Abstract
This study constructed an educational intervention based on the common-sense model of self-regulation for lung cancer patients after thoracoscopic surgery and evaluated the effects of the educational intervention. From July 2023 to January 2024, ninety patients with lung cancer after initial thoracoscopic surgery were divided into an intervention group (N = 45) and a control group (N = 45). Patients in the intervention group received a nursing intervention based on the common-sense model of self-regulation. Patients in the control group received usual care. The intervention group received face-to-face and telephone counselling for 4 weeks, and they had a manual. Pulmonary exercise compliance, frailty, and illness perception were assessed before and after the intervention. After the implementation of the nursing intervention based on the common-sense model of self-regulation, there were statistically significant differences in lung function exercise compliance scores and illness perception scores between the intervention group and the control group, but there was no statistically significant difference in frailty scores between the two groups after the intervention. This educational intervention is effective for the rehabilitation behaviour of lung cancer patients following thoracoscopic surgery. Clinical trial registration: This study has been registered in the Chinese Clinical Trial Registry through this website www.chictr.org.cn, and the registration number is ChiCTR2400087033. The first registration date was 17 July 2024.
Similar content being viewed by others
Introduction
According to the Global Cancer Statistics Report 2020 released by the International Agency for Research on Cancer, lung cancer ranks second in incidence and first in mortality among all cancers, accounting for 18% of all cancer-related deaths1. Mediastinal, hilar, and segmental lymph node dissection is an indispensable component of complete lung cancer resection. Lobectomy or total lung resection combined with lymph node dissection is considered the standard surgical procedure and is ideally performed using minimally invasive techniques2. Video-assisted thoracoscopic surgery (VATS), a minimally invasive technique, is associated with reduced trauma and faster recovery, facilitating the implementation of enhanced recovery after surgery (ERAS) protocols, with hospital discharge typically occurring within 2 to 6 days3. Domestic retrospective data have also confirmed the safety and feasibility of thoracoscopic surgery with a hospital stay of less than 48 h for Chinese patients4. The future of thoracoscopic surgery as a day surgery means that patients will have shorter hospital stays and faster bed turnover. At present, ERAS has been widely applied in the perioperative management of lung cancer patients to promote postoperative recovery and reduce the length of hospital stay5. ERAS protocols include prehabilitation (smoking cessation, preoperative exercise, respiratory physiotherapy, nutritional counselling), intraoperative anaesthetic management, and postoperative measures promoting early ambulation and oral nutritional intake; however, they do not explicitly emphasize postoperative respiratory exercises6. Postoperative recovery in lung cancer patients is a complex process in which breathing exercises may play a crucial role in enhancing pulmonary function and quality of life (QoL)7. After surgical resection of lung lesions, lung tissue and its surrounding tissues may be damaged, resulting in decreased lung function. Therefore, active postoperative lung function exercise is essential for promoting functional recovery8.
Compliance refers to the behaviour in which patients voluntarily cooperate to follow the prescribed program, comply with medical advice and maintain consistency9. The level of compliance with lung function exercises among lung cancer patients after surgery directly affects the process of postoperative recovery, such as the length of hospitalization, quality of life and readmission of patients after discharge10. We conducted a thoracoscopic postoperative investigation in patients with lung cancer, which has been published. In accordance with the results of previous investigations, most of the patients in the current investigation reported moderate levels of compliance with lung function exercise11. The adherence to pulmonary function exercises among lung cancer patients after thoracoscopic surgery remains to be improved. To address this situation, domestic and foreign studies have conducted interventions based on the psychological aspects of patients and self-behavioural decision-making, which have been effective12,13. However, few intervention studies on thoracoscopic postoperative conditions in lung cancer patients have been conducted, and the intervention content was not detailed or the research repeatability was poor. It is necessary to choose a theoretical framework that can include many factors to support the intervention content.
The common-sense model of self-regulation (CSM) proposed by Leventhal states that stimuli activate the current or future threat of disease, and individuals produce cognitive and emotional manifestations of disease, thus taking disease-behaviour measures and producing outcomes14. CSM has a history of more than 50 years and provides a theoretical basis for illness perception, and it is effective for disease management for patients seeking treatment15. From the perspective of the structure of the common-sense model of self-regulation16, applying the model should focus on disease threats and psychological characteristics associated with illness to improve disease-related behavioural interventions. Early-stage exploration and intervention measures, such as supporting patients’ recovery behaviours, are recommended by this model. Research has indicated that understanding changes in patients’ perceptions of their condition can facilitate the implementation of health management plans16. The core of a nursing intervention based on the common-sense model of self-regulation is the patient’s illness perception, that is, the intervention of disease cognition and psychology, which focuses on the patient’s present or future disease threat to influence behaviour and outcomes. The application of this model not only affects patients’ psychology and cognition but also improves patients’ health behaviours, such as compliance, and outcomes, such as quality of life, depression and physical function15,17. In cancer patients, the effect of intervention was determined through a systematic review of the common-sense model of self-regulation. This review revealed that this model is effective for clinical interventions for cancer patients, such as nursing satisfaction, physical function, emotional distress, and quality of life18. The effect of this model intervention on rehabilitation compliance in cancer patients still needs to be explored.
Therefore, in this study, the CSM model was used to construct and apply an intervention scheme for patients with lung cancer after thoracoscopic surgery to explore whether the intervention scheme is effective for compliance with lung function exercise. We hypothesize that lung cancer patients recognize disease threat after thoracoscopic surgery compared with their preoperative state, which affects their disease perception (cognitive and emotional representations) and consequently influences postoperative rehabilitation outcomes (pulmonary function exercise compliance). Frailty, as an indicator of health deterioration, can be used to assess disease threat in surgical patients, elderly individuals, and cancer patients19. Cancer and its treatment can pose some threats to patients. Frailty represents the loss of functional reserves, and we evaluated changes in patients before and after interventions. Illness perception is central to the self-regulation knowledge model20, which refers to the process through which patients analyse and interpret their disease experiences and acquired knowledge. The illness perception cognition representations in this study included patients’ awareness of disease risks, postoperative symptom complications, disease knowledge, understanding of surgical treatment, and rehabilitation awareness. Emotional representations included postoperative hospitalization and home-based emotional states, as well as disease-related concerns. The intervention incorporated coping strategies for both cognitive and emotional representations. Understanding whether nursing interventions based on the common sense model of self-regulation can improve compliance with lung function exercise among lung cancer patients after thoracoscopic surgery is our research direction and provides a basis for future health education for lung cancer patients after thoracoscopic surgery.
Methods
Design
This study used a nonrandomized controlled trial design. Single blindness was also assessed. The data collectors did not know the grouping status, and the research subjects and the intervention practitioner knew the grouping status.
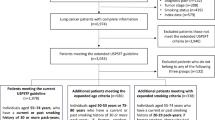
Participants
Lung cancer patients who underwent thoracoscopic surgery in the Department of Thoracic and Cardiac Surgery from July 2023 to January 2024 were selected as the study objects. With respect to convenience sampling, the inclusion criteria were as follows: (a) age ≥ 18 years; (b) with rapid intraoperative pathological findings of lung cancer or confirmed pathological findings of lung cancer; (c) underwent thoracoscopic surgery for the first time; (d) showing normal communication and expression; (e) willing to participate in the study after the provision of informed consent. The exclusion criteria were as follows: (a) having metastatic tumour disease; (b) unable to cooperate with lung function exercise; and (c) with pathological results revealing nonmalignant lung tumours.
The sample size was calculated using G*power software (version 3.1.9.7), with α = 0.05 and β = 0.05, according to the lung function exercise compliance score after intervention21, which yielded 28 as the minimum total sample size.
Control
After admission, patients in the control group who had undergone thoracic and cardiac surgery were evaluated and provided instructions by nurses. Respiratory function exercises were taught before the operation, and precautions for preparing preoperative articles were given. Daily postoperative rounds were performed to urge patients to perform respiratory function exercises, blow up balloons, and get out of bed as early as possible. Tips on postoperative cough and diet were provided on the blackboard in the corridor, and a video of functional exercises behind the door of the ward could be feely accessed. Wounds were dressed and reexamined after surgery, and the reexamination time was determined according to the doctor’s instructions. Before discharge, the nurses educated the patient.
Intervention
Development of the intervention and educational manual
The research team consisted of a doctoral supervisor, two nursing postgraduates, two cardiothoracic surgeons, three nurses, one psychologist, and one rehabilitation doctor. The main tasks of the research team included a literature search and evaluation, expert inquiry form development, expert selection, expert recommendation analysis and integration, and protocol determination. Relevant books and literature were consulted, and members of the research team were consulted11. After discussion, the research team developed the first draft of the intervention and the Manual of Health Education after thoracoscopic surgery.
We then conducted two rounds of expert correspondence. Delphi experts are usually consulted to ensure the credibility of a study, and several Delphi experts are usually consulted22. In this study, 15–50 experts were consulted. On the basis of the needs of the subject and the actual situation, the final number of experts in this study was determined to be 15. Seven head nurses with more than 10 years of working experience, three physicians, four rehabilitation physicians and one psychotherapist were included. In this study, the expert authority coefficient reached 0.863 in the first round of expert consultations and further increased to 0.890 in the second round. Generally, an expert authority coefficient (Cr) > 0.80 indicates a high reliability of expert opinions, demonstrating that the experts demonstrated strong judgement criteria and familiarity with the content, ensuring reliable conclusions. The coordination coefficient (W value) for the first round of expert consultations was 0.311, whereas that of the second round was 0.230. W values ranging between 0 and 1 indicated that the level of coordination was acceptable. All the variation coefficients in the second round were < 0.25, indicating satisfactory coordination. We defined the intervention theme as the primary indicator, the intervention focus as the secondary indicator, and the specific intervention content as the tertiary indicator. In the first round, the variation coefficients (CV values) for all the indicators ranged from 0.072 to 0.196. On the basis of the variation coefficient scores (average item score < 3.5 or CV > 0.3), adjustments to the intervention recommendations for these indicators were necessary. Consequently, two tertiary indicators (1.1.4 and 2.1.3) were added, and one (4.1.1) was removed. The final variation coefficients for all the indicators in the second round ranged from 0.052 to 0.164, indicating the establishment of an intervention plan. Detailed content is provided in Supplementary file 1.
A preliminary experiment was conducted following the initial formation of the intervention scheme. In accordance with the inclusion and exclusion criteria, five patients with lung cancer after thoracoscopic surgery were selected to test the feasibility of this study method. The results showed that the process of forming the final intervention draft is feasible and scientific. A final draft of the intervention plan was completed.
Intervention group
In the intervention group, on the basis of the control group, trained and qualified nurses provided nursing interventions on the basis of the common-sense model of self-regulation starting on the third day after surgery. There were four interventions in total, once a week for 20–40 min. The interveners were the nurses. The intervention methods included face-to-face education and telephone education. In the intervention process, the educational manual Health Education Manual After Thoracoscopic Surgery was used as a tool (Supplementary file 2).
The first intervention involved disease threat assessment and response to thoracoscopic surgery, and on the third day after surgery, patients were evaluated for frailty, illness perception, and compliance with pulmonary exercise. They were asked about the physical and psychosocial changes they experienced before and after surgery and were asked about their goals for recovery. The disease threat following thoracoscopic surgery was discussed with them, and they were encouraged to seek help and gain confidence in the treatment of thoracoscopic surgery. Common problems such as thoracoscopic surgery, the use of a thoracic drainage tube, wound care, pain, fever, cough, asthma, insomnia, and constipation were discussed. The relationship between the degree of disease threat after surgery and compliance with lung function exercises was indicated. The nature of and response to lung function exercises were presented, in particular, upper limb exercises, lower limb exercises, and breathing training; in addition, evaluating the number and duration of daily exercises; and evaluating whether the movements are standardized were presented. The impediments to and facilitators of pulmonary exercise were assessed, and facilitators and impediments were identified, and the patients were encouraged to comply with pulmonary exercise. Finally, the patients were provided with an educational manual to teach them patient rehabilitation knowledge.
The second intervention involved exploring misunderstandings and determining the correct disease understanding by telephone, and the current postoperative rehabilitation of patients was compared with the target to further promote postoperative patient rehabilitation. The consequences of the disease, its timelines, the patient’s personal control, the treatment control, recognition of the symptoms, the disease congruence, and the representations of concern were explored. In particular, the classification of the disease and its symptoms, causes, high-risk groups, diagnostic methods, treatment methods, and treatment effects were covered. The current status of lung function exercises was assessed. The problems associated with the obstructive factors of home lung function exercise were addressed. To reduce the inconvenience of home exercise and lack of social support from medical staff, efforts were made to establish patients’ confidence in self-regulation.
The third intervention included assessment of formal illness, promotion of a positive mental state, providing instructions by telephone, evaluating the psychological status of patients, understanding the methods of psychological adjustment of patients, and encouraging effective psychological adjustment of patients. At this time, the common psychological conditions of patients included doubt, denial, depression, anxiety, relapse, fear, and anger. Common psychological adjustment methods include communication with relatives and friends, exercise, environmental atmosphere transformation, and problem solving. The patients were introduced to self-regulating emotional methods through expressive writing and expression. Self-regulating expressive writing can promote patients’ attention to emotions and make cognitive structural adjustments to problems, affecting their ability to actively cope with problems. This method requires an undisturbed environment for 15–20 min per day for 3–4 days. Other issues could be influenced by the patient’s experience of being diagnosed with lung cancer and the reasons for their specific psychological challenges, such as the fear of recurrence.
On the basis of the patient’s postoperative lung function exercises, participants were instructed to respond to the following statements:
-
1.
Objective experience and subjective feelings of postoperative pulmonary function exercise.
-
2.
Analyse the hindrance factors and promotion factors of following the pulmonary function exercise program.
-
3.
Whether solutions to the obstructive factors of lung function exercise exist and whether the lung function exercise program is successfully carried out to achieve the desired rehabilitation goals.
-
4.
Imagine completing the pulmonary function exercise plan, achieving the desired rehabilitation goals, and assessing the impact of postoperative pulmonary function exercise problems on various aspects.
The fourth intervention included learning about self-regulation and facing it positively, preaching by telephone and exploring future health threats and responses to patients. Patients need to summarize the overall intervention measures and propose future prospects. The current postoperative rehabilitation of the patients was compared with the target, and self-evaluations were performed to determine whether the target was achieved. Positive disease cognition and emotion were reinforced, and regular checks were performed. Finally, evaluation indices were measured.
Instruments
Demographic and clinical characteristics
The general questionnaire data included age, sex, education level, type of medical insurance, height and weight, presence of hypertension, presence of diabetes, and the presence of two lung nodules. The questionnaire concerning surgical conditions included the pathological type of lung cancer, presence of lymph dissection, presence of postoperative fever (within 3 days of surgery), presence of postoperative defecation (within 3 days of surgery), and degree of postoperative pain measured by the Numerical Rating Scale. NRS), postoperative sleep status (patient self-rated sleep as good or bad), preoperative hospital stay, and the first day of drainage of the thoracic drainage tube.
Frailty
Patient frailty was assessed using the Groningen Frailty Indicator (GFI). The GFI contains 15 questions concerning the following areas of life: physical (nine items), cognitive (one item), social (three items), and psychological (two items). Each item was marked with a score of “0” or “1”, one point for “never” or “sometimes” for social Items 11–13, one point for “sometimes”, “often”, or “always” for psychological Item 14, and one point for “never”, “occasionally”, “sometimes” or “often”, on a scale of 0 to 15. Frailty was defined as a GFI ≥ 4. The Cronbach’s α coefficient of the Chinese version of the Groningen Frailty Indicator was 0.712.
Illness perception
The Chinese version of the Brief Illness Perception Questionnaire (BIPQ) was used to quantify illness perception. The questionnaire consisted of eight quantified items and one question and answer about the cause of the disease. Items 1 to 5 (consequences, timelines, personal control, treatment control, and identity) constituted the cognitive dimension of the disease. Items 6 and 8 (attention and emotional response) constituted the emotional dimensions of the disease. Item 7 (disease coherence) represents consistency in illness perceptions. The score range for each item was 0–10 points, with a total score of 80 points. Three of the items were graded backwards (Items 3, 4, and 7). The data for these entries are summarized as follows: higher illness perception scores indicate that patients have more negative perceptions and emotions about the impact of the disease on their health. The reliability coefficient of Cronbach’s α for the simplified Chinese version of the illness perception questionnaire was 0.7723. In this study, the Cronbach’s α reliability coefficient of the questionnaire was 0.645.
Lung function exercise compliance questionnaire
The patient’s compliance with postoperative pulmonary function exercise was measured using the functional exercise compliance questionnaire prepared by the teacher Lu Fengjuan (previous studies have stated that this questionnaire was adapted and applied to the measurement of pulmonary function exercise, as explained in the introduction). The content of the questionnaire in this study was evaluated on the basis of the degree of compliance with lung function exercises that we reviewed after thoracoscopic surgery. The questionnaire consists of four dimensions: exercise monitoring, precautions after surgery, exercise compliance, and actively seeking exercise suggestions. After the dimension was divided and specific items were indicated, the dimensions were divided into exercise compliance, Items 1–6; exercise monitoring, Items 7–9; asking for advice, Items 10–12; and postoperative precautions, Items 13–15. The 5-point Likert scoring method was used, from “completely able to do it” to “not able to do it at all”, with a higher score indicating higher compliance with the exercise. Previous studies have indicated that the Cronbach’s α reliability coefficient of this questionnaire in patients with lung cancer is 0.8624. In this study, the Cronbach’s α reliability coefficient of the questionnaire was 0.755.
Data collection and analysis
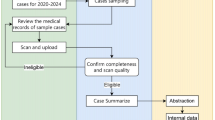
Data collection
The intervention was performed preintervention (day 3 after thoracoscopic surgery) and postintervention (1 month after thoracoscopic surgery). Methods of data collection included face-to-face collection during hospitalization and telephone collection after discharge.
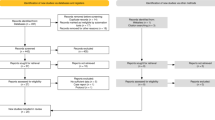
Statistical analyses
SPSS software (version 25.0) was used for data entry and statistical analysis. The counting data were expressed as frequencies and component ratios, and the measurement data were statistically described as means ± standard checks. Nonparametric rank sum tests were used to describe the data in terms of the mean, SD, and median (min; max). Data in the intervention and control groups were compared using the t test, Wilcoxon-Mann-Whitney test, or chi-square test. A paired t test or Wilcoxon signed-rank test was used for in-group comparisons between the intervention and control groups. Comparisons between the intervention and control groups were performed using the independent sample t test or Wilcoxon-Mann‒Whitney test.
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the Affiliated Hospital of Jiangnan University and Wuxi School of Medicine, Jiangnan University. The attributes, benefits, uses, and disadvantageous effects of the study were explained to all the participants, and informed consent was obtained from all the participants included in this study. The patients had the right to refuse to participate in the trial if they did not want to. An ethical review was performed before the start of this study, and after ethical approval for JNU20230301IRB12 and LS2024249 was obtained, a clinical intervention study was conducted. This study was registered with the Chinese Clinical Trial Registry.
Results
Characteristics of the participants
During patient recruitment, 60 eligible participants in the intervention group met the inclusion/exclusion criteria, while 9 declined participation, with another 6 ultimately dropping out of follow-up. The control group included 65 patients, 13 of whom declined enrolment, and 7 of whom withdrew from follow-up. Ultimately, both groups included 45 lung cancer patients each. The enrolment rate was 82.4%, and the follow-up rate was 87.4% in this study. The basic data of the study subjects revealed that the age of the patients in the intervention group was 60.18 ± 13.176 years, and the age of the patients in the control group was 61.13 ± 10.483 years. There was no statistically significant difference between the two groups in terms of general or operation-related information (p > 0.05), indicating that the basic information of the two groups was balanced and comparable (Table 1).
Outcome evaluation
Comparisons of frailty scores between the intervention group and control group
Before the intervention, the total score of frailty and scores of frailty in each dimension of the study participants in the intervention and control groups were nonnormally distributed, and the balance between groups was compared using the Wilcoxon-Mann‒Whitney test. The results revealed that the total score of frailty and the scores of the physical, cognitive, social, and psychological aspects of frailty in the two groups were not significantly different (p > 0.05), indicating that the baseline comparison of patients in the two groups was comparable.
After the intervention, the mean frailty and frailty scores of the subjects in the intervention and control groups were not normally distributed; thus, the Wilcoxon–Mann–Whitney test was used to compare the frailty scores between the intervention and control groups after the intervention. The results revealed that the total score of frailty and the scores of the physical, cognitive, social, and psychological aspects of frailty were not significantly different between the two groups (p > 0.05). However, it is worth noting the psychological aspect of frailty (z=−1.908; p = 0.056), which suggests that compared with conventional care, nursing interventions based on the common-sense model of self-regulation may be more beneficial for psychological improvement (Table 2).
The frailty scores of the intervention and control groups were nonnormally distributed before and after the intervention, and the Wilcoxon signed-rank test of two samples was used as a nonparametric test. The frailty scores in both groups were lower after the intervention than before the intervention, and the range of decline in the intervention group was wider, but the P value (p = 0.142) was not significantly different between the two variables at the 0.05 level. For more details, see Table 3.
Comparisons of illness perceptions between the intervention group and the control group
The results revealed that before the intervention, the total illness perception scores of the two groups were not significantly different (p > 0.05), indicating that the baseline levels of the two groups of patients were comparable. After the intervention, the results revealed that the total score for illness perception was significantly different between the two groups (p < 0.05). These findings suggest that compared with conventional care, nursing interventions based on the common-sense model of self-regulation have greater effect on the perception of negative illness. For more details, see Table 2.
The results revealed that patients in the intervention group had significantly different illness perception scores before and after the intervention (p < 0.001). These findings further indicate that compared with conventional nursing interventions, common-sense model of self-regulation-based nursing interventions are more beneficial for reducing negative illness perceptions. For more details, see Table 3.
Comparisons of lung functional adherence between the intervention group and control group
Before the intervention, the total score of pulmonary function exercise compliance was not significantly different between the two groups (p > 0.05), indicating that the baseline levels of patients in the two groups were comparable.
Compliance with pulmonary function exercise was significantly greater in the experimental group than in the control group after the intervention (t = 5.252; p < 0.001). In addition, the change in pulmonary function exercise compliance in the experimental group before and after the intervention was significant. These findings indicate that compared with conventional nursing interventions, common-sense model of self-regulation-based nursing interventions are more effective at improving compliance with lung function exercises. For more details, see Table 2.
The results revealed that patients in the intervention group (p = 0.022) and the control group (p = 0.003) had significantly different lung function exercise compliance scores before and after the intervention. For more details, see Table 3.
Comparisons of postoperative indicators between the intervention group and control group
The postoperative hospitalization time, total drainage volume and drainage tube retention time were compared between the intervention and control groups, and the postoperative hospitalization time significantly differed (p = 0.005), whereas the total drainage volume and drainage tube retention time did not significantly differ (p > 0.05) (Table 2).
Discussion
This was a nonrandomized controlled trial to explore the effects of nursing interventions based on the common-sense model of self-regulation on pulmonary function exercise adherence. The results supported the hypothesis that a nursing intervention based on the common-sense model of self-regulation can improve compliance with lung function exercise. These findings indicate that the intervention measures based on the common-sense model of self-regulation have a certain effect on thoracoscopic postoperative rehabilitation of patients with lung cancer.
There were no significant differences in the frailty scores across the other outcomes of the intervention according to the common-sense model of self-regulation. A possible reason is that patients with debilitating cancer may need to participate for at least four weeks and reserve rehabilitation training prior to receiving treatment to benefit from these interventions25. A large, long-term randomized data analysis of the effects of physical activity on frailty by Andrea et al. revealed that a 24-month structured, moderate-intensity physical activity program was not associated with a reduced risk of overall frailty in old age26. Physical activity or health education can reduce the burden of frailty27. A 6-month education program effectively improved the physical function, sleep pattern and nutritional status of elderly people in communities with frailty or prefrailty28. A possible reason for this is that those with weakened bodies would benefit more from the intervention. For the clinical lung cancer patients included in this study, after thoracoscopic surgery, the degree of recovery at this stage, such as that resulting in few mental symptoms and complications, was not enough to reach the level of physical and cognitive decline measured by the scale. Therefore, there was no difference in the frailty measurements in our intervention study.
The core goal of nursing interventions based on the common-sense model of self-regulation is to intervene in patients’ illness perceptions to influence behaviours and outcomes29. The common-sense model of self-regulation focuses on the cognition and psychology of diseases/symptoms. In this study, an intervention protocol based on the common-sense model of self-regulation was developed to improve compliance with lung function exercises among lung cancer patients. The protocol addresses disease threats, cognitive–emotional states, and coping strategies encountered by patients after thoracoscopic surgery. The intervention plan underwent two rounds of expert consultation, ensuring its reliability and scientific validity. The results revealed that lung function exercise compliance improved in the intervention group, with a score of 41.22 ± 10.47 (a total score of 60). As in the review by Jones, common-sense model-based interventions are effective at improving compliance behaviour. Six of the nine included studies reported statistically significant improvements in compliance17. Notably, patients in the control group scored lower on lung function exercise compliance than those in the intervention group did, which may indicate that the current education of lung cancer patients after thoracoscopic surgery is insufficient. Many studies have investigated interventions designed to improve adherence to lung function exercises. Naylor’s transitional care model and Hoffman’s perceived symptom self-management theory focused on the continuity of care, a perceived exercise environment and exercise outcomes to promote exercise and thus improve patient outcomes. The self-managed exercise compliance rate increased after six weeks of intervention30. A health belief model can promote respiratory exercise compliance and improve lung function and quality of life in patients with lung cancer after thoracoscopic surgery. This study focused on the effects of breathing exercises and health education on postoperative complications of lung cancer and strengthened the understanding of the relationship between the two, namely, reinforcement motivation intervention. Compliance with lung function exercise was higher in the intervention group than in the control group12. These studies focused on interventions with lung function exercise actions that were effective in terms of outcomes. However, some studies lacked psychological education, some lacked disease education, and more research is needed to focus on specific clinical situations. The treatment of any chronic disease requires physical and mental adjustment. Starting from the overall concept of the common-sense model, this study focused on patients’ disease threat, focusing on the cognition and emotional representation of illness perception and its coping, as well as pulmonary function exercise, which together constitute the intervention. The results showed that this intervention is beneficial to patients’ postoperative rehabilitation behaviour.
In this study, the illness perception and adherence scores before and after the intervention were significantly different. Research indicates that when common-sense models are applied to behavioural change interventions, behaviours are typically assumed to improve through specific theoretical constructs. In such cases, if interventions fail to alter illness perceptions but increase compliance, determining the causal mechanism behind this behavioural change becomes impossible. Alternatively, this model may not be optimal for improving compliance behaviours. However, our study revealed significant differences in illness perception interventions and corresponding compliance changes, indicating that this model can be applied to improve compliance behaviour and that there may be a causal relationship between disease perception and compliance14. A one-month nursing intervention based on self-regulation theory effectively reduced the illness perception level of thyroid cancer patients and significantly improved their quality of life31. Brief psychological intervention after the diagnosis of head and neck cancer could improve patients’ perception of treatment and social quality of life and target patients’ pain intervention to achieve maximum benefits32. After 4 months of nursing intervention, the illness perception level and knee function and functional exercise compliance of elderly patients with knee joints improved33. These findings demonstrate that illness perception interventions based on the common-sense model of self-regulation can effectively improve health behaviours and outcomes. However, it should be noted that current intervention programs developed using this model have varying emphases and inconsistent effectiveness. Future research should focus more on intervention studies to better explore the practical applications of this model.
Postoperative hospital stay, retention time of the thoracoscopic drainage tube and drainage flow are indicators for evaluating patient status after thoracoscopic surgery. The results revealed that the intervention of pulmonary function exercise compliance based on common-sense model of self-regulation had an effect on reducing the hospital stay of lung cancer patients after thoracoscopic surgery, but the retention time and drainage volume of the thoracic drainage tube did not significantly differ between the intervention and control groups. Zhao carried out personalized nursing for 36 patients who underwent thoracoscopic lobectomy, and the results showed that personalized nursing could accelerate patient recovery. Compliance with respiratory rehabilitation exercises, postoperative hospitalization time, drainage tube retention time and postoperative complication rate were significantly lower in the intervention group than in the control group. This study also revealed that the animation education program effectively promoted postoperative rehabilitation in lung cancer patients, and the exercise compliance, incidence of postoperative pulmonary complications, and retention time of the thoracic drainage tube in the intervention group were lower than those in the control group34. Yoga breathing exercises greatly improved lung function recovery and exercise compliance but did not significantly affect drainage tube retention time35. Therefore, the change in the intervention effect on the thoracoscopic drainage rate and retention time may be due to the different contents of the intervention exercise or other reasons, which still need to be explored.
Strengths and limitations of the study
Theoretically, intervention studies based on the common-sense model of self-regulation are relatively rare, and our research contributes to the application of this model. Furthermore, we considered the application of the model as a whole, developing an intervention plan that starts from the disease cognition, emotional characteristics, and coping strategies faced by patients with lung cancer after thoracoscopic surgery, while evaluating rehabilitation behaviour compliance and assessing overall patient condition through frailty assessment. In terms of practice, this intervention promotes behaviours conducive to pulmonary function recovery, and clinical medical staff can draw on relevant information from the intervention to better educate patients about their diseases.
This study had several limitations. As a nonrandomized controlled study, its results are susceptible to potential confounding factors, limiting the power of causal inference. This study combined the common-sense model framework to improve the educational content for postoperative rehabilitation of lung cancer patients undergoing thoracoscopic surgery. We anticipate that future research interventions will be more targeted and personalized and incorporate technological approaches. There is a lack of long-term follow-up data, and the long-term effectiveness of the intervention has yet to be verified. To address these shortcomings, future research should focus on adopting a randomized controlled design, incorporating more comprehensive evaluation indicators, and conducting long-term follow-up assessments, thereby providing more solid and in-depth evidence-based support for intervention studies based on the common-sense model of self-regulation.
Conclusions
The results show that a nursing intervention based on the common-sense model of self-regulation has a positive effect on compliance with lung function exercise in lung cancer patients after thoracoscopic surgery. This study provides a reference for nursing education in lung cancer patients after thoracoscopic surgery.
Data availability
The datasets presented in this article are not readily available. Requests to access the datasets should be directed to jiang178dajishan@163.com. After the research results are published, the original data will be placed on the website http://www.medresman.org.cn/.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J. Clin. 71, 209–249. https://doi.org/10.3322/caac.21660 (2021).
Hardavella, G. et al. Stage I and II nonsmall cell lung cancer treatment options. Breathe (Sheff). 20 https://doi.org/10.1183/20734735.0219-2023 (2024).
Tahiri, M. et al. Enhanced recovery after video-assisted thoracoscopic surgery lobectomy: a prospective, historically controlled, propensity-matched clinical study. Can. J. Surg. 63, E233–e240. https://doi.org/10.1503/cjs.001919 (2020).
Dong, Y. et al. Safety and feasibility of Video-Assisted thoracoscopic day surgery and inpatient surgery in patients with Non-small cell lung cancer: A Single-Center retrospective cohort study. Front. Surg. 8 (779889). https://doi.org/10.3389/fsurg.2021.779889 (2021).
Zhang, W., Zhang, Y., Qin, Y. & Shi, J. Outcomes of enhanced recovery after surgery in lung cancer: A systematic review and meta-analysis. Asia-Pacific J. Oncol. Nurs. 9 (100110). https://doi.org/10.1016/j.apjon.2022.100110 (2022).
Batchelor, T. J. P. et al. Guidelines for enhanced recovery after lung surgery: recommendations of the enhanced recovery after surgery (ERAS®) society and the European society of thoracic surgeons (ESTS). Eur. J. Cardiothorac. Surg. 55, 91–115. https://doi.org/10.1093/ejcts/ezy301 (2019).
Ren, J. et al. Systematic review and meta-analysis of breathing exercises effects on lung function and quality of life in postoperative lung cancer patients. J. Thorac. Dis. 16, 4295–4309. https://doi.org/10.21037/jtd-23-1733 (2024).
Tao, W., Huang, J., Jin, Y., Peng, K. & Zhou, J. Effect of pulmonary rehabilitation exercise on lung volume and respiratory muscle recovery in lung cancer patients undergoing lobectomy. Altern. Ther. Health Med. 30, 90–96 (2024).
Nilsen, T. S. et al. Novel methods for reporting of exercise dose and adherence: an exploratory analysis. Med. Sci. Sports Exerc. 50, 1134–1141. https://doi.org/10.1249/mss.0000000000001545 (2018).
Romero-Ruiz, L., Cuña-Carrera, D., Alonso-Calvete, I., González-González, Y. & A. & Effects of therapeutic exercises in patients with lung cancer. A scoping review. J. Bodyw. Mov. Ther. 31, 22–29. https://doi.org/10.1016/j.jbmt.2022.03.003 (2022).
Gu, X. et al. Illness perception and lung functional exercise adherence in lung cancer patients after thoracoscopic surgery. Patient Prefer Adherence. 17, 2773–2787. https://doi.org/10.2147/ppa.S435944 (2023).
Hu, X. Y., Yang, Y., Zheng, L. L. & Lin, Q. Effect of health belief model on respiratory exercise compliance and lung function in patients with lung cancer. J. Nurses Train. 36, 1042–1044. https://doi.org/10.16821/j.cnki.hsjx.2021.11.017 (2021).
Ha, D. M. et al. Telemedicine-based inspiratory muscle training and walking promotion with lung cancer survivors following curative intent therapy: a parallel-group pilot randomized trial. Support Care Cancer. 31 https://doi.org/10.1007/s00520-023-07999-7 (2023).
McAndrew, L. M. et al. Using the common sense model to design interventions for the prevention and management of chronic illness threats: from description to process. Br. J. Health. Psychol. 13, 195–204. https://doi.org/10.1348/135910708x295604 (2010).
Leventhal, H., Phillips, L. A. & Burns, E. The Common-Sense model of Self-Regulation (CSM): a dynamic framework for Understanding illness self-management. J. Behav. Med. 39, 935–946. https://doi.org/10.1007/s10865-016-9782-2 (2016).
Hagger, M. S. & Orbell, S. The common sense model of illness self-regulation: a conceptual review and proposed extended model. Health Psychol. Rev. 16, 347–377. https://doi.org/10.1080/17437199.2021.1878050 (2022).
Jones, C. J., Smith, H. E. & Llewellyn, C. D. A systematic review of the effectiveness of interventions using the common sense Self-Regulatory model to improve adherence behaviours. J. Health Psychol. 21, 2709–2724. https://doi.org/10.1177/1359105315583372 (2016).
Gu, X., Shen, X., Zhou, J. R., Chu, J. H. & Jiang, L. The effects of common-sense model interventions on cancer patients: A systematic review. Med. (Baltim). 103, e37777. https://doi.org/10.1097/md.0000000000037777 (2024).
Vigorè, M. et al. Cognitive impairment, frailty and rehabilitation outcome in older cardiorespiratory patients. DEC_FRAinRIAB: Study Protoc. PLoS 17, e0272132. https://doi.org/10.1371/journal.pone.0272132 (2022).
Kucukarslan, S. N. A review of published studies of patients’ illness perceptions and medication adherence: lessons learned and future directions. Res. Social Adm. Pharm. 8, 371–382. https://doi.org/10.1016/j.sapharm.2011.09.002 (2012).
Yuan, Z., Gao, L., Zheng, M., Ye, X. & Sun, S. Effect of multimodal health education combined with the feedback method in perioperative patients with lung cancer: A randomised controlled study. Patient Prefer Adherence. 17, 413–420. https://doi.org/10.2147/PPA.S394826 (2023).
Mullen, P. M. Delphi: Myths and reality. J. Health Organ. Manag. 17, 37–52. https://doi.org/10.1108/14777260310469319 (2003).
Mei, Y. Q. et al. Reliability and validity of simplified version of Chinese version of disease perception questionnaire in female breast cancer patients. J. Nurs. (China). 22, 11–14. https://doi.org/10.16460/j.issn1008-9969.2015.24.011 (2015).
Li, J. et al. Impact of an animation education program on promoting compliance with active respiratory rehabilitation in postsurgical lung cancer patients. Cancer Nurs. 44, 106–115. https://doi.org/10.1097/ncc.0000000000000758 (2021).
McIsaac, D. I. et al. Home-based prehabilitation with exercise to improve postoperative recovery for older adults with frailty having cancer surgery: the PREHAB randomised clinical trial. Br. J. Anaesth. 129, 41–48. https://doi.org/10.1016/j.bja.2022.04.006 (2022).
Trombetti, A. et al. Effect of physical activity on frailty. Ann. Intern. Med. 168, 309–316. https://doi.org/10.7326/m16-2011 (2018).
Quach, J. et al. Effect of a physical activity intervention and frailty on frailty trajectory and major mobility disability. J. Am. Geriatr. Soc. 70, 2915–2924. https://doi.org/10.1111/jgs.17941 (2022).
Casals, C. et al. Effects of an educational intervention on frailty status, physical function, physical activity, sleep patterns, and nutritional status of older adults with frailty or pre-frailty: the FRAGSALUD study. Front. Public. Health. 11, 1267666. https://doi.org/10.3389/fpubh.2023.1267666 (2023).
Kong, Y., Tang, T., Cha, H. X., Dou, B. & Liu, K. Y. Visualized analysis of research hotspots and evolution of common sense model. Chin. J. Mod. Nurs. 28, 1573–1579. https://doi.org/10.3760/cma.j.cn115682-20210813-03589 (2022).
Hoffman, A. J. et al. Using perceived Self-efficacy to improve fatigue and fatigability in postsurgical lung cancer patients: A pilot randomized controlled trial. Cancer Nurs. 40, 1–12. https://doi.org/10.1097/ncc.0000000000000378 (2017).
Huang, Y. H. Effects of Intervention on Illness Perception and Quality of Life in Thyroid Cancer Patients Based on Self-regulation Model Master thesis. Nanhua University, (2021). https://doi.org/10.27234/d.cnki.gnhuu.2021.000346
Richardson, A. E., Tennant, G., Morton, R. P. & Broadbent, E. A. Self-Regulatory intervention for patients with head and neck cancer: pilot randomized trial. Ann. Behav. Med. 51, 629–641. https://doi.org/10.1007/s12160-017-9885-1 (2017).
Liu, S. Y. The Influence of Nursing Intervention based on Self-Regulatory Model for Illness perception in Elderly Patients with Knee Arthroplasty. Zhengzhou University, (2021). https://doi.org/10.27466/d.cnki.gzzdu.2021.002197
Zhao, L., Liu, Z., Li, L., Ma, L. & Chen, X. Effects of perioperative individualized nursing on elderly patients undergoing video–assisted thoracoscopic lobectomy. Exp. Ther. Med. 25 https://doi.org/10.3892/etm.2023.11929 (2023).
Lu, H. B. et al. Clinical indicators of effects of yoga breathing exercises on patients with lung cancer after surgical resection: A randomized controlled trial. Cancer Nurs. 47 (158), E151–E. https://doi.org/10.1097/ncc.0000000000001208 (2023).
Acknowledgements
The authors thank all patients who participated in this study. In addition, the authors express their sincere gratitude to the expert correspondence with specialists, nursing staff implementing intervention programs, for providing technical support for the development of the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Xue Gu contributed in the conceptualization, formal analysis, investigation, methodology, writing – original draft, writing – review & editing. Lei Jiang contributed in the conceptualization, formal analysis, methodology, validation, writing – review & editing. Yin Dou contributed in the conceptualization, formal analysis, validation, writing –original draft. Ping Cai contributed in the data curation, methodology. Jianghui Chu contributed in the investigation, validation. Yanling Huang contributed in the writing – review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Disclosure of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gu, X., Jiang, L., Dou, Y. et al. Effectiveness of an educational intervention based on the common-sense model of self-regulation for lung cancer patients after thoracoscopic surgery. Sci Rep 15, 44833 (2025). https://doi.org/10.1038/s41598-025-29106-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-29106-y