Abstract
Patient satisfaction with medical care is one of the key outcome indicators of chronic disease healthcare service quality. However, the factors influencing patient satisfaction, particularly from the perspectives of information technology perception and value cocreation, are underexplored. This study aims to examine the relationships between information technology perception, value cocreation behavior, patient trust, and patient satisfaction in chronic disease patients in China community health centers (CHCs). It also investigates the mediating role of value cocreation behavior and the moderating effect of patient trust. A cross-sectional survey was conducted from September 2019 to December 2019 in Wuhan and Taiyuan, China. Participants were selected using a multistage stratified random sampling method. Data were collected via self-administered questionnaires from 722 chronic disease patients in Wuhan and Taiyuan (with a response rate of 90.36%). Patient satisfaction with medical care was measured using a four-item scale. Information technology perception was assessed using scales for perceived ease of use and perceived reliability, adapted from Deng Chaohua et al.‘s measurement of mobile banking system perception. Value co-creation behavior was measured using a 21-item scale adapted from Yi and Gong’s measurement of customer value co-creation behavior, and patient trust was measured using a four-item scale. Pearson correlation analysis was used to assess the relationships among perceived ease of use, perceived reliability, value co-creation behavior, patient trust, and patient satisfaction. Structural equation modeling (SEM) was employed to examine the hypothesized relationships among these variables. The proposed model demonstrated good model fit. Perceived ease of use (β = 0.339, 95% CI 0.188 to 0.493) and value cocreation behavior (β = 0.459, 95% CI 0.387 to 0.530) had direct positive effects on patient satisfaction, while perceived reliability (β = 0.049, 95% CI -0.099 to 0.200) did not have a direct effect on patient satisfaction. Perceived ease of use (β=-0.746, 95% CI -0.907 to -0.623) had a direct negative effect on value cocreation behavior, whereas perceived reliability (β = 0.408, 95% CI 0.283 to 0.577) had a direct positive effect on value cocreation behavior. Perceived ease of use (β=-0.342, 95% CI -0.444 to -0.270) and perceived reliability (β = 0.187, 95% CI 0.127 to 0.277) indirectly influenced patient satisfaction through value cocreation behavior. Patient trust had a significant moderating effect on the relationship between value cocreation behavior and patient satisfaction (β = -0.127, 95% CI -0.197 to -0.056). The study reveals that perceived ease of use and value cocreation behavior significantly influence patient satisfaction, with patient trust playing a moderating role in these relationships. These findings suggest that enhancing patients’ perception of ease of use and promoting value cocreation behavior can improve patient satisfaction, particularly in contexts with low patient trust. To this end, healthcare providers should optimize the design of information systems to support seamless doctor-patient interactions and encourage active patient participation in care processes. Additionally, policymakers are advised to implement strategies that foster trust and facilitate communication within CHCs, especially for patients with chronic diseases.
Similar content being viewed by others
Introduction
With global demographic aging, intensifying environmental pollution, and shifts in lifestyle patterns, the incidence of chronic diseases is on the rise worldwide1,2. In China, chronic diseases account for 87% of total mortality and 70% of the overall disease burden3. Advances in medical technology have continuously enhanced the levels of early screening and prevention of chronic diseases, creating favorable conditions for timely detection and effective management4. However, despite ongoing improvements in chronic disease prevention and treatment in China, patient satisfaction with medical care(hereafter referred to as patient satisfaction) remains low5. Patient dissatisfaction has been associated with doubts regarding the quality of primary healthcare services, a lack of trust in the competence of primary care physicians, and dissatisfaction with the effectiveness of early interventions for chronic diseases6,7. For instance, Chai reported that weak service capacity in rural CHCs contributes to low patient satisfaction6, while Hall et al. highlighted the critical role of trust in shaping patients’ perceptions of care quality and their overall experience7. Consequently, many patients who could be treated in CHCs are instead concentrating in secondary and tertiary hospitals, which contradicts the principles of the Chinese government’s tiered diagnosis and treatment policy8,9,10. Therefore, understanding the factors associated with patient satisfaction in CHC chronic disease management has become particularly important in the current Chinese context.
Several previous studies have investigated potential factors related to the satisfaction of CHC chronic disease patients, such as age, gender, occupation, long waiting times, types of follow-up, and doctor-patient communication5,11,12. However, these studies have primarily focused on demographic factors and job characteristics, neglecting other potential factors (such as perceptions of information technology, value cocreation behaviors, and patient trust).
In fact, effective chronic disease management increasingly relies on active patient participation rather than passive reception of care. This perspective aligns with Service-Dominant Logic (SDL), which views the provider–patient relationship as a collaborative process. Within this framework, value cocreation behavior is defined as the active involvement of patients in shaping healthcare outcomes through actions such as monitoring health indicators, following treatment plans, and sharing personal insights13. For example, diabetic patients who regularly track blood sugar levels and communicate findings to physicians enable more tailored and responsive care14. Gong and Yi developed and validated a multidimensional scale of customer value cocreation behavior in their study, which includes two main dimensions: customer participation behaviors (e.g., information seeking, information sharing, responsible behavior, and personal interaction) and customer citizenship behaviors (e.g., feedback giving, advocacy, helping others, and tolerance)15. This scale demonstrated good reliability and validity, and the study also revealed that these two types of behaviors have distinct antecedents and consequences. However, in practice, the lack of transparency and poor communication between doctors and patients hinder the implementation of value cocreation behaviors16.
Since the advent of the information age, internet-based information technology has been widely applied in chronic disease management, doctor–patient communication, and patient engagement17,18,19. Examples include digital communication tools (DCT)20, eHealth systems21, remote patient monitoring (RPM)19, and patient portals22, all of which provide technological support for patient participation in value cocreation behaviors. In this study, information technology includes both tools used directly by patients—such as mobile appointment scheduling and access to health records—and technologies used by CHC doctors to assist patients. For instance, CHC doctors use information technology to help patients schedule appointments with specialists in higher-level hospitals, enabling online booking and referral functions. Additionally, CHC doctors can connect with physicians in higher-level hospitals via information technology to assist patients in completing remote consultations. The abstract diagram of the information technology used by doctors and patients in this study is shown in Fig. 1, with real-world screenshots provided in supplementary materials 1.
Nevertheless, chronic disease patients are predominantly elderly, and their ability to absorb and accept new technologies is generally lower compared to younger populations23. As information systems become more prevalent, elderly patients are often forced to use these technologies, leading to usability challenges and security concerns24, which in turn suppresses their proactive participation in value cocreation behaviors for chronic diseases and ultimately affects patient satisfaction. Therefore, understanding the relationships among IT perception, value cocreation behavior, trust, and patient satisfaction is essential for exploring pathways to improved service experiences and health outcomes among chronic disease patients from a practical perspective.
According to the classic Technology Acceptance Model (TAM)25 and the theoretical framework constructed by Wang et al. based on the classic model26, information technology in primary care settings today mainly remains at the level of common tools such as CHC information management systems. This study categorizes patients’ perceptions of information technology into two dimensions: perceived ease of use and perceived reliability27. Perceived ease of use refers to the extent to which patients find it effortless to use information technology, while perceived reliability refers to the degree of confidence patients have that hospital information technology is free from security risks26,28. Patient trust is another crucial factor. It is defined as “the acceptance by patients of their relatively disadvantaged position in the medical process, under conditions where they lack the ability to supervise or control the physician, and their expectation that healthcare providers will act in their best interest”29, and has been proven to be significantly associated with patient satisfaction30.
Existing studies have explored the relationships between value cocreation behavior, perceptions of information technology, and patient satisfaction31,32,33,34. However, most focus on commonly used technologies such as online consultations and information retrieval, with limited attention to patient-autonomous or physician-assisted tools in CHCs—such as mobile appointment scheduling, health record access, online referrals, and remote consultations. Furthermore, patient trust, as a critical factor in patient–provider interactions35, has not been clearly defined in terms of its role in the relationship between value cocreation behavior and patient satisfaction. To address this theoretical gap, our study extends prior research in three key ways. First, we consider both patient-autonomous and physician-assisted uses of information technology, capturing the dual dynamics of how patients and CHC doctors jointly engage in care facilitation. Second, we refine the classic Technology Acceptance Model (TAM) by incorporating perceived reliability, a construct particularly salient for elderly patients who are more attuned to issues of digital security and stability. Third, we propose an integrated theoretical model that combines TAM and Service-Dominant Logic (SDL), positioning value cocreation behavior as a mediator between IT perception and patient satisfaction, with patient trust moderating this mediation path.
This study aims to address a key theoretical gap in the health IT literature by linking patients’ technology perceptions with satisfaction through behavioral mechanisms grounded in value cocreation. In doing so, we shift the lens from passive technology use toward active patient engagement—a shift that is particularly important in chronic disease care among elderly patients in primary care settings. By integrating TAM and SDL and introducing trust as a moderator, our research provides a more comprehensive model for understanding satisfaction formation in digitally mediated healthcare. The remainder of this paper is structured as follows. The next section reviews relevant theoretical frameworks and develops the research hypotheses. This is followed by the methodology, results, and discussion of theoretical and practical implications.
Study hypotheses
Perceived ease of use and value cocreation behavior
According to the TAM model, perceived ease of use is defined as the degree to which a user believes that using information technology will be effortless27. Previous studies have explored the positive effects of perceived ease of use on information technology.
According to Srinivas, the ease of use of personal health records plays a mediating role in the perceived value of communication between patients and physicians36. The perceived ease of use of healthcare information systems has a positive impact on patients’ intention to use them, thereby facilitating improved interactions between patients and healthcare providers37. There is an urgent need for research to demonstrate the impact of patients’ perceived ease of use on value cocreation behavior in CHC settings. Therefore, we propose the following hypothesis:
H1
Patients’ perceived ease of use is positively correlated with value cocreation behavior.
Perceived ease of use and patient satisfaction
According to the conceptual analysis of patient satisfaction in healthcare environments by Janet et al.38, this study defines patient satisfaction as a subjective evaluation of the provider’s attitude, technical competence, system accessibility, and effectiveness after receiving care at a CHC. A previous finding indicated that patients’ perceived ease of use of telemedicine products has a positive impact on their satisfaction39. Similarly, studies on satisfaction with mobile applications have shown that consumers’ perceived ease of use of these applications positively influences their satisfaction40. Therefore, we propose the following hypothesis:
H2
Patients’ perceived ease of use is positively correlated with patient satisfaction.
Perceived reliability and value cocreation behavior
Perceived reliability is a new factor introduced by Wang et al. (2003) within the Technology Acceptance Model (TAM) framework, defined as the degree to which patients believe that hospital information technology poses no security risks26. In previous research, Agaku et al. found that patients, due to concerns over the security of their EHR systems, deliberately withheld personal information from their healthcare providers, which in turn negatively impacted patient-provider interactions41. Moreover, it has been demonstrated that consumers’ perceptions of privacy-security risks associated with corporate digital platforms can hinder their participation in value cocreation activities42. However, in the context of chronic disease services, there is an urgent need for evidence demonstrating the impact of perceived reliability on value cocreation behavior among chronic disease patients. We propose the following hypothesis:
H3
Patients’ perceived reliability is positively correlated with value cocreation behavior.
Perceived reliability and patient satisfaction
A prior study explored the role of perceived security in customer satisfaction, demonstrating a significant positive relationship between perceived security and satisfaction43. Research by Dong Wei et al. found that effective communication and trust reduce patients’ perceived risks, thereby enhancing their satisfaction with medical services44. However, there is an urgent need for research demonstrating the relationship between chronic disease patients’ perceptions of information technology and patient satisfaction in CHC. We propose the following hypothesis:
H4
Patients’ perceived reliability is positively correlated with patient satisfaction.
The mediating role of value cocreation behavior
Previous studies have demonstrated the positive effect of perceived ease of use on patients’ engagement with information technology45. The easier the technology is for patients to use, the more it facilitates their active participation in chronic disease management and patient-provider communication46. As patients continue to engage in value cocreation, these behaviors provide more satisfactory experiences, which positively affect their satisfaction with healthcare services47. Additionally, previous research has shown that patients’ perceived safety of information technology can influence their participation in information technology48. When patients perceive low security risks, they are more willing to engage in treatment planning48,49, which directly contributes to their satisfaction. As patients continue to participate in value cocreation, they are more likely to derive benefits from these activities, leading to higher satisfaction scores with the technology. Based on this foundation, we propose the following hypothesis:
H5
The relationship between perceived ease of use, perceived reliability, and patient satisfaction is mediated by value cocreation behavior.
The moderating role of patient trust
Patient trust is defined as “the patient’s acceptance of their relatively vulnerable position in the healthcare process, in the absence of direct oversight or control over the physician, while expecting the provider to act in their best interest”50. In this study, we define patient trust as the cognitive trust patients build toward healthcare providers, based on rational thinking, past experiences, and knowledge. Patient trust can negatively impact value cocreation behavior, thereby indirectly influencing patient satisfaction. Prior studies in various fields have shown similar mechanisms. In the marketing domain, long-term relationships can have a negative effect, inhibiting the positive outcomes of relationship marketing activities51. Younger buyer-seller relationships require more frequent interactions, as these interactions help buyers gain important information, while in more established relationships, such interactions become less necessary52. Similarly, in the medical field, when patients’ trust in healthcare institutions is not high, factors such as patient-provider interactions and value cocreation become important cues for evaluating healthcare satisfaction. As patients gain more direct experience with the services and their trust increases, these factors become less critical as “substitute cues” for satisfaction judgments. Therefore, we propose the following hypothesis:
H6
The effect of value co-creation behavior on patient satisfaction is moderated by patient trust.
Figure 2 illustrates the hypothesized model exploring the interactions examined in this study. Our research contributes to the existing body of knowledge by providing a deeper understanding of the relationships between information technology perception, value cocreation behavior, patient trust, and patient satisfaction.
Methods
Study population and sampling
A cross-sectional survey was conducted from September 2019 to December 2019 in Wuhan and Taiyuan, China. A multistage sampling strategy was employed for data collection53. First, two districts each from Wuhan and Taiyuan were selected based on criteria including geographic location, population density, economic development level, and distribution of healthcare resources. Subsequently, systematic sampling was used to randomly select six CHCs in Taiyuan and seven in Wuhan. Finally, within each selected center, patients diagnosed with chronic diseases were randomly invited to participate in the survey based on their consultation numbers. To ensure a representative sample, potential chronic disease patients presenting during the survey period were also included.
The study included participants who met the following criteria: (1) aged 18 years or older; (2) diagnosed with at least one chronic condition (e.g., hypertension, diabetes, cardiovascular diseases); (3) receiving medical care at one of the selected CHCs; (4) attending the CHC during the survey period (September to December 2019); and (5) willingness to participate and provision of informed consent. Patients were excluded if they: (1) were not diagnosed with a chronic disease; (2) had severe cognitive or mental impairments that might affect their ability to understand or complete the questionnaire; (3) had language barriers that hindered effective communication; (4) were duplicates (only one valid response per individual was retained); or (5) submitted incomplete or invalid questionnaires with substantial missing data or logical inconsistencies. A total of 799 patient questionnaires were distributed, with 722 valid questionnaires returned, yielding an effective response rate of 90.36%.
Accordance statement
This study was reviewed and approved by the Institutional Review Board (IRB) of Yuebei People’s Hospital, Shaoguan, Guangdong, China (Approval Number: YBEC-202406-K11). All methods were carried out in accordance with the principles of the Declaration of Helsinki and relevant ethical guidelines.
Written informed consent was obtained from all participants prior to data collection. For secondary data analysis, we confirm that participants had previously provided consent for future use of their anonymized data, and this secondary use was approved by the IRB without requiring additional consent.
To protect participant privacy, all collected data were fully anonymized and stored securely to prevent unauthorized access. No identifiable personal information, including names, images, or other identifiers, is included in the manuscript or supplementary materials.
As a token of appreciation, each participant who completed the survey received a small non-monetary compensation (a pack of napkins valued at approximately $1.4). This form of compensation was chosen to express gratitude without constituting undue influence or conflict of interest.
Instrument and measurement
Demographic characteristics
The demographic data collected in this study included Gender, Age, and Educational background. These factors were used as control variables in the analysis.
Measurement
In this study, a questionnaire was developed based on well-established scales from authoritative academic sources. The questionnaire was designed to assess perceived ease of use, perceived reliability, value cocreation behavior, satisfaction, and trust in specific technologies and services. To ensure content validity, all items were adapted from previous studies, with modifications made to fit the healthcare context of CHCs. To ensure the quality and relevance of the questionnaire, a pilot test was conducted with 20 graduate students from Tongji Medical College. These participants were assumed to be relatively young and generally familiar with community-based information technologies, making them well-suited to provide insightful feedback. The final version of the questionnaire was refined based on their suggestions and comments. The questionnaire consisted of five scales, measuring 39 items. Each item was rated on a 7-point Likert scale, ranging from “strongly disagree” (1) to “strongly agree” (7).
Patient satisfaction
Patient satisfaction was assessed using a tool adapted from Jillian C. Sweeney et al.‘s measurement of customer satisfaction with healthcare services54. This tool was used to measure customer satisfaction with health services. Our study adapted this tool to the CHC context, designing three questions to evaluate patient satisfaction: (1) I am very satisfied with this CHC, (2) It was a wise decision to choose this center for treatment, and (3) I feel happy with my choice to seek treatment here.
Perceived ease of use
Perceived ease of use was measured using questions adapted from a scale that assessed mobile banking customers’ perceived ease of use of mobile banking systems55. This scale is a brief self-report measure used to evaluate the ease with which customers use mobile banking. Our study adapted this tool to the CHC setting, designing four questions to assess patients’ perceived ease of use of information technology: (1) When I visit the CHC, I am accustomed to using these systems to access services or check my information, (2) I find the system very easy to use, (3) I particularly enjoy using the system to access services/information or to make appointments, payments, and view information, and (4) The system here makes it easy to obtain information.
Perceived reliability
Perceived reliability was assessed using questions adapted from a scale that measured mobile banking customers’ perceived reliability of mobile banking systems55. The perceived reliability tool was used to evaluate the security of personal information in mobile banking. Our study tailored this tool to the specific context of CHCs, designing three questions to assess patients’ perceived security risks related to information technology: (1) When I use the system to access services/information, I trust this system, (2) I trust the medical staff’s ability to use these technologies in the CHC, and (3) I trust the medical staff’s ability to solve problems using technology.
Value cocreation behavior
Patient value cocreation behavior was measured using a scale adapted from Yi and Gong’s description and measurement of value cocreation behavior14. In their study, value cocreation behavior is divided into participation behavior and citizenship behavior. Participation behavior includes several role behaviors essential for successful value cocreation, such as information seeking, information sharing, responsible behavior, and interpersonal interaction. Citizenship behavior includes voluntary extra-role behaviors, such as providing feedback, advocacy behavior, helping behavior, and tolerance behavior. Our study adapted this framework to the CHC context, designing six types of behavior—responsible behavior, interpersonal interaction, positive feedback, voluntary behavior, providing help, and tolerance—encompassing 25 items, including “I completed all tasks necessary for the treatment of my illness.”
Patient trust
Patient trust was measured using a scale adapted from Hoffmann C P et al.‘s measurement of trust56. Our study tailored this tool to the CHC context, designing four questions to assess patients’ trust in the CHC: (1) This CHC is sometimes unreliable, (2) This CHC is absolutely honest and trustworthy, (3) This CHC cares about patients, and (4) This CHC is fully trustworthy.
Statistical analysis
Respondents’ demographic characteristics were described using numbers and percentages. Descriptive statistics were conducted using IBM SPSS version 25 (IBM Corporation, Somers, NY, USA). To evaluate the measurement model, we first assessed the reliability and validity of the constructs. Internal consistency reliability was examined using Cronbach’s Alpha. Convergent validity was evaluated through Composite Reliability (CR) and Average Variance Extracted (AVE), while discriminant validity was assessed using the Fornell–Larcker criterion. These psychometric properties are reported in subsequent tables. Confirmatory factor analysis (CFA) and structural equation modeling (SEM) were performed using Mplus version 8.3. CFA was used to test the factor structure and assess model fit. The overall fit criteria for the structural equation model57 are shown in Table 1. Pearson correlation analysis was conducted using SPSS 25.0 to explore the relationships between variables, with significance set at P <.05. Based on the theoretical model, we tested both mediation and moderated mediation pathways using SEM. The significance of direct, indirect, and interaction effects was evaluated using bias-corrected 95% bootstrap confidence intervals based on 5,000 resamples58. To visualize the moderating effect of patient trust, we employed a simple slope analysis, which is a suitable method for continuous moderators. To improve robustness, we included Health and Treatment Evaluation as a control variable. Additional model outputs, including item-level indicators and structural results controlling for this variable, are provided in supplementary materials 2.
Results
Characteristics of respondents
Among the 722 respondents, more than half of the chronic disease patients were female (55.54%). Patients under the age of 65 comprised 52.35% of the sample. The majority of respondents had an educational level of junior high school or below (44.04%). Nearly half (49.31%) of the chronic disease patients were currently employed or had previously worked in government institutions, public institutions, or enterprises (Table 2).
Correlations among perceived ease of use, perceived reliability, value cocreation behavior, patient trust, and patient satisfaction
Table 3 presents the correlation coefficients between perceived ease of use, perceived reliability, value cocreation behavior, patient trust, and patient satisfaction. Overall, most of the coefficients are statistically significant at the P <.01 level. Specifically, perceived ease of use is positively correlated with perceived reliability and value cocreation behavior. Perceived reliability is positively correlated with value cocreation behavior, patient satisfaction, and patient trust. Value cocreation behavior is positively correlated with both patient satisfaction and patient trust. Additionally, patient satisfaction is positively correlated with patient trust.
Measurement model evaluation
To ensure the psychometric robustness of the study’s constructs, the measurement model was evaluated in terms of reliability, convergent validity, and discriminant validity. The evaluation process followed the two-step approach recommended by Hair et al.59, which includes assessing (1) the reliability and convergent validity of individual constructs and (2) the discriminant validity among constructs. Internal consistency reliability was first examined using both Cronbach’s Alpha and Composite Reliability (CR). As shown in Table 3, all Cronbach’s Alpha values exceeded the recommended threshold of 0.7060, indicating satisfactory internal consistency. Additionally, all CR values were above the recommended threshold of 0.70, confirming composite reliability across all constructs59. Convergent validity was evaluated using the Average Variance Extracted (AVE). All AVE values exceeded the 0.50 threshold61, suggesting that the constructs explained more than half of the variance of their respective indicators (Table 4).
Discriminant validity was assessed using the Fornell–Larcker criterion, based on the AVE values and inter-construct correlations presented above. According to this criterion, the square root of the AVE for each latent variable should exceed its correlations with all other latent constructs, thereby confirming that each construct shares more variance with its own indicators than with any others62. As demonstrated in Table 5, all constructs fulfill this requirement, indicating satisfactory discriminant validity.
Results of the Structural equation modeling (SEM) for perceived ease of use, perceived reliability, value cocreation behavior, and patient satisfaction
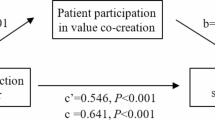
Figure 3 illustrates the model paths with standardized coefficients, while Table 6 presents the direct and indirect effects of the model paths. The significance of all effects was evaluated using 95% confidence interval estimates. The overall model fit was high based on four goodness-of-fit indices: CFI = 0.962, TLI = 0.955, RMSEA = 0.067, and SRMR = 0.073.
Overall, nearly all effects in the model paths were significant, with H2, H4, and H5 being supported, while H1 and H3 were not supported. Specifically, perceived ease of use had a significant direct effect on patient satisfaction (β = 0.339, 95% CI: 0.188 to 0.493) and on value cocreation behavior (β=−0.746, 95% CI: −0.907 to −0.623). Perceived reliability did not have a significant effect on patient satisfaction (β = 0.049, 95% CI: −0.099 to 0.200) but had a significant direct effect on value cocreation behavior (β = 0.408, 95% CI: 0.283 to 0.577). Value cocreation behavior had a significant direct effect on patient satisfaction (β = 0.459, 95% CI: 0.387 to 0.530). In terms of indirect effects, the study found that value cocreation behavior mediated the relationship between perceived ease of use (β=−0.342, 95% CI: −0.444 to −0.270) and perceived reliability (β = 0.187, 95% CI: 0.127 to 0.277) with patient satisfaction.
Structural model pathways and standardized coefficients for perceived ease of use, perceived reliability, value cocreation behavior, and patient satisfaction. This figure illustrates the structural model with standardized path coefficients depicting the relationships among perceived ease of use, perceived reliability, value cocreation behavior, and patient satisfaction.
The moderating role of patient trust
Since patient trust is modeled as a continuous rather than a categorical variable, we employed simple slope analysis to probe the nature of the moderation effect. This approach allows us to estimate the conditional impact of value co-creation behavior on patient satisfaction at varying levels of trust, without introducing arbitrary group splits. This method is considered a robust technique for probing interaction effects in studies involving continuous moderators in health informatics and behavioral research contexts64. Based on this approach, we incorporated patient trust into the structural model and tested its moderating effect on the relationship between value co-creation behavior and patient satisfaction. The model demonstrated good fit (CFI = 0.945, TLI = 0.937, SRMR = 0.092, RMSEA = 0.073). The moderation analysis showed that the interaction term between value co-creation behavior and patient trust had a significant negative effect on patient satisfaction (β=−0.127, 95% CI: −0.197 to −0.056), indicating that patient trust significantly moderates the relationship between value co-creation behavior and satisfaction. As shown in Fig. 4, the simple slope analysis further revealed that the slope for the low-trust group was steeper than that for the high-trust group. This suggests that when patient trust is low, value co-creation behavior has a stronger effect on improving satisfaction, thereby supporting Hypothesis H6.
The moderating effect of patient trust on the relationship between value cocreation behavior and patient satisfaction. This figure illustrates the moderating role of patient trust in the relationship between value cocreation behavior (VCCB) and patient satisfaction. The graph presents three levels of patient trust: High Trust (M + 1SD), Medium Trust (M), and Low Trust (M − 1SD).
Discussion
The direct and indirect effects of perceived ease of use on patient satisfaction
Perceived ease of use is a pivotal determinant of patient satisfaction, exerting both direct and indirect effects. Patients’ perception of the ease of using health information technology (HIT) is closely tied to the functional efficacy of the technology itself. Empirical evidence has suggested that electronic health records (EHRs) with superior system and information quality enable patients to efficiently retrieve and update their medical data, thereby enhancing accessibility and, consequently, user experience and satisfaction65. However, this convenience may inadvertently reduce the frequency of face-to-face communication between patients and primary care physicians, potentially fostering detrimental communication behaviors such as verbal interruptions, reduced eye contact, and increased multitasking66,67,68. This may account for the finding that contradicted Hypothesis 1, where perceived ease of use had a negative effect on value co-creation behavior. This observation is further supported by interview data collected from CHCs in Wuhan and Taiyuan, China. For example, during clinical consultations, physicians frequently relied on system-uploaded data (provided by nurses and medical technicians) to diagnose patients, which, while streamlining the process, diminished direct patient–provider interaction. Looking forward, developers of health information systems (HIS) for chronic disease management (CDM) should prioritize facilitating value co-creation. For instance, mobile health (mHealth) applications tailored for CDM could include features that allow patients to self-monitor key health metrics (e.g., blood pressure, heart rate), share real-time updates with clinicians, and receive personalized feedback. Such designs may enhance the frequency of interactions while simultaneously improving the timeliness and accuracy of clinical interventions.
The direct and indirect effects of perceived reliability on patient satisfaction
In our study, we found that patients’ perceived reliability of information technology did not have a direct positive impact on patient satisfaction, which is inconsistent with findings from previous research69,70. Dhagarra et al. reported that in unfamiliar healthcare environments, patients’ concerns about health information privacy could lead them to avoid certain services altogether71. In this study, perceived reliability was defined as the extent to which patients with chronic diseases at CHCs believed that the information systems were free from security risks. The patients we surveyed typically visited CHCs frequently, as the Chinese government had designated the standardized management of hypertension and diabetes as a performance target for these institutions. This familiarity may have resulted in an unconscious normalization of system reliability, thus rendering it less impactful on patient satisfaction. The saturation effect72 theoretically supports our finding that perceived reliability did not significantly influence value co-creation behavior within this community-based context. Clinically, this implies that while ensuring system security remains essential, such features alone may not substantially contribute to patient satisfaction unless they directly support the care process or strengthen provider–patient relationships. Therefore, rather than focusing solely on technical reliability, future IT systems should emphasize functionalities that promote shared decision-making, enable remote monitoring, and facilitate timely communication—core elements of effective chronic disease management. That said, the role of perceived reliability in CHC IT systems should be further investigated using larger and more diverse samples.
The moderating role of patient trust
We found that patient trust negatively moderated the relationship between value co-creation behavior and patient satisfaction, suggesting that the positive impact of co-creation behavior was stronger when trust levels were low. This finding aligns with evidence from other fields73. In marketing research, for example, buyer–seller relationships characterized by lower levels of trust tend to require more frequent and intensive interactions to compensate for informational asymmetries, thereby enhancing transactional satisfaction74,75. In the healthcare setting, this implies that when patient trust in providers is low, value co-creation behaviors—such as active engagement, feedback, and open communication—become particularly crucial. These behaviors enable providers to tailor care strategies, especially in chronic disease management, thereby increasing satisfaction. However, as trust increases, the marginal benefit of such interactions diminishes, consistent with the principle of diminishing marginal returns76. Hence, value co-creation plays a more central role in improving satisfaction among patients with lower baseline trust. Health systems aiming to optimize outcomes should therefore focus on enhancing collaborative communication, promoting patient engagement, and expanding support services in low-trust scenarios.
Theoretical contributions
This study refines and extends two foundational frameworks in health IT research—Technology Acceptance Model (TAM) and Service-Dominant Logic (SDL). First, the observed negative relationship between perceived ease of use and value co-creation behavior challenges traditional TAM assumptions that ease of use invariably promotes engagement. This suggests that in primary care contexts, overly simplified systems may reduce patient–provider communication, thereby hindering co-creation. Second, by introducing perceived reliability as a key antecedent, we enrich TAM with a construct particularly salient to elderly chronic disease patients who are sensitive to issues of security and trust.Third, the integration of SDL enabled us to reconceptualize patients as active co-creators rather than passive recipients, offering a relationally grounded behavioral mechanism for satisfaction formation. Finally, the moderating role of patient trust sheds light on how interpersonal dynamics influence the effectiveness of co-creation, revealing nuanced boundary conditions for digital health interventions.
Practical and managerial implications
From a practical standpoint, the findings provide actionable insights for CHCs, system developers, and health policymakers. First, our results underscore the critical role of value co-creation in driving satisfaction, particularly among patients with lower levels of trust. Therefore, intervention designs should prioritize enhancing patient engagement strategies, such as incorporating goal-setting, real-time feedback, and bidirectional communication features in digital tools. Second, the non-significant direct effect of perceived reliability suggests that technical soundness alone is insufficient—CHC systems must go beyond stability to support relational and collaborative functions. To this end, designers should embed modules that facilitate shared decision-making, patient education, and caregiver coordination. Third, since trust moderates co-creation effects, fostering trust must be a strategic priority, especially in environments where patient skepticism is high. Training programs for providers on empathetic communication, transparency in care plans, and continuity of care may build trust and enhance the patient experience. These implications offer a roadmap for optimizing chronic care delivery in aging populations using community-based digital platforms.
Limitations and future directions
Several limitations should be noted. The observed associations—particularly the negative link between perceived ease of use and satisfaction and the absence of a significant effect of reliability on value co-creation—may be influenced by the study sample. Participants were drawn exclusively from CHCs in two Chinese cities, which may limit the generalizability of the findings. Future research should replicate this study across different regions and healthcare systems to assess the robustness of these relationships in broader contexts. Such efforts will help determine whether the findings reflect universal trends or context-specific phenomena.
Conclusion
In summary, this study identified three pathways influencing patient satisfaction. Perceived ease of use and value co-creation behavior had significant direct effects on patient satisfaction, whereas perceived reliability did not demonstrate a direct effect. Both perceived ease of use and perceived reliability indirectly influenced patient satisfaction through value co-creation behavior. Patient trust moderated the effect of value co-creation behavior on patient satisfaction.
Data availability
Data are available upon reasonable request to author Jing Liu(jliu19871st@163.com).
References
Milani, R. V. & Lavie, C. J. Health care 2020: reengineering health care delivery to combat chronic disease. Am. J. Med. 128 (4), 337–343. https://doi.org/10.1016/j.amjmed.2014 (2015).
Raghupathi, W. & Raghupathi, V. An empirical study of chronic diseases in the united states: A visual analytics approach. Int. J. Environ. Res. Public. Health. 15 (3), 431. https://doi.org/10.3390/ijerph15030431 (2018).
Huang, Z., Cao, C., Xu, M. & Yang, X. Impact of environmental exposure on chronic diseases in China and assessment of population health vulnerability. ISPRS Int. J. Geo-Information. 12 (4), 155. https://doi.org/10.3390/ijgi12040155 (2023).
Huang, P., Xu, L. & Xie, Y. Biomedical applications of electromagnetic detection: A brief review. Biosens. (Basel). 11 (7), 225. https://doi.org/10.3390/bios11070225 (2021).
Lu, Y., Zhao, Y., Shangguan, X., Lv, B. & Huang, R. Patient attitude and determinants toward chronic diseases control: A cross-sectional survey in rural China. Front. Public. Health. 10, 970032. https://doi.org/10.3389/fpubh.2022.970032 (2022).
Chai, S. Research on Status and Countermeasures of Interpersonal Continuity of Health Care in Rural Areas (Huazhong University of Science & Technology, 2016).
Hall, M. A., Dugan, E., Zheng, B. & Mishra, A. K. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter?. Milbank Q 79(4), 613–39. https://doi.org/10.1111/1468-0009.00223 (2001).
Jiang, S. et al. Tertiary hospitals or community clinics? An enquiry into the factors affecting patients’ choice for healthcare facilities in urban China. China Econ. Rev. 63, 101538. https://doi.org/10.1016/j.chieco.2020.101538 (2020).
Xu, J., Wang, X., Hao, H., Wang, J. & Nicholas, S. Impact of hierarchical hospital reform on patients with diabetes in china: a retrospective observational analysis. BMJ Open. 11, e041731. https://doi.org/10.1136/bmjopen-2020-041731 (2021).
Li, C., Chen, Z. & Khan, M. M. Bypassing primary care facilities: health-seeking behavior of middle age and older adults in China. BMC Health Serv. Res. 21 (1), 895. https://doi.org/10.1186/s12913-021-06908-0 (2021).
Ng, J. X. et al. Chronic disease self-management competency and care satisfaction between users of public and private primary care in Singapore. Ann. Acad. Med. Singap. 50 (2), 149–158. https://doi.org/10.47102/annals-acadmedsg.2020216 (2021).
Parizad, N., Goli, R., Mirzaee, R., Baghaie, R. & Habibzadeh, H. Satisfaction with nursing care and its related factors in patients with COVID-19: A descriptive correlational study. J. Educ. Health Promot. 10, 437. https://doi.org/10.4103/jehp.jehp_79_21 (2021).
David, G. Co-Creation of Value in Patient-Centered Care: A Service- Dominant Logic Approach in Pharmacy Practice. (2021). https://doi.org/10.13140/RG.2.2.33279.32160
Shirish, C. & Srivastava Bridging the service divide through digitally enabled service innovations. MIS Q. 39 (1), 245–267 (2015). https://www.jstor.org/stable/26628349
Yi, Y. & Gong, T. Customer value co-creation behavior: Scale development and validation. J. Bus. Res. 66(9), 1279–1284. https://doi.org/10.1016/j.jbusres.2012.02.026 (2013).
Sandhu, M. A., AlMeraikhi, M. H., Saleem, A. & Farooq, M. Effectiveness of value co-creation in healthcare system from patients’ perspectives. Benchmarking: Int. J. https://doi.org/10.1108/BIJ-10-2023-0688 (2024).
Seljelid, B., Varsi, C., Solberg Nes, L., Øystese, K. A. & Børøsund, E. Feasibility of a digital Patient-Provider communication intervention to support shared Decision-Making in chronic health Care, involveme: pilot study. JMIR Form. Res. 6 (4), e34738. https://doi.org/10.2196/34738 (2022).
Wannheden, C. et al. Digital health technologies enabling partnerships in chronic care management: scoping review. J. Med. Internet Res. 24 (8), e38980. https://doi.org/10.2196/38980 (2022).
Xu, R. H., Zhou, L. M., Wong, E. L. & Wang, D. The association between patients’ eHealth literacy and satisfaction with shared Decision-making and Well-being: multicenter Cross-sectional study. J. Med. Internet Res. 23 (9), e26721. https://doi.org/10.2196/26721 (2021).
Balki, E., Holland, C. & Hayes, N. Use and acceptance of digital communication technology by older adults for social connectedness during the COVID-19 pandemic: mixed methods study. J. Med. Internet Res. 25, e41535. https://doi.org/10.2196/41535 (2023).
Bitar, H. & Alismail, S. The role of eHealth, telehealth, and telemedicine for chronic disease patients during COVID-19 pandemic: A rapid systematic review. Digit. Health. 7, 20552076211009396. https://doi.org/10.1177/20552076211009396 (2021).
Kinney, A. P. & Sankaranarayanan, B. Effects of patient portal use on patient satisfaction: survey and partial least squares analysis. J. Med. Internet Res. 23 (8), e19820. https://doi.org/10.2196/19820 (2021).
Phalswal, U., Pujari, V., Sethi, R. & Verma, R. Impact of social media on mental health of the general population during Covid-19 pandemic: A systematic review. J. Educ. Health Promot. 12(1), 23. https://doi.org/10.4103/jehp.jehp_460_22 (2023).
Cheshmehzangi, A., Zou, T. & Su, Z. The digital divide impacts on mental health during the COVID-19 pandemic. Brain Behav. Immun. 101, 211–213. https://doi.org/10.1016/j.bbi.2022.01.009 (2022).
Lu, Y. B. & Xu, H. M. A comparative study of the technology acceptance model and related theories. Sci. Technol. Progress Policy. 22 (10), 176–178. https://doi.org/10.3969/j.issn.1001-7348.2005.10.063 (2005).
Zandhessami, H. & Geranmayeh, P. Determinants of user acceptance of internet banking: an empirical study. Int. J. Ind. Eng. Comput. 4 (7). https://doi.org/10.5267/j.msl.2014.6.035 (2014).
Li, X. et al. The primary health-care system in China. Lancet 390 (10112), 2584–2594. https://doi.org/10.1016/S0140-6736(17)33109-4 (2017).
Jaradat, M. I. R. M. & Smadi, Z. M. A. Applying the technology acceptance model to the introduction of mobile healthcare information systems. Int. J. Behav. Healthc. Res. 28(2) https://doi.org/10.1504/ijbhr.2013.057363 (2013).
Punyatoya, P. Effects of cognitive and affective trust on online customer behavior. Mark. Intell. Plann. 25(1), 80–96. https://doi.org/10.1108/MIP-02-2018-0058 (2019).
Yan, Y. H., Kung, C. M. & Kung, L. H. The Trust and Interaction in Doctor-Patient Relationship on Patient Satisfaction. In Proceedings for Annual Meeting of The Japanese Pharmacological Society WCP2018 (The 18th World Congress of Basic and Clinical Pharmacology). Japanese Pharmacological Society, PO2-8-29 (2018).
Peng, Y., Yin, P., Deng, Z. & Wang, R. Patient-Physician interaction and trust in online health community: the role of perceived usefulness of health information and services. Int. J. Environ. Res. Public. Health. 17 (1), 139. https://doi.org/10.3390/ijerph17010139 (2019).
Liu, W., Fan, X., Ji, R. & Jiang, Y. Perceived community Support, users’ Interactions, and value Co-Creation in online health community: the moderating effect of social exclusion. Int. J. Environ. Res. Public. Health. 17 (1), 204. https://doi.org/10.3390/ijerph17010204 (2019).
Woratschek, H., Horbel, C. & Popp, B. Determining customer satisfaction and loyalty from a value co-creation perspective. Serv. Ind. J. 40 (11–12), 777–799. https://doi.org/10.1080/02642069.2019.1606213 (2019).
Fusco, F., Marsilio, M. & Guglielmetti, C. Co-creation in healthcare: framing the outcomes and their determinants. J. Service Manage. 34 (6), 1–26. https://doi.org/10.1108/JOSM-06-2021-0212 (2023).
Dang, B. N., Westbrook, R. A., Hartman, C. M. & Giordano, T. P. Retaining HIV patients in care: the role of initial patient care experiences. AIDS Behav. 20 (10), 2477–2487. https://doi.org/10.1007/s10461-016-1340-y (2016).
PEmani, S. et al. Patient perceptions of a personal health record: a test of the diffusion of innovation model. J. Med. Internet Res. 14 (6), e150. https://doi.org/10.2196/jmir.2278 (2012).
MPai, F. Y. & Huang, K. I. Applying the technology acceptance model to the introduction of healthcare information systems. Technol. Forecast. Soc. Chang. 78 (4), 650–660. https://doi.org/10.1016/j.techfore.2010.11.007 (2011).
Ng, J. H. Y. & Luk, B. H. K. Patient satisfaction: concept analysis in the healthcare context. Patient Educ. Couns. 102 (4), 790–796. https://doi.org/10.1016/j.pec.2018.11.013 (2019).
Wijaya, I. G. A. & Darma, G. S. Measuring The Role of Patient Satisfaction as A Mediation of Perceived Usefulness and Ease of Use Telemedicine Towards Patient Loyalty. Jurnal Manajemen Bisnis 2022 Fab 19(1), 70–84. https://doi.org/10.38043/jmb.v19i1.4603 (2022).
Khatimah, H. & Halim, F. The influence of perceived usefulness, percieved ease of use and awareness of services on consumers intention to use e-money mobile. Am.-Eurasian J. Sustain. Agric. (2014). http://www.aensiweb.com/AEJSA/
Walker, D. M., Johnson, T., Ford, E. W. & Huerta, T. R. Trust Me, i’m a doctor: examining changes in how privacy concerns affect patient withholding behavior. J. Med. Internet Res. 19 (1), e2. https://doi.org/10.2196/jmir.6296 (2017).
Shah, S. H. H., Noor, S., Shen, L., Butt, A. S. & Ali, M. Role of privacy/safety risk and trust on the development of prosumption and value co-creation under the sharing economy: a moderated mediation model. Inf. Technol. Dev. https://doi.org/10.1080/02681102.2021.1877604 (2021).
Goode, S., Lin, C., Tsai, J. C. & Jiang, J. J. Rethinking the role of security in client satisfaction with software-as-a-service (saas) providers. Decis. Support Syst. 70, 73–85. https://doi.org/10.1016/j.dss.2014.12.005 (2015).
Wei, D., Xu, A. & Wu, X. The mediating effect of trust on the relationship between doctor-patient communication and patients’ risk perception during treatment. Psych J. 9 (3), 383–391. https://doi.org/10.1002/pchj.327 (2020).
Kalayou, M. H., Endehabtu, B. F. & Tilahun, B. The applicability of the modified technology acceptance model (TAM) on the sustainable adoption of eHealth systems in Resource-Limited settings. J. Multidiscip Healthc. 13, 1827–1837. https://doi.org/10.2147/JMDH.S284973 (2020).
van de Vijver, S. et al. Evaluation of a digital Self-management platform for patients with chronic illness in primary care: qualitative study of stakeholders’ perspectives. JMIR Form. Res. 6 (8), e38424. https://doi.org/10.2196/38424 (2022).
Kim, J. Customers’ value co-creation with healthcare service network partners: the moderating effect of consumer vulnerability. J. Service Theory Pract. 29 (3), 309–328. https://doi.org/10.1108/jstp-08-2018-0178 (2019).
Kisekka, V. & Giboney, J. S. The effectiveness of health care information technologies: Evaluation of trust, security beliefs, and privacy as determinants of health care outcomes. J. Med. Internet Res. 20(4), e107. https://doi.org/10.2196/jmir.9014 (2018).
Burkhard, R. J., Schooley, B., Dawson, J. & Horan, T. A. Information systems and healthcare XXXVII: when your employer provides your personal health record—exploring employee perceptions of an employer-sponsored PHR system. Commun. Association Inform. Syst. 27 (1), 19. https://doi.org/10.17705/1CAIS.02719 (2010).
Punyatoya, P. Effects of cognitive and affective trust on online customer behavior. Mark. Intell. Plann. 37 (1), 80–96. https://doi.org/10.1108/MIP-02-2018-0058 (2019).
Grayson, K. & Ambler, T. The dark side of long-term relationships in marketing services. J. Mark. Res. 36 (1), 132–141. https://doi.org/10.1177/00222437990360011 (1999).
Nicholson, C. Y., Compeau, L. D. & Sethi, R. The role of interpersonal liking in Building trust in long-term channel relationships. J. Acad. Mark. Sci. 29, 3–15. https://doi.org/10.1177/0092070301291001 (2001).
Bian, D. et al. Determinants influencing the adoption of internet health care technology among Chinese health care professionals: extension of the Value-Based adoption model with burnout theory. J. Med. Internet Res. 25, e37671. https://doi.org/10.2196/37671 (2023).
Sweeney, J. C., Danaher, T. S. & Mccoll-Kennedy, J. R. Customer effort in value cocreation activities. J. Serv. Res. 18(3), 1419–24. https://doi.org/10.1177/1094670515572128 (2015).
Deng, C. H., Lu, Y. B. & Zhang, J. L. The impact of TAM, reliability, and usability on users’ adoption of mobile banking services. Manag. Rev. 21(1), 59–66 (2009).
Wang, Q. E., Myers, M. D. & Sundaram, D. Digital natives and digital immigrants. Bus. Inf. Syst. Eng. 5(6), 409–419. https://doi.org/10.1007/s12599-013-0296-y (2013).
Quintana, S. M. & Maxwell, S. E. Implications of recent developments in structural equation modeling for counseling psychology. Couns. Psychol. 27(4), 485–527. https://doi.org/10.1177/0011000099274002 (1999).
Qiu, L. et al. The mediating effects of stigma on depressive symptoms in patients with tuberculosis: A structural equation modeling approach. Front. Psychiatry. 9, 618. https://doi.org/10.3389/fpsyt.2018.00618 (2018).
Hair, J. F., Sarstedt, M., Ringle, C. M. & Mena, J. A. An assessment of the use of partial least squares structural equation modeling in marketing research. J. Acad. Mark. Sci. 40, 414–433 (2012).
Legate, A. E., Hair, J. F., Chretien, J. L. & Risher, J. L. PLS-SEM: Prediction-oriented solutions for HRD researchers. Hum. Res. Dev. Q. 1–19. https://doi.org/10.1002/hrdq.21466 (2021).
Hair, J. F., Sarstedt, M., Hopkins, L., Kuppelwieser, G. & V Partial least squares structural equation modeling (PLS-SEM): an emerging tool in business research. Eur. Bus. Rev. 26, 106–121. https://doi.org/10.1108/EBR-10-2013-0128 (2014).
Henseler, J., Ringle, C. M. & Sinkovics, R. R. The use of partial least squares path modeling in international marketing. New. Challenges Int. Mark. Adv. Int. Mark. 20, 277–319. https://doi.org/10.1108/S1474-7979(2009)0000020014 (2009).
Lowry, P. B. & Gaskin, J. Partial least squares (PLS) structural equation modeling (SEM) for Building and testing behavioural causal theory: when to choose it and how to use it. IEEE Trans. Prof. Commun. 57 (2), 123–146 (2014).
Jin, H. & Qu, Y. Association between intergenerational Support, technology perception and Trust, and intention to seek medical care on the internet among Chinese older adults: Cross-Sectional questionnaire study. J. Med. Internet Res. 27, e65065. https://doi.org/10.2196/65065 (2025).
Samha, A. K., Alrashdi, A. M. & Alshammri, G. H. The influencing factors of digital health passport adoption and acceptance during COVID-19 in Saudi Arabia. Digit. Health. 8, 20552076221142668. https://doi.org/10.1177/20552076221142668 (2022).
Heidt, E. L. Health information technology and physician-patient interactions: impact of computers on communication during outpatient primary care visits. J. Am. Med. Inf. Assoc. 2006 Mar-Apr. 13 (2), 236. https://doi.org/10.1197/jamia.M (1999).
Doyle, R. J. et al. Computers in the examination room and the electronic health record: physicians’ perceived impact on clinical encounters before and after full installation and implementation. Fam. Pract. 29 (5), 601–608. https://doi.org/10.1093/fampra/cms015 (2012).
Alkureishi, M. A. et al. Impact of electronic medical record use on the Patient-Doctor relationship and communication: A systematic review. J. Gen. Intern. Med. 31 (5), 548–560. https://doi.org/10.1007/s11606-015-3582-1 (2016).
Wang, S., Wang, X., Zhou, Y. & Xu, J. Utilization of, satisfaction toward, and challenges for Internet-based healthcare services provided by primary health institutions: evidence from China. Front. Public. Health. 10, 1100634. https://doi.org/10.3389/fpubh.2022.1100634 (2023).
Izzatty, I. N. & Hazana, A. N. A systematic review of patient satisfaction on health information exchange in Malaysian Public Healthcare Organizations. J. Phys.: Conf. Ser. 1049(1), 12024. https://doi.org/10.1088/1742-6596/1049/1/012024 (2018).
Dhagarra, D., Goswami, M. & Kumar, G. Impact of trust and privacy concerns on technology acceptance in healthcare: an Indian perspective. Int. J. Med. Inf. 141, 104164. https://doi.org/10.1016/j.ijmedinf.2020.104164 (2020).
Haidekker, M. A. Chapter 8 - Linearization of Nonlinear Components. In Linear Feedback Controls: The Essentials 1st edn 113–120 (Elsevier, 2013). https://doi.org/10.1016/B978-0-12-405875-0.00008-5.
Coulter, K. S. & Coulter, R. A. Determinants of trust in a service provider: the moderating role of length of relationship. J. Serv. Mark. 16(1), 35–50. https://doi.org/10.1108/08876040210419406 (2002).
Grayson, K. & Ambler, T. The dark side of long-term relationships in marketing services. J. Mark. Res. 36 (1), 132–141. https://doi.org/10.1177/002224379903600111 (1999).
Nicholson, C. Y., Compeau, L. D. & Sethi, R. The role of interpersonal liking in building trust in long-term channel relationships. J. Acad. Mark. Sci. 29(1), 3–15. https://doi.org/10.1177/0092070301291001 (2001).
Shephard, R. W. & Färe, R. The law of diminishing returns. Z. Natl. 34(1), 69–90. https://doi.org/10.1007/BF01289147 (1974).
Acknowledgements
We would like to express our sincere gratitude to all participants. This research was supported by the National Natural Science Foundation of China (No. 72204153), National Natural Science Foundation of China (No. 72574133), National Natural Science Foundation of China (No. 72204069), National Natural Science Foundation of China (No. 72464012), Project of Hainan Natural Science Foundation(No. 821RC578).
Author information
Authors and Affiliations
Contributions
Wei Lu contributed to the conceptualization, methodology, supervision, and resources. Jing Liu was responsible for research design, data analysis, data interpretation, and manuscript writing. Kuanlie Jiang, Tingting Yang, Ruoxin Xu, Yan Xuan and Ying Han contributed to software, investigation, writing revisions, and editing. Kuanlie Jiang were responsible for data interpretation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, J., Jiang, K., Yang, T. et al. Information technology perception and value cocreation behavior influence patient satisfaction in chronic disease care. Sci Rep 15, 42985 (2025). https://doi.org/10.1038/s41598-025-27001-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-27001-0