Abstract
Collateral channel wiring (CCW) is important in a retrograde chronic total occlusion (CTO) procedure. However, the guidance is insufficient. To investigate the optimal CCW time, patients who had received retrograde CTO procedures were enrolled. The optimal CCW time was derived by Receiver Operating Characteristic curves regarding success rates or complications. The clinical outcomes in terms of success and complication rates were addressed by cutoff value of optimal CCW time. With cutoff values of 25 min, 191 (54.9%) had shorter CCW times and 157 (45.1%) had longer CCW times. The success rates were significantly higher in the group with shorter CCW times than in the group with longer CCW times (p < 0.05). Procedure-related myocardial infarction (MI) and collateral channel (CC) related complications were more frequently observed in longer CCW times group than shorter group. The CCW time less than 25 min was more likely to result in a technical success (adjusted odds ratio [aOR]: 3.69) and the odds of CC perforation decreased by approximately 80% (aOR: 0.20). A CCW time of less than 25 min may facilitate the success results and minimize the risk of complications in retrograde CTO procedures.
Similar content being viewed by others
Introduction
For chronic total occlusion (CTO) procedures, the retrograde approach is an important step for improving technical success1,2. According to current guidelines, retrograde approach is recommended when antegrade attempts have failed (rescue retrograde approach). Alternatively, if a CTO lesion exhibits anatomical characteristics – such as an ambiguous proximal cap, absence of a stump, or the presence of bridging collaterals – that render an antegrade-only approach less likely to succeed, and suitable interventional collateral channels (CCs) are available, a primary retrograde approach may be selected3,4.
The retrograde approach requires collateral channel wiring (CCW), which requires a comprehensive assessment of the characteristics of the collateral channel (CC) and expert skills to cross it. Over time, novel devices that can cross the CC have been developed, and new techniques have been matured. However, still many interventionists are in trouble to overcome this barrier due to some difficulties for CC crossing and increasing the risk of CC-related complications.
Studies on the optimal selection of suitable CCs, guidewires, or microcatheters have been conducted over the last decade5,6,7,8. However, to the best of our knowledge, data on the optimal CCW time for CTO percutaneous coronary intervention (CTO-PCI) are very limited, leading to a lack of guidance. In the present study, we evaluated the characteristics and procedural outcomes based on CCW time, with a focus on the optimal CCW time that ensures an effective and safe procedure.
Methods
Study population
This study was a retrospective analysis of prospectively collected data from the Asan Medical Center-CTO registry. The design and eligibility criteria of this registry have been previously reported9,10. The registry included patients who underwent CTO-PCI. CTO-PCI was performed by three high-volume dedicated operators (S.W Lee, J.Y Lee, and P.H Lee). In this study, all patients who underwent procedure via the retrograde approach were eligible for CCW time analysis. This study was approved by the institutional review board of Asan Medical Center, and all patients provided written informed consent. All methods were performed in accordance with the relevant guidelines and regulations.
Procedure
The retrograde approach was selected at the discretion of the operator. A primary retrograde approach was generally employed when lesion characteristics—such as an ambiguous proximal cap, absence of a proximal stump, or the presence of bridging collaterals—were considered unfavorable for an antegrade-only attempt. Conversely, a rescue retrograde approach was adopted when initial antegrade attempts failed. All decisions were made based on angiographic assessment and operator judgment in real-world clinical practice. Using data from this registry, we previously reported that 191 (54.3%) and 161 (45.7%) retrograde procedures were performed as primary and rescue retrograde approaches, respectively11.
Definitions and endpoints
The retrograde CTO-PCI was defined as an attempt to cross the CC. CCW time was defined as the time from initial insertion of the guidewire into the CC to the successful crossing of the guidewire through the CC or the guidewire being pulled out of the CC due to crossing failure. Technical success was defined as an achieving Thrombolysis in Myocardial Infarction (TIMI) 3 flow with ≤ 30% stenosis in the residual diameter of the treated vessel. Procedural success was defined as technical success without any in-hospital major adverse events. In-hospital major adverse events included any of the following adverse events during the index hospitalization: death; myocardial infarction (MI); repeat target vessel revascularization (TVR); or cerebrovascular attack (CVA)12. Periprocedural MI was defined as peak elevations of the creatine kinase-myocardial band exceeding 10 times the upper reference limit within 48 h post-procedure13. Contrast-induced nephropathy (CIN) Contrast-induced nephropathy (CIN) was defined as a ≥ 25% increase in serum creatinine or an absolute increase of ≥ 0.5 mg/dL from baseline within 48–72 h post-procedure. Procedural outcomes included technical and procedural success rates, in-hospital major adverse events, CIN and CC-related complications (cardiac tamponade, pericardial effusion without cardiac tamponade, CC perforation or hematoma). Post-procedural transthoracic echocardiography (TTE) was not performed routinely on all patients. In accordance with standard clinical practice, TTE was performed promptly when a complication was suspected based on specific clinical signs or symptoms, including: injury in a coronary artery (including a CC), hemodynamic instability, persistent chest pain, or relevant ECG changes.
Statistical analysis
Categorical variables are represented as numbers (percentages) and were analyzed using χ2 statistics or Fisher’s exact test. Continuous variables are reported as the mean (standard deviation [SD]) or median (interquartile range [IQR]) and were analyzed using Student’s t test or the Wilcoxon rank sum test, as appropriate. Receiver operating characteristic (ROC) curve analyses were performed to assess the optimal cutoff values for CC crossing time for predicting efficacy or safety outcomes. Subsequently, baseline characteristics and procedural outcomes were compared between patients with CCW times above and below this optimal cutoff. Pearson correlation analyses were performed to assess the relationship between CCW time and total procedure time, as well as procedure time excluding CCW time in a subgroup of patients with successful CTO-PCI. To evaluate whether the effect of collateral channel wiring (CCW) time on procedural outcomes differed between the earlier and later periods of the study, we performed a subgroup analysis stratified by the procedural wave (Wave 1 vs. Wave 2). Logistic regression analysis was used to identify the predictors of a CC crossing times less than 25 min and the odds ratios (ORs) of shorter CCW times (< 25 min) for procedural outcomes. Variables with P values < 0.1 in the univariate analyses (septal CC, tortuous CC, and small CC) were included in the multivariate model. However, variable of Werner’s classification was not included in the final model due to the multilinearity problem. Statistical analysis was performed using the Statistical Package for Social Sciences version 21 (SPSS Inc., Chicago, IL, USA). Two-sided P values < 0.05 were considered significant.
Results
Baseline characteristics
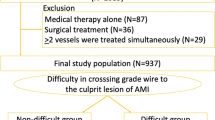
Of 1619 CTO-PCI procedures performed between January 2007 and January 2019, 352 cases were retrograde CTO-PCI. Four patients with unavailable CCW data were excluded from this study, leaving 348 procedures for the final analysis (Fig. 1). Among a total of study population, technical success rates were 87.6% (305/348 patients; 88.5% via septal CC and 85.2% via non-septal CC, p = 0.43, Supplementary Table 6). CC crossing were successfully done in 276 (79.3%) patients, while 72 (20.7%) patients did not. There was a significant difference in procedural outcomes between the successful CC wiring group and the failed CC wiring group in terms of success rates and CC perforation (Supplementary Table 1). ROC curve analysis for predicting those clinical events revealed that the areas under the curve (AUC) of CCW time were 0.724 (95% confidence interval [CI] 0.63–0.81, p < 0.001) for CC perforation and 0.669 (95% CI 0.58–0.76, p = 0.004) for technical failure (Fig. 2). A CCW time of 25 min was the cutoff value for the increased risk of CC perforation, which was not only a key safety outcome, but also a factor that played an important role in the procedural success.
Population flow. Procedural outcomes and complications were evaluated based on collateral channel wiring (CCW) times in chronic total occlusion-percutaneous coronary intervention (CTO-PCI). Efficacy outcomes included success rates (technical success and procedural success), and safety outcomes included in-hospital major adverse events and collateral channel (CC)-related complications. CCW, collateral channel wiring; CTO-PCI, chronic total occlusion-percutaneous coronary intervention; MI, myocardial infarction; CC, collateral channel.
Receiver operating characteristic curves for CCW times as a Cutoff for predicting success and complications in CTO-PCI. Receiver operating characteristic (ROC) curves demonstrating the use of collateral channel wiring (CCW) time as a cutoff for predicting (A) CCW success, (B) technical failure, and (C) collateral channel perforation. The optimal cutoff values are indicated by the arrows: 28.5 min for both CCW success and technical failure, and 24.5 min for collateral channel perforation. CCW, collateral channel wiring; CTO-PCI, chronic total occlusion-percutaneous coronary intervention.
One hundred ninety-one patients had shorter CCW times (< 25 min) and 157 patients had longer CCW times (≥ 25 min). Clinical, lesion, and procedural characteristics were represented and analyzed based on CCW time (Tables 1 and 2). There were no differences in clinical characteristics between the two groups, except for peripheral artery disease. A history of peripheral artery disease was significantly more frequently observed in the group with longer CCW times than shorter CCW group (8 [5.1%] vs. 3 [1.6%], p = 0.07). There were no differences in lesion or procedural characteristics, especially in terms of target CTO locations or Japanese CTO (J-CTO) scores.
Favorable CC features are important for successful CC crossing (less than 25 min)
As represented in Table 3, unfavorable CC features (tortuous, small) were frequently observed in the group with longer CCW times (tortuous CC: p = 0.002, small CC: p < 0.001). Similarly, Werner’s grade 2 CCs were more common in the group with shorter CCW times than in the group with longer CCW times (p < 0.001). In Supplement Table 2, we demonstrated that the favorable features of the CC were independent predictors of a shorter CC crossing time (< 25 min), which included ‘not tortuous’ or ‘large (≥ 1 mm)’ CCs.
Procedural outcomes
The correlation analysis showed that CCW time was positively correlated with total procedure time (Pearson r = 0.224, p < 0.001). As expected, the longer CCW group was associated with a significantly longer total procedure time (166.8 ± 60.5 vs. 142.0 ± 55.4 min, p < 0.001). Since CCW time contributes to total procedure time, it could bias the assessment of procedural efficiency. Therefore, we evaluated the subsequent procedure time, excluding CCW time. To avoid potential bias from early termination in failed cases, we performed a subgroup analysis limited to successful procedures. However, the duration of the subsequent procedure did not differ between the two groups (p = 0.83, Table 4). This confirmed no significant correlation between CCW time and the remaining procedure time (r = − 0.034, p = 0.56), suggesting that procedural delay was primarily attributable to the CC wiring phase itself.
We also found that the success rate was higher in the group with shorter CCW times than in the group with longer CCW times (technical success: 92.1% vs. 82.2%, p = 0.005; procedural success: 86.9% vs. 74.5%, p = 0.003, Fig. 3). Periprocedural MI, CC perforation and CC hematoma occurred less frequently in the group with shorter CCW times than in those with longer CCW times (periprocedural MI: 2.6% vs. 7.0%, p = 0.052; CC perforation: 3.1% vs. 16.6%, p < 0.001; CC hematoma: 1.0% vs. 5.1%, p = 0.048) (Table 4; Fig. 3).
Procedural outcomes based on CCW times. A CCW time of 25 min was used as the cutoff. Shorter CCW times (< 25 min) were associated with higher technical and procedural success rates, as well as lower complication rates compared to longer CCW times (≥ 25 min). CCW, collateral channel wiring; CWT, collateral channel wiring time; MI, myocardial infarction; CI, confidence interval.
As shown in Supplement Table 3, the procedural outcomes were stratified as successful or failed CC wire crossing according to CCW time. Among cases in which CC crossing failed, patients with longer CCW times experienced higher rates of periprocedural MI (3 [5.5%] vs. 0) and CC-related complications (cardiac tamponade : 1 [1.8%] vs. 0, pericardial effusion : 2 [3.6%] vs. 0, CC perforation : 12 [21.8%] vs. 2 [11.8%], and CC hematoma : 4 [7.3%] vs. 0), compared with those with shorter CCW times.
As shown in Fig. 4, we calculated the adjusted ORs of shorter CCW times for procedural outcomes (Table 5). The adjusted ORs of shorter CCW times compared with longer CCW times for technical and procedural success were 3.69 (95% CI 1.71–7.98, p = 0.001) and 2.96 (95% CI 1.60–5.47, p = 0.001), respectively. In contrast, the adjusted ORs for periprocedural MI, CC perforation and CC hematoma were 0.24 (95% CI 0.07–0.83, p = 0.024), 0.20 (95% CI 0.08–0.52, p = 0.001) and 0.20 (95% CI 0.04–0.95, p = 0.043), respectively.
Impact of Collateral Channel Wiring Time on CTO-PCI Outcomes. This figure highlights the impact of collateral channel wiring (CCW) time on the efficacy and safety outcomes in chronic total occlusion-percutaneous coronary intervention (CTO-PCI). Shorter CCW times (< 25 min) are associated with higher technical success (odds ratio 3.69, 95% CI 1.71–7.98) and procedural success (odds ratio 2.96, 95% CI 1.60–5.47). They are also associated with lower rates of collateral channel (CC) perforation (odds ratio 0.20, 95% CI 0.08–0.52) and periprocedural myocardial infarction (MI) (odds ratio 0.24, 95% CI 0.04–0.95). The illustration shows coronary anatomy, including the aorta (Ao), right coronary artery (RCA), left anterior descending artery (LAD), and a collateral channel crossing a chronic total occlusion (CTO). The inset highlights a wire and microcatheter causing a perforation, underscoring the increased risks associated with longer CCW times. CCW, collateral channel wiring; CTO-PCI, chronic total occlusion-percutaneous coronary intervention; MI, myocardial infarction; CC, collateral channel; Ao, aorta; RCA, right coronary artery; LAD, left anterior descending artery.
Subgroup analysis according to study periods (Wave 1: 2007 ~ 2012, Wave 2: 2013 ~ 2019).
As shown in Supplementary Table 4, a p-value for interaction was calculated to formally test for any significant effect modification by the procedural period. No significant P for interaction was observed between wave 1 and wave 2, suggesting that the main outcomes were consistent across the two waves.
Specific CTO crossing techniques
We also analyzed the specific CTO crossing techniques utilized after successful CC crossing (Supplementary Table 5). The use of complex techniques, such as reverse CART, CART, or the parallel wire technique, did not significantly differ between the groups with shorter and longer CCW times. The kissing wire technique was more frequently observed in the shorter CCW time group, while the single antegrade wire technique was more common in the longer CCW time group.
Discussion
Using the retrograde CTO-PCI data, we investigated the optimal CCW time for enhancing the success rate and reducing the incidences of periprocedural MI and CC-related complications. Because all procedures were performed via a retrograde approach due to complex CTO lesions, the findings of this study supply the appropriate guidance for CC tracking in retrograde CTO-PCI.
Retrograde CTO-PCI has been improved as a result of the development of new devices (wires and microcatheters), optimized techniques and the accumulation of experiences with current updated CTO algorithms, which have led to favorable outcomes14,15,16,17. However, the rates of complications are higher with the retrograde approach than with the antegrade-only approach, especially during CC wiring18. For this reason, many operators still tend to prefer the antegrade approach, which leads to complex CTO-PCI procedures failing or being inefficient in terms of procedure time, radiation dose or used contrast amount11. To address this gap between guideline recommendations and real-world practice, we conducted this study to provide operators with practical information to compensate for the lack of guidance for CCW strategies.
Indeed, CC injury during retrograde CTO-PCI usually does not cause serious problems and resolves without any treatment. However, it can sometimes be fatal due to cardiac tamponade requiring emergent pericardiocentesis or surgery. According to the results of our study, CC perforation occurred in 32 patients (9.2%). Among them, only one patient with cardiac tamponade required surgical treatment, while 3 patients with pericardial effusion did not require further treatment but were managed with close observation. Although fatal complications are rare, operators should remain vigilant, as CTO-PCI is typically performed in clinically stable patients to relieve anginal symptoms or to improve the function of viable myocardium. Regarding the safety of retrograde CTO-PCI, our results can be incorporated into our clinical practice - a shorter (less than 25 min) CCW time is associated with a higher success rate and a lower chance of CC perforation or hematoma.
We represented the magnitude of the adjusted ORs for efficacy and safety outcomes. Compared with a longer CCW times, a CCW time less than 25 min was more likely to result in technical or procedural success (adjusted odds ratio: 3.69 for technical success, 2.96 for procedural success). Moreover, compared to those in the group with longer CCW times, the odds of CC perforation or periprocedural MI decreased by approximately 80% (adjusted odds ratio: 0.20 for CC perforation, 0.24 for periprocedural MI). Additionally, by stratifying procedural outcomes by successful or failed CC wire crossing, we found that there were consistently more chances of periprocedural MI and CC-related complications in the group with longer CCW times than in the group with shorter CCW times. Notably, there were no cases of in-hospital MACCEs and only 2 cases of CC perforation in the group with shorter CCW times even among patients with failed CC crossing. Therefore, if it is difficult for the wire to cross the CC, we may need to reassess the CC and reapproach it carefully while considering other treatment strategies within 25 min. These results suggest that operators should plan CC tracking through comprehensive assessment and selection of the optimal CC before procedure and prepare other treatment options as well.
While our interaction analysis confirmed that the overall impact of CCW time on outcomes was consistent across both waves (Pinteraction > 0.05), it is still worth noting the clear descriptive improvements over time in terms of success rate. Notably, the increase was more substantial in the longer CCW time group, with technical success rising from 79.8% to 84.9% and procedural success from 71.4% to 78.1%. It is noteworthy that no instances of urgent revascularization, in-hospital CVA, or major collateral-related complications (cardiac tamponade, pericardial effusion) occurred in wave 2. This suggests that the procedural safety of CC tracking has substantially improved, like reflecting the positive real-world impact of accumulated operator experience and the adoption of new devices like ‘SUOH 03’ and ‘Sion Black’ wires.
With this optimal CCW time, the best selection of CC is important for ensuring the wire crosses the CC. To date, there have been several studies on this issue. Huang et al. reported that large size (Werner grade 2 CCs with continuous, small side branch-like structures throughout the course)19 and lack of tortuosity of the CC are independent predictors of successful CC tracking20. Using an epicardial CC, the independent predictors of procedure success were reported, which included CC tortuosity, CC size (> 0.9 mm), side branch at CC tortuosity, and inadequate CC exit location (< 5 mm distal to the CTO segment)21. Nagamatsu et al. developed the J-channel score, which is a tool for estimating the success of CC wire crossing6. Authors emphasized the importance of CC size and understanding the anatomy of the CC, such as continuous bends, reverse bends, or corkscrews stratified by septal or non-septal CCs. These results were in line with our study.
One of the most clinically significant findings of our study is the dynamic and distinct safety profiles of different CC types. Overall, we observed no significant difference in procedural efficiency, such as CCW time or technical success rates. However, the incidence of complications was markedly higher in the epicardial CCs (Supplementary Table 6) compared to septal CCs.
In the shorter CCW group, the rate of periprocedural MI was significantly higher in epicardial CCs compared to septal CCs, while the rates of CC perforation were comparable between the groups. In the longer CCW group, the rate of CC perforation in epicardial CCs was more than doubling that in the septal CCs (26.1% vs. 12.6%, p = 0.039). In these difficult cases, the difference in periprocedural MI rates became non-significant, as the rate in the septal CC group also increased with prolonged CCW time. Taken together, these findings provide a robust, multifaceted rationale for a “septal-first” strategy.
Limitations
This study has several limitations. First, as a retrospective study, it was not feasible to analyze every procedural details. While operators typically save the fluoroscopic images of successful or complicated CCs, failed attempts are often not documented. This practice makes it impossible to reliably quantify the exact number or types of CCs attempted or to analyze the unfavorable characteristics of every CC explored. To overcome this limitation, we utilized CCW time as a more comprehensive surrogate variable. Second, the generalizability of our findings may be limited. Patients with significantly reduced left ventricular function (EF < 40%) were seldom included. Caution is warranted when applying these results to cases involving patients with severely impaired systolic function. Third, the study was conducted over a long enrollment period (more than 10 years), during which devices, techniques, and medications may have evolved. To evaluate the influence of these temporal changes on our outcomes, we performed an interaction analysis between the two waves. The results showed no significant interaction between the study period and the primary findings of our study (p for interaction > 0.05), suggesting that the effect of our main predictors on outcomes was consistent over time. Fourth, while our study identified important differences in complication profiles between septal and non-septal (mainly epicardial) CCs, the relatively small sample size of the non-septal group (n = 88) limited the statistical power for a fully stratified multivariable analysis based on channel type.
Conclusion
In retrograde CTO-PCI, CCW time is a critical determinant of both technical success and patient safety. Our study establishes a 25-minute cut-off for CCW time, as longer wiring times are associated with a lower success rate and a significantly higher risk of complications, particularly CC perforation. These findings suggest that operators should consider reassessing their approach or choosing an alternative strategy as this threshold is approached. Ultimately, integrating this optimal CCW time with a septal-first approach is expected to lead to safer and more efficient retrograde CTO-PCI.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- CCW:
-
collateral channel wiring
- CI:
-
confidence interval
- CIN:
-
contrast-induced nephropathy
- CTO:
-
chronic total occlusion
- CTO-PCI:
-
chronic total occlusion-percutaneous coronary intervention
- CVA:
-
cerebrovascular attack
- J-CTO:
-
Japanese chronic total occlusion
- MACCE:
-
major adverse cardiac and cerebrovascular events
- MI:
-
myocardial infarction
- OR:
-
odds ratio
- ROC:
-
receiver operating characteristic
- TIMI:
-
Thrombolysis in Myocardial Infarction
- TVR:
-
target vessel revascularization
References
Patel, V. G. et al. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc. Interv. 6, 128–136 (2013).
Kwon, O. et al. Retrograde approach for the percutaneous recanalisation of coronary chronic total occlusions: contribution to clinical practice and long-term outcomes. EuroIntervention 15, e354–e361 (2019).
Wu, E. B. et al. Global chronic total occlusion crossing algorithm: JACC State-of-the-Art review. J. Am. Coll. Cardiol. 78, 840–853 (2021).
Tanaka, H. et al. A novel algorithm for treating chronic total coronary artery occlusion. J. Am. Coll. Cardiol. 74, 2392–2404 (2019).
Zhong, X. et al. Microcatheter collateral channel tracking failure in retrograde percutaneous coronary intervention for chronic total occlusion: incidence, predictors, and management. EuroIntervention 15, e253-e260 (2019).
Nagamatsu, W. et al. Successful guidewire crossing via collateral channel at retrograde percutaneous coronary intervention for chronic total occlusion: the J-Channel score. EuroIntervention 15, e1624–e1632 (2020).
Wang, Y. et al. Active Retrograde Extra Backup with a Mother-and-Child Catheter to Facilitate Retrograde Microcatheter Collateral Channel Tracking in Recanalization of Coronary Chronic Total Occlusion. J Interv Cardiol 4245191 (2020). (2020).
Wu, K., Luo, B., Huang, Z. & Zhang, B. Simplified Dual-Lumen Catheter-Facilitated reverse wire technique for markedly angulated collateral channel entry in retrograde chronic total occlusion intervention. Int. Heart J. 62, 416–421 (2021).
Lee, P. H. et al. Successful recanalization of native coronary chronic total occlusion is not associated with improved Long-Term survival. JACC Cardiovasc. Interv. 9, 530–538 (2016).
Lee, P. H. et al. Full metal jacket with Drug-Eluting stents for coronary chronic total occlusion. JACC Cardiovasc. Interv. 10, 1405–1412 (2017).
Lee, K. et al. Primary versus rescue retrograde approach for chronic total coronary occlusion. Catheter Cardiovasc. Interv. 99, 219–225 (2022).
Karmpaliotis, D. et al. Outcomes with the use of the retrograde approach for coronary chronic total occlusion interventions in a contemporary multicenter US registry. Circ. Cardiovasc. Interv. 9 10.1161/CIRCINTERVENTIONS.1115.003434e003434 (2016).
Moussa, I. D. et al. Consideration of a new definition of clinically relevant myocardial infarction after coronary revascularization: an expert consensus document from the society for cardiovascular angiography and interventions (SCAI). J. Am. Coll. Cardiol. 62, 1563–1570 (2013).
Nikolakopoulos, I. et al. Equipment utilization in chronic total occlusion percutaneous coronary interventions: insights from the PROGRESS-CTO registry. Catheter Cardiovasc. Interv. 97, 658–667 (2021).
Whitlow, P. L. et al. Use of a novel crossing and re-entry system in coronary chronic total occlusions that have failed standard crossing techniques: results of the FAST-CTOs (Facilitated antegrade steering technique in chronic total Occlusions) trial. JACC Cardiovasc. Interv. 5, 393–401 (2012).
Carlino, M., Demir, O. M., Colombo, A. & Azzalini, L. Microcatheter knuckle technique: A novel technique for negotiating the subintimal space during chronic total occlusion recanalization. Catheter Cardiovasc. Interv. 92, 1256–1260 (2018).
Walsh, S. J., Cosgrove, C., Spratt, J. C. & Hanratty, C. G. A technical focus on antegrade dissection and Re-entry for coronary chronic total occlusions: a practice update for 2019. Korean Circ. J. 49, 559–567 (2019).
Megaly, M. et al. Outcomes with retrograde versus antegrade chronic total occlusion revascularization. Catheter Cardiovasc. Interv. 96, 1037–1043 (2020).
Werner, G. S. et al. Angiographic assessment of collateral connections in comparison with invasively determined collateral function in chronic coronary occlusions. Circulation 107, 1972–1977 (2003).
Huang, C. C. et al. Collateral channel size and tortuosity predict retrograde percutaneous coronary intervention success for chronic total occlusion. Circ. Cardiovasc. Interv. 11, e005124 (2018).
Huang, Z. et al. Epicardial collateral channel for retrograded recanalization of chronic total occlusion percutaneous coronary intervention: predictors of failure and procedural outcome. J. Interv Cardiol. 31, 23–30 (2018).
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
Kyusup Lee and Tae Oh Kim conceptualization, data curation, project administration, formal analysis, methodology, Writing – Original Draft Preparation, Woojin Kwon visualization, Yong-Hoon Yoon, Osung Kwon and Jong-Young Lee resources, data curation, supervision, validation, Pil Hyung Lee methodology, supervision, formal analysis, Writing – Review & Editing, Soo-Jin Kang conceptualization, methodology, supervision, Writing – Review & Editing, Young-Hak Kim, project administration, Writing – Review & Editing, Cheol Whan Lee resources, Writing – Review & Editing, Seung-Whan Lee conceptualization, methodology, project administration, supervision, validation, formal analysis, Writing – Review & Editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Disclosures
The sponsors played no role in this study. There was no industry involvement in the design or conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; or decision to submit the manuscript for publication. The authors have no conflicts of interest or financial disclosures to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, K., Kim, T.O., Kwon, W. et al. Optimal time for collateral channel wiring in retrograde chronic total occlusion percutaneous coronary intervention. Sci Rep 16, 931 (2026). https://doi.org/10.1038/s41598-025-30503-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-30503-6