Abstract
In the case of humeral shaft aseptic nonunions treatment with the Ilizarov apparatus can achieve optimal results. We included 21 patients (10 females and 11 males), who underwent posttraumatic humeral nonunion treatment at the Orthopedics and Musculoskeletal Trauma Surgery, Medical University of Warsaw, in the period between 2011 and 2023. Patient age ranged from 21.0 to 68.0 years, with a median age of 42.3 years. Clinical and radiological pre- and postoperative records were collected, including the radiological Weber and Pech and Paley classifications, as well as questionnaires validated in Polish, such as the Shoulder Strength Index, the University of California–Los Angeles (UCLA) Shoulder Scale, and the Constant Score. Study evaluated the duration of treatment with an Ilizarov apparatus, the rates of achieved and maintained bone union, changes in questionnaire scores and the radiological and functional outcomes measured with an Association for the Study and Application of the Method of Ilizarov scoring systems. All methods were carried out in accordance with available relevant guidelines and regulations.
The study protocol was approved by the Supervisor of the WUM Department and the Warsaw Medical University. Informed consent was obtained from each patient. 90% of patients achieved bone union maintained during 12-month follow-up. The ASAMI scores reveal that the majority of patients achieved ‘very good’ outcomes. The median UCLA scores improved from 11.0 to 31.0 (p < 0.001), the Constant scores rose from 28 to 94 (p < 0.001), the SSI-ASES scores demonstrated increases from 43 to 95 (p < 0.001). The most common complications were Kirschner wire-track infections (8 cases). The use of the Ilizarov apparatus is recommended in patients with coexisting nonunion and ones with bone segment deformity or shortening. The preferred closed reduction approach is dedicated for patients with chronic conditions in whom an open approach might result in delayed surgical wound healing or surgical site infection.
Similar content being viewed by others
Introduction
Humeral shaft nonunion occurs in 0.3–13% of all humeral shaft fractures1,2. Posttraumatic nonunion, or pseudoarthrosis, of the humerus results in chronic pain, upper limb dysfunction, decreased quality of life, and long-term absence from work1,3.
Factors that produce problems with bone union include smoking, alcohol abuse, certain medications (such as corticosteroids and nonsteroidal anti-inflammatory drugs), comorbidities, incorrect fracture immobilization, or incorrect fixation1,4.
The surgical treatment approach depends on the type of nonunion. Hypertrophic nonunion requires only bone fragment fixation. Atrophic nonunion additionally requires bone fragment contouring and, in some cases, the use of bone grafts3,4,5.
There are a number of articles presenting the outcomes of surgical treatment for humeral nonunion with the use of plate osteosynthesis and intramedullary fixation. Both methods usually yield good outcomes. These surgical techniques may require bone grafting1,6,7.
When used for the treatment of long bone fracture nonunion, the Ilizarov method helps achieve high rates of union that are maintained throughout long-term follow-up. Modular structure of the Ilizarov apparatus allows for simultaneous deformity correction, bone segment elongation, and fracture site fixation8,9,10,11.
In recent years, few studies have examined in more detail the use of a ring external apparatus in the treatment of humeral nonunion12.
The purpose of this study was to evaluate the radiological and functional outcomes following posttraumatic humeral shaft pseudoarthrosis treatment with an Ilizarov apparatus.
Material and methods
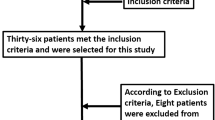
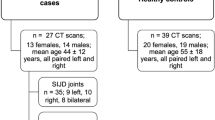
A total of 21 patients (10 females and 11 males), who underwent posttraumatic humeral nonunion treatment at the Orthopedics and Musculoskeletal Trauma Surgery, Medical University of Warsaw, in the period between 2011 and 2023, were included in our retrospective observational cohort study. The study was approved by the Bioethics Committee of the Medical University of Warsaw.
Five of these patients had developed radial nerve palsy resulting from previous surgical treatment; six had a concomitant varus deformity of the humerus (ranging between 25 and 30 degrees); three patients had been undergoing type 2 diabetes treatment; and seven patients smoked tobacco products.
Study inclusion criteria were complete radiological and clinical records, follow-up period of > 1 year, and the patient’s consent to participate in a survey comparing pre- and postoperative limb function. Quality of life was assessed based on the following scales: Constant Score, SSI-ASES (Shoulder Strength Index) and UCLA (University of California-Los Angeles Shoulder Scale). All of these questionnaires had been validated and translated into Polish.
Study exclusion criteria were incomplete radiological and/or clinical records, lack of consent to complete the questionnaires, and non-traumatic causes of humeral nonunion (such as a metabolic condition or a neoplasm).
This study evaluated the duration of treatment with an Ilizarov apparatus, the rates of achieved and maintained bone union, changes in questionnaire scores on limb function, and the radiological and functional outcomes measured with ASAMI (Association for the Study and Application of the Method of Ilizarov) scoring systems.
Preoperative planning was based on X-ray film analysis. We used the radiological classification of Weber and Cech and the Paley classification.
Hypertrophic pseudarthroses were treated via closed reduction. The Ilizarov external apparatus was mounted under fluoroscopy. Its exact configuration depended on the location of the nonunion. The proximal frame had two rings anchored with 3–4 Schanz screws (5 or 6 mm in diameter) and was connected in a hinged manner to the distal ring anchored with two Kirschner wires (1.8–2.0 mm in diameter) passing through the humeral epicondyles and with one Schanz screw. Decortication of the nonunion surfaces was performed through a small incision on the anterolateral aspect of the arm. The procedure was completed by pseudoarthrosis compression with threaded rods (Fig. 1).
Cases of oligotrophic and atrophic nonunion were managed with an open anterolateral (Henry) approach. The fracture gap was visualized, and a microbiological sample was routinely collected. Once excess granulation tissue was removed, the unfused bone ends were contoured and the intramedullary canals were reopened. A Steinmann pin was used for temporary intramedullary splinting, followed by the mounting of an Ilizarov apparatus in a configuration similar to that used for hypertrophic nonunions (Fig. 2).
Treatment of pseudarthroses located at the distal third of the humerus often requires exposing the radial nerve to protect it against accidental damage.
After surgery, the patients were encouraged to begin active exercises of their shoulder, elbow, wrist, and hand joints as soon as possible. Qualified personnel conducted rehabilitation at the hospital ward.
Outpatient follow-up visits took place, initially, every two weeks, and later, every four weeks. Application of cyclic compression (1 mm) was done by the patients themselves at a home setting.
Bone union was assessed via anteroposterior and lateral X-ray images. Callus formation was observed in the fracture gap. Union of three out of four cortices was considered to be evidence of a healed pseudarthrosis. Clinical bone union was confirmed by loosening the hinged connections and evaluating any pathological mobility at the nonunion site. The lack of pathological mobility and radiographic evidence of callus maturation qualified patients for Ilizarov apparatus removal.
Analyses were conducted using the R Statistical language (version 4.3.1; R Core Team, 2023) on Windows 10 pro 64 bit (build 19,045), using the packages emmeans (version 1.8.9; Lenth R, 2023), sjPlot (version 2.8.15; Lüdecke D, 2023), report (version 0.5.7; Makowski D et al., 2023), gtsummary (version 1.7.2; Sjoberg D et al., 2021), MASS (version 7.3.60; Venables WN, Ripley BD, 2002), and dplyr (version 1.1.3; Wickham H et al., 2023).
The level of statistical significance for this study was set at an alpha (α) of 0.05. Numeric variables that exhibited non-normal distributions were described using the median (Mdn) and the interquartile range, specifically the first (Q1) and third (Q3) quartiles. The distribution of categorical variables was presented as counts (n) and proportions (%).
For assessing differences between two dependent groups with regard to numeric variables the Wilcoxon signed-rank test was employed. The effect size for this test was quantified using the rank-biserial correlation coefficient ().
The impact of the exposure variable on the numeric outcome was analyzed using regression techniques. To enhance the robustness of these analyses against violations of assumptions, a robust estimator was utilized. The influence of the exposure variable was further examined by stratifying it according to a moderator variable, thus allowing for the evaluation of effect modification.
The estimated marginal means were calculated to assess the outcomes within subgroups defined by the moderator variable. Differences between categories of exposure within these subgroups were analyzed using contrast analysis. P-values for these analyses were estimated using the asymptotical approximation of the Wald z-test.
Effect sizes were calculated using Cohen’s d, adhering to the established conventions for interpreting the magnitude of observed effects.
Results
Clinical and surgical characteristics of patients undergoing Ilizarov external fixation
We analyzed a cohort comprising 21 adult individuals who had undergone Ilizarov External Fixation. Patient age ranged from 21.0 to 68.0 years, with a median age of 42.3 years and a mean age of 43.0 years. Additionally, the first and third quartiles of age were 32.48 and 58.11 years, respectively.
Analysis of the type of pseudarthritic joint revealed nearly equal distribution between the ‘flaccid’ and ‘stiff’ categories, indicating that the optimal surgical approach must be versatile enough to address both conditions effectively. This is further corroborated by the surgical technique data, where a majority of the procedures (57.14%) involved open surgery. The preference for open surgery might be attributed to the complexity or severity of cases that required more direct manipulation and correction.
This study evaluated the clinical and surgical outcomes of patients undergoing surgeries. Table 1 presents data on key clinical and surgical parameters, including recovery metrics, pseudarthritic joint types, the surgical techniques used, and the previous operations performed. Analyzing the distribution of these parameters provides essential insights into the initial challenges and conditions encountered in different surgical contexts.
The ASAMI radiological and functional scores reveal that the majority of patients achieved ‘very good’ outcomes (66.67% radiologically and 52.38% functionally), indicating successful surgical interventions in most cases. However, the small proportion of ‘bad’ outcomes (9.52% for both) points to the need for further evaluation and, possibly, revision strategies for those not benefitting as expected.
The effect of the surgical technique on time to bone union
Stratified by the surgical technique and patient age, the data on time to bone union presented in Table 2 provide important insights into the clinical effectiveness of open versus closed surgical techniques across different age groups.
For individuals under 43 years of age, the Estimated Marginal Mean (EMM) time to bone union was shorter (121.0 days) for those undergoing a closed surgical technique than for those undergoing an open surgical technique (203.0 days). The substantial difference of 82 days, coupled with a narrow confidence interval for each group, underscores the closed technique’s superior efficacy in promoting faster bone healing in younger patients. This finding is clinically significant, as it suggests that younger individuals, who may benefit from quicker recovery times due to lifestyle or employment demands, should be considered for the closed technique in order to achieve optimal outcomes.
Conversely, the difference in time to bone union between the closed and open techniques diminished substantially in patients older than 43 years. In this age group the EMM time to bone union was 179.0 days for the closed technique and 170.0 days for the open technique. These nearly equal values, reflected in overlapping confidence intervals, indicate that the choice of surgical technique may be less critical in older patients. This could be attributed to age-related biological changes that potentially lessen the advantages offered by various surgical techniques.
The effect of pseudarthritic joint type on time to bone union
The data from Table 3 provide a comprehensive analysis of the impact of pseudoarthritic joint type (flaccid vs. stiff) on time to bone union stratified by age. This data is crucial for understanding how joint characteristics influence surgical outcomes and recovery timelines.
For patients under 43 years old, the EMM time to bone union differed between the flaccid and stiff joint types. Patients with flaccid joints had a notably higher EMM time to bone union of 202 days, compared to those with stiff joints, who had an EMM time to bone union of 120 days. The disparity of 82 days between these groups is substantial, indicating that younger patients with stiff joints experience much quicker bone fusion. The standard errors and confidence intervals, while indicating some variability, still support a robust difference between these joint types. This suggests that the mechanical properties and stability offered by stiff joints may facilitate a more conducive environment for bone healing and fusion in younger individuals.
In the “over 43 years” age category, the difference in time to bone union between the flaccid and stiff joint types was less pronounced but still evident. The EMM time to bone union in patients with flaccid joints was 165 days, whereas in those with stiff joints it was 180 days. Unlike younger patients, the older group shows a reversed pattern, with patients with stiff joints having a slightly longer time to bone union. This small difference, supported by overlapping confidence intervals, indicates that the influence of joint type on time to bone union becomes less significant as age increases.
In older patients, in whom the difference in time to bone union between joint types is minimal and less consistent, a broader range of factors may need to be considered during therapeutic decision-making. These factors might include patient comorbidities, overall physical condition, and specific preferences or lifestyle needs.
Comparative analysis of UCLA, constant, and SSI-ASES scores: assessing patient progress from baseline to post-treatment
The data presented in Table 4 offer a comprehensive evaluation of therapeutic interventions by comparing baseline and post-treatment scores obtained with three distinct scoring systems: UCLA, Constant, and SSI-ASES. These scoring systems are pivotal for assessing shoulder function and overall patient outcomes in clinical settings.
The clinical data presented in Table 4 highlight a substantial improvement in UCLA, Constant, and SSI-ASES scores from baseline to post-treatment, indicating a significant improvement in patients’ shoulder functionality and quality of life following treatment. Specifically, the median UCLA scores improved markedly from 11.0 to 31.0 (p < 0.001). This significant increase suggests that patients experienced considerable pain relief and enhanced shoulder function, which in turn likely facilitated their activities of daily living and increased their overall satisfaction with the condition of their shoulder.
Similarly, the Constant scores rose from 28 to 94 (p < 0.001). This improvement reflects not only reduced pain levels but also substantial gains in shoulder strength and functionality. Such improvements are critical, as they directly influence the patients’ ability to perform routine tasks and can significantly enhance their overall physical health and independence.
Lastly, the SSI-ASES scores also demonstrated dramatic increases from 43 to 95 (p < 0.001). This suggests that the treatment effectively addressed specific functional deficits and disabilities, leading to a near-optimal state of shoulder health post-treatment.
Discussion
Humeral shaft nonunion adversely affects the patient’s quality of life, causes chronic pain, and impairs upper limb function1,13. In the elderly patients, additional risk factors of nonunion include: chronic conditions and treatment with certain medications, such as corticosteroids or nonsteroidal anti-inflammatory drugs2,14.
There are a number of literature reports on surgical techniques for the treatment of humeral shaft nonunion. A systematic review by Peters et al. included the results of 36 studies on this topic1. Those authors reported achieving bone union in 98% of patients treated with open reduction and internal fixation (ORIF) with the use of autologous bone grafting. Bone union was achieved in 95% of patients from the subgroup treated with internal fixation alone, without bone grafting. Intramedullary nailing with autologous bone grafting helped achieve bone union in 88% of patients, and intramedullary nailing alone helped achieve bone union in 66% of patients. External fixation helped heal nonunion in 98% of cases. Peters et al. recommended plate fixation with autologous bone grafting as the method of choice in the treatment of humeral shaft nonunion.
Similar conclusions were presented by Naclerio et al., who also indicated plate fixation as the standard surgical technique for treating humeral nonunion. Those authors also emphasized that the use of a bone graft or a vascularized fibular flap in patients with poor bone quality (osteoporosis, osteopenia), and bone defects improved treatment outcomes13.
Oliver et al. reported high bone union rates (95%) with the use of plate fixation without bone grafting. Those authors emphasized that the technique reduced the risk of iliac crest donor site complications15.
Padhye et al. analyzed the outcomes of various surgical techniques and recommended plate fixation as the most effective technique; nonetheless, they emphasized that an Ilizarov fixator is an effective technique in the case of bone infection16.
The variety of techniques used and the good treatment outcomes achieved by various authors indicate a lack of consensus as to the optimal surgical approach in the treatment of humeral fracture nonunion. Despite the fact that most authors prefer ORIF as the method of choice, there have been almost no studies on the use of external fixation, except a handful of papers on septic nonunions6,17,18,19,20.
The use of an Ilizarov apparatus offers simultaneous treatment for long bone nonunion and correction of the deformity resulting from the original injury or its previous treatment. Ilizarov fixator configuration can be adjusted to fracture morphology and the shape and size of the patient’s limb.
In our study, 90% of patients achieved bone union, maintained during 12-month follow-up. The treatment improved upper limb functional parameters and overall quality of life.
The most common complications were Kirschner wire-track infections (8 cases) which were managed with local antiseptics and oral antibiotics. No cases of deep tissue infection, osteomyelitis, or neurological or vascular complications were observed in our study population.
We also acknowledge the limitations of our study. One limitation of our study was a small sample size however, the cases described are relatively rare in clinical practice. Further limitations include its retrospective design, possible single-center bias and absence of a control group. Studies on a larger population are needed to establish a recommended treatment protocol with the use of the Ilizarov method for humeral shaft nonunion.
Conclusions
According to our knowledge and clinical practice, the Ilizarov method is an effective technique for treating aseptic humeral nonunions. It allows for a high rate of long-term bone healing over an extended follow-up period.
We achieved a shorter treatment time using the closed technique in the patient group under 43 years of age (121 days vs. 203 days) and a significantly shorter healing period for hypertrophic nonunions in the same age group (120 days vs. 202 days). The above differences were not as pronounced in the group over 43 years of age. All patients showed statistically significant improvements on the applied functional scales (UCLA, Constant, SSI-ASES).
We find that the use of the Ilizarov apparatus is particularly reasonabled in patients with coexisting nonunion and bone segment deformity or shortening.
The preferred closed reduction approach is dedicated for patients with chronic conditions (smokers, patients with type 2 diabetes), in whom an open approach might result in delayed surgical wound healing or surgical site infection.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Peters, R. M. et al. Union rate after operative treatment of humeral shaft nonunion: a systematic review. Injury 46, 2314–2324 (2015).
Toro, G. et al. Humeral shaft non-union in the elderly: results with cortical graft plus stem cells. Injury 50(Suppl. 2), S75–S79 (2019).
Nicholson, J. A., Makaram, N., Simpson, A. & Keating, J. F. Fracture nonunion in long bones: a literature review of risk factors and surgical management. Injury 52, S3–S11 (2020).
Bégué, T., Mouchantaf, M. & Aurégan, J. C. Aseptic humeral shaft nonunion. Orthop. Traumatol. Surg. Res. 109, 103462 (2023).
Rupp, M. et al. Diaphyseal long bone nonunions – types, aetiology, economics, and treatment recommendations. Int. Orthop. 42, 247–258 (2018).
Dheenadhayalan, J. et al. Consistent protocol-based management of humerus shaft nonunion: an analysis of 100 cases. Indian J. Orthop. 57, 552–564 (2023).
Garnavos, C., Mouzopoulos, G. & Morakis, E. Fixed intramedullary nailing and percutaneous autologous concentrated bone-marrow grafting can promote bone healing in humeral-shaft fractures with delayed union. Injury 41, 563–567 (2010).
Inam, M. et al. Outcome of ilizarov fixator in tibial non-union. J. Pak. Med. Assoc. 65, S94–S99 (2015).
Paley, D. et al. Ilizarov treatment of tibial nonunions with bone loss. Clin. Orthop. Relat. Res. 241, 146–165 (1989).
Szelerski, Ł et al. A new criterion for assessing Ilizarov treatment outcomes in nonunion of the tibia. Arch. Orthop. Trauma Surg. 141, 879–889 (2021).
Szelerski, Ł et al. The outcomes of Ilizarov treatment in aseptic nonunions of the tibia stratified by treatment strategies and surgical techniques. Sci. Rep. 10, 20511 (2020).
Zarek, S. & Macias, J. The Ilizarov method in the treatment of pseudoarthrosis of the humerus. Ortop. Traumatol. Rehabil. 4, 434–440 (2002).
Naclerio, E. H. & McKee, M. D. Approach to humeral shaft nonunion: evaluation and surgical techniques. J. Am. Acad. Orthop. Surg. 30, 50–59 (2022).
Oliver, W. M. et al. Factors associated with humeral shaft nonunion. J. Shoulder Elbow Surg. 30, 2283–2295 (2021).
Oliver, W. M. et al. Open reduction and internal fixation for humeral shaft nonunion: bone grafting is not routinely required and avoids donor site morbidity. J. Orthop. Trauma 35, 414–423 (2021).
Padhye, K. P. et al. Plating, nailing, external fixation, and fibular strut grafting for non-union of humeral shaft fractures. J. Orthop. Surg. (Hong Kong) 21, 327–331 (2013).
Pollon, T. et al. Persistent non-union of the humeral shaft treated by plating and autologous bone grafting. Int. Orthop. 41, 367–373 (2017).
Rollo, G. et al. Plate-and-bone-strut fixation of distal third humeral shaft aseptic non-unions: a consecutive case series. J. Clin. Orthop. Trauma 10, S127–S132 (2019).
Unal, M. et al. Single versus double plate fixation of humeral shaft nonunion. Arch. Orthop. Trauma Surg. 144, 693–699 (2024).
Zalavras, C. G., Yasmeh, S. & Bougioukli, S. Surgical management of humeral shaft nonunions: success of a consistent protocol over 17 years. Injury 52, 3580–3587 (2021).
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Authors ŁS, SŻ, KM,RG - Collected the data.Authors ŁS,AS wrote the manuscript with support from authors SŻ,KM,RG,PŁ.Authors ŁZ,AS,SŻ performed the measurements, authors SŻ,KM,RG were involved in planning and supervised thework, author AS performed the analysis, authors ŁS,AS drafted the manuscript and designed the figures. Authors SŻ and PŁ were reviewing the article before submission not only for spelling and grammar but also for its intellectual content.All the authors agreed for the final version of the manuscript.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Szelerski, Ł., Sibilska, A., Żarek, S. et al. Comparison of surgical techniques for the treatment of humeral nonunion using the Ilizarov method. Sci Rep 16, 1716 (2026). https://doi.org/10.1038/s41598-025-31334-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-31334-1