Abstract
The objective of this study was to investigate the impact of the thoracolumbar kyphotic Cobb angle on surgical prognosis following percutaneous kyphoplasty (PKP) in patients with thoracolumbar osteoporotic vertebral compression fractures (OVCF). We collected clinical data of 204 patients with OVCF of the thoracolumbar segment and analyzed them retrospectively. All patients were divided into four groups based on their postoperative thoracolumbar kyphotic Cobb angle. The basic clinical data, visual analog scale (VAS) score, and Oswestry disability index (ODI) score were subjected to statistical analysis and comparison among the groups. There was no significant difference in the general information of the patients in each group. In the post-operative period, patients in Groups A and B demonstrated significant reductions in VAS and ODI scores. The follow-up results at all time points were superior to those observed in Groups B and C. Patients in Group A exhibited the best ODI scores, which essentially recovered to the optimal state one month after surgery. The present study demonstrated a correlation between the thoracolumbar kyphotic Cobb angle and the prognosis of PKP surgery. Furthermore, the 0–5° thoracolumbar kyphotic Cobb angle was found to facilitate more rapid and superior patient recovery.
Similar content being viewed by others
Introduction
Thoracolumbar fractures represent a highly prevalent form of spinal injury, constituting a substantial proportion of all such injuries1. Indeed, research has shown that more than 50% of spinal fractures occur in the thoracolumbar region2,3. Thoracolumbar fractures have been shown to have a significant impact on patients’ lives and health, causing severe pain and functional impairment4. In severe cases, neurological dysfunction, including paraplegia, can result. This has a considerable impact on the patient’s quality of life and can impose a significant burden on the family and wider society5,6.
From an anatomical perspective, the thoracolumbar segment is conventionally defined as the region extending from the 10th thoracic vertebra (T10) to the second lumbar vertebra (L2)7. The region under consideration is distinguished by its role as the point at which the two physiologic curves of the thoracic and lumbar spine converge. It exhibits anatomical characteristics that are distinct from those of other regions8. The thoracic spine is connected to the sternum by the ribs and forms the thorax, which exhibits relatively low mobility and high stability, while the lumbar spine bears the majority of the body weight and possesses high mobility and flexibility9. The thoracolumbar segment is located in the transition region between these two distinct mechanical environments and is subject to greater stress10. Patients suffering from osteoporosis are more prone to fractures in the thoracolumbar region11.
Osteoporotic vertebral compression fractures (OVCF) have become a prevalent condition among middle-aged and elderly individuals12, and percutaneous kyphoplasty (PKP) has been shown to expedite pain relief and facilitate early mobilisation13. PKP has been demonstrated to have excellent therapeutic effects and has been widely used in clinical practice14. A significant number of scholars have conducted in-depth studies on the factors affecting the recovery of PKP15,16; however, the effect of thoracolumbar kyphotic cobb angle on the prognosis of PKP has rarely been studied. The thoracolumbar kyphotic Cobb angle is defined as the angle between the plumb line of the superior margin of the T10 vertebra and the plumb line of the inferior margin of the L2 vertebra (see Fig. 1a). The thoracolumbar kyphotic Cobb angle is a reflection of the curvature pattern of the thoracolumbar segment of the spine, a factor which is of great importance to the patient’s postoperative rehabilitation. A substantial body of research has indicated that spinal alignment is a critical factor in improving spinal health17,18,19. Consequently, the present study hypothesises that the thoracolumbar kyphotic Cobb angle is a significant factor influencing the prognosis of patients undergoing PKP surgery. In order to ascertain the appropriate thoracolumbar kyphotic Cobb angle, clinical data from 204 patients with OVCF of the thoracolumbar segment was collected and a retrospective analysis conducted. The objective of this study is to explore the impact of thoracolumbar vertebral kyphotic Cobb angle on the prognosis of PKP, thereby providing additional reference for clinical practitioners.
The thoracolumbar segment’s X-ray pictures before and after surgery. (a, b) Preoperative lateral and orthostatic radiographs of the thoracolumbar segment. (c, d) Postoperative lateral and orthostatic radiographs of the thoracolumbar segment. (T10: the 10th thoracic vertebra; L2: the Second lumbar vertebra; The thoracolumbar kyphotic Cobb angle is defined as the angle between the plumb line of the superior margin of the T10 vertebra and the plumb line of the inferior margin of the L2 vertebra.)
Methods
Patients
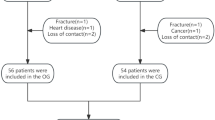
A total of 204 patients with OVCF of the thoracolumbar segment were selected for inclusion in the study. This selection was made from January 2022 to December 2023 at the Suzhou Hospital of Anhui Medical University. All patients were divided into four groups based on their postoperative thoracolumbar kyphotic Cobb angle. The thoracolumbar kyphotic Cobb angles for Group A are in the range of 0–5°, for Group B they are in the range of 5–10°, for Group C they are in the range of 10–15°, and for Group D they are in the range of 15–20°. There were 36 patients in Group A, 50 patients in Group B, 73 patients in Group C and 45 patients in Group D. Comparison of the preoperative general information of all patients is shown in Table 1, and the differences in the preoperative general information of patients in each group were not statistically significant. The study was approved by the Ethics Committee of Suzhou Hospital of Anhui Medical University (Ethical Review Comment No.: A2024014). The study was performed in accordance with the Declaration of Helsinki. All patients were informed about the study and signed an informed consent form.
Inclusion criteria: (1) Patients met the criteria for osteoporosis by the DXA method; (2) Injured vertebrae were in the range of T10-L2. (3) Patients’ follow-up data were complete.
Exclusion criteria: (1) Posterior vertebral wall rupture or pedicle fracture; (2) Spinal cord or nerve root compression; (3) pathologic fracture caused by metastatic tumors; (4) Patients with missing follow-up data.
Surgical methods
The patient was then placed in a prone position, and the optimal skin entry point was determined by C-arm X-ray, according to the position of the pedicle. The patient was routinely sterilised, and the surgical field was covered with a sterile patch. The local infiltration anaesthesia was induced using 1:1 diluted lidocaine. The puncture needle was inserted 2–3 mm into the vertebral body in the direction of the anterior inferior border of the injured vertebrae under X-ray monitoring. Thereafter, the core of the puncture needle was withdrawn and the guide needle was inserted to reach the anterior inferior border of the vertebral body. The outer sleeve of the puncture needle is then removed, after which the dilatation trocar and the working trocar are inserted along the guide needle. This is done so that the anterior end of the working trocar is located 2–3 mm anterior to the posterior border of the vertebral body at the anterior cortex. The guide needle is then removed and a fine drill is inserted through the working trocar to reach the anterior inferior border of the vertebral body. Remove the drill and take a small amount of bone tissue for pathologic examination. The expandable balloon is inserted, a syringe is attached, contrast medium is injected into the balloon, and the balloon is expanded with pressure. C-arm X-ray was utilised to meticulously monitor the balloon expansion and vertebrae fracture reduction. Once the vertebrae were adequately reduced or the balloon reached the cortex surrounding the vertebrae, push-in was halted, and the pressure was not more than 300 pounds per square inch (psi). The contrast medium was withdrawn and the balloon was removed. The same method was used to complete the contralateral operation. Polymethylmethacrylate bone cement was prepared and injected into the bone cement injection tube. Bone cement in the liquid stage was injected into the intravertebral cavity through the working channel with low pressure, and the appropriate amount of bone cement was injected into both sides concurrently. C-arm X-ray was utilised to ensure adequate filling of the bone cement within the injured vertebrae, and to ascertain the absence of leakage. The cement pusher is then tamped down until the cement is fully cured, and then withdrawn to avoid backflow along the working channel. The skin puncture point must be sutured and covered with a sterile dressing. Postoperative vital signs were monitored for the patients. All patients underwent surgery performed by the same surgeon. The pre- and post-operative radiographs are shown in Fig. 1.
Evaluation indicators
The number of days of hospitalisation, the preoperative thoracolumbar kyphotic Cobb angle and the length of surgery were recorded for the purpose of comparing the perioperative data of each group. The visual analogue scale (VAS) and Oswestry disability index (ODI) scores were used to evaluate the patients’ clinical recovery. Thoracolumbar segment X-ray examinations were performed preoperatively and postoperatively to record the thoracolumbar kyphotic Cobb angle. All patients were regularly followed up for at least six months. The measurement of the thoracolumbar kyphotic Cobb angle is shown in Fig. 1a. The follow-ups and related scores for all patients were conducted by the same person.
Statistical analysis
All data analysis and graphical production for this study were conducted using GraphPad Prism 9.4.1 software. The quantitative data were subjected to one-way ANOVA analysis, while the qualitative data were analysed using the X2 test. The repeated measures data were analysed using two-way ANOVA. P < 0.05 was deemed to indicate a statistically significant difference.
Results
We statistically compared the perioperative data of patients in each group, and the results are shown in Fig. 2. This figure shows that there were no significant differences in the number of hospitalisation days (p = 0.4416), the preoperative thoracolumbar kyphotic Cobb angle (p = 0.3757) or the duration of surgery (p = 0.2922) among the groups. The statistical results are presented in Table 2.
The VAS and ODI scores of patients in each group were tallied at varying time points to facilitate a comparative analysis of the postoperative rehabilitation effects of each group. The results of the comparison of VAS and ODI scores of patients in each group are shown in Fig. 3. There was no significant difference in the VAS scores and ODI scores of patients in each group prior to surgery. Postoperatively, a gradual decrease in the VAS and ODI scores was observed in patients from each group. However, at one month and three months postoperatively, the VAS scores of groups A and B were lower than those of groups C and D. At six months postoperatively, patients in group A exhibited significantly lower VAS scores in comparison to those in the other three groups (see Fig. 3a–c). As demonstrated in Fig. 3d–f, there was no significant difference in the ODI scores of patients within each group at the preoperative. However, in the postoperative period, a gradual decline in ODI scores was observed over time. One month and three months postoperative, patients in Group A exhibited the lowest ODI scores, with no significant differences observed between Groups C and D. At the six-month follow-up, ODI scores for patients in Groups A and B were lower than those in Groups C and D. These findings suggest that patients in Group A demonstrated the most optimal postoperative recovery during the follow-up period, exhibiting faster recovery times. The statistical results of VAS and ODI scores of patients in each group are shown in Table 3. The mean differences and 95% confidence intervals for all data can be found in the supplementary materials.
Discussion
Thoracolumbar compression fracture represents a prevalent complication of osteoporosis, with a notable increase in its prevalence observed in recent years20. The principal manifestations of OVCF are pain and activity limitation21. In the contemporary medical context, patients diagnosed with OVCF are frequently subjected to surgical interventions. PKP, recognised as the prevailing surgical modality, constitutes a minimally invasive surgical technique that entails percutaneous puncture through the pedicle or lateral approach to the compromised vertebrae22. The objective of this procedure is to introduce cement into the fractured vertebrae, thereby achieving stabilisation, restoration of bone hardness and mechanical strength, and alleviation of pain23. However, it is important to note that there are significant individual differences in surgical outcomes, which are influenced by a variety of factors, such as the degree of fracture, recovery of vertebral height, and cement dispersion4,24,25,26.
The present study concentrated on the impact of the thoracolumbar kyphotic Cobb angle on the surgical prognosis of PKP. Previous studies have focused on the localization of the diseased vertebrae. However, the overall physiologic curvature of the thoracolumbar segment, which is the junction of the physiologic kyphosis of the thoracic spine and the physiologic anterior kyphosis of the lumbar spine, is critical for spinal stability27,28. In the present study, the overall physiologic curvature of the thoracolumbar vertebrae was responded to by the thoracolumbar kyphotic Cobb angle. The findings of this study demonstrated that the surgical prognosis of Groups A and B were superior to that of Groups C and D, suggesting that a reduced thoracolumbar kyphotic Cobb angle was more conducive to the prognosis of PKP surgery in patients with OVCF. The findings of this study indicate that, in performing PKP surgery on patients, our focus should extend beyond the localized condition of the diseased vertebrae to encompass a holistic assessment of the thoracolumbar vertebral, with the objective of ensuring that the thoracolumbar kyphotic Cobb angle is restored to a range that is deemed to be within an acceptable limit. The thoracolumbar vertebrae of the spine exhibit the appropriate physiological curvature, thus ensuring equilibrium in the forces exerted on the vertebrae and reducing the likelihood of postoperative complications29. A comparison of VAS scores between Group A and Group B patients in the first and third postoperative months with those in Group B revealed no significant difference. However, a significant difference was observed in VAS scores between Group A and Group B patients in the sixth postoperative month, indicating that Group A patients experienced more pronounced postoperative pain relief. Furthermore, the ODI scores of patients in Group A exhibited superiority over those of Group B during the first and third postoperative months following surgery. However, no significant discrepancy in ODI scores was observed between the two groups in the sixth month post-surgery. This finding signifies that the functional recovery of patients in Group A was more expeditious than that of patients in Group B. This phenomenon was attributed to the presence of a more optimal physiological curvature in the thoracolumbar region of patients in Group A. This phenomenon was ascribed to the more moderate physiologic curvature of the thoracolumbar segment observed in Group A patients.
It has been established during surgical procedures that certain vertebral heights are challenging to fully restore. It is imperative to note that if the restoration of vertebral height is pursued excessively, the operation time will be prolonged and the risk of cement leakage will be increased. These factors, in turn, may result in an increased number of surgical risks for patients30. For instance, certain vertebrae exhibit an absence of wedge-shaped compression, instead manifesting near-horizontal compression. Consequently, complete restoration of vertebral height frequently poses a significant challenge. At this juncture, priority should be accorded to ensuring the physiological curvature of the patient’s thoracolumbar segment. It is posited by virtue of our prior experiential knowledge that, under the premise of ensuring the physiological curvature of the thoracolumbar vertebrae, even in the case of an inability to restore the height of the injured vertebrae to its pre-injury state, the patients can still obtain a satisfactory prognosis following surgical intervention.
The findings of this study indicate that a thoracolumbar kyphosis Cobb angle of 0–5° is more conducive to patient recovery. This phenomenon may be attributed to the fact that a more optimal Cobb angle facilitates enhanced spinal loading equilibrium. Consequently, during PKP surgery, it is imperative to meticulously restore the patient’s intrinsic thoracolumbar curvature. Maintaining the Cobb angle of thoracolumbar kyphosis within the 0–5° range has been demonstrated to engender superior patient outcomes.
Moreover, the study exhibits certain deficiencies, including a limited sample size, an inadequate grouping strategy, and an insufficient duration of follow-up. In future work, the sample size will be expanded and the duration of follow-up will be increased. Furthermore, more appropriate grouping methodologies will be explored, and more robust scientific evidence will be provided for determining optimal thoracolumbar Cobb angles. Furthermore, the study did not adequately account for confounding factors such as bone density and bone cement dosage, which may introduce certain biases into the findings. Subsequent phases of the study will involve multicentre randomised controlled trials and biomechanical modelling studies, with the objective of further validating the reliability of these results.
Conclusion
In this study, the ODI and VAS scores for all patient groups progressively decreased over time following surgery, indicating that postoperative outcomes improved steadily for all groups. However, a significant divergence in ODI and VAS scores was observed between the groups at the same time points. Statistical analysis revealed that patients in Group A demonstrated faster recovery, suggesting that a thoracolumbar Cobb angle of 0–5° is more conducive to postoperative rehabilitation. The results of this study provide a new reference for a wide range of clinicians.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Kong, L. & Wang, W. Thoracolumbar fractures. Eur. Spine J. 16, 1737; author reply 1738, https://doi.org/10.1007/s00586-007-0354-6 (2007).
Sun, L. L. et al. Clinical characteristics and intraoperative reduction technique of thoracolumbar fractures combined with posterior column injury. J. Coll. Phys. Surg. Pak. 33, 1188–1193. https://doi.org/10.29271/jcpsp.2023.10.1188 (2023).
Wood, K. B., Li, W., Lebl, D. R. & Ploumis, A. Management of thoracolumbar spine fractures. Spine J. 14, 145–164. https://doi.org/10.1016/j.spinee.2012.10.041 (2014).
Yang, X. G. et al. Incidence and prognostic factors of residual back pain in patients treated for osteoporotic vertebral compression fractures: A systematic review and meta-analysis. Eur. Spine J. 33, 4521–4537. https://doi.org/10.1007/s00586-024-08426-z (2024).
Lu, W. et al. A pain that is easily overlooked: Referred pain caused by OVCF. J. Pain Res. 16, 961–971. https://doi.org/10.2147/JPR.S375966 (2023).
Li, J. et al. Modified pedicle subtraction osteotomy for osteoporotic vertebral compression fractures: A retrospective study of 104 patients. Eur. Spine J. 33, 3275–3283. https://doi.org/10.1007/s00586-024-08335-1 (2024).
Prajapati, H. P. & Kumar, R. Thoracolumbar fracture classification: Evolution, merits, demerits, updates, and concept of stability. Br. J. Neurosurg. 35, 92–97. https://doi.org/10.1080/02688697.2020.1777256 (2021).
Guo, L. X. & Li, W. J. A biomechanical investigation of thoracolumbar burst fracture under vertical impact loads using finite element method. Clin. Biomech. (Bristol) 68, 29–36. https://doi.org/10.1016/j.clinbiomech.2019.05.018 (2019).
Ruf, M. et al. The effect of posterior compression of the facet joints for initial stability and sagittal profile in the treatment of thoracolumbar fractures: A biomechanical study. Eur. Spine J. 31, 28–36. https://doi.org/10.1007/s00586-021-07034-5 (2022).
Wehner, C., Wehner, C., Schwameder, H. & Schobersberger, W. Thoracolumbar rotation during Tai Chi movements-a biomechanical analysis of the entire Peking style routine. Front. Sports Act Living 4, 834355. https://doi.org/10.3389/fspor.2022.834355 (2022).
Li, J. et al. Open surgical treatments of osteoporotic vertebral compression fractures. Orthop. Surg. 15, 2743–2748. https://doi.org/10.1111/os.13822 (2023).
Wen, X. et al. Clinical evaluation of unilateral vertebroplasty for OVCF. Emerg. Med. Int. 2022, 2037185. https://doi.org/10.1155/2022/2037185 (2022).
Otsuka, R. et al. Independent living 1 year after balloon kyphoplasty for osteoporotic vertebral compression fracture. World Neurosurg. 155, e646–e654. https://doi.org/10.1016/j.wneu.2021.08.116 (2021).
Al Taha, K. et al. Multidisciplinary and coordinated management of osteoporotic vertebral compression fractures: Current state of the art. J Clin Med https://doi.org/10.3390/jcm13040930 (2024).
Yu, D. et al. Treatment of elderly patients with acute symptomatic OVCF: A study of comparison of conservative treatment and percutaneous kyphoplasty. Front. Surg. 9, 942195. https://doi.org/10.3389/fsurg.2022.942195 (2022).
Zhou, T., Lin, H., Wang, H., Chen, X. & He, F. Comparative study on the biomechanics between improved PVP and traditional PKP in the treatment of vertebral peripheral wall damage-type OVCF. Exp. Ther. Med. 14, 575–580. https://doi.org/10.3892/etm.2017.4542 (2017).
Daher, M. et al. The importance of alignment in the management of thoracolumbar trauma. World Neurosurg. 192, 109–116. https://doi.org/10.1016/j.wneu.2024.09.058 (2024).
Saini, Y., Rai, A. & Sen, S. Relationship between sleep posture and low back pain: A systematic review. Musculoskelet. Care 23, e70114. https://doi.org/10.1002/msc.70114 (2025).
Daniels, A. H. et al. Segmental sagittal alignment in lumbar spinal fusion: A review of evidence-based evaluation of preoperative measurement, surgical planning, intraoperative execution, and postoperative evaluation. Oper Neurosurg. 27, 533–548. https://doi.org/10.1227/ons.0000000000001179 (2024).
Liawrungrueang, W. et al. Osteoporotic vertebral compression fracture (OVCF) detection using artificial neural networks model based on the AO spine-DGOU osteoporotic fracture classification system. N. Am. Spine Soc. J. 19, 100515. https://doi.org/10.1016/j.xnsj.2024.100515 (2024).
Liu, Y., Liu, J., Suvithayasiri, S., Han, I. & Kim, J. S. Comparative efficacy of surgical interventions for osteoporotic vertebral compression fractures: A systematic review and network meta-analysis. Neurospine 20, 1142–1158. https://doi.org/10.14245/ns.2346996.498 (2023).
Ning, L. et al. Correlation analysis between basic diseases and subsequent vertebral fractures after percutaneous kyphoplasty (PKP) for osteoporotic vertebral compression fractures. Pain Phys. 24, E803–E810 (2021).
He, Z. et al. Bone cements for percutaneous vertebroplasty and balloon kyphoplasty: Current status and future developments. J. Orthop. Translat. 3, 1–11. https://doi.org/10.1016/j.jot.2014.11.002 (2015).
You, Z., Wu, K., Jiang, Y. & Chen, J. Effect of vertebral kyphoplasty versus vertebroplasty on pain and indicators of imaging parameters of the injured vertebrae in patients with osteoporotic vertebral compression fractures: A meta-analysis. J. Orthop. Surg. Res. 20, 199. https://doi.org/10.1186/s13018-025-05621-6 (2025).
Hwang, S. H. et al. What are the risk factors for a second osteoporotic vertebral compression fracture?. Spine J. 23, 1586–1592. https://doi.org/10.1016/j.spinee.2023.07.010 (2023).
Sun, K. et al. Lower psoas mass indicates worse prognosis in percutaneous vertebroplasty-treated osteoporotic vertebral compression fracture. Sci. Rep. 14, 13880. https://doi.org/10.1038/s41598-024-64626-z (2024).
Li, Y., Shen, Z., Huang, M. & Wang, X. Stepwise resection of the posterior ligamentous complex for stability of a thoracolumbar compression fracture: An in vitro biomechanical investigation. Medicine (Baltimore) 96, e7873. https://doi.org/10.1097/MD.0000000000007873 (2017).
Wu, C. C. et al. Biomechanical role of the thoracolumbar ligaments of the posterior ligamentous complex: A finite element study. World Neurosurg. 112, e125–e133. https://doi.org/10.1016/j.wneu.2017.12.171 (2018).
Pishnamaz, M. et al. Muscular changes after minimally invasive versus open spinal stabilization of thoracolumbar fractures: A literature review. J. Musculoskelet. Neuronal Interact. 18, 62–70 (2018).
Dai, C., Liang, G., Zhang, Y., Dong, Y. & Zhou, X. Risk factors of vertebral re-fracture after PVP or PKP for osteoporotic vertebral compression fractures, especially in Eastern Asia: A systematic review and meta-analysis. J. Orthop. Surg. Res. 17, 161. https://doi.org/10.1186/s13018-022-03038-z (2022).
Acknowledgements
We would like to express our sincere appreciation to all the patients who participated in this study.
Funding
The present study was supported by the University Research Fund of Anhui Medical University (Grant no.: 2023xkj074).
Author information
Authors and Affiliations
Contributions
All the authors contributed significantly. PY and XG contributed equally to this work. Conception and design of the experiments and surgery and drafting of the article: PY, XG and ZY; statistical analysis: PY; data collection: XG; writing–original draft preparation: QS and YW; writing–review and editing: ZY. All the authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yuan, P., Ge, X., Shi, Q. et al. Influence of thoracolumbar kyphotic Cobb angle on prognosis after PKP surgery. Sci Rep 15, 44293 (2025). https://doi.org/10.1038/s41598-025-27970-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-27970-2