Abstract
Postnatal depression is a global challenge for healthcare system, affecting a large number of mothers globally. The present study was designed to examine the role of obstetric factors such as delivery method, birth complications, perceived birth trauma, and satisfaction with childbirth in postnatal depression (PND) among Pakistani women. By adopting a cross-sectional research design, a purposive sampling technique was used to collect data from the 335 women within the postpartum period (42–84 days) from six public and private hospitals and clinics of Punjab, Pakistan. Age of the sample ranged between 18 and 47 years (M = 29.41, SD = 5.32). Demographic and Birth Information sheet, Edinburgh Postnatal Depression Scale and Birth Satisfaction Scale-Revised were used to collect data for hypotheses testing. After assessing intercorrelations between the study variables, a hierarchical regression analysis was run by controlling age and education. The results showed that a significant amount of variance (R2 = 0.39) in PND was accounted for by low birth satisfaction, mother birth complications, previous birth trauma, and birth trauma perception. The findings suggest that providing a secure, respectful, and supportive environment during childbirth can substantially reduce the risk of PND. Positive childbirth experiences—characterized by care, respect, and fulfillment of psychological needs—serve as protective factors against PND. Study has implications for researchers, midwives, and obstetricians.
Similar content being viewed by others
Introduction
The birth of a child is an exciting yet potentially overwhelming experience, often accompanied by feelings of burden, worry, sadness, and self-doubt. Postnatal depression (PND), a persistent depressive disorder following childbirth, ranges from mild sadness to severe depression and often co-occurs with anxiety. If untreated, PND can last for years. Also referred to as postpartum depression (PPD), up to 40% of PND cases begin during pregnancy1.
Key indicators of PND include severe sadness, loneliness, mood swings, hopelessness, fatigue, guilt, loss of appetite, and frequent crying spells2. According to the International Classification of Diseases (ICD-10), postpartum depression occurs within the first 42 days after childbirth3,4. If left untreated, it adversely affects maternal relationships, physical health, childcare, and professional functioning, and is associated with substance abuse and breastfeeding difficulties5.
PND is a major public health concern, affecting up to 17% of healthy mothers globally, though prevalence varies widely6,7. In high-income countries such as Singapore, the Netherlands, and Switzerland, rates range from 3 to 11%, whereas in low- and middle-income countries (LMICs) like Pakistan, India, and Nepal, rates are much higher due to socioeconomic disparities, maternal/infant mortality, and women’s workload6. Studies in Pakistan report prevalence rates from 28% to 63%, with cesarean delivery linked to higher risk8,9.
Despite the higher vulnerability of women in LMICs, research on PND remains limited. Understanding its predictors and consequences within diverse sociocultural contexts is essential for developing effective interventions. Although demographic, social, and obstetric factors have been identified as contributors, they remain underexplored in LMIC settings.
Although the exact etiology of PND remains unclear, studies have identified multiple risk factors, including low educational attainment10, prior psychiatric history, perinatal stress, insufficient partner or family support, relationship conflicts, domestic violence, and major life stressors such as bereavement or separation11,12. Economic hardships and limited access to healthcare also exacerbate the risk13. Additionally, maternal characteristics such as age, parenting confidence, and socioeconomic status—often inferred through education level—significantly influence PND risk. For example, women with higher education are less likely to experience PND10,14. In Pakistan, PND is more prevalent among young, low-income, less-educated housewives living in extended families15.
Obstetric complications and traumatic birth experiences are also significant contributors to PND. Severe obstetric complications have been associated with increased risk for PND and poorer physical health15,16. Negative experiences, such as obstetric violence and invasive medical interventions, further exacerbate the risk17,18,19. Obstetric violence includes mistreatment, negligence, and human rights violations during childbirth20. Traumatic childbirth experiences often lead to increased PND risk, future fear of childbirth, and preferences for cesarean delivery21,22.
Satisfaction with childbirth is another critical obstetric factor that determines PND. Factors influencing satisfaction include personal expectations, support during delivery, quality of caregiver-patient relationships, and participation in decision-making23. Studies consistently report an inverse relationship between birth satisfaction and PND risk24,25. For example, Urbanová et al.26 found that lower childbirth satisfaction significantly predicted higher PND risk, even after controlling for sociodemographic and clinical variables.
Postnatal depression is a pressing public health concern in Pakistan, with prevalence rates ranging from 28% to 63%. These figures are alarmingly higher than those reported in many developed countries, reflecting a significant burden on maternal and infant health. Despite its prevalence and adverse outcomes—including impaired maternal well-being, negative infant development, and strained family dynamics—PND remains an underexplored area in Pakistan. Most of the existing research has been conducted in Western contexts, where sociocultural, economic, and healthcare conditions differ significantly from those in low- and middle-income countries (LMICs) like Pakistan. The lack of indigenous studies on PND limits the understanding of its prevalence, underlying factors, and cultural nuances in Pakistan. In particular, obstetric factors such as delivery method, birth complications, perceived birth trauma, and satisfaction with childbirth, which have been shown to influence PND risk in other contexts, are understudied in the Pakistani population. Pakistani women represent a unique population for studying birth satisfaction and postnatal depression due to the country’s distinct sociocultural context, family structures, and maternal care practices. Traditional gender roles, limited mental health awareness, and varying access to maternal healthcare services influence women’s childbirth experiences and emotional well-being in ways that differ from Western populations. Understanding these factors within the Pakistani context is essential for developing a culturally sensitive interventions and policies to support maternal mental health.
Although international research has extensively explored birth satisfaction and postnatal depression, there is limited empirical evidence from Pakistan addressing how healthcare practices, and other negative birth experiences lead to PND in postnatal women. Existing studies in the region often focus on medical outcomes rather than women’s psychological and emotional well-being. Moreover, few studies have simultaneously examined birth satisfaction and postnatal depression using standardized measures within the Pakistani context. This gap highlights the need for context-specific research to understand the psychological dimensions of childbirth. The current study addresses these gaps by examining the relationship between obstetric factors and PND symptoms during the postpartum period (42–84 days). By focusing on the Pakistani context, this research will contribute to the take evidence-based, culturally sensitive preventive and curative measures for identifying and addressing PND in vulnerable women in Pakistan.
Hypotheses
Following hypotheses were tested in the study:
H1:
Delivery method, mother birth complications, infant birth complications, birth trauma perception, previous birth trauma, and birth satisfaction significantly correlate with the post-natal depression in postnatal Pakistani women;
H2:
Delivery method, mother birth complications, infant birth complications, birth trauma perception, previous birth trauma, and birth satisfaction significantly predict post-natal depression in Pakistani women after controlling demographic variables (viz., age, income groups, area, and education).
Materials and methods
Sample
A cross-sectional research design was employed, and a purposive sampling technique was utilized to collect data from 335 women between 42 and 84 days postpartum. Purposive sampling was used to recruit postpartum women from hospitals and clinics who met the inclusion criteria. The purposive sampling method ensured the inclusion of participants with direct experience of childbirth, making them most relevant for assessing birth satisfaction and postnatal depression. Data were gathered from six public and private hospitals and clinics in Punjab, Pakistan, because Punjab is the most populous and socio-culturally diverse province of Pakistan, offering access to a large and varied sample of postpartum women. The availability of healthcare facilities and institutional permissions in this region also made it feasible to collect reliable data within the study’s time and resource constraints. Therefore, Punjab provided a representative and practical context for examining birth satisfaction and postnatal depression. Prior to data collection, formal permission was obtained from the gynecology and obstetrics departments of the respective institutions, and data were collected from hospitals and clinics that granted permission to participate in the study. A written informed consent was secured from all participants. The socio-economic status was measured via income groups (low, high and middle) and was used as a control variable in the regression analysis. Income group was assessed through participants’ self-perceived household economic status (e.g., low, middle, or high income). Fixed income ranges were not used because the study was part of the multi-country INTERSECT project, where substantial differences in currencies, purchasing power, and cost of living across participating countries make direct numeric comparisons inappropriate. Subjective income perception is therefore used as a culturally valid indicator of socioeconomic positioning in cross-national research. The sample included women from lower, middle, and high-income groups, with ages ranging from 18 to 47 years (M = 29.41, SD = 5.32). For analysis, participants were categorized into two age groups: young adults (18–34 years) and middle adults (35–47 years).
Inclusion/exclusion criteria
The women, who reported any chronic condition like; diabetes, hypertension, tuberculosis, arthritis and osteoporosis etc., were not included in the study. In order to ensure that the women in the study did not have any pre-existing psychiatric illnesses, it was confirmed during initial meetings with the participants that they had never been diagnosed with any psychiatric condition like; depression, anxiety and PTSD before child birth.
Measures
Demographic and birth information datasheet
Demographic and Birth Information sheet was prepared to collect the relevant information was included in the set of questionnaires. Following questionnaires were administered on the participants who were fulfilling the inclusion criteria.
Edinburgh postnatal depression scale (EPDS)
In order to measure postnatal depression, the Edinburgh Postnatal Depression Scale (EPDS) was used. The Edinburgh Postnatal Depression Scale (EPDS) is a self-report instrument originally developed by Cox et al. in the UK in 198727,28. Its application has expanded globally, including both English- and non-English-speaking countries, and across diverse economic contexts (low, middle, and high-income nations). The EPDS consists of 10 items that assess emotional experiences over the past seven days (e.g., “I have been able to laugh and see the funny side of things,” “I have been anxious or worried for no good reason,” and “Things have been getting to me”). Responses are rated on a four-point Likert scale ranging from 0 to 3. The scale’s brevity and effectiveness have contributed to its widespread popularity. In its initial British validation study27, the EPDS accurately identified nine out of ten women diagnosed with postnatal depression by a psychiatrist, based on scores exceeding a designated cut-off in a blinded comparison.
The EPDS score ranges from 0 to 30. Scores below 8 suggest depression is unlikely, scores between 9 and 11 indicate possible depression, and scores between 12 and 13 suggest a fairly high likelihood of depression. A score of 14 or higher screens positively for probable depression. Importantly, a positive response (score of 1, 2, or 3) to question 10, which assesses suicidal thoughts, signals a risk of suicidality. Such cases require immediate attention, including discussion with the individual and notification of family members, mental health professionals, or emergency services for further assessment and intervention27.
The EPDS was translated and validated by the authors, before using for the current study via following the backward-forward translation method suggested by Brislin29 and applying exploratory and confirmatory factor analyses. Two factors emerged on the Pakistani sample namely: Factor 1: Depressive symptoms (items 1,2.4,5,6,7,8,9) and Factor 2: Self-harm (items 3 and 10). The Cronbach alpha of the total scale and its subscales (Depressive symptoms and Self-harm) appeared as 0.88, 0.89, and 0.51 respectively in the current study.
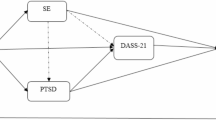
Birth satisfaction Scale-Revised (BSS-R)
Birth satisfaction was measured via Birth Satisfaction Scale-Revised. Birth Satisfaction Scale-Revised (BSS-R) was originally developed by Hollins Martin and Martin30 in the UK. In the current study, Urdu translated version of BSS-R by Zafar et al.31 was used to collect data. The BSS-R is a multi-dimensional ten-item birth satisfaction self-report measure, which is scored on a five-point Likert scale ranging from (1) strongly agree (2), agree (3), neither agree or disagree (4), disagree (5), strongly disagree. Four items (viz., 2,4,7,8) are reverse scored, with three sub-scales (viz., Stress experienced during labor and birth (SE); Quality of care (QC); and Women’s attributes (WA). SE and QC sub-scales each comprise 4-items and the WA sub-scale comprises 2-items. Items 1, 2, 7 and 9 comprise SE subscale (e.g., I came through childbirth virtually unscathed), items 3, 5, 6, 10 comprise QC subscale (e.g., I felt well supported by staff during my labor and birth), and items 4 and 8 comprise WA subscale (e.g., I felt very anxious during my labor and birth). The BSS-R can be used to measure individual subscales, and also accumulated to provide a total score of birth satisfaction, which together make it a perfect tool for both research and clinical purposes32. Several translation and validation studies have revealed that the BSS-R has good to excellent psychometric properties and a transferable theory-informed measurement model across a variety of cultural contexts33,34,35,36. Total score was used to measure overall birth satisfaction and the Cronbach alpha of BSS-R in the present study was = 0.61.
Procedure
The study was formally approved by the Bioethics Committee of GC University Lahore, ensuring adherence to APA ethical research guidelines; The World Medical Association Declaration of Helsinki; The Belmont Report; the International Ethical Guidelines for Health-related Research Involving Humans; and Ethics in Social Science and Humanities. All methods were performed in accordance with the relevant guidelines and regulations. Data collection spanned over two years, from April 27th, 2021, to June 5th, 2023. Participants included postnatal women, who were representing a diverse population.
Prior to initiating data collection, official permissions were obtained from the gynecology and obstetrics departments of the participating healthcare facilities. Written informed consent was then secured from each participant for anonymized participants’ information to be published in this article. Detailed information about the study’s objectives, procedures, and their rights as participants, including the right to withdraw at any stage without any repercussions was provided to the participants.
To determine the required sample size, a priori power analysis was conducted using G*Power software. The sample size was estimated using G*Power 3.1 for hierarchical multiple regression with six predictors, assuming a medium effect size (f² = 0.15), α = 0.05, and power = 0.80, which required approximately 97 participants. However, a larger sample of 350 participants was approached to ensure higher statistical power and the generalizability of the findings.
Based on the analysis, 350 participants were initially targeted for recruitment. Of these, 10 participants declined to participate after reviewing the study materials, citing personal reasons or time constraints. Additionally, five questionnaires were excluded due to incomplete responses.
Data collection was carried out personally by the first, third and fourth authors, ensuring consistency and clarity during the administration of the questionnaires. Most participants completed and returned the questionnaires on the same day they were approached. However, a subset of participants required more time due to personal circumstances or time limitations during their visit and opted to return the completed questionnaires during their next scheduled appointment with their healthcare provider.
To maintain data quality and confidentiality, all completed questionnaires were immediately reviewed for completeness and securely stored. This meticulous approach ensured a final sample size that met the study’s statistical and methodological requirements.
Analyses and results
Descriptive statistics were calculated to examine the average scores on postnatal depression and birth satisfaction in postnatal women in Pakistan.
Results in Table 2 shows that the mean score of the study participants on birth satisfaction = 28.30 lies slightly lower than the median = 30, and their mean score = 15.22 on postnatal depression indicates that on the average women in the study lie in the range of probable depression.
Figure 1 Shows prevalence of depression in the study participants. The pie chart reflects that 36 women (13.73%) reported no indication of depression, 55 women (16.40%) reported possible depression, 32 women (9.6%) reported fairly high likelihood of Depression, and 202 women (60%) reported probable depression.
Correlation analysis
Before running Hierarchical Regression Analysis, Pearson’s correlation analysis was run to assess the intercorrelations between the study variables.
Results in Table 3 display that mother birth complications, infant birth complications and birth trauma perception have significant negative correlation with birth satisfaction (r = − .0.22, − 0.14, − 0.22; p < .001), and age has significant positive correlation with birth satisfaction (r-0.20; p < .01). Whereas, Delivery method and previous birth trauma show non-significant correlations with birth satisfaction. On the other hand, mother birth complications, infant birth complications, birth trauma perception, and previous birth trauma have significant positive correlations with postnatal depression (r = .0.44, 0.31, 0.30, 0.14; p < .0.001) and birth satisfaction shows significant negative correlation with postnatal depression (r = − .0.49; p < .0.01). Delivery method does not show significant correlation with postnatal depression.
Hierarchical regression
In order to test the 2nd hypothesis, hierarchical regression analysis was run to assess the strength of negative birth experiences and birth satisfaction in the prediction of postnatal depression among Pakistani women.
In order to assess the impact of birth satisfaction and negative birth experiences on postnatal depression, the impact of age and education was controlled in the first block that show (Table 4) non- significant impact of demographics on postnatal depression with F (1232) = 1.15, P = .220. In the second block, birth satisfaction, Mother birth complications, Previous birth trauma, Birth trauma perception, Delivery method, and Infant birth complications were entered. Birth satisfaction, mother birth complications, previous birth trauma and birth trauma perception appeared as significant predicters of postnatal depression and accounted for 39% variance in postnatal depression with R2 change = 0.392, F (8326) = 28.25.
Discussion
This study aimed to investigate the relationship between obstetric factors—delivery methods, birth complications, perceived birth trauma, and satisfaction with childbirth—and postnatal depression (PND) among postpartum women in Pakistan. The findings revealed significant correlations among these variables, partially supporting the first hypothesis (see Table 3). Specifically, maternal and infant birth complications, as well as perceptions of birth trauma, were significantly negatively correlated with birth satisfaction, which in turn showed a significant negative correlation with PND. Furthermore, maternal complications, infant complications, perceptions of birth trauma, and previous birth trauma were significantly positively correlated with PND.
For testing the second hypothesis, hierarchical regression analysis, controlling for demographic variables such as age and education, showed that birth satisfaction, maternal complications, previous birth trauma, and perceived birth trauma accounted for a significant portion of the variance in PND (see Table 4). Among these predictors, birth satisfaction emerged as the most salient factor, emphasizing the protective role of positive birth experiences in reducing postpartum psychological distress.
These findings align with existing research. Negative birth experiences, including low levels of birth satisfaction, have been identified as significant predictors of PND in numerous studies21,22,24,25,26. Globally, dissatisfaction with childbirth often arises when women’s psychological and emotional needs are unmet, social support is lacking, and their autonomy is compromised during labor and delivery. In Pakistan, sociocultural norms, such as limited involvement of women in decisions regarding the mode and place of delivery, exacerbate the negative impact of childbirth experiences on mental health23. When women feel disrespected, neglected, or unsupported during childbirth, their risk of developing PND increases significantly. On the other hand, when women experience care, respect, and psychological support during childbirth, their likelihood of developing PND decreases.
Results also indicate that mother complications, previous birth trauma, and birth trauma perception increased the risk of PND. These results are in line with the studies that a higher percentage of women with PND suffered from severe obstetric complications as compared to non-depressed women15,16,21,37,38 demonstrating the fact that traumatic experiences with childbirth play a major role in the development of PPD. Psychologically and physically traumatic childbirth experiences play a substantial negative role in the onset of postnatal depression39. When women subjected to mistreatment, disrespect, abuse, negligence, and violation of human rights by health professionals, it is termed is obstetric violence20. Obstetric violence that was measured as child birth trauma in the current study and it has also been reported to be associated with increased risk for depression in postnatal women17,18,19,40. In Pakistan, where healthcare resources are often constrained, and healthcare professionals may lack training in respectful maternal care, such violations are not uncommon. The implications of obstetric violence extend beyond immediate physical harm to long-term psychological consequences, including postnatal depression.
Implications
The findings have significant implications for researchers, healthcare providers, and policymakers in Pakistan. Gynecologists, obstetricians, and midwives must prioritize the psychological and emotional needs of women during childbirth. Ensuring respect, dignity, and informed consent can significantly enhance birth satisfaction and reduce the risk of PND. Healthcare systems in Pakistan should also address the issue of obstetric violence by implementing policies and training programs that promote respectful maternity care. This includes educating healthcare professionals about the importance of empathy, effective communication, and shared decision-making during childbirth. Social support systems, such as family involvement and peer counseling, should also be strengthened to provide postpartum women with the necessary psychological and emotional support. It is recommended that routine screening for postnatal depression (PND) be integrated into antenatal and postnatal care to enable early identification of women at risk. Healthcare providers should also ensure the provision of psychological support and counseling services as part of comprehensive maternal healthcare. Such preventive measures can promote maternal well-being, improve birth-related experiences, and reduce the long-term psychological impact of postnatal depression.
Limitations and future suggestions
This study makes a valuable contribution to the literature as the first investigation of postnatal depression in Pakistan to examine the predictive strength of negative and traumatic birth experiences. The findings provide a foundation for future research and intervention programs tailored to the Pakistani context. However, there are some limitations. The sample was drawn exclusively from hospitals and clinics in Punjab, as the authors who collected data were based in this region, and data collection was conducted in person. This geographic limitation restricts the generalizability of the findings to other provinces of Pakistan. Future studies should aim to include participants from across the country to ensure a more representative sample. Moreover, participants were selected from specific hospitals and clinics that granted permission that indicate the risk of sampling bias. This limits the representativeness of the sample and may not fully capture the experiences of all postpartum women. Future studies should consider random or stratified sampling to enhance generalizability. Additionally, the data were collected through self-report questionnaires, which may introduce common method variance and social desirability bias. This reliance on self-reported data may therefore limit the objectivity of the findings, and future research could benefit from incorporating multi-method approaches, such as clinical interviews or observer ratings, to enhance validity. Most data were collected during postpartum visits, resulting in an overrepresentation of women who experienced birth complications. Consequently, the findings may not fully capture the perspectives of women with uncomplicated deliveries, potentially limiting the generalizability of the results to the broader population of postpartum women.
Conclusion
This study highlights the significant role of birth satisfaction, maternal complications, previous birth trauma, and perceptions of birth trauma in the development of PND among postpartum women in Pakistan. The findings suggest that providing a secure, respectful, and supportive environment during childbirth may substantially reduce the risk of PND.
Positive childbirth experiences—characterized by care, respect, and fulfillment of psychological needs—appear to serve as protective factors against PND. Conversely, when women’s basic rights are violated, their autonomy is ignored, and their psychosocial needs are unmet, the risk of PND increases. Healthcare systems in Pakistan must prioritize respectful maternal care, ensure informed decision-making, and address obstetric violence to improve maternal mental health outcomes. Future research should focus on expanding geographic representation and exploring the impact of sociocultural factors on childbirth experiences and PND.
Data availability
The corresponding author Prof. Dr Syeda Shahida Batool should be contacted if someone wants data from this study.
References
Department of Health, Government of Western Australia. Edinburgh Postnatal Depression Scale (EPDS): Translated versions – validated (State Perinatal Mental Health Reference Group, 2006).
Husain, N. et al. Treatment of maternal depression in urban slums of Karachi, Pakistan: A randomized controlled trial (RCT) of an integrated maternal psychological and early child development intervention. Asian J Psychiatr. (2017).
Hadi, H. & Hadi, S. Uncovering the concealed part of motherhood: Postpartum depression in mothers. Clin Mother Child Health. 12(1):1–4.https://ecommons.aku.edu/pakistan_fhs_son/74/ (2015).
Rukh, R., Kafeel, H., Naveed, S. & Sarwar, G. Prevalence of postpartum depression in primigravida and multigravida with normal physiological status. RADS J. Pharm. Pharm. Sci. 1, 16–20 (2013).
CloutD & BrownR Marital relationship and attachment predictors of postpartum stress, anxiety, and depression symptoms. J. Consult Clin. Psychol. 35 (3), 322–341. https://doi.org/[insert DOI if available] (2016).
Hahn-Holbrook, J., Cornwell-Hinrichs, T. & Anaya, I. Economic and health predictors of National postpartum depression prevalence: A systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Front. Psychiatry. 8, 248. https://doi.org/10.3389/fpsyt.2017.00248 (2018).
Shorey, S. et al. Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. J. Psychiatr Res. 104, 235–248. https://doi.org/10.1016/j.jpsychires.2018.08.001 (2018).
Gulamani, S. S., Shaikh, K. & Chagani, J. Postpartum depression in Pakistan. Nurs Womens Health. ;17(2):147–152. (2013).
Muhammad, A. Comparison of Postnatal Depression and its Risk Factors in Females with Cesarean Section and Normal Vaginal Delivery [PhD dissertation]. Lahore: The University of Lahore. (2021).
Matsumura, K., Hamazaki, K., Tsuchida, A., Kasamatsu, H. & Inadera, H. Education level and risk of postpartum depression: results from the Japan environment and children’s study (JECS). BMC Psychiatry. 19, 419. https://doi.org/10.1186/s12888-019-2296-6 (2019).
O’Hara, M. W. & Swain, A. M. Rates and risk of postpartum depression—a meta-analysis. Int. Rev. Psychiatry. 8 (1), 37–54 (1996).
Stewart, D. E. et al. Postpartum depression: Literature review of risk factors and interventions. Geneva: World Health Organization. (2003).
Halbreich, U. & Karkun, S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J. Affect. Disord.. 91 (2–3), 97–111. https://doi.org/10.1016/j.jad.2005.12.051 (2006).
Khan, M. M. et al. Frequency of postpartum depression in women attending Fauji Foundation Hospital Peshawar. J. Med. Sci. 11:190–193. https://www.jmedsci.com/index.php/Jmedsci/article/view/205 (2015).
Muneer, A., Minhas, F. A., Nizami, T. U. N., Mujeeb, F. & Usmani, A. T. Frequency and associated factors for postnatal depression. J. Coll. Physicians Surg. Pak.. 19 (4), 236–239 (2009).
Waterstone, M., Wolfe, C., Hooper, R. & Bewley, S. Postnatal morbidity after childbirth and severe obstetric morbidity. BJOG 110 (2), 128–133 (2003).
Silveira, M. F. et al. The association between disrespect and abuse of women during childbirth and postpartum depression: findings from the 2015 Pelotas birth cohort study. J. Affect. Disord.. 256, 441–447. https://doi.org/10.1016/j.jad.2019.06.016 (2019).
Xu, S. et al. Esketamine pretreatment during Cesarean section reduced the incidence of postpartum depression: a randomized controlled trial. BMC Anesthesiol. 24, 20. https://doi.org/10.1186/s12871-023-02398-1 (2024).
Xu, Y. et al. Systematic review and meta-analysis of prevalence and risk factors for psychological birth trauma. Nurs. Res. 74 (2), 123–129. https://doi.org/10.1097/NNR.0000000000000792 (2025).
World Health Organization. The prevention and elimination of disrespect and abuse during facility-based childbirth. Geneva: WHO. http://apps.who.int/iris/bitstream/10665/134588/1/WHO_RHR_14.23_eng.pdf?ua=1&ua=1 (2014).
Yakupova, V. A. & Suarez, A. Postpartum depression and birth experience in Russia. Psychol. Russ. 14 (1), 28–38. https://doi.org/10.11621/pir.2021.0103 (2021).
Nilvér, H., Begley, C. & Berg, M. Measuring women’s childbirth experiences: A systematic review for identification and analysis of validated instruments. BMC Pregnancy Childbirth. 17, 203. https://doi.org/10.1186/s12884-017-1393-6 (2017).
Kalar, M. U. et al. Prevalence and predictors of postnatal depression in mothers of Karachi. Int. J. Collab. Res. Intern. Med. Public Health. 4:830–9 https://www.iomcworld.org/abstract/prevalence-and-predictors-of-postnatal-depression-in-mothers-of-karachi-18631.html. (2012).
Mariño-Narváez, C., Puertas-Gonzales, J. A., Romero-Gonzales, B. & Peralta-Ramirez, M. I. Giving birth during the COVID-19 pandemic: the impact on birth satisfaction and postpartum depression. Int. J. Gynaecol. Obstet. 153 (1), 83–88. https://doi.org/10.1002/ijgo.13565 (2021).
Unsal Atan, Ş. et al. Relation between mothers’ types of labor, birth interventions, birth experiences and postpartum depression: A multicenter follow-up study. Sex. Reprod. Healthc. 18, 13–18. https://doi.org/10.1016/j.srhc.2018.07.002 (2018).
Urbanová, E., Škodová, Z. & Bašková, M. The association between birth satisfaction and the risk of postpartum depression. Int. J. Environ. Res. Public. Health. 18 (19), 10458. https://doi.org/10.3390/ijerph181910458 (2021).
Cox, J. L., Holden, J. M. & Sagovsky, R. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br. J. Psychiatry. 150 (6), 782–786. https://doi.org/10.1192/bjp.150.6.782 (1987).
Cox, J. & Holden, J. Perinatal Psychiatry: Use and Misuse of the Edinburgh Postnatal Depression Scale (Royal College of Psychiatrists, 1994).
Brislin, R. W. Translation and content analysis of oral and written material. In: (eds Triandis, H. C. & Berry, J. W.) Handbook of cross-cultural Psychology: Methodology. Boston: Allyn and Bacon; 389–444. (1980).
Hollins Martin, C. J. & Martin, C. R. Development and psychometric properties of the birth satisfaction Scale-Revised (BSS-R). Midwifery 30 (6), 610–619. https://doi.org/10.1016/j.midw.2013.10.006 (2014).
Zafar, S. et al. Translation and validation of the birth satisfaction Scale-Revised in Urdu for use in Pakistan. Int. J. Childbirth
Martin, C. R. et al. The birth satisfaction Scale - Revised (BSS-R): should the subscale scores or the total score be used? J. Reprod. Infant Psychol. 1–6. https://doi.org/10.1080/02646838.2018.1490498 (2018).
Burduli, E., Barbosa-Leiker, C., Fleming, S., Hollins Martin, C. J. & Martin, C. R. Cross-cultural invariance of the birth satisfaction Scale-Revised (BSS-R): comparing UK and US samples. J. Reprod. Infant Psychol. 35 (3), 248–260. https://doi.org/10.1080/02646838.2017.1310374 (2017).
Goncu Serhatlioglu, S., Karahan, N., Hollins Martin, C. J. & Martin, C. R. Construct and content validity of the Turkish birth satisfaction Scale-Revised (T-BSS-R). J. Reprod. Infant Psychol. 1–11. https://doi.org/10.1080/02646838.2018.1443322 (2018).
Nasiri, S., Kariman, N. & Ozgoli, G. Psychometric properties of the Iranian version of birth satisfaction Scale-Revised. J. Res. Med. Sci. 25 (1), 90. https://doi.org/10.4103/jrms.JRMS_248_19 (2020).
Romero-Gonzalez, B. et al. Spanish validation and factor structure of the birth satisfaction Scale-Revised (BSS-R). Midwifery 70, 31–37. https://doi.org/10.1016/j.midw.2018.12.009 (2019).
Bell, A. F. & Andersson, E. The birth experience and women’s postnatal depression: A systematic review. Midwifery 39, 112–123. https://doi.org/10.1016/j.midw.2016.04.014 (2016).
Gosselin, P., Chabot, K., Béland, M., Goulet-Gervais, L. & Morin, A. J. Fear of childbirth among nulliparous women: relations with pain during delivery, post-traumatic stress symptoms, and postpartum depressive symptoms. Encephale 42 (2), 191–196. https://doi.org/10.1016/j.encep.2016.01.007 (2016).
Yildiz, P. D., Ayers, S. & Phillips, L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. J. Affect. Disord. 208, 634–645. https://doi.org/10.1016/j.jad.2016.10.009 (2017).
Souza, É. L. et al. Factors influencing the mode of delivery in Brazil. Rev. Med. (São Paulo). 101 (5), e172947 (2022).
Acknowledgements
This research was conducted as part of the International Survey of Childbirth-Related Trauma (INTERSECT, www.intersectstudy.org).
Author information
Authors and Affiliations
Contributions
S .S.B: design of the work, data acquisition, analysis, interpretation of data, drafted the manuscriptS.K.C: Analysis and final draft of the manuscriptS.A.B: Data acquisition, interpretation, proof read the manuscriptR.B: Data acquisition, data entry, analysisS.A: Design of work, proofread final draftW.R: Design of work, Proofread final draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Bioethics Committee of GC University Lahore vide certificate No. (GCU/IIIB/138). All participants provided informed consent prior to interview (Detailed information has been provided in procedure). There are no potentially harmful activities involved in the study.
Consent for publication
The Participants gave consent for the publication of their provided information.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Batool, S.S., Chatrath, S.k., Batool, S.A. et al. Interplay of traumatic birth experiences and postnatal depression in Pakistani women. Sci Rep 15, 43165 (2025). https://doi.org/10.1038/s41598-025-27209-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-27209-0