albumin non-exposures 3697; albumin exposures 1524) were included in the analysis. After propensity score matching and adjustment for residual confounders, albumin exposure was associated with higher risk of postoperative AKI (odds ratio = 1.82; 95% confidence interval, 1.41–2.34; p < 0.001). This association persisted in sensitivity analyses, including a subgroup with estimated blood loss < 500 mL (odds ratio = 2.40; 95% confidence interval, 1.76–3.28; p < 0.001), and in the entire cohort (odd ratio = 2.44; 95% confidence interval, 1.97–3.02; p < 0.001). Intraoperative 5% albumin use during noncardiac surgery was associated with increased risk of postoperative AKI. Our results should be verified in further studies to guide the optimal choice of fluid in noncardiac surgery.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a common complication following noncardiac surgery, associated with increased morbidity, prolonged hospital stays, and higher mortality rates1,2,3. AKI is a syndrome with multifactorial etiologies, involving hemodynamic instability, ischemia–reperfusion injury, and inflammation, highlights the complexity of prevention and management strategies4,5. Among potential interventions, intravenous fluid administration is the mainstay in the initial treatment of hemodynamic instability during the intraoperative period6. Traditionally, colloid solutions have been used along with crystalloid solution to achieve optimal intravascular volume, because colloids have been suggested to address volume deficiency more effectively with smaller volumes7. Nevertheless, whether colloid solutions are clinically superior to crystalloid solutions with respect to AKI remains a subject of considerable debate8.
Human albumin has been widely used to maintain circulating blood volume in various clinical situations such as trauma, blood loss from surgery, septic shock, and burn management9,10. Of note, it has been reported that albumin may exert clinical benefit in critically ill patients by reducing oxidative stress, inflammatory reaction, and stabilizing the endothelial glycocalyx integrity11,12,13,14. This hypothesis has led clinicians to expand the use of albumin to noncardiac surgery in the belief that it may also improve postoperative outcomes in noncardiac surgical patients. However, the rationale for albumin administration in non-cardiac surgery remains weak, and the question of whether albumin improves postoperative renal function in this context remains unclear. Considering the expanding landscape of noncardiac surgeries in the current era, a comprehensive understanding of its influence on postoperative renal function is urgently needed. Therefore, we aimed to investigate the association between intraoperative 5% albumin use and postoperative AKI in noncardiac surgery.
Results
Patient characteristics
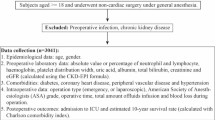
This registry included a total of 203,787 adult patients who underwent noncardiac surgery from January 2011 to June 2019. Of these, we finally identified 39,336 patients after excluding 164,451 patients who met the exclusion criteria (Fig. 1). These patients were divided into two groups accordingF to exposure to 5% albumin during the intraoperative period. There were 37,611 (95.6%) patients in the albumin non-exposure group and 1725 (4.4%) patients in the albumin exposure group in the unmatched population. The median amount of 5% albumin administered during the intraoperative period was 250 mL (IQR 250–500). After PSM, a total of 5221 patients (3697 albumin non-exposure and 1524 albumin exposure) were included in the final analysis. The baseline and perioperative characteristics of the two groups in unmatched and matched populations are presented in Table 1. The balance between the two groups after PSM was satisfactory (ASD < 0.1) for all variables except operation duration.
Intraoperative characteristics of patients before and after PSM are summarized in Table 2. Before matching, albumin exposure group averaged greater estimated blood loss (350 mL vs. 150 mL) and was more frequently administered artificial colloid (42.6% vs. 30.1%) and blood products (28.5% vs. 3.9%). Also, they featured a higher rate of intraoperative hypotension (84.8% vs. 46.3%) and more frequent use of inotropics/vasopressors (66.4% vs. 11.1%). After matching, these variables remained imbalanced (ASD > 0.1) along with infused crystalloid amount and intraoperative temperature, which were incorporated in subsequent logistic regression analyses to adjust for residual intraoperative confounding.
Postoperative AKI and intraoperative albumin use in propensity score-matched cohort
The incidence of postoperative AKI was 3.4% (1285/37,611) in the albumin non-exposure group and 13.0% (225/1725) in the albumin exposure group. In an unmatched analysis, intraoperative albumin exposure was significantly associated with increased risk of postoperative AKI (OR = 4.24; 95% CI, 3.64 − 4.92; p < 0.001). After PSM and adjusting for imbalanced variables, postoperative AKI was still significantly higher in the albumin exposure group (OR = 1.82; 95% CI, 1.41 − 2.34; p < 0.001; Table 3). In subgroup analysis, albumin exposure did not interact with any predefined subgroups except hypertension. The association between albumin exposure and postoperative AKI was more evident in patients without hypertension (OR = 2.38; 95% CI, 1.63 − 3.48; p < 0.001) than in patients with hypertension (OR = 1.49; 95% CI, 1.05 − 2.10; p = 0.03) (Table 4).
Sensitivity analyses
The E value for the association of intraoperative albumin use with postoperative AKI was 3.0, for the estimates 2.2, for the lower confidence limit. In the entire cohort, a multivariable logistic regression analysis showed that intraoperative albumin exposure was independently associated with postoperative AKI (OR = 2.44; 95% CI, 1.97–3.02; p < 0.001). The detailed results of univariable and multivariable logistic regression analyses are presented in Supplemental Tables 1 and 2. This association remained consistent in PSM cohort, where a similar effect size was observed (OR = 2.20; 95% CI, 1.69–2.85; p < 0.001, Supplemental Table 3). Furthermore, in the subgroup of patients with estimated blood loss less than 500 mL, the association between intraoperative albumin administration and AKI persistent after PSM and additional adjustment for residual confounding (OR = 2.40; 95% CI, 1.76–3.28; p < 0.001). Supplemental Table 4 and 5 present the clinical characteristics of patients with estimated blood loss < 500 mL, categorized by albumin exposure status.
Overall survival after propensity score matching
The median (interquartile range) follow-up year was 7.4 (5.3–9.9) years and 4.5 (1.4–6.9) years for the albumin non-exposure and albumin exposure group, respectively. The Kaplan–Meier curve, after propensity score matching, demonstrated that the overall survival was significantly lower in the albumin-exposure group compared to the non-exposure group (p < 0.001 after PSM by log-rank test; Fig. 2).
Discussion
This retrospective study demonstrated that intraoperative 5% albumin use was associated with an increased risk of postoperative AKI and lower overall survival in adult patients undergoing intermediate-high risk noncardiac surgery. We analyzed a large number of patients undergoing various types of noncardiac surgery and attempted to minimize the effects of confounding factors through propensity score matching. We also observed a similar result for postoperative AKI in a multivariable logistic regression analysis in the entire cohort.
Iso-oncotic albumin has been commonly used to maintain intravascular volume effectively in perioperative settings such as hypotension or hypovolemia15. This practice is driven by the concept that albumin has the advantage of rapid resuscitation and longer duration of volume expansion16,17, which therefore may prevent volume overload and its adverse effects. Nevertheless, the largest study to date in cardiac surgery, ALBICS (Albumin in Cardiac Surgery), has shown that the use of 4% albumin did not reduce postoperative major adverse events, including AKI18. Furthermore, recent meta-analysis reported that there is little evidence to support the use of albumin to improve postoperative renal function in major surgery.8 Despite these ongoing debates, unfortunately, its effect on noncardiac surgery has not yet been extensively studied. Hence, albumin continues to be used without clear evidence in noncardiac surgical patients.
Recently, Lazzareschi et al.19 reported that intraoperative albumin administration was associated with an increased risk of postoperative complications, such as AKI, pulmonary complications, and 30-day mortality, in major noncardiac surgery. However, our study differs from the previous research in several key aspects. While the authors evaluated acute AKI as a secondary outcome, our study specifically focuses on AKI as the primary outcome, allowing for a more targeted investigation into the association between intraoperative albumin use and postoperative renal function. Second, Lazzareschi et al. did not exclude patients who may have been exposed to albumin after surgery but prior to the occurrence of AKI, which could introduce temporal ambiguity in the causal relationship. In contrast, our study strictly includes only patients who were administered 5% albumin intraoperatively, ensuring that albumin exposure precedes AKI development. Lastly, their study included both 5% and 25% albumin, which may have introduced variability in the physiological effects and clinical outcomes due to differences in concentration and dosing. In our research, we focused exclusively on 5% albumin to reduce such heterogeneity and provide clearer insights into its specific role during surgery. These methodological differences underscore the strengths of our study design and highlight its contribution to addressing some of the limitations present in prior research.
In this study, we observed a significant association between intraoperative albumin administration and an increased risk of postoperative AKI. While the underlying mechanisms were not investigated in the present study, two primary hypotheses may explain this finding. First, albumin itself may contribute to renal injury through changes in osmotic pressure. By increasing intracapillary oncotic pressure, albumin can reduce the hydrostatic-oncotic pressure gradient, thereby impairing glomerular filtration20. However, given that 5% albumin is less likely to cause osmotic stress than hyperosmotic solutions, this mechanism may only be effective when administered in large doses. While albumin has been thought to possess anti-inflammatory and antioxidative properties that could protect against organ damage, the clinical relevance of these effects remains uncertain. Alternatively, it is possible that the observed association reflects the underlying severity of illness in patients receiving albumin. Patients who were administered albumin during surgery had greater hemodynamic instability and higher comorbidity burden, which were per se associated with higher risk for AKI. Although we attempted to adjust for most of these variables through multivariate logistic regression analysis, further randomized studies are needed to determine whether administration of albumin is truly associated with postoperative AKI in noncardiac surgery.
Postoperative AKI is not only a significant perioperative complication but also a predictor of adverse long-term outcomes, including increased mortality. AKI reflects underlying renal injury and systemic stress, which can initiate a cascade of events leading to chronic kidney disease, cardiovascular complications, and persistent inflammation21. These sequelae may exacerbate vulnerability to long-term organ dysfunction and mortality. Given the strong association between AKI and long-term mortality observed in previous studies22,23, our findings emphasize the importance of strategies aimed at preventing AKI during surgery. These efforts could have a lasting impact on patient outcomes beyond the immediate postoperative period.
This study had several limitations. First, this was a retrospective observational study, so unmeasured or residual confounding factors may be still present. Especially, several intraoperative variables remained imbalanced after PSM and were therefore included as covariates in the logistic regression model. While this additional adjustment aimed to minimize residual confounding, we acknowledge that residual intraoperative confounding may still have persisted. Although the consistency of our findings across multiple sensitivity analyses support robustness of our result, the association between intraoperative albumin use and postoperative AKI should be interpreted with caution. Second, the decision to use albumin was at the discretion of the attending anesthesiologists, so we could not adjust for specific indications for albumin use during propensity score analyses. Our findings need to be confirmed in future studies conducted in well-controlled perioperative settings. Third, the variability in dosing was insufficient to assess a dose–response relationship because most patients received a uniform dose of 250 mL albumin. As such, albumin administration was modeled as a binary exposure. Further research with a wider dose range is needed to determine whether dose-dependent effects exist. Lastly, this was a single-center study, which makes it challenging to generalize the results to other ethnic groups or the patients managed with different strategies. Additional research should validate these findings on intraoperative albumin use and its association with postoperative AKI.
In conclusion, the use of 5% albumin during the intraoperative period was associated with higher risk of postoperative AKI in patients undergoing noncardiac surgery. Our findings do not support the administration of albumin during surgery and may help clinicians choose appropriate types of fluids in noncardiac surgery. Future prospective or randomized clinical studies are required to establish evidence-based guidelines for fluid management in noncardiac surgery.
Methods
Study design and population
This was a retrospective study using data retrieved from the Samsung Medical Center-Non-cardiac operation (SMC-NoCop) registry (registration number KCT0006363, Clinical Research Information Service). This registry included preoperative, intraoperative, and postoperative data of adult patients (≥ 18 years) who underwent noncardiac surgery between January 2011 and June 2019 at Samsung Medical Center, Seoul, Korea. The registry was approved by the institutional review board of Samsung Medical Center (SMC 2021-06-078) and they granted exemption for this study. The institutional review board of Samsung Medical Center waived the requirement for written informed consent because the data were collected in an anonymized form. This study was conducted following the Declaration of Helsinki and was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines24.
From the entire SMC-NoCop registry, this study included the patients who underwent intermediate-high risk noncardiac surgery. The risk of surgery (low, intermediate, and high-risk) was defined according to the non-cardiac surgery guidelines from the European Society of Cardiololgy25. Patients with outpatient surgery, American Society of Anesthesiologists (ASA) physical status ≥ 4, urologic surgery, transplantation surgery, an operation lasting less than two hours, preoperative dialysis, albumin administration only before or after surgery, or missing data related to the covariates used for adjustment were excluded. To limit our subjects to the patients who were administered 5% albumin, patients who were treated with 20% albumin were also excluded26.
Data collection and potential confounders
All data for this study were collected by reviewing electronic medical records with the aid of “Clinical Data Warehouse DARWIN-C” of Samsung Medical Center. This is an electronic data retrieval system that allows investigators to extract medical records in de-identified form from all types of records, laboratory results, and image findings. This system processes 4.4 million patients’ hospital records, 1.3 billion laboratory or image findings, and 400 million prescriptions.
The two authors independently identified the following covariates for propensity score matching (PSM): patient baseline demographics, social and past medical history, preoperative laboratory results, preoperative medications, and surgery-related data. The baseline demographics included age, sex, body mass index, and ASA physical status. Social and past medical history included information about current alcohol consumption, current smoking status, and the presence of hypertension, diabetes mellitus, chronic kidney disease, stroke, coronary artery disease, arrhythmia, liver disease, and chronic obstructive pulmonary disease. Definitions of these comorbidities, along with International Classification of Diseases, 9th and 10th Revision code mappings and search strategies, are summarized in Supplementary Table 6. In addition, the Charlson Comorbidity Index was used to assess the overall severity of comorbidities and general health. Data on preoperative laboratory results included the most recent measurements of hemoglobin, glucose, and creatinine before surgery. Perioperative medication data included the use of β blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, nonsteroidal anti-inflammatory drugs, antiplatelet agents, and statins. Surgery-related data included a year of surgery, type of surgery (abdominal, orthopedic, head & neck surgery, thoracic, and pelvic cavity surgery), emergency surgery, and duration of surgery. Given the variations in intraoperative albumin use year to year, likely reflecting evolving practice patterns and institutional policies, year of surgery was included as a covariate for adjustment.
In addition to preoperative variables, we also collected key intraoperative variables that could influence the development of postoperative AKI. These included intraoperative hypotension (≥ 1 episode of mean arterial pressure < 65 mmHg lasting ≥ 15 min), use of vasoactive or inotropic agents, fluid intake and output variables (crystalloid and colloid volume, estimated blood loss, urine output), blood product transfusion, intraoperative core body temperature, and the use of intraoperative nephrotoxic agents (diuretics or nonsteroidal anti-inflammatory drugs).
Study outcomes and definitions
The primary outcome of this study was the occurrence of AKI within seven days after surgery. AKI was defined according to the Kidney Disease: Improving Global Outcomes (KDIGO) criteria using serum creatinine27. Specifically, AKI was defined as an increase in serum creatinine by at least 0.3 mg/dL within 48 h, or an increase to at least 1.5 times the baseline value within seven days. AKI was further categorized into three stages based on severity. Stage 1 was defined as a mild increase in serum creatinine (0.3 mg/dL or 1.5–1.9 times the baseline value) and stage 2 involved a moderate increase in serum creatinine (2.0–2.9 times the baseline value). Stage 3, the most severe form, was characterized by a significant increase in serum creatinine (≥ 4.0 mg/dL or ≥ 3 times the baseline value) or the initiation of renal replacement therapy. The secondary outcome was overall mortality after surgery. Survival time was calculated from the day of surgery and the final follow-up date was designated as the date of death or the final date of data extraction (September 30, 2023). Mortality data from outside our institution were confirmed from the National Population Registry of the Korea National Statistical Office using an identification number assigned to each patient.
Statistical analysis
Potential confounders were compared between the two groups in both unmatched and propensity score matched cohorts. For descriptive statistics, categorical variables were presented as numbers with percentages and were compared with an χ2 test or Fisher’s exact test. Continuous variables were presented as a median with inter-quartile range (IQR) and were compared with the Mann–Whitney U test.
The 1:3 PSM method was used to balance the potential confounding factors affecting the postoperative outcomes, ensuring the comparability of variables prior to albumin exposure. To estimate the propensity score for albumin exposure, a logistic regression model including all variables listed in Table 1 was used as the predictor. Then, the estimated propensity scores were used to pair exposed individuals with unexposed individuals using the nearest neighboring matching method with calipers of 0.3 standard deviations of propensity score in the logit scale28. Balance between the two groups was assessed before and after matching using absolute standardized differences (ASD), with ASD < 0.10 considered to be well-balanced29.
The variable with ASD ≥ 0.10 after PSM was further adjusted in the outcome model to minimize remaining confounding. In addition, intraoperative variables—which were not included in the initial PSM—were examined separately. Those with residual imbalance (ASD > 0.1) were also incorporated into a post-PSM regression analysis to account for potential intraoperative confounding. The results were presented as an odds ratio (OR) with 95% confidence interval (CI).
To test heterogeneity in treatment effect among patients with different comorbidities, further subgroup analysis was performed using a propensity score matched cohort. The primary outcome was repeatedly analyzed in predefined subgroups, including age (< 65 vs. ≥ 65 years), sex (female vs. male), ASA physical status (< 3 vs. ≥ 3), hypertension (no vs. yes), diabetes mellitus (no vs. yes), and liver disease (no vs. yes).
To assess the robustness of our findings, we conducted the following sensitivity analyses. Frist, to evaluate the influence of unmeasured or unknown confounding factors, we calculated the E value. The E value specifically quantifies the magnitude of association that an unmeasured confounder would need to have with both the exposure and the outcome to nullify the observed effect30. We also reported the E value for the limit of the 95% CI to include the null. Second, we performed multivariable logistic regression analysis of postoperative AKI for the entire cohort to (a) determine whether the findings from the propensity score-matched cohort were valid in the entire cohort, and (b) to assess the independent association between intraoperative albumin use and postoperative AKI while controlling other significant covariates that were not adjusted in PSM. All variables listed in Table 1 and Table 2 were included in the multivariable logistic regression model. We confirmed the absence of multicollinearity among the variables by ensuring all variance inflation factor values were < 5. Third, to assess the reproducibility of our primary findings, we applied multivariable logistic regression again within the matched cohort. Finally, to address potential confounding by indication—specifically that albumin may have been administered in response to massive bleeding—we performed a subgroup analysis of patients with estimated blood loss < 500 mL. In this subset, we repeated the primary analysis to determine whether the association between albumin use and postoperative AKI persisted even when the decision to administer albumin was less likely to be influenced by hemorrhage.
Finally, to compare overall mortality between the two groups as time-to-event outcomes, we constructed survival curves with the Kaplan–Meier method and tested statistical significance using log-rank test. All statistical analysis was performed in R 4.2.0 (Vienna, Austria; http://www.R-project.org/) and considered statistically significant when the p-value was less than 0.05.
Data availability
All data related to the present research are available from the corresponding author upon reasonable request.
References
O’Connor, M. E., Kirwan, C. J., Pearse, R. M. & Prowle, J. R. Incidence and associations of acute kidney injury after major abdominal surgery. Intensive Care Med. 42, 521–530. https://doi.org/10.1007/s00134-015-4157-7 (2016).
Vaught, A. J. et al. Acute kidney injury in major gynaecological surgery: An observational study. BJOG 122, 1340–1348. https://doi.org/10.1111/1471-0528.13026 (2015).
O’Connor, M. E. et al. Acute kidney injury and mortality 1 year after major non-cardiac surgery. Br. J. Surg. 104, 868–876. https://doi.org/10.1002/bjs.10498 (2017).
Basile, D. P., Anderson, M. D. & Sutton, T. A. Pathophysiology of acute kidney injury. Compr. Physiol. 2, 1303–1353. https://doi.org/10.1002/cphy.c110041 (2012).
Gaut, J. P. & Liapis, H. Acute kidney injury pathology and pathophysiology: A retrospective review. Clin. Kidney J. 14, 526–536. https://doi.org/10.1093/ckj/sfaa142 (2021).
Gupta, R. & Gan, T. J. Peri-operative fluid management to enhance recovery. Anaesthesia 71(Suppl 1), 40–45. https://doi.org/10.1111/anae.13309 (2016).
Raghunathan, K. et al. Choice of fluid in acute illness: What should be given? An international consensus. Br. J. Anaesth. 113, 772–783. https://doi.org/10.1093/bja/aeu301 (2014).
Lee, K. S., Kim, J. E., Kang, G., Won, Y. J. & Choi, Y. J. The effect of human albumin administration on postoperative renal function following major surgery: A systematic review and meta-analysis. Sci. Rep. 14, 16599. https://doi.org/10.1038/s41598-024-62495-0 (2024).
Tseng, C. H. et al. Resuscitation fluid types in sepsis, surgical, and trauma patients: A systematic review and sequential network meta-analyses. Crit. Care 24, 693. https://doi.org/10.1186/s13054-020-03419-y (2020).
Lewis, S. R. et al. Colloids versus crystalloids for fluid resuscitation in critically ill people. Cochrane Database Syst. Rev. 8, CD000567. https://doi.org/10.1002/14651858.CD000567.pub7 (2018).
Ferrer, R. et al. Non-oncotic properties of albumin. A multidisciplinary vision about the implications for critically ill patients. Expert Rev. Clin. Pharmacol. 11, 125–137. https://doi.org/10.1080/17512433.2018.1412827 (2018).
Arques, S. Human serum albumin in cardiovascular diseases. Eur. J. Intern. Med. 52, 8–12. https://doi.org/10.1016/j.ejim.2018.04.014 (2018).
Belinskaia, D. A., Voronina, P. A., Shmurak, V. I., Jenkins, R. O. & Goncharov, N. V. Serum albumin in health and disease: Esterase, antioxidant, transporting and signaling properties. Int. J. Mol. Sci. 22, 10318. https://doi.org/10.3390/ijms221910318 (2021).
Aldecoa, C., Llau, J. V., Nuvials, X. & Artigas, A. Role of albumin in the preservation of endothelial glycocalyx integrity and the microcirculation: A review. Ann. Intensive Care 10, 85. https://doi.org/10.1186/s13613-020-00697-1 (2020).
Raynor, B., Huang, A., Udrea, D. & Montano, N. The role of albumin in the resuscitation of hypotensive patients. Curr. Emerg. Hosp. Med. Rep. 11, 89–94. https://doi.org/10.1007/s40138-023-00268-1 (2023).
Hahn, R. G., Zdolsek, M., Hasselgren, E., Zdolsek, J. & Bjorne, H. Fluid volume kinetics of 20% albumin. Br. J. Clin. Pharmacol. 85, 1303–1311. https://doi.org/10.1111/bcp.13897 (2019).
Hasselgren, E. et al. Long intravascular persistence of 20% albumin in postoperative patients. Anesth. Analg. 129, 1232–1239. https://doi.org/10.1213/ANE.0000000000004047 (2019).
Pesonen, E. et al. Effect of 4% albumin solution vs ringer acetate on major adverse events in patients undergoing cardiac surgery with cardiopulmonary bypass: A randomized clinical trial. JAMA 328, 251–258. https://doi.org/10.1001/jama.2022.10461 (2022).
Lazzareschi, D. V. et al. Intraoperative use of albumin in major noncardiac surgery: Incidence, Variability, and association with outcomes. Ann. Surg. 278, e745–e753. https://doi.org/10.1097/SLA.0000000000005774 (2023).
Moran, M. & Kapsner, C. Acute renal failure associated with elevated plasma oncotic pressure. N. Engl. J. Med. 317, 150–153. https://doi.org/10.1056/NEJM198707163170306 (1987).
Ikizler, T. A. et al. A prospective cohort study of acute kidney injury and kidney outcomes, cardiovascular events, and death. Kidney Int. 99, 456–465. https://doi.org/10.1016/j.kint.2020.06.032 (2021).
Lafrance, J. P. & Miller, D. R. Acute kidney injury associates with increased long-term mortality. J. Am. Soc. Nephrol. 21, 345–352. https://doi.org/10.1681/ASN.2009060636 (2010).
Bihorac, A. et al. Long-term risk of mortality and acute kidney injury during hospitalization after major surgery. Ann. Surg. 249, 851–858. https://doi.org/10.1097/SLA.0b013e3181a40a0b (2009).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 370, 1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X (2007).
Halvorsen, S. et al. 2022 ESC guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. Eur. Heart J. 43, 3826–3924. https://doi.org/10.1093/eurheartj/ehac270 (2022).
Ryhammer, P. K. et al. Colloids in cardiac surgery-friend or foe?. J. Cardiothorac. Vasc. Anesth. 31, 1639–1648. https://doi.org/10.1053/j.jvca.2017.02.001 (2017).
Kellum, J. A. et al. Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. https://doi.org/10.1038/kisup.2012.1 (2012).
Austin, P. C. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm. Stat. 10, 150–161. https://doi.org/10.1002/pst.433 (2011).
Zhang, Z., Kim, H. J., Lonjon, G., Zhu, Y. & written on behalf of, A. M. E. B.-D. C. T. C. G. Balance diagnostics after propensity score matching. Ann. Transl. Med. 7, 16 (2019). https://doi.org/10.21037/atm.2018.12.10.
VanderWeele, T. J. & Ding, P. Sensitivity analysis in observational research: Introducing the E-value. Ann. Intern. Med. 167, 268–274. https://doi.org/10.7326/M16-2607 (2017).
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization and design of study: ARO, JP Data extraction and analysis plan design: ARO, SL Data interpretation: all authors Drafting of article: ARO, JP.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Oh, A.R., Park, J. & Lee, S. Intraoperative albumin use and postoperative acute kidney injury in patients undergoing noncardiac surgery. Sci Rep 15, 41842 (2025). https://doi.org/10.1038/s41598-025-25750-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-25750-6