Abstract
Invasive candidiasis (IC) remains an infection with high incidence and mortality rates in the ICU setting, particularly among patients treated with broad-spectrum antibiotics. This study aims to investigate the association between detailed antibiotic usage profiles and the occurrence of IC, and to develop an IC-predictive model specialized for patients who received broad-spectrum antibiotics. We retrospectively collected detailed information on antibiotic categories, treatment duration, combination therapies and other clinical data of enrolled patients. Univariate and multivariate logistic regression analyses were performed to identify risk factors for IC and to construct a nomogram model. We analyzed 1,260 patients treated with broad-spectrum antibiotics and 877 without. After adjusting for IC-related risk factors using propensity score matching (PSM) and inverse probability of treatment weighting (IPTW), broad-spectrum antibiotics remained an independent risk factor for IC. Among patients receiving antibiotic monotherapy, lipopeptides, glycopeptides and oxazolidinones were the top three antibiotic classes associated with an increased risk of IC. The duration of antibiotic therapy showed a positive correlation with IC risk. Combination therapy significantly increased the risk of IC (odds ratio [OR] = 2.341, 95% confidence interval [CI]: 1.316–4.162), with the combination of beta-lactams/beta-lactamase inhibitors and glycopeptides showing the highest IC risk. Based on univariate and multivariate regression analyses, we developed an IC risk nomogram specific to patients receiving broad-spectrum antibiotics, including smoking history, sepsis, continuous renal replacement therapy (CRRT), prognostic nutritional index (PNI), use of beta-lactams/beta-lactamase inhibitors and plasma (1,3)-β-D-glucan (BDG) positivity. The model demonstrated good predictive performance with an area under the curve (AUC) of 0.863 (95% CI: 0.806–0.920) in the training dataset and 0.784 (95% CI: 0.685–0.883) in the validation dataset. Decision curve analysis (DCA) and clinical impact curve (CIC) analysis demonstrated favorable clinical benefits of the model. Our findings suggest that specific antibiotic profiles—type, duration, and combination—were significantly associated with IC. Furthermore, we developed a nomogram to predict IC risk among patients treated with broad-spectrum antibiotics, which showed good predictive performance and potential clinical utility.
Similar content being viewed by others
Introduction
Invasive candidiasis (IC) is the most common invasive fungal infection among critically ill patients, with a high mortality rate ranging from 40 to 71%1,2. Over the past decades, the incidence of IC has continued to rise sharply, especially in the intensive care unit (ICU)3,4. This increase is likely attributable to the growing use of complex medical interventions and pharmacologic agents in the ICU, among which broad-spectrum antibiotics represent a prominent risk factor for IC5,6. Notably, the utilization of broad-spectrum antibiotics is highly prevalent in ICU settings, with approximately 71% of patients receiving antimicrobial therapy—90% of which involves antibiotics7,8. Timely initiation of empirical antifungal therapy is crucial for reducing IC-related mortality9. However, administering empirical antifungal treatment to all high-risk IC patients receiving broad-spectrum antibiotics is not feasible due to concerns regarding drug toxicity, high costs, and the potential for promoting antifungal resistance10. There is still a lack of strong evidence to guide the diagnosis and treatment of IC for ICU patients receiving broad-spectrum antibiotics.
Broad-spectrum antibiotics can promote translocation of intestinal microbiota and impair the function or proliferation of intestinal lymphocytes, thereby increasing susceptibility to Candida infections11. Previous studies have identified broad-spectrum antibiotic use as a risk factor for IC, but most have treated antibiotic exposure as a single entity. Limited evidence is available regarding the association between specific antibiotic types, durations, and combination patterns and the risk of IC. Besides, although broad-spectrum antibiotics and other risk factors have been well recognized, early identification of IC patients remains a critical challenge necessitating immediate solutions. Given that delayed antifungal therapy can further increase the mortality rate of ICU-associated IC, recent studies have explored various non-culture diagnostic methods to improve diagnostic efficiency, including (1,3)-β-D-glucan (BDG), Candida albicans germ tube antibody, PCR-based fungal DNA detection, and T2 magnetic resonance analysis12,13. Nonetheless, these methods exhibit varying sensitivities and possess distinct limitations14,15. Therefore, there is an urgent need for an improved, simple, and accurate diagnostic model to enable early identification of IC and timely initiation of antifungal therapy.
Candida spp. can infiltrate sterile tissue and proliferate uncontrollably and then be sensed by individual and/or synergistic pattern recognition receptors, triggering an inflammatory cascade reaction and initiating the release of pro-inflammatory cytokines and chemokines16. Previous studies have confirmed that patients with IC exhibit elevated levels of various inflammatory cytokines, along with poor nutritional status17,18,19. In this research, we incorporated several novel serological markers, including the NLR (Neutrophil-to-Lymphocyte Ratio), MLR (Monocyte-to-Lymphocyte Ratio), PLR (Platelet-to-Lymphocyte Ratio), CAR (C-Reactive Protein-to-Albumin Ratio), SII (Systemic Inflammation Index), and PNI (Prognostic Nutrition Index)—all of which are representative indicators of systemic inflammation and nutrition. These biomarkers have been shown to serve as indicators in a variety of diseases20,21. However, their potential as markers for IC remains to be further investigated. In this retrospective study, we focus on the association between detailed antibiotic usage profiles and IC by analyzing data on antibiotic categories, duration of use, and combination therapy regimens in critically ill patients; simultaneously, we aim to promote the early and accurate identification of IC in ICU patients receiving broad-spectrum antibiotics and to enable the timely initiation of antifungal therapy by developing a predictive model that incorporates population-specific clinical characteristics, patterns of antibiotic use, non-specific diagnostic tools, and novel serological biomarkers.
Methods
Study population
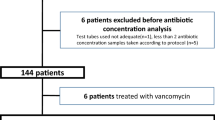
In this retrospective study, we included patients hospitalized in the ICU at Xiangya Hospital of Central South University between January 2018 and December 2022. The inclusion criteria were as follows: (1) age ≥ 18 years; (2) severe illness requiring intensive care. Patients were excluded if they met any of the following criteria: (1) ICU stay < 48 h, (2) presence of a non-Candida fungal infection at admission, (3) incomplete medical records, (4) pregnancy, (5) undocumented or unclear medical history. A total of 2137 patients were included in this study, and the inclusion process is detailed in the flowchart shown in Fig. 1.
Data collection
Baseline clinical characteristics and laboratory data were independently extracted from the electronic medical record system by a team of experienced physicians. Demographic and clinical information at ICU admission included sex, age, smoking history, comorbidities, vital signs, Sequential Organ Failure Assessment (SOFA) score and laboratory testing results on admission. Laboratory tests comprised complete blood counts, routine chemistry, C-reactive protein (CRP) and blood BDG, all of which were completed within 24 h of ICU admission. Additional IC-related risk factors were also recorded, including the use of broad-spectrum antibiotics, continuous renal replacement therapy (CRRT), total parenteral nutrition (TPN), mechanical ventilation and indwelling catheters (central venous catheter [CVC], extracorporeal membrane oxygenation [ECMO], urinary catheter, invasive mechanical ventilation [IMV]), and receipt of a high dose of corticosteroids. To further investigate the relationship between antibiotic usage patterns and IC, we collected information about specific antibiotic categories, duration of use, and combination regimens. The primary outcome of this study was the incidence of IC, secondary outcomes included 30-day mortality after ICU admission, total length of hospital stay, length of ICU stay, and hospitalization costs. Patients with incomplete medical records, defined as missing one or more essential elements (ICU admission/discharge dates, outcome status and date, microbiological confirmation, systemic antibiotic exposure, or core covariates such as age, sex, major comorbidities and severity scores), were excluded after repeated retrieval attempts.
Diagnosis of IC
IC was diagnosed by experienced respiratory physicians. Specifically, patients exhibited clinical manifestations consistent with IC and met at least one of the standard diagnostic criteria outlined by the European Organization for Research and Treatment of Cancer/Mycoses Study Group Education and Research Consortium (EORTC/MSGERC): (1) Candida detected in normal sterile tissues by pathological or microscopic examinations; (2) Candida detected in sterile fluid specimen such as pleural effusion; (3) Candida detected in blood22.
Definition of specific exposure
Broad-spectrum antibiotics were defined as agents with activity against methicillin-resistant Staphylococcus aureus (MRSA), such as linezolid or vancomycin, or against Pseudomonas aeruginosa, such as fourth-generation cephalosporins or fluoroquinolones (Table S1)23,24,25, and only parenteral/systemic formulations were considered. Antibiotic combination therapy was defined as the concurrent use of two or more antibiotics from different antimicrobial classes for a duration exceeding 48 hours26,27. A history of corticosteroid use was defined as administration of prednisone at a dose ≥ 20 mg/kg/day for at least 72 consecutive hours28.
Statistical analysis
Continuous variables were presented as mean ± standard deviation or median and interquartile range (IQR), and differences between groups were compared using the Student’s t-test or Mann–Whitney U test. Categorical variables were presented as frequencies and percentages, and group differences were assessed using the chi-square test or Fisher’s exact test. We employed 1:1 propensity score matching (PSM) and inverse probability of treatment weighting (IPTW) to minimize the influence of potential confounding factors and to further validate the association between broad-spectrum antibiotic use and IC. Patients treated with broad-spectrum antibiotics were randomly assigned to a training cohort (70%) and a validation cohort (30%). Continuous variables potentially associated with IC risk were converted into categorical variables using optimal cut-off values determined by receiver operating characteristic (ROC) analysis. Univariate logistic regression was performed to identify potential risk factors for IC in the training cohort. Variables with a P value < 0.05 in univariate analysis were entered into a multivariate logistic regression using stepwise forward selection to determine independent predictors. Antibiotic classes with very small exposure or event counts were not included in regression modeling to avoid sparse-data bias and were instead summarized descriptively. The regression coefficients (β) of these independent predictors from the final multivariable model were then used to construct a nomogram, which provides a visual representation of the predictive model by assigning a weighted score to each predictor. The total score calculated from the nomogram corresponds to the predicted probability of IC for individual patients. The discriminatory ability of the nomogram was evaluated using the area under the ROC curve (AUC), and its calibration and clinical utility were further assessed through calibration plots, decision curve analysis (DCA) and clinical impact curve (CIC) analysis. The Hosmer-Lemeshow test was also performed to evaluate goodness-of-fit, with a P value > 0.05 indicating good model fitness. These evaluation methods were also applied to assess the model in the validation cohort. All statistical analyses were conducted using SPSS version 26.0 (SPSS, Chicago, IL, USA) and R Statistical Software version 4.1.3 (R Foundation for Statistical Computing, Vienna, Austria), considering P < 0.05 as statistically significant.
Results
Baseline characteristics of included participants
This study included 1,260 patients who received broad-spectrum antibiotics and 877 patients who did not. ICU patients receiving broad-spectrum antibiotics were more likely to be male, had a higher prevalence of chronic renal disease, pulmonary tuberculosis, and sepsis, and were more likely to undergo various invasive treatments such as IMV, CRRT and CVC (Table 1). Among patients receiving broad-spectrum antibiotics, those who developed IC had significantly longer ICU stays (11.5 vs. 8.0 days, P < 0.001), longer total hospital stays (15.0 vs. 12.0 days, P = 0.010), and higher hospitalization costs (141714.71 vs. 78269.22 CNY, P < 0.001). However, no significant difference in 30-day mortality was observed between the two groups (24.39% vs. 17.66%, P = 0.126) (Table 2).
Correlation between specific antibiotic profiles with the onset of IC
The incidence of IC in broad-spectrum antibiotics group was significantly higher than that in the non-broad-spectrum antibiotics group (6.51% vs. 1.71%, P < 0.001). After applying 1:1 PSM, stable IPTW and unstable IPTW, three datasets were derived from the original data (Table 1; Table S2). Across all datasets, univariate logistic regression consistently identified broad-spectrum antibiotic use as a significant risk factor for IC, with odds ratios (ORs) ranging from 1.021 to 1.048 (P < 0.05) (Fig. 2).
(A) Comparison of IC incidence between broad-spectrum antibiotics and non-broad spectrum antibiotics groups. (B) Forest plot of the association between use of broad-spectrum antibiotics with IC in different scoring matching conditions. Abbreviations: PSM, propensity score match; IPTW, inverse probability of treatment weighting; OR, odds ratio; CI: confidence interval; IC, invasive candidiasis.
We further explored the relationship between antibiotic categories, treatment duration, combination regimens and the incidence of IC. Patients were stratified into four groups based on the duration of broad-spectrum antibiotics administration: < 7 days, 7–14 days, 14–28 days, and more than 28 days. The corresponding IC incidence rates were 3.54%, 6.15%, 10.04%, and 15.00%, respectively, indicating a positive correlation between prolonged antibiotic exposure and IC onset (Fig. 3). Among antibiotic monotherapy regimens, beta-lactams/beta-lactamase inhibitors were the most commonly prescribed, followed by carbapenems and oxazolidinones. The incidence of IC under different monotherapies was highest with lipopeptides (16.67%), followed by glycopeptides (13.19%), oxazolidinones (10.25%), aminoglycosides (9.43%), carbapenems (7.83%), cephalosporins (7.41%), fluoroquinolones (7.25%), and beta-lactams/beta-lactamase inhibitors (6.84%) (Fig. 4A; Table S3). Regarding combination therapies, the most frequently used dual-antibiotic regimen was beta-lactams/beta-lactamase inhibitors plus oxazolidinones. The incidence of IC varied among patients receiving different antibiotic combinations. Among dual-antibiotic combination groups with more than 10 patients, the combination of beta-lactams/beta-lactamase inhibitors with glycopeptides was associated with the highest IC incidence (18.67%, 14/75), followed by the combination with aminoglycosides (11.76%, 2/17) (Fig. 4B; Table S4).
Development of the nomogram in the broad-spectrum antibiotic group
We randomly divided patients treated with broad-spectrum antibiotics into the training dataset and the validation dataset at a ratio of 7:3, with no significant differences in baseline characteristics between the two datasets (Table S5). Continuous variables were dichotomized based on cut-off values determined by the optimal Youden index from ROC analysis. In the training set, univariate logistic regression was performed to identify potential risk factors for IC. Notably, the number of patients receiving lipopeptides was small (n = 12) with 2 IC events (16.7%); therefore, this category was analyzed descriptively and not entered into regression models to avoid sparse-data bias. Nineteen variables with P < 0.05 derived from univariate analysis were included in multivariate forward stepwise logistic regression analysis, including sex, smoking history, sepsis, IMV, CRRT, TPN, ECMO, urinary catheter, CVC, SOFA score (≥ 4.5), PNI (< 272.25), CAR (≥ 3.13), plasma BDG positivity, duration of beta-lactams/beta-lactamase inhibitors (≥ 10.5 days), carbapenems (≥ 5.5 days), glycopeptides (≥ 2.5 days), oxazolidinones (≥ 4.5 days), total antibiotic duration ≥ 11 days, dual or multi-drug combinations (Table 3). Multivariate logistic regression analysis identified six independent risk factors for IC: smoking history, sepsis, CRRT, PNI (< 272.25), duration of beta-lactams/beta-lactamase inhibitors (≥ 10.5 days), and plasma BDG positivity (Table 4). A nomogram was constructed based on the six independent predictors to estimate the probability of IC occurrence in patients receiving broad-spectrum antibiotics. Each predictor was assigned a weighted point proportional to its regression coefficient (β) in the final model. The cumulative points of all predictors correspond to an individual patient’s total points, which were then mapped to the predicted probability of developing IC using a probability scale embedded within the nomogram. (Fig. 5).
Nomogram model for predicting the risk of IC in patients receiving broad-spectrum antibiotics. Each variable corresponds to a point, and the total points are obtained by summing the points of the six variables. The probability corresponding to the total points represents the predicted risk of IC in the patient. Abbreviations: CRRT, continuous renal replacement therapy; PNI, prognostic nutritional index; BDG, (1,3)-β-D-glucan; IC, invasive candidiasis.
Validation of the predictive nomogram
The ROC curves indicated that the model presented superior predictive performance with an AUC of 0.863 in the training cohort and 0.784 in the validation cohort—both higher than that of the Candida score. The calibration curve showed excellent agreement between predicted probabilities and observed outcomes, and the Hosmer-Lemeshow test ( P > 0.05) confirmed the good fitness of the nomogram, further validating its reliability in predicting the risk of IC (Fig. 6). The results of DCA demonstrated that the nomogram provided superior clinical benefit compared to strategies of treating all or no patients. Moreover, CIC analysis showed that the predicted IC risk closely matched actual outcomes when the predicted probability exceeded 0.3 in the training dataset and 0.4 in the validation dataset (Fig. 7). Overall, the nomogram exhibited favorable predictive performance and clinical utility for identifying patients at high risk of invasive candidiasis.
(A–B) The comparisons of receiver operating characteristic curves between Nomogram model and Candida score in (A) the training dataset and (B) the validation dataset. (C–D) The calibration curves of the nomogram model in (C) the training dataset and (D) the validation dataset. Abbreviations: AUC, areas under receiver operating characteristic curves; CI, confidence interval.
Discussion
In this study, we first characterized the association between specific broad-spectrum antibiotic usage patterns and the incidence of IC. Our findings revealed that lipopeptides, glycopeptides, and oxazolidinones were the top three antibiotic classes most strongly associated with IC. Moreover, the incidence of IC increased progressively with the duration of antibiotic exposure. Among dual-antibiotic regimens administered to more than 10 patients, the combination of beta-lactams/beta-lactamase inhibitors and glycopeptides posed the highest risk. Based on a population of critically ill patients receiving broad-spectrum antibiotics, we developed an early predictive model for IC that integrated clinical characteristics (smoking history, sepsis, and CRRT), novel serological biomarkers (PNI < 272.25), antibiotic exposure duration (beta-lactams/beta-lactamase inhibitors ≥ 10.5 days), and a non-culture diagnostic biomarker (plasma BDG positivity). This nomogram demonstrated robust predictive accuracy and promising clinical utility.
Our findings suggest that broad-spectrum antibiotics represent a prevalent clinical risk factor for IC. After employing multiple propensity score methods to balance other risk factors for IC, we found that broad-spectrum antibiotic use remained significantly associated with increased IC incidence. Previous studies have found that broad-spectrum antibiotics can promote Candida overgrowth and colonization in the gastrointestinal tract, compromise mucosal barrier integrity, and deplete host phagocytes, thereby facilitating Candida translocation into the bloodstream29,30. Additionally, the gut microbiota can enhance the production of IL-17 A to counteract Candida invasion, but broad-spectrum antibiotics can disrupt this protective effect by causing dysbiosis of gut microbiota31. Despite these mechanistic insights, most existing studies have assessed antibiotics as a uniform category, without distinguishing between specific classes or treatment regimens. The risk of IC likely varies among antibiotic types due to differing antimicrobial spectra and immunomodulatory effects. In our study, we analyzed IC incidence by antibiotic class and observed the following proportions: lipopeptides (16.67%, 2/12), glycopeptides (13.19%, 24/182), oxazolidinones (10.25%, 41/400), aminoglycosides (9.43%, 5/53), carbapenems (7.83%, 61/779), cephalosporins (7.41%, 6/81), fluoroquinolones (7.25%, 25/345), and beta-lactams/beta-lactamase inhibitors (6.84%, 62/906). These findings indicate that different antibiotic classes carry differential risks of IC. A more nuanced understanding of these associations may aid clinicians in selecting antimicrobial therapies that balance efficacy against bacterial infections while minimizing the risk of fungal complications.
In addition to the type of broad-spectrum antibiotics used, we also identified a positive association between the duration of broad-spectrum antibiotic use and the risk of IC. Specifically, the incidence of IC was 3.54% among patients who received antibiotics for less than 7 days, but increased to 15.00% when the duration exceeded 28 days, underscoring the importance of antibiotic stewardship in terms of treatment duration. Notably, it is estimated that nearly 50% of antibiotic prescriptions worldwide are unnecessary32, and clinicians are often reluctant to discontinue antibiotic therapy prematurely. Several randomized clinical trials have shown that shortened courses of antimicrobial therapy are non-inferior to standard durations in terms of clinical outcomes, while also reducing adverse events33,34,35,36. However, there is currently no universally accepted guideline on how to determine the optimal duration of antibiotic therapy. Some advocate for developing novel technologies to improve the speed of microbial diagnostics37, while others propose tailoring antibiotic duration based on dynamic changes in biomarkers such as CRP and procalcitonin38. Furthermore, combination antibiotic therapy also appears to be a significant risk factor for IC. In our study, among combinations used by more than 10 individuals, the combination of beta-lactams/beta-lactamase inhibitors with glycopeptides presented the highest risk for IC (14/75, 18.67%). Researchers found that MRSA strains highly resistant to vancomycin were extremely sensitive to beta-lactam antibiotics, indicating a synergistic antimicrobial effect of the combination of beta-lactams with glycopeptides39. Beta-lactams and glycopeptides both exert their antimicrobial effects by inhibiting bacterial cell wall synthesis through targeting peptidoglycan. However, some studies have indicated that beta-lactams can induce a “peptidoglycan storm” by releasing substantial amounts of bacterial peptidoglycan, promoting the growth of Candida albicans hyphae in mouse intestines, thus leading to IC40. Glycopeptides may potentiate this effect through complementary mechanisms, collectively exacerbating fungal overgrowth and translocation. These findings highlight the need for heightened caution when administering this antibiotic combination, particularly in critically ill patients with known risk factors for fungal infections. However, given the influence of antibiotic usage frequency in our cohort and the likelihood of prescription bias—since such combinations are often used in the sickest ICU patients—these results should be interpreted with caution and validated in larger multicenter studies.
Early diagnosis of IC remains a clinical challenge, as each diagnostic modality presents inherent limitations. As a result, increasing attention has been directed toward integrating patient-specific clinical characteristics into diagnostic and predictive models. In the present study, we developed an IC prediction model tailored to a high-risk population receiving broad-spectrum antibiotics, incorporating clinical features, antibiotic usage patterns, and microbiological results. The patient-related factors included in the model were smoking history, sepsis, and continuous renal replacement therapy (CRRT). Both sepsis and CRRT are well-established risk factors for IC41. The association between smoking and IC has been less frequently investigated, but it was identified as a significant risk factor for IC in this cohort. Previous research has shown that smoking significantly increases the risk of oral candidiasis, which, in immunocompromised individuals, may disseminate hematogenously or through the upper gastrointestinal tract, leading to invasive disease42. Our study focused on critically ill patients in the ICU, with a significant number exhibiting impaired immune status, potentially explaining the phenomenon of smoking as a risk factor for IC.
Beyond individual and clinical characteristics, novel serological biomarker—PNI was also incorporated into the predictive model. Persistent systemic inflammation and malnutrition are common among ICU patients and are known to increase susceptibility to fungal invasion. Several studies have shown that malnutrition is independently associated with the prognosis of IC patients18,43, and indices such as the Geriatric Nutritional Risk Index have been shown to predict IC risk in elderly populations44. We also incorporated plasma BDG test, a commonly used fungal biomarker based on the detection of fungal cell wall components. Meta-analyses have reported a pooled sensitivity of 75–80% and specificity of approximately 80% for BDG in diagnosing IC45. However, BDG testing is known to be susceptible to false-positive results due to factors such as hemodialysis, filtration therapies, enteral nutrition, and certain Gram-positive bacterial infections, thereby limiting its reliability when used as the sole diagnostic marker for IC46. Importantly, recent studies suggest that BDG often becomes positive before culture-confirmed candidemia and that serial monitoring improves clinical utility compared with single measurements47,48. Accordingly, BDG should be interpreted in context and preferably used as a dynamic adjunct rather than a stand-alone diagnostic. Our predictive model integrates multiple host-specific risk factors to improve diagnostic accuracy and clinical relevance rather than relying on any single indicator. The variables included in the nomogram are readily available in routine clinical practice and easily accessible at the bedside, which makes it particularly suitable for application in resource-limited healthcare settings, including primary and community hospitals.
This study has several limitations. First, it is a single-center retrospective analysis with a relatively limited sample size, particularly for certain antibiotic combination regimens with few participants. Second, the nomogram was only validated internally; although calibration and decision-curve performance were favorable, the lack of external validation limits its generalizability and necessitates testing in multicenter cohorts. Third, species-level identification of Candida was inconsistently available in the medical records, preventing further species-stratified analyses. Fourth, dichotomizing several continuous variables using ROC-derived thresholds from limited events improved clinical usability but may have reduced information and precision. Fifth, because the baseline incidence of invasive candidiasis is low, the model’s positive predictive value is inherently constrained; therefore, clinical utility depends on carefully selected probability thresholds and use alongside other diagnostics rather than as a stand-alone trigger.
Conclusion
In this study, we identified that specific antibiotic usage patterns—including antibiotic class, duration, and combination regimens—were significantly associated with the risk of IC. Furthermore, we developed a nomogram to predict IC risk in a high-risk population receiving broad-spectrum antibiotics. The final model incorporated six key variables: smoking history, sepsis, CRRT, low PNI (< 272.25), prolonged use of beta-lactams/beta-lactamase inhibitors (≥ 10.5 days), and plasma BDG positivity, which exhibited strong predictive performance and favorable clinical utility.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author (Pinhua Pan, Phone: +86-0731-89753287, E-mail: pinhuapan668@csu.edu.cn) on reasonable request.
References
Alenazy, H., Alghamdi, A., Pinto, R. & Daneman, N. Candida colonization as a predictor of invasive candidiasis in non-neutropenic ICU patients with sepsis: A systematic review and meta-analysis. Int. J. Infect. Dis. 102, 357 (2021).
O’Leary, R. A. et al. Management of invasive candidiasis and candidaemia in critically ill adults: Expert opinion of the European Society of Anaesthesia Intensive Care Scientific Subcommittee. J Hosp Infect 98, 382 (2018).
Baldesi, O. et al. ICU-acquired candidaemia in France: Epidemiology and temporal trends, 2004–2013—a study from the REA-RAISIN network. J. Infect. 75, 59 (2017).
Schroeder, J. A., Wilson, C. M. & Pappas, P. G. Invasive candidiasis. Infect. Dis. Clin. N. Am. 39, 93 (2025).
Wang, Y. et al. ICU patients’ antibiotic exposure and triazole-resistance in invasive candidiasis: parallel analysis of aggregated and individual data. Front. Pharmacol. 12, 586893 (2021).
Vazquez, J. A., Whitaker, L. & Zubovskaia, A. Invasive candidiasis in the intensive care unit: Where are we now?. J. Fungi (Basel, Switzerland) 11, 258 (2025).
Kollef, M. H. et al. Timing of antibiotic therapy in the ICU. Crit Care 25, 360 (2021).
Ronda, M. et al. Long-term effects of a stepwise, multimodal, non-restrictive antimicrobial stewardship programme for reducing broad-spectrum antibiotic use in the ICU. Antibiotics-Basel 13, 132 (2024).
Grim, S. A. et al. Timing of susceptibility-based antifungal drug administration in patients with Candida bloodstream infection: correlation with outcomes. J. Antimicrob. Chemother. 67, 707 (2012).
White, S. K., Schmidt, R. L., Walker, B. S. & Hanson, K. E. (1–>3)-beta-D-glucan testing for the detection of invasive fungal infections in immunocompromised or critically ill people. Cochrane Database Syst. Rev. 7, CD009833 (2020).
Drummond, R. A. et al. Long-term antibiotic exposure promotes mortality after systemic fungal infection by driving lymphocyte dysfunction and systemic escape of commensal bacteria. Cell Host Microbe 30, 1020 (2022).
Zhang, J. et al. Prospective evaluation of lymphocyte subtyping for the diagnosis of invasive candidiasis in non-neutropenic critically ill patients. Int. J. Infect. Dis. 78, 140 (2019).
Cornely, O. A. et al. Global guideline for the diagnosis and management of candidiasis: An initiative of the ECMM in cooperation with ISHAM and ASM. Lancet Infect. Dis 25, e280 (2025).
Bloos, F. et al. (1 –> 3)-beta-D-Glucan-guided antifungal therapy in adults with sepsis: the CandiSep randomized clinical trial. Intens. Care Med. 48, 865 (2022).
Martin-Mazuelos, E. et al. beta-D-Glucan and Candida albicans germ tube antibody in ICU patients with invasive candidiasis. Intens. Care Med. 41, 1424 (2015).
Pappas, P. G., Lionakis, M. S., Arendrup, M. C., Ostrosky-Zeichner, L. & Kullberg, B. J. Invasive candidiasis. Nat. Rev. Dis. Prim. 4, 18026 (2018).
Chumpitazi, B. F. F. et al. Characteristic and clinical relevance of Candida mannan test in the diagnosis of probable invasive candidiasis. Med. Mycol. 52, 462 (2014).
Lee, Y. et al. Impact of nutritional assessment on the clinical outcomes of patients with non-Albicans candidemia: A multicenter study. Nutrients 13, 3218 (2021).
Wunsch, S. et al. Longitudinal evaluation of plasma cytokine levels in patients with invasive Candidiasis. J. Fungi (Basel, Switzerland) 7, 101 (2021).
Mousa, N. et al. Can combined blood neutrophil to lymphocyte ratio and C-reactive protein be used for diagnosis of spontaneous bacterial peritonitis?. Br. J. Biomed. Sci. 75, 71 (2018).
Xue, G. et al. Novel serological biomarkers for inflammation in predicting disease severity in patients with COVID-19. Int. Immunopharmacol. 89, 107065 (2020).
Bassetti, M. et al. EORTC/MSGERC definitions of invasive fungal diseases: Summary of activities of the intensive care unit working group. Clin. Infect. Dis. 72, S121 (2021).
Webb, B. J., Sorensen, J., Jephson, A., Mecham, I. & Dean, N. C. Broad-spectrum antibiotic use and poor outcomes in community-onset pneumonia: a cohort study. Eur. Respir. J. 54, 1900057 (2019).
Smoke, S., Raja, K., Narayanan, N. & Brunetti, L. Selective antibiotic susceptibility reporting and broad-spectrum intravenous antibiotic use: A multicentre ecological study. Int. J. Antimicrob. Agent 54, 367 (2019).
Castanheira, M., Sader, H. S., Deshpande, L. M., Fritsche, T. R. & Jones, R. N. Antimicrobial activities of tigecycline and other broad-spectrum antimicrobials tested against serine carbapenemase- and metallo-beta-lactamase-producing Enterobacteriaceae: Report from the SENTRY antimicrobial surveillance program. Antimicrob. Agents Chemother. 52, 570 (2008).
Liang, C. A. et al. Antibiotic strategies and clinical outcomes in critically ill patients with pneumonia caused by carbapenem-resistant Acinetobacter baumannii. Clin. Microbiol. Infect. 24, 901 (2018).
Kumar, A., Safdar, N., Kethireddy, S. & Chateau, D. A survival benefit of combination antibiotic therapy for serious infections associated with sepsis and septic shock is contingent only on the risk of death: a meta-analytic/meta-regression study. Crit. Care Med. 38, 1651 (2010).
Kluge, S. et al. Aspergillosis: Emerging risk groups in critically ill patients. Med MycoL 60, myab064 (2021).
Fan, D. et al. Activation of HIF-1alpha and LL-37 by commensal bacteria inhibits Candida albicans colonization. Nat. Med. 21, 808 (2015).
Guinan, J., Wang, S., Hazbun, T. R., Yadav, H. & Thangamani, S. Antibiotic-induced decreases in the levels of microbial-derived short-chain fatty acids correlate with increased gastrointestinal colonization of Candida albicans. Sci. Rep.-UK 9, 8872 (2019).
Li, M. et al. Microbiota-driven interleukin-17 production provides immune protection against invasive candidiasis. Crit. Care 24, 268 (2020).
Holmes, A. H. et al. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet 387, 176 (2016).
Wald-Dickler, N. & Spellberg, B. Short-course antibiotic therapy-replacing constantine units with “shorter is better”. Clin. Infect. Dis. 69, 1476 (2019).
Dinh, A. et al. Discontinuing beta-lactam treatment after 3 days for patients with community-acquired pneumonia in non-critical care wards (PTC): a double-blind, randomised, placebo-controlled, non-inferiority trial. Lancet 397, 1195 (2021).
Drekonja, D. M., Trautner, B., Amundson, C., Kuskowski, M. & Johnson, J. R. Effect of 7 vs 14 days of antibiotic therapy on resolution of symptoms among afebrile men with urinary tract infection: a randomized clinical trial. JAMA-J. Am. Med. Assoc. 326, 324 (2021).
Lee, R. A., Stripling, J. T., Spellberg, B. & Centor, R. M. Short-course antibiotics for common infections: What do we know and where do we go from here?. Clin. Microbiol. Infect. 29, 150 (2023).
Egli, A., Schrenzel, J. & Greub, G. Digital microbiology. Clin. Microbiol. Infect. 26, 1324 (2020).
Bassetti, S., Tschudin-Sutter, S., Egli, A. & Osthoff, M. Optimizing antibiotic therapies to reduce the risk of bacterial resistance. Eur. J. Intern. Med. 99, 7 (2022).
Kebriaei, R. et al. Combinations of (lipo)glycopeptides with beta-lactams against MRSA: Susceptibility insights. J. Antimicrob. Chemother. 75, 2894 (2020).
Tan, C. T., Xu, X., Qiao, Y. & Wang, Y. A peptidoglycan storm caused by beta-lactam antibiotic’s action on host microbiota drives Candida albicans infection. Nat. Commun. 12, 2560 (2021).
Lass-Florl, C. et al. Invasive candidiasis. Nat. Rev. Dis. Primers 10, 20 (2024).
Akpan, A. & Morgan, R. Oral candidiasis. Postgrad. Med. J. 78, 455 (2002).
Piazza, O. et al. Candidemia in intensive care patients. Risk factors and mortality. Minerva Anestesiol. 70, 63 (2004).
Dong, Y. et al. The association between geriatric nutritional risk index and the risk of invasive candidiasis in critically ill older adults. BMC Infect. Dis. 23, 530 (2023).
Clancy, C. J. & Nguyen, M. H. Non-culture diagnostics for invasive candidiasis: promise and unintended consequences. J. Fungi 4, 27 (2018).
Clancy, C. J. & Nguyen, M. H. Finding the “missing 50%” of invasive candidiasis: How nonculture diagnostics will improve understanding of disease spectrum and transform patient care. Clin. Infect. Dis. 56, 1284 (2013).
Träger, J. et al. Detailed β-(1→3)-D-glucan and mannan antigen kinetics in patients with candidemia. J. Clin. Microbiol. 61, e0059823 (2023).
Pappas, P. G. et al. Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of America. Clin. Infect. Dis.: Off. Publ. Infect. Dis. Soc. Am. 62, e1 (2016).
Acknowledgements
We thank all the participants and their families involved in this study. Thank the medical teams of Xiangya Hospital, Central South University. We thank all the reviewers who provide feedback on this manuscript.
Funding
This study was supported by the Hunan Natural Science Youth Foundation (2025JJ60503, 2025JJ60739), the National Natural Science Foundation of China (No. 82470078), the National Key Clinical Specialist Construction Programs of China (No. z047-02), Major Research Project for High-Level Talents of Healthcare in Hunan Province (No. R2023032), the Natural Science Foundation of Chang Sha (No. kq2208368), the Natural Science Foundation of Hunan Province of China (No. 2023JJ30930, 2022JJ40800), the National Natural Science Foundation of China (No. 82100100), the Natural Science Foundation of Hunan Province (No. 2022JJ40810), the China Postdoctoral Science Foundation (No. 2022M723558), the National Natural Science Foundation of China (82200099), the Natural Science Foundation of Hunan Province (2022JJ40775) and the Natural Science Foundation of Hunan Province for Excellent Young Scholars (2024JJ4076).
Author information
Authors and Affiliations
Contributions
YL and PP conceived, supervised the study and approved the final version of manuscript. YL revised the manuscript. GC and WL were responsible for data analysis, chart production, and manuscript writing. YZ and YC provided codes for statistical analysis. CS, HL and BL collected data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study was approved by the Ethics Committee of Xiangya Hospital, Central South University (approval number: 202104005). Owing to the retrospective design and the anonymized handling of all data prior to analysis, the Ethics Committee of Xiangya Hospital waived the requirement for informed consent. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, G., Li, W., Zhao, Y. et al. Correlation of broad-spectrum antibiotic utilization patterns with invasive candidiasis in critically ill patients and development of an early prediction model. Sci Rep 15, 39053 (2025). https://doi.org/10.1038/s41598-025-26212-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-26212-9