Abstract
To examine the effect of the Integrated Theory of Health Behavior Change (ITHBC) model on self-efficacy, adherence, and rehabilitation outcomes in pelvic floor muscle training among postpartum women. This study recruited primiparas who underwent vaginal delivery at five medical institutions in China between January 2020 and January 2025. Participants were randomly assigned to either the ITHBC nursing model combined with conventional care group (observation group) or the conventional care group (control group). Outcomes included compliance with pelvic floor muscle training, self-efficacy, pelvic floor function, muscle strength, surface electromyography, ultrasound parameters, quality of life, and nursing satisfaction. The observation group showed better performance than the control group in terms of compliance, self-efficacy, and nursing satisfaction. Statistically significant differences were observed in pelvic floor function and quality of life pre- and post-intervention, with the observation group outperforming the control group post-intervention. For pelvic floor muscle strength, statistically significant changes occurred pre- and post-intervention; however, no significant difference was found in type I muscle fiber fatigue degree between groups. Surface electromyography showed significant improvements pre- and post-intervention, with the observation group performing better across most indicators except endurance contraction variability. Ultrasound parameters revealed no significant differences in bladder detrusor muscle thickness, residual urine volume, or bladder neck initial position but showed significant differences in other parameters, with the observation group performing better overall except for the right anal angle. The ITHBC model shows promise for improving adherence and short-term pelvic floor function, but further validation in diverse populations is needed.
Clinical Trial Number: www.chictr.org.cn, ID: ChiCTR2300070607. Registered on 18/4/2023.
Similar content being viewed by others
Introduction
In the female physiological framework, damage to pelvic floor tissues can lead to functional disorders affecting reproductive organs, urinary tract, and anus, resulting in pelvic floor dysfunction. This disrupts daily life, work routines, and sexual intimacy, impacting both physical and mental health1,2,3. Pregnancy and childbirth are key risk factors for pelvic floor dysfunction4,5,6, making postpartum pelvic floor rehabilitation crucial in preventing these issues7. Central to this rehabilitation is restoring pelvic floor muscle function, which research shows can be effectively achieved through biofeedback electrical stimulation combined with pelvic floor muscle training (PFMT)8. Success in PFMT depends on adherence, which is closely linked to self-efficacy, which is defined as the confidence to carry out the courses of action necessary to accomplish desired goals9,10. However, limited awareness of pelvic floor dysfunction, insufficient social support, and negative emotions often reduce compliance, hindering effective rehabilitation11. Therefore, an intervention model that enhances self-efficacy and improves adherence to PFMT is essential.
The Integrated Theory of Health Behavior Change (ITHBC), proposed by American nursing expert Ryan, is a patient-centered nursing management model that enhances self-management skills through knowledge, beliefs, and social support12. By integrating principles from various health education theories—such as patient-centered care, health behavior change, self-regulation, and social cognition—ITHBC provides a comprehensive framework for promoting healthier lifestyles13. It advocates for multifaceted interventions: delivering tailored knowledge, strengthening self-management abilities, enhancing personal resilience, and expanding social support networks. These strategies help individuals reshape health-related habits and achieve sustainable behavioral changes14. In clinical practice, ITHBC has been effectively applied to manage conditions like type 2 diabetes15 and spinal cord injury16. Given the effect of ITHBC on deepening the understanding of patients about their conditions and improving their objective initiative and self-care management behaviors, it is reasonable to believe that ITHBC could enhance the adherence of PFMT, thereby leading to favorable clinical outcomes. However, no work has been conducted to explore the role of ITHBC in pelvic floor muscle training (PFMT). This study evaluates the compliance and efficacy of an ITHBC-based nursing model in promoting pelvic floor muscle exercises among primiparas after vaginal delivery. Results from this study showed that early intervention with ITHBC-based comprehensive rehabilitation significantly improves pelvic floor muscle strength, reduces fatigue, enhances self-efficacy and compliance, and promotes recovery. These findings support further research into ITHBC as a component of postpartum rehabilitation programs.
Data and methods
Clinical information
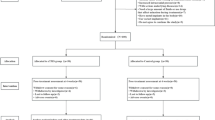
This trials has been registered with www.chictr.org.cn with a number of ChiCTR2300070607 (Registered on 18 April 2023). There was no change to trial methods occurred post-commencement.This study recruited primiparas who underwent vaginal deliveries at five medical institutions in China between January 2020 and January 2025. All participants received comprehensive diagnosis, treatment, and follow-up within their respective hospitals. Informed consent was obtained from all participants, per the Declaration of Helsinki. After signing informed consent forms, participants were randomly assigned to either the ITHBC nursing model combined with conventional care (observation group) or conventional care alone (control group). Subjects who were lost to follow-up or voluntarily withdrew from the study during its progression were respectfully excluded from the analysis. Due to the nature of the comparative study on the effects of distinct intervention, it is not feasible to blind participants. A single-blind test will be conducted, where only the evaluators will be blinded. Our well-trained researchers will use a randomization table to divide participants into a control group and an intervention group, in order to compare the results before and after the intervention. Ultimately, the observation group comprised 263 cases, while the control group encompassed 374 cases.
Inclusion criteria
(1)Primiparas experiencing a singleton pregnancy; (2)Pregnant women who underwent vaginal delivery; (3)Individuals with no history of pelvic floor dysfunction prior to childbirth; (4)Possessing intact cognitive, communicative, and interactive abilities; (5)Having not received any treatments that could influence the trial prior to enrollment; (6)With fully documented clinical data, including comprehensive and accurate symptom records, physical examinations, and auxiliary diagnostic evaluations; (7)Willingly signed the informed consent form, consenting to participate in clinical data research and subsequent follow-up observations.
Exclusion criteria
(1)A history of pelvic floor dysfunction prior to pregnancy; (2)Deliveries involving twin or multiple pregnancies; (3)Women who have given birth to multiple children; (4)Pregnant women who underwent cesarean delivery; (5)Individuals incapable of self-care and unable to perform pelvic floor muscle training; (6)The history of diseases or surgeries that may compromise pelvic floor muscle function; (7)Those with impaired consciousness, cognitive deficits, or an inability to communicate effectively; (8)A history of infectious diseases during the prenatal period; (9)Contraindications for pelvic floor muscle training; (10)Accompanied by neurological conditions like spinal cord injury or cerebral infarction, which can impact the functioning of pelvic floor muscles; (11) Coexisting injuries or functional impairments in other vital organs; (12) Incomplete clinical data or recording errors during the research period.
This study followed the ethical guidelines set forth in the 2013 Declaration of Helsinki and received approval from the appropriate institutional ethics committee (YYLL20240130-YNXM-LL-01–2.0.0).The CONSORT guidelines for the clinical trial research process are provided, and the CONSORT flowchart, CONSORT checklist and trial study protocol are included in the supplementary materials. All participants and their families provided informed consent voluntarily, demonstrating a comprehensive understanding of the study procedures. Detailed data are presented in Table 1 (Baseline demographic and clinical indicators of patients).
Intervention method
Pelvic floor rehabilitation treatment
Training for pelvic floor muscles
① Exercises for Contracting the Pelvic Floor: Prior to training, the new mother must learn to accurately locate her pelvic floor muscles. She should then take a deep breath, contract her pelvic floor muscles while holding for 5 s, and subsequently exhale slowly to release the tension. Perform 10–15 repetitions per set, completing 3–4 sets daily. ② Abdominal Breathing Technique: Lie on a bed or yoga mat with knees bent and feet flat on the floor. Rest your hands on your abdomen, inhale deeply to expand your belly while simultaneously tightening your pelvic floor muscles, and then exhale slowly to contract your abdomen and relax your pelvic floor muscles. Perform 10–15 repetitions per set, completing 3 sets daily. ③ Kegel Exercise: Lie on a bed or yoga mat with knees bent and feet grounded. Tighten your pelvic floor muscles, lift your hips to form a 90° angle with the ground, and hold for 5 s. Gently lower your hips and relax your muscles. Perform 10–15 repetitions per set, completing 3 sets daily. The treatment commenced 12 weeks post-delivery, which is chosen according to a previous study17. (2) Biofeedback Electrical Stimulation: ① Preparation Phase: Assess the parturient’s physical condition, delivery process, and postpartum recovery. Develop an individualized biofeedback electrical stimulation plan based on these findings. ② Position Adjustment: Have the parturient lie on her side with her body relaxed to ensure optimal results. ③ Probe Insertion: Gently insert the probe into the vagina, ensuring full contact with the vaginal wall. Respect the parturient’s privacy and comfort throughout this process. ④ Intensity Adjustment: Use pulsed radio waves to stimulate vaginal muscles. Start at a low intensity and gradually increase based on the parturient’s tolerance, monitoring her reactions closely. ⑤ Treatment Duration and Frequency: Conduct 30-minute sessions three times per week for six weeks, starting 42 days post-delivery. ⑥ Final Evaluation: Evaluate the therapy’s effectiveness after completion.
Grouping and intervention plan
The intervention period aligned with pelvic floor rehabilitation treatment, starting post-delivery and lasting 12 weeks.
Control group
Conventional pelvic floor rehabilitation treatment and nursing intervention methods were implemented. (1) Psychological Intervention: provide routine communication with patients and routine counseling to address their questions. (2) Health Education and Guidance: providide routine education to patients and families about pelvic floor muscle training (PFMT), abdominal breathing, rehabilitation procedures, and treatment precautions. Adjust electrical stimulation intensity based on the parturient’s tolerance and sensation, enabling independent instrument-guided treatment. Advise suspending treatment during menstruation and explain possible post-treatment conditions like lochia or bruising to reduce fears. (3) Basic Intervention: Encourage regular urination, conscious pelvic floor muscle contraction before exertion or coughing, avoidance of sexual activity during treatment, and refraining from strenuous exercise or fatigue for optimal recovery. (4) Dietary Guidance: Promote a diet rich in fresh fruits, vegetables, high-protein, and high-vitamin foods while avoiding spicy or stimulating foods, smoking, alcohol, coffee, and strong tea. Discourage prolonged squatting or sitting to prevent increased abdominal pressure.
Observation group
The pelvic floor muscle rehabilitation treatment and nursing intervention program based on the Integrated Theory of Health Behavior Change (ITHBC) was implemented. (1) Establishment of a Multidisciplinary Team: A multidisciplinary team (MDT) comprising experienced obstetricians, rehabilitation physicians, therapists, and nurses was formed. All members underwent specialized training in pelvic floor dysfunction (PFD) and the ITHBC model to ensure proficiency in its core principles and application methods. (2) Enhancement of Knowledge and Belief: Patients were informed about pelvic floor rehabilitation precautions and dietary guidance. Tailored exercise plans were developed based on individual recovery progress and endurance. Collaborative discussions ensured timely treatment adherence, while relatives were encouraged to provide support and supervision. During sessions, pre-treatment communication emphasized home-based training adherence, with clocking records reviewed meticulously. Privacy was safeguarded, and electrical stimulation amplitudes were adjusted in real-time for optimal effects. Post-treatment, patients were motivated to engage fully in exercises with standardized movements, minimizing reliance on abdominal muscles. Family-based exercises were reinforced through encouraging language. (3) Improvement of Self-Management Ability: Follow-up groups via WeChat enabled parturients to share progress and receive standardized exercise videos. Exercise sessions required clocking in and submitting recorded videos for documentation. Outstanding performers received public praise, while those needing improvement were contacted by phone for support. (4) Strengthening Social Support: Online and offline gatherings via WeChat fostered a supportive community for exchanging questions and experiences. Family members provided daily psychological and behavioral support, assisting with goal-setting for muscle training and functional exercises. Continuous encouragement from medical staff and family members helped parturients recognize and celebrate milestones.
Observation index
Compliance with pelvic floor muscle training
The adherence to pelvic floor muscle training was assessed using the Pelvic Floor Muscle Training Compliance Questionnaire18. This meticulously designed questionnaire evaluates and documents the average daily engagement in pelvic floor muscle training through three distinct items. Item 1 measures daily time spent on pelvic floor muscle training, rated 1 to 5. Item 2 quantifies daily pelvic floor muscle exercises, also rated 1 to 5. Item 3 uses the Visual Analogue Scale (0–10) to assess training compliance. The total score vary between 2 and 20: <6 indicates poor adherence, 6–13 moderate adherence, > 13 excellent adherence. The Cronbach’s α is 0.81, showing strong internal consistency.
Self-efficacy in pelvic floor muscle training
The Pelvic Floor Muscle Exercise Self-Efficacy Scale19 was used for assessment. This scale includes two dimensions: expected self-efficacy (14 items) and anticipated outcome (9 items). Each item is scored from 0 to 10. A total score > 70 indicates high self-efficacy, 50–70 indicates moderate self-efficacy, and < 50 indicates low self-efficacy. The Cronbach’s α is 0.912, demonstrating strong internal consistency.
Pelvic floor function assessment
The Pelvic Floor Distress Inventory Short Form (PFDI-20) and the Pelvic Floor Impact Questionnaire Short Form 7 (PFIQ-7)20 were used for assessment before and after treatment. The PFDI-20 includes three dimensions: POPDI-6 (score range: 0–24), CRADI-8 (score range: 0–32), and UDI-6 (score range: 0–24). Higher scores indicate more severe pelvic floor dysfunction. Its Cronbach’s α is 0.93, showing strong reliability. The PFIQ-7 evaluates seven areas: distress level (1–4), work/daily activity impact, family role/relationship influence, social/leisure effects, sexual life implications, mood/emotional well-being impact, and self-esteem/self-image influence. Each question is scored 1–4, with a total score of 7–28. Its Cronbach’s α is 0.801, indicating internal consistency.
Assessment of pelvic floor muscle strength
The modified Oxford Scale (MOS)21 Scoring: Evaluated both pre- and post-treatment, this scale categorizes muscle contraction intensity into six distinct grades ranging from 0 to 5. The degree of contraction is defined as follows: no contraction corresponds to grade 0, weak contraction to grade 1, slight contraction to grade 2, average contraction to grade 3, good contraction to grade 4, and strong contraction to grade 5. A higher grade signifies progressively stronger muscle strength. At 12 weeks postpartum, a PHENIX USB4 pelvic floor rehabilitation therapy device was utilized to insert a balloon pressure probe into the vagina of the examinee22. This advanced technology enabled precise detection of the muscle strength and fatigue levels (percentage decrease in muscle strength per second) of both type I and type II pelvic floor muscle fibers. Pelvic floor muscle strength is assessed based on the intensity and duration of pelvic floor muscle contractions and classified into six hierarchical grades (0–5). Grade 0 indicates an absence of contraction, grade 1 denotes a faint tremor, grade 2 reflects incomplete contraction, grade 3 signifies complete contraction without resistance, grade 4 represents complete contraction with slight resistance, and grade 5 embodies complete contraction with persistent resistance.
Pelvic floor surface electromyography assessment
Surface electromyography (sEMG) is a widely recognized method for quantifying neuromuscular activation and detecting early muscle abnormalities. In clinical practice, sEMG using vaginal probes is one of the most commonly used clinical tools for evaluating and treating patients with pelvic floor muscle (PFM) dysfunction. Importantly, the correlation between sEMG and PFD has been validated23. The standardized Glazer protocol system, utilizing sEMG signal acquisition and processing technology, has been widely applied in clinical practice. Therefore, approximately 11% of published studies utilize sEMG based on the Glazer protocol24. The Glazer pelvic floor surface electromyography assessment (MLD A0 Pelvic Floor Surface Electromyography Analysis System)25 was employed both prior to and following the treatment: (1) Observation of the Abdominal Muscle Line: During pelvic floor muscle contractions, abdominal involvement should be avoided. Actions such as holding one’s breath or drawing in the abdomen may cause the abdominal muscle line to rise. Ideally, the abdominal muscle line should remain low, flat, stable, and free of fluctuations, indicating proper contraction movement. (2) Observation of the Contraction Line: The Glazer Agreement encompasses five activities:1. A 60-second break (before baseline) - instruct women to feel PFM during the break. 2. Five-phase (flick) contraction - the female is instructed to contract the PFM as quickly as possible (2-second contraction, with a 2-second break in between). (3) Five 10-second tonic contractions, with a 10-second break in between - instruct the female to contract the PFM as hard as possible, maintain the contraction for 10 s, and then fully relax the PFM after the contraction, maintaining relaxation for 10 s. (4) A 60-second endurance contraction - women were instructed to maintain the PFM contraction at a certain level for 60 s. (5) A 60-second break (after baseline) - instruct women to feel PFM during the break.The reference value for the rapid contraction test assessing fast muscle function is between 35 and 45 µV. The reference value for the tension-contraction test assessing the coordination of fast and slow muscles is 30–40 µV. The 60-second endurance contraction test for slow muscle function has a reference value of 25–35 µV26. The report captures the maximum or average values of each section and provides the coefficient of variation to evaluate muscle stability. 3. Observation of the Relaxation Line: The relaxation line is categorized into the anterior and posterior resting lines, as well as the post-exercise relaxation line. The reference value for the resting line is between 2 and 4 µV. A value exceeding 4 µV or a coefficient of variation greater than 0.2 may indicate muscle overactivity. Post-exercise relaxation time must also fall within the prescribed limits—for instance, the relaxation time for rapid contractions is 0.5 s, and for tension contractions, it is 1 s. Abnormal relaxation times may similarly suggest muscle overactivity25. Electromyogram parameters were collected to assess endurance contraction values, tension contraction values, maximum rapid contraction values, coefficients of variation for tension contractions, and coefficients of variation for endurance contractions. (Since no muscle hyperactivity occurred, the relaxation indicators held no evaluative significance. Consequently, the average values and coefficients of variation for the pre- and post-resting stages, as well as the relaxation times for rapid and tension contractions, were not calculated.The sEMG data were filtered using a built-in hardware first-order high-pass filter set to a cutoff of 10 Hz ± 10%. The raw sEMG data were visually inspected for artifacts. The root mean square (RMS) values were determined within a 200-millisecond window27. Subsequently, mean and peak amplitude values, as well as time parameters, were calculated28. In the Glazer protocol, signal processing for mean and peak amplitude was performed by averaging the sEMG RMS from the appropriate phase of the test (average from the start to the end of the phase). The mean peak amplitude represents the average of all peaks during the assessment activity. The pre-peak time and post-peak time in the Glazer protocol were calculated strictly according to the original procedure implemented in the Noraxon MyoResearch software. Resting activity was considered as 0% (minimum), and peak amplitude was considered as 100% (maximum). The relative threshold of 50% between the minimum and maximum values was considered as the onset of contraction (rise before the peak) and the end of contraction (fall after the peak). Signal processing in our protocol was also based on the sEMG RMS. For resting activity, the mean amplitude was calculated by averaging the sEMG RMS within the assessment activity. The mean amplitude during tonic and phasic contractions (tonic contraction and phasic rest) was calculated as the average between the onset and offset points. The final value was the average of five intervals. When the signal amplitude reached more than 3SD of the resting mean amplitude, the onset time was determined. The onset-to-peak time was calculated as the time between the onset and the peak (highest amplitude value). The peak-to-offset time was between the peak and the offset point (point below 3sD of the resting mean amplitude). Fatigue-related changes, such as mean frequency and median frequency, were calculated using FFT (Fast Fourier Transform) in the Glazer protocol and STFT (Short-Time Fourier Transform) in our protocol. During a 60-second static contraction, unfiltered RAW sEMG signals were analyzed using a 512-point window29,30.
Pelvic floor ultrasound parameter assessment
Prior to and following the treatment evaluation, two skilled ultrasound physicians, each with more than five years of specialized experience and having completed thorough standardized training in three-dimensional pelvic floor ultrasound, conducted the examination. The GE Voluson E8 ultrasound diagnostic instrument was employed, utilizing the abdominal three-dimensional volume probe (model RM6C4D) with a frequency range of 4–8 MHz. Ten minutes prior to the examination, the examinee was instructed to fully empty their bladder. During the procedure, the examinee assumed the lithotomy position. A layer of coupling agent was applied to the surface of the probe, which was then carefully wrapped in a probe sleeve to ensure all air bubbles were expelled. An ample amount of coupling agent was subsequently applied to the exterior of the probe sleeve before placing it gently on the perineum of the examinee. In accordance with the standardized operation guidelines31, image acquisition was performed using dual-frame contrast mode, volume rendering mode, and tomographic ultrasound imaging mode to capture both 2D and 4D pelvic floor ultrasound parameters in three distinct states: rest, anal contraction, and maximum Valsalva maneuver. At rest, measurements included bladder detrusor thickness, residual urine volume, bladder neck position, urethral inclination angle, anal-rectal angle, and levator ani hiatus area. Under Valsalva conditions, the posterior bladder-urethra angle, levator ani hiatus area, and anal-rectal angle were assessed. Bladder neck mobility and urethral rotation angle were calculated as positional changes between resting and Valsalva states (values subtracted if in the same direction, added if opposite). Additionally, levator ani muscle strain rates were computed: contraction strain rate = ΔA1 / resting hiatus area, Valsalva stretching strain rate = ΔA2 / resting hiatus area.
Evaluation of life quality
The quality of life before and after treatment was assessed using the WHO-QOL-BREF32 and SF-3633 scales. The WHO-QOL-BREF uses a 1–5 rating system: 1 = “basically unable,” 2 = “rarely able,” 3 = “able/average,” 4 = “mostly able,” 5 = “completely able.” It includes 29 items (excluding the open-ended self-evaluation), with scores directly reflecting quality of life (Cronbach’s α = 0.88). The SF-36 consists of 36 items across 8 health dimensions, scored from 0 to 100 (higher scores indicate better quality of life). Its Cronbach’s α for urinary system diseases is 0.849. The SF-36 consists of 36 items that assess the degree of health-related limitations in physical and psychological functioning. Previous studies on the Chinese version of the SF-36 have demonstrated its reliability and validity34.
Assessment of patient satisfaction in nursing
The Newcastle Nursing Service Satisfaction Scale (NSNS)35 was used to evaluate patient satisfaction in both groups. Scores: 95 = exceptional satisfaction, 76–94 = high satisfaction, 57–75 = moderate satisfaction, 38–56 = dissatisfaction, 19–37 = significant dissatisfaction. The scale’s Cronbach’s α is 0.935, indicating strong reliability.
Statistical analysis
A sample size calculation was conducted before the study. To calculate the sample size, we extracted the changes in muscle strength after electrical stimulation from previous studies36,with a type I error ratio α (two-sided) of 0.05 and a type II error ratio β of 0.1. PASS software was uased for sample size calculation. Statistical analysis was performed using SPSS 26.0. Categorical data were expressed as n (%) and compared using the χ² test. Ordinal data were analyzed with the rank-sum test. Continuous data following a normal distribution were presented as mean ± SD (x̄ ± s) and compared between groups using the independent-samples t-test. A P value < 0.05 indicated statistical significance.
Result
Compliance with pelvic floor muscle training
The observation group showed significantly better pelvic floor muscle training compliance compared to the control group (P < 0.05). Specific data and graphs are shown in Table 2 (Adherence to pelvic floor muscle training).
Pelvic floor muscle training self-efficacy
Compared with the control group, the self-efficacy score for pelvic floor muscle training in the observation group was markedly higher, demonstrating a statistically significant difference (all P values < 0.05). Detailed numerical data and graphical representations are illustrated in Table 3 (Pelvic Floor Muscle Training to Enhance Self-Efficacy).
Pelvic floor function assessment
Before the intervention, there was no significant difference in PFDI-20 or PFIQ-7 scores between the two groups (P > 0.05). After the intervention, both groups showed a significant decrease in PFDI-20 and PFIQ-7 scores, but the observation group had significantly lower scores than the control group (P < 0.05). Detailed results are shown in Table 4 (Pelvic Floor Dysfunction Assessment Scale).
Pelvic floor muscle strength assessment
Before the intervention, there was no significant difference in MOS ratings between the two groups (P > 0.05). After the intervention, both groups showed significant improvement in MOS ratings, but the observation group had significantly higher scores than the control group (P < 0.05). Details are shown in Table 5 (MOS Classification for Pelvic Floor Muscle Strength). Compared to the control group, the observation group had significantly better ratios of type I and type II pelvic floor muscle fibers (P < 0.05); see Table 6 (Type Ⅰ Muscle Fiber Strength) and Table 7 (Type Ⅱ Muscle Fiber Strength). No significant difference was observed in type I fiber fatigue between the groups (P > 0.05), but the observation group had significantly lower fatigue in type II fibers compared to the control group (P < 0.05). Refer to Table 8 (The Degree of Fatigue in Muscle Fibers) .
Pelvic floor surface electromyography assessment
Before the intervention, there were no significant differences in endurance contraction, tension contraction, or maximum rapid contraction values between the two groups (P > 0.05). After the intervention, all three values increased significantly in both groups, but the observation group had significantly higher values than the control group (P < 0.05). Similarly, there were no significant differences in the coefficient of variation for tension and contraction before the intervention (P > 0.05). Post-intervention, this coefficient decreased significantly in both groups, with the observation group showing significantly lower values than the control group (P < 0.05). For endurance contraction variability, no significant differences were observed between the groups either before or after the intervention (P > 0.05). Refer to Tables 9, 10, 11, 12 and 13 (9-Value of Endurance Contraction; 10-Tension-contraction value; 11-Value of Maximum Rapid Contraction; 12-Coefficient of Variation for Tension and Contraction; 13-Coefficient of Variation for Endurance Contraction) for detailed results.
Evaluation of pelvic floor ultrasound parameters
Before the intervention, there were no significant differences in ultrasound indicators between the two groups (P > 0.05). After the intervention, no significant changes were observed in bladder detrusor muscle thickness, residual urine volume, or initial bladder neck position compared to pre-intervention values (P > 0.05). However, other indicators such as urethral inclination angle, anal rectal angle, bladder neck mobility, urethral rotation angle, posterior vesicourethral angle, levator ani hiatus area, contraction strain rate of the levator ani muscle, and stretching strain rate of the levator ani muscle showed significant improvements in both groups compared to pre-intervention levels. Between groups, no significant difference was found in the anal rectal angle (P > 0.05), but the observation group had significantly better outcomes for all other indicators compared to the control group (P < 0.05). Refer to Tables 14, 15, 16, 17, 18, 19, 20, 21, 22 and 23 (14-Bladder Detrusor Muscle Thickness; 15-Residual urine volume; 16-Initial Position of the Bladder Neck; 17-Urethral inclination Angle; 18-Anal Rectal Angle; 19-Area of the Levator Ani Muscle Hiatus; 20-Mobility of the Bladder Neck; 21-Angle of Urethral Rotation; 22-Posterior Vesicourethral Angle; 23-Strain Rate of the Levator Ani Muscle for detailed results.
Quality of life assessment
Before the intervention, there were no significant differences in WHO-QOLBREF or SF-36 scores between the two groups (P > 0.05). After the intervention, both groups showed significant improvements in these scores, but the observation group had significantly higher scores than the control group (P < 0.05). Detailed results are shown in Table 24 (Comparison of Quality of Life Scale Scores).
Evaluation of nursing satisfaction
In comparison to the control group, the observation group showed significantly higher nursing satisfaction and overall satisfaction (P < 0.05). Detailed data and graphs are shown in Table 25 (Patient Satisfaction with Nursing Care).
Discussion
The extreme expansion and rapid contraction of the uterus during first-time natural delivery exert significant pressure on pelvic floor muscles, causing damage that disrupts uterine involution and may lead to long-term pelvic floor dysfunction, such as urinary incontinence or sexual dysfunction25. Physiologically, pelvic floor muscles maintain pelvic organ integrity, support urine control and defecation regulation, and preserve vaginal tightness37. Timely intervention is essential for restoring postpartum physiological changes. For high-risk parturients during vaginal delivery, early pelvic floor muscle training combined with electrical stimulation therapy effectively prevents pelvic floor disorders (PFD) and serves as a non-surgical treatment option38. Type I fibers provide structural support, while type II fibers focus on urethral closure. Pelvic floor muscle training enhances pubococcygeus muscle function through varied postures and techniques, promoting blood circulation and strengthening pelvic floor tension39. Bioelectrical stimulation evaluates muscle fiber conditions, repairs nerve damage, and improves muscle strength and elasticity by tailoring frequencies and pulse widths to individual needs40. However, successful training requires patient awareness of muscle group activities. Limited understanding of bioelectrical stimulation can lead to resistance or fear, reducing compliance. Thus, clinical nursing plays a key role in assessing patients’ physical and psychological states and providing appropriate guidance.
In this study, the observation group showed significantly higher self-efficacy and compliance in pelvic floor muscle training than the control group. Reasons for this include: (1) As the intervention progressed, parturients noticed improvements in their pelvic floor muscle function in daily life, which positively reinforced their self-efficacy; (2) The ITHBC intervention model places great emphasis on psychological care for parturients, focusing on stimulating positive emotions such as satisfaction, gratitude, hope, and a sense of self-worth during the pelvic floor rehabilitation process. Through diverse channels, encouragement and guidance were provided to parturients, and successful cases were shared, thereby increasing their awareness of pelvic floor rehabilitation treatment and effectively alleviating their fear of rehabilitation exercises. (3) The ITHBC intervention model also prioritizes enhancing communication and interaction between parturients and the outside world. By enriching their social support network, it further strengthens their self-efficacy in pelvic floor muscle training, thereby improving exercise compliance. Bridging the gap between the medical team and patients.
In this study, pelvic floor muscle strength (MOS grades) significantly increased after intervention, confirming that pelvic floor muscle training combined with biofeedback therapy effectively enhances muscle strength. Improvements were more pronounced in the observation group, indicating that the ITHBC intervention model amplifies rehabilitation efficacy. Reasons for the ITHBC-based comprehensive rehabilitation treatment’s success include: (1) Tailored pelvic floor muscle training (PFMT) by an MDT team enhances muscle strength and restores postpartum function; (2) Appropriate exercise stimulates dopamine secretion, improving nervous system excitability and coordination; (3) Follow-up communication and targeted PFMT training improve overall pelvic floor muscle strength.
In this research, both groups showed significant improvements in WHO-QOLBREF and SF-36 scores pre- and post-intervention. Analysis of the reasons is as follows: (1) Within the ITHBC intervention model, the MDT team has refined the precision of pelvic floor rehabilitation treatment. Effective communication and seamless information sharing not only foster trust but also elevate patients’ satisfaction with the medical process. By establishing attainable short-term and medium-to-long-term goals aligned with patients’ lifestyle habits, a sense of accomplishment can be instilled, thereby empowering patients to cultivate confidence in adopting healthier behaviors in the future. The ITHBC model integrates multiple theoretical frameworks from psychology and behavioral science, enabling a more holistic analysis and interpretation of the transformation process in healthy behaviors. (2) The ITHBC nursing model enhances compliance and self-management capabilities in pelvic floor rehabilitation treatment. Quality of life is intrinsically linked to the quality of self-management; high-quality self-management directly contributes to an improved quality of life. The ITHBC nursing model emphasizes enriching health knowledge and reinforcing beliefs, guiding patients to strengthen their conscious behaviors and control abilities while enhancing social support across various dimensions. This approach enhances parturients’ participation in pelvic floor rehabilitation, reduces postpartum anxiety and depression, and achieves the primary goal of pelvic floor recovery.
Limitations
We have to acknowledge the limitations of this study: (1) The high cost of pelvic floor MRI, its comparable value to pelvic floor ultrasound, and the discomfort of urodynamic exams led to a smaller sample size, limiting comprehensive analysis. (2) Intervention measures were assessed only during the rehabilitation period, allowing evaluation of short-term efficacy but not long-term outcomes such as urinary incontinence or pelvic organ prolapse. (3) Although multicenter, most research units were in China’s eastern plain region, with limited representation from other areas, affecting regional generalizability. Participants were all Han Chinese women, precluding ethnic comparisons. (4) Dietary influences could not be explored due to homogeneous dietary habits across regions. (5) Risk factors and process deficiencies were not analyzed using FMEA41, nor were improvement plans proposed. Future work should focus on refining the ITHBC nursing model for better pelvic floor rehabilitation outcomes. (6). It should be noted that Scharschmidt et al.42 concluded that electrode arrangement (longitudinal versus circumferential) had no impact on the reliability of sEMG data. However, whether the body positioning will affect the results remains unclear, which might lead to different results.
Conclusion
In conclusion, the puerperium is a critical period for rehabilitation in primiparas after natural childbirth. Early intervention with ITHBC-based comprehensive rehabilitation significantly improves pelvic floor muscle strength, reduces fatigue, enhances self-efficacy and compliance, and promotes recovery. These findings support further research into ITHBC as a component of postpartum rehabilitation programs. More clinical data needs to be collected before a solid recommendation could be made.
Data availability
All data generated or analysed during this study are included in this published article.The data is available at Ye, X. (2025). Application Research of Biofeedback Electrical Stimulation Synergized with Pelvic Floor Muscle Self-Exercise for Postpartum Pelvic Floor Rehabilitation for Primiparas Undergoing Vaginal Delivery Within the Framework of the ITHBC Nursing Model: A Multicenter Randomized Controlled Trial [Data set]. Zenodo. https://doi.org/10.5281/zenodo.16742010.
References
Cristine, J. et al. Pelvic floor muscle training as treatment for female sexual dysfunction: a systematic review and meta-analysis. Am. J. Obstet. Gynecol. 231 (1), 51–66 (2024).
Qian, G. et al. Pelvic floor dysfunction in postpartum women: A cross-sectional study. PLoS One. 19 (10), e0308563 (2024).
Celia, R. L., Olga, L. T., Amelia, G. G. & Miguel, G. R. Pelvic floor muscle training interventions in female athletes: A systematic review and Meta-analysis. Sports Health. 16 (5), 766–775 (2024).
Stephanie, P. & Jandra, M. Pelvic floor physical therapy and female sexual dysfunction. Clin. Obstet. Gynecol. 68 (1), 37–43 (2025).
Laura, C. et al. Pelvic floor ultrasound findings and symptoms of pelvic floor dysfunction during pregnancy. Int. Urogynecol. J. 35 (12), 2423–2430 (2024).
Laura, C., Dominique, S., Christine, B., Sophie, G. & Jan, D. Body image and pelvic floor dysfunction in pregnancy and postpartum: A prospective one-year follow-up cohort study. BJOG 131 (10), 1420–1429 (2024).
Andrea, S., Glaucia, P., Elaine, M., Cassia, J. & Luiz, B. Prolonged second stage of labor and postpartum pelvic floor dysfunction. Urogynecology 31 (6), 561–570 (2025).
Yaqin, H. et al. Meta-analysis of the therapeutic effect of electrical stimulation combined with pelvic floor muscle exercise on female pelvic floor dysfunction. Eur. J. Med. Res. 29 (1), 380 (2024).
Cinara, S., Bary, B., Rob, B., IIse, M. & Fernando, C. Predictors for adherence to a home-based pelvic floor muscle exercise program for treating female urinary incontinence in Brazil. Physiother Theory Pract. 36 (1), 186–195 (2020).
Carolina, A. et al. Adherence and self-efficacy of pregnant women to perform pelvic floor muscle training through a health education application: a feasibility study. Mhealth 14 (3), 11–17 (2025).
Aida, J. et al. Improving pelvic floor muscle training adherence among pregnant women: validation study. JMIR Hum. Factors. 9 (1), e30989 (2022).
Polly, R. Integrated theory of health behavior change: background and intervention development. Clin. Nurse Spec. 23 (3), 161–170 (2009).
Qiaoyue, Y., Genzhen, Y., Maoling, F., Juanjuan, Y. & Xinyu, L. The effectiveness of a transition programme based on the integrated theory of health behavior change in adolescents with chronic kidney disease: a quasi-experimental study. BMC Pediatr. 25 (1), 111 (2025).
Honghong, W. et al. Effect of a WeChat-Based hybrid intervention on the adaptation outcomes of people living with HIV/AIDS: pilot randomized controlled trial. J. Med. Internet Res. 3 (27), e65268 (2025).
Lan, Z. et al. Effectiveness of a family-Based Self-Management intervention for type 2 diabetes patients receiving family Doctor contract services: A Community-Based randomized controlled trial. J. Prim. Care Community Health. 12 (16), 21501319251330384 (2025).
Hang, L., Xueyun, W., Lingyan, B., Jialei, Z. & Jing, L. Development and psychometric evaluation of a self-management ability assessment scale for individuals with spinal cord injury. J. Clin. Neurosci. 3 (133), 111049 (2025).
Ghaderi, F., Bastani, P., Hajebrahimi, S., Jafarabadi, M. A. & Berghmans, B. Pelvic floor rehabilitation in the treatment of women with dyspareunia: a randomized controlled clinical trial. Int. Urogynecol. J. 30 (11), 1849–1855 (2019).
Fangfang, D. et al. Enhancing pelvic floor muscle training efficacy for Middle-Aged women with stress urinary incontinence through square dance integration: A Quasi-Experimental study. J. Multidiscip Healthc. 9 (17), 3863–3873 (2024).
Yasmin, E. R., María, T. L., José, C., Rodrigo, N. C. & Joaquín, C. Correlation of Self-Efficacy for pelvic floor muscle exercise with symptoms of stress urinary incontinence in women. Int. Urogynecol. J. 35 (7), 1487–1493 (2024).
Catharina, F. & Ulrika, J. Sexual function and pelvic floor function five years after hysterectomy. Acta Obstet. Gynecol. Scand. 104 (5), 948–957 (2025).
Hongmei, Z. et al. Effect of pelvic floor workout on pelvic floor muscle function recovery of postpartum women: protocol for a randomized controlled trial. Int. J. Environ. Res. Public. Health. 19 (17), 11073 (2022).
Wang, S. et al. Evaluation of pelvic floor muscle function (PFMF) in cervical cancer patients with Querleu-Morrow type C hysterectomy: a multicenter study. Arch. Gynecol. Obstet. 305 (2), 397–406 (2022).
Min, L. et al. Two year follow-up and comparison of pelvic floor muscle electromyography after first vaginal delivery with and without episiotomy and its correlation with urinary incontinence: a prospective cohort study. Acta Obstet. Gynecol. Scand. 102 (2), 200–208 (2023).
Oliveira, J. et al. Techniques for registration of myoelectric activity of women’s pelvic floor muscles: a scoping review. Int. Urogynecol. J. 35 (5), 947–954 (2024).
Zhang, H. et al. Analysis of pelvic floor electromyography in women screened 42 days postpartum: A cross-sectional study. Med. (Baltim). 102 (21), e33851 (2023).
Oleksy, Ł. et al. The reliability of pelvic floor muscle bioelectrical activity (sEMG) assessment using a Multi-Activity measurement protocol in young women. Int. J. Environ. Res. Public. Health. 18 (2), 765 (2021).
Hermens, H., Freriks, B., Disselhorst-Klug, C. & Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 10 (5), 361–374 (2000).
Dehail, P. et al. Kinematic and electromyographic analysis of rising from a chair during a Sit-to-walk task in elderly subjects: role of strength. Clin. Biomech. 22 (10), 1096–1103 (2007).
Cifrek, M., Medved, V., Tonković, S. & Ostojić, S. Surface EMG based muscle fatigue evaluation in biomechanics. Clin. Biomech. 24 (4), 327–340 (2009).
MacIsaac, D., Parker, P. & Scott, R. The short-time fourier transform and muscle fatigue assessment in dynamic contractions. J. Electromyogr. Kinesio. 11 (6), 439–449 (2001).
Bernard, H. et al. AIUM/IUGA practice parameter for the performance of Urogynecological ultrasound examinations: Developed in collaboration with the ACR, the AUGS, the AUA, and the SRU. Int. Urogynecol. J. 30(9), 1389–1400 (2019).
Guido, V. et al. Quality of life is associated with vaccine reluctance via mental health and fear of covid-19: an exploratory investigation on a Palestinian sample. Psychol. Health Med. 28(9), 2647–2659 (2023).
Brian, H. et al. Association between PROMIS10, SF-36 and NeuroQoL in persons with multiple sclerosis. Mult Scler. Relat. Disord. 79(11), 105003 (2023).
Lam, C., Tse, E., Gandek, B. & Fong, D. The SF-36 summary scales were valid, reliable, and equivalent in a Chinese population. J. Clin. Epidemiol. 58 (8), 815–822 (2005).
Ayşe, K., Sibel, E. & Serap, K. Relationship between missed nursing care and patients’ trust in nurses and satisfaction with care: A cross-sectional study. Nurs. Health Sci. 26 (3), e13149 (2024).
Correia, G., Pereira, V., Hirakawa, H. & Patricia, D. Effects of surface and intravaginal electrical stimulation in the treatment of women with stress urinary incontinence: randomized controlled trial. Eur. J. Obstet. Gynecol. Reprod. Biol. 173 (2), 113–118 (2014).
Andrea, B. & Maurizio, S. New advances in female pelvic floor dysfunction management. Medicina 59 (6), 1010 (2023).
Huma, R., Hadia, N. & Farooq, R. Recent advances in the pelvic floor assessment and rehabilitation of women with pelvic floor dysfunction. J. Pak Med. Assoc. 72 (7), 1456–1459 (2022).
Maria Letícia, C., Lívia, B., Joyce, O., Maria, O. & Maria, M. Pelvic floor muscle training in women with urinary incontinence and pelvic organ prolapse: A protocol study. PLoS One. 19 (8), e0308701 (2024).
Xiuqi, W. et al. Pressure-Mediated biofeedback with pelvic floor muscle training for urinary incontinence: A randomized clinical trial. JAMA Netw. Open. 7 (11), e2442925 (2024).
Marco, V. et al. Healthcare application of failure mode and effect analysis (FMEA): is there room in the infectious disease setting? Scoping Rev. Healthc. 13 (1), 82 (2025).
Scharschmidt, R., Derlien, S., Siebert, T., Herbsleb, M. & Stutzig, N. Intraday and interday reliability of pelvic floor muscles electromyography in continent woman. Neurourol. Urodyn. 39 (1), 271–278 (2020).
Acknowledgements
The study would like to thank each of the women who participated in the study, who have maintained contact with our hospital over the years so that we can observe the safety and effectiveness of the treatment.
Funding
This research received funding from the clinical medical research center for obstetrics and gynecology diseases in Qinghai Province(Grant No. 2024-SF-L03).
Author information
Authors and Affiliations
Contributions
Xi Ye is the first author, responsible for research design and paper writing; Yulin Wu is the second author, responsible for data collection; Tian Le is the third author, responsible for the smooth progress of the research procedures; Zhiqing Song is the fourth author, responsible for contacting the funding project; Yanjie Cao is the fifth author, responsible for statistics; Yanyue Zhang is the sixth author, responsible for statistical analysis; Xuanxuan Hong is the seventh author, responsible for data classification; Le Yu is the eighth author, responsible for data summary; Liehong Wang is the corresponding author, responsible for the calibration and review of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Human ethics approval and consent to participate
This study protocol was reviewed and approved by the Medical Ethics Committee of Hefei Maternal and Child Health Hospital(YYLL20240130-YNXM-LL-01-2.0). All patients are allowed to participate in this research only after signing the informed consent form.
Consent to participate
Written informed consent was obtained from all participating patients.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ye, X., Wu, Y., Le, T. et al. Exploring the application of an integrated health behavior change-based nursing model in pelvic floor muscle self-training. Sci Rep 15, 44542 (2025). https://doi.org/10.1038/s41598-025-28329-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-28329-3