Abstract
To introduce and validate the real axial length (RAL)—the distance from the corneal vertex to the posterior choroidal surface measured by swept-source OCT angiography (OCTA). RAL aims to reduce the influence of choroidal thickness on conventional axial length (AL) measurements. The study also compared OCTA-derived parameters with those from the IOL Master 700 to confirm measurement accuracy and established age-specific RAL references in children and adolescents without myopia. This cross-sectional study enrolled Chinese children with normal uncorrected vision. VG 200D and IOL Master700 were used to measure AL, central corneal thickness (CCT), anterior chamber depth (ACD), aqueous depth (AQD), and lens thickness (LT). VG 200D additionally provided new AL parameter - RAL. The intraclass correlation coefficient (ICC) and Bland–Altman analysis were applied to assess device concordance in general parameter. Subsequently, VG 200D-derived RAL values were analyzed across age groups. Of 1833 participants aged 5–17 years (909 males, 924 females) were enrolled. The mean RAL was 24.04 mm and the mean AL was 23.52 mm, showing a statistically significant difference (p < 0.001), measured by VG 200D. AL were 23.49 ± 0.99 mm and 23.52 ± 1.02 mm respectively in Master 700 and VG 200D, showed good agreement (ICC = 0.956). At age 5, boys exhibited a significantly shorter RAL than girls, with median values of 23.55 mm (interquartile range, IQR: 22.91–23.76 mm) and 22.32 mm (IQR: 21.99–23.15 mm), respectively (p = 0.04). By age 17, the RAL increased to 25.26 mm (IQR: 24.75།25.64 mm) in boys and 25.24 mm (IQR: 24.49།25.81 mm) in girls, showing no significant sex difference (p = 0.73). RAL exceeded AL by approximately 0.5 mm. The VG 200D demonstrated strong agreement with IOL Master 700 for standard biometric parameters. The difference in RAL length between boys and girls may progressively narrow with increasing age. RAL may offer a valuable tool for objectively evaluating true ocular growth and myopia control efficacy.
Similar content being viewed by others
Introduction
Myopia has become a public health problem worldwide, with epidemiologists predicting that approximately 4758 million people will be affected by 2050, representing 49.8% of the world’s total population1. The development of myopia is usually caused by excessive growth of the axial length (AL) of the eye2,3,4. The AL was previously called the “anteroposterior length,” which is usually the longitudinal length of the eyeball5. The AL reflects the developmental state of the eye and also has a large effect on the overall refractive state of the eye. Normally, the AL of a newborn eye is 16 to 17 mm, and the corresponding refractive degree is + 2.50 D to + 3.00 D6,7. As age increases, the AL also grows longer and continues to grow into adulthood. The current methods for preventing and controlling myopia, such as defocus incorporated multiple segments (DIMS) spectacle lenses, orthokeratology lenses, and low concentration atropine eye drops, aim to control axial growth2,4,8,9,10,11. Therefore, AL is a core indicator in the research, clinical treatment, prevention, and control of myopia; accurate measurement of AL is important.
The measurement of AL has evolved considerably from ultrasonic and photographic methods to optical biometry in the present day5,12,13,14. Although some specialized methods, such as magnetic resonance imaging, can be used for AL measurements, they are not widely used15. The biometric devices that doctors use in the clinic to measure AL usually measure the distance from the apex of the cornea through the lens to the macula. However, these devices indirectly reflect the length of the AL. The AL is important for normal physiological development, but there is controversy regarding AL after an intervention. Effective prevention and control measures for myopia generally cause thickening of the choroid, which in turn causes relative regression of the AL16,17,18. This finding raises the question of whether myopia prevention and control methods truly control the growth of the AL. Changes in the thickness of the choroid have a considerable effect on the measurement of the eye axis, especially when some commonly used myopia prevention and control methods, such as low-dose atropine, orthokeratology, and DIMS, are used, as they can cause choroidal thickening4,17,18.
This study aimed to develop a new AL measurement mode for swept-source optical coherence tomography angiography (SS-OCTA). SS-OCTA encompasses the distance from the corneal vertex to the posterior surface of the choroid within a single AL measurement called the real axial length (RAL). The choroidal thickness (ChT) in the SS-OCT images was defined as the volume from the outer boundary of the retinal pigment epithelium-Bruch membrane complex to the choroid-sclera junction19. After confirming the consistency of the biometric parameters—including central corneal thickness (CCT), anterior chamber depth (ACD), aqueous depth (AQD), and lens thickness (LT)—we subsequently analyzed the RAL in non-myopic participants across different age groups.
Results
A total of 1,833 subjects with normal uncorrected vision, aged 5–17 years were included in the study (85% from within Changsha and 15% from outside Changsha who visited the hospital on their own initiative). Among them, 909 (49.59%) were male and 924 (50.41%) were female. The subjects had a mean age of 9.97 ± 2.59 years, with males at 9.94 ± 2.60 years and females at 9.98 ± 2.59 years.The number of subjects in each age group is shown in Table 1.
The mean RAL measured by the VG 200D was 24.04 ± 0.99 mm, which was 0.55 ± 0.33 mm (95% CI: 0.54 to 0.56, p < 0.001) greater than the mean AL of 23.49 ± 0.99 mm obtained with the IOL Master 700. Additionally, the mean ChT was 556.13 ± 33.36 μm using the VG 200D. As demonstrated in Table 2, the two devices exhibit a high degree of consistency. The mean values of the AL, ACD, and AQD measured using the IOL Master 700 and VG 200D were 23.49 ± 0.99 and 23.52 ± 1.01 mm, 3.57 ± 0.27 and 3.53 ± 0.25 mm, and 3.01 ± 0.40 and 2.98 ± 0.29 mm, respectively (ICC > 0.9). The mean CCT and LT were 546.77 ± 32.43 and 556.13 ± 33.36 μm and 3.47 ± 0.19 and 3.50 ± 0.19 mm, respectively (ICC > 0.8). A Bland–Altman plot with 95% limits of agreement was used to assess the concordance line. The proximity of this line to zero suggested a high level of agreement between the two machines across conventional parameter measurements. Most of the observed differences fell within the established limits of agreement (Supplementary Fig. S1).
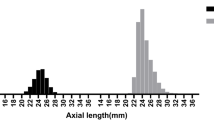
The AL, CCT, AQD, and RAL were significantly positively correlated with age (Figure 2). The AL showed a progressive increase from 22.40 ± 0.88 mm (5 years) to 24.58 ± 0.78 mm (17 years), with strong correlation coefficients (Pearson’s r = 0.98, p < 0.001). A progressive increase in the RAL was similar to that of the AL, increasing from 22.96 ± 0.86 mm to 25.09 ± 0.77 mm (r = 0.98, p < 0.001). Similarly, CCT values increased from 553.57 ± 36.00 μm (5 years) to 565.13 ± 43.54 μm (17 years) (r = 0.80, p = 0.001), while the AQD increased from 2.70 ± 0.25 mm to 3.12 ± 0.27 mm over the same age range (r = 0.93, p < 0.001). In contrast, the LT and ChT showed inverse correlations with age. The LT decreased significantly from 3.73 ± 0.17 mm (5 years) to 3.45 ± 0.16 mm (17 years) (r = − 0.81, p = 0.001), while the ChT showed a significant reduction from 357.44 ± 65.92 μm to 310.67 ± 56.24 μm during the observation period (r = − 0.89, p < 0.001).
As shown in Table 3, at age 5, boys exhibited a significantly shorter RAL than girls, with median values of 23.55 mm (interquartile range, IQR: 22.91–23.76 mm) and 22.32 mm (IQR: 21.99–23.15 mm), respectively (p = 0.04). By age 17, the RAL increased to 25.26 mm (IQR: 24.75།25.64 mm) in boys and 25.24 mm (IQR: 24.49།25.81 mm) in girls, showing no significant sex difference (p = 0.73). Although the RAL for boys was consistently greater than that for girls, this disparity diminished with age. A similar pattern was observed in ChT. At age 5, boys had a significantly thinner ChT compared with girls, with median values of 334.10 μm (IQR: 287.63–355.87 μm) and 387.42 μm (IQR: 350.48–438.78 μm), respectively (p = 0.02). With increasing age, the rate of choroidal thinning appeared greater in girls. By age 17, the ChT decreased to 313.07 μm (IQR: 274.79–338.99 μm) in boys and 332.94 μm (IQR: 292.58–350.73 μm) in girls, with no significant difference between sexes (p = 0.71).
Discussion
In this study, we investigated a new concept of AL measurement using OCTA and verified its consistency with conventional parameters measured by the IOL Master 700. We also examined RAL values in children and adolescents aged 5 to 17 years with normal uncorrected vision. These findings provide a new reference for the ocular development status of children and adolescents and could facilitate scientific evaluation of the effectiveness of preventing and controlling the progression of myopia.
Across populations, AL elongation shows marked regional and ethnic variability even at the same chronological age20,21,22. Therefore, the population in this study was mainly concentrated in the Hunan Province of China, so the measurement and reference of RAL may have certain limitations. This study primarily aimed to explore a novel method for axial length measurement; therefore, refractive matching following cycloplegia was not performed. All participants exhibited a non-cycloplegic autorefraction value exceeding 0D, and their uncorrected visual acuity was at least 0.10 logMAR or better. Furthermore, in this cohort, the majority of parents were reluctant to consent to cycloplegia for their children without myopia.
The IMI 2023 report noted that rapid changes in ChT can induce inverse fluctuations in AL, implying that short-term AL variations may not reflect true ocular growth and should be interpreted together with ChT23. The RAL, which integrates retinal and ChT, may therefore provide a more stable and physiologically relevant metric for assessing ocular development and the efficacy of myopia control interventions.
The IOL Master 700 is a commonly used biometric device for evaluating biological parameters, and its measurements are well recognized by clinicians. The VG 200D (SS-OCTA) is used clinically for measurements of the anterior and posterior segments of the eye. Both measurement devices use swept lasers with a central wavelength of 1050 nm. The IOL Master 700 operates at a scanning speed of 2000 scans/s, whereas the VG 200D achieves a much higher scanning speed of 200,000 scans/s. Regarding the resolution of these devices, the IOL Master 700 provides 22 μm, while the VG 200D provides a superior resolution of 3.8 μm. Consequently, the VG 200D theoretically delivers more precise measurement values than the IOL Master 700. The VG 200D is also capable of measuring up to 12 mm deep into the tissue, facilitating the assessment of the retina and choroid24. In our study, we observed good agreement between the two devices in the measurement of AL, CCT, ACD, AQD, and LT. In particular, the ICCs for the AL, ACD, and AQD measurements were all > 0.9. This finding indicates that the RAL measurements are accurate and reliable.
We grouped the biological parameters measured with the VG 200D by age. We found that as age increased, the RAL and AL became longer, the CCT became thicker, the AQD became deeper, and the crystalline and choroid became thinner. This finding is consistent with the trend of changes in parameters with age in previous related studies25,26,27,28,29,30. The choroidal data measured with the VG 200D support this result and are consistent with previous studies31,32,33, Which further demonstrates the feasibility of using the VG 200D to measure RAL.
This study also examined the RAL at all ages by sex. We observed that the RAL of boys was longer than that of girls. However, the sex disparity in the RAL tended to diminish with age. We hypothesize that the change in the RAL is mostly driven by the ChT because of its consistent trend across the different age groups. Sex-related differences in ocular growth may, at least in part, be attributed to variations in choroidal structure and dynamics. Previous studies have consistently reported that females exhibit thinner choroids compared with males, even after adjusting for axial length and age34. Furthermore, longitudinal data suggest that choroidal thinning in females occurs earlier and progresses more rapidly with age35. Given the established association between choroidal thinning and axial elongation in children, it is plausible that the choroid serves as a structural mediator linking sex and axial growth rate32,36. The IMI 2023 report further highlights the rapid plasticity of the choroid and its integral role in ocular growth regulation, providing a biological rationale for this potential pathway23. Collectively, these findings support a hypothesis that sex-related differences in ChT may partly explain the faster axial elongation observed in females. Future studies should integrate RAL into myopia management. For instance, after using treatments like atropine drops or peripheral defocus glasses, axial length fluctuations may occur. Comparing RAL with AL will help assess the eyes’ true developmental state.
Conclusion
In this study, the RAL exceeded the AL by approximately 0.5 mm. The VG 200D shows strong agreement with the IOL Master 700 in measuring the AL, CCT, ACD, AQD, and LT. The difference in RAL length between boys and girls may progressively narrow with increasing age. This study delineates the distribution of RAL in children and adolescents aged 5 to 17 years with normal uncorrected vision in Changsha, China. These findings could help establish preliminary clinical reference data for using the RAL in monitoring ocular development, particularly in the context of prevention and control strategies for myopia.
Limitations
This study’s first limitation is this was a single-center study conducted in the Changsha area, which constitutes a regional limitation, so further multi-center validation is needed. Second, since the subjects did not undergo cycloplegia, no correlation analysis was conducted between refractive error and RAL. Third The cross-sectional design limits tracking individual growth, a key gap for understanding RAL/ChT dynamics over time. A longitudinal follow-up would clarify patterns, especially given smaller adolescent subgroups (per Table 1), which may inflate variability.
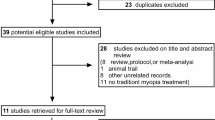
Methods
This observational study was conducted at the Aier Institute of Optometry and Science in Changsha, Hunan Province, from June 2023 to January 2024. The study was approved by the Ethics Committee of Changsha Aier Eye Hospital (ID: 2023KYPJ019) and adhered to the tenets of the Declaration of Helsinki. All subjects and their legal guardians provided written informed consent before participating in the study.
The inclusion criteria of this study were children and adolescents aged 5 to 17 years who were able to complete a biometric examination. The inclusion criteria comprised a refractive error exceeding 0.00 D as measured by non-cycloplegic autorefraction, concurrently with an uncorrected visual acuity of 0.10 logMAR or superior in both eyes. The exclusion criteria were as follows: (1) ocular diseases, such as glaucoma, retinopathy of prematurity, and retinitis pigmentosa; (2) systemic cardiovascular, immune system, and endocrine-related diseases; (3) surgery on the eye or other organs of the body; (4) current or previous use of control interventions for myopia, such as atropine eye drops, DIMS lenses, orthokeratology lenses, and red light therapy. All subjects underwent a basic eye health examination before enrollment, including visual acuity and intraocular pressure measurements and a slit lamp examination.
The AL, CCT, ACD, AQD and LT were measured using the IOL Master 700 (Carl Zeiss Meditec AG, Jena, Germany) and the VG 200D (SS-OCT/OCTA; SVision Imaging, Henan, China). The VG 200D was also used to measure ChT and RAL (Fig. 1). The RAL is the length from the corneal vertex to the posterior surface of the choroid included in a single biometric measurement. Furthermore, the SVision VG 200D was used to measure six sets of data at the same location each time. The results are displayed as the mean of the six sets.
SVision VG 200D measurement interface. The figure presents the page of SVision VG 200D’s measurement results, including relevant measured parameters: CCT, ACD, AQD, LT, AL, ChT, and RAL.SVision VG 200D measures 6 sets of data at the same location each time, and the results are displayed as the mean of the 6 sets of data.
In this study, data were collected from both eyes. The consistency of the biological parameters measured by the two devices was evaluated using data from both eyes. However, analyses examining the correlation between parameters measured by the VG 200D and age, as well as gender differences in RAL and ChT across various age groups, were conducted using data exclusively from the right eye. Descriptive statistics were used to summarize the baseline demographic characteristics of the participants. The normality of continuous variables was evaluated using the Kolmogorov–Smirnov test. Continuous variables are presented as mean with standard deviation (SD), while age-specific and gender-specific percentiles of RAL and ChT were presented as median with quantiles. A paired sample t-test was used to compare the AL and RAL measured by the VG 200D. The following tests were used as appropriate: The intraclass coefficient (ICC) and Bland–Altman analysis with 95% limits of agreement were used to verify the consistency of the two devices. The ICC for inter-rater reliability was used to quantify the degree of agreement between two raters assessing the same group of subjects. ICCs were interpreted as follows: p < 0.5 indicate poor reliability, values between 0.5 and 0.75 indicate moderate reliability, values between 0.75 and 0.9 indicate good reliability, and p > 0.90 indicate excellent reliability37. Given the bilateral consistency in ocular parameter trends, subsequent analyses were restricted to right eye measurements. Pearson correlation analysis quantified associations between core biometric indices (AL, CCT, AQD, LT ChT and RAL) and age. Concurrently, sex-related differences in RAL and ChT across stratified age were evaluated through independent samples t-tests. A p value < 0.05 indicates significance. Statistical analysis was performed using SPSS(V.27.0; IBM, USA) and GraphPad Prism(V.9.0; GraphPad Software, USA).
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to restrictions in the ethical approval concerning participant confidentiality and privacy. Data are available from the corresponding authors (Zhikuan Yang, yangzhikuan@aierchina.com) upon reasonable request and with permission from the Ethics Committee of Changsha Aier Eye Hospital (Ethics Approval ID: 2023KYPJ019).
Abbreviations
- AL:
-
Axial length
- RAL:
-
Real axial length
- CCT:
-
Central corneal thickness
- ACD:
-
Anterior chamber depth
- AQD:
-
Aqueous depth
- LT:
-
Lens thickness
- ChT:
-
Choroidal thickness
References
Holden, B. A. et al. Global prevalence of myopia and high myopia and Temporal trends from 2000 through 2050. Ophthalmology 123, 1036–1042 (2016).
Wolffsohn, J. S. et al. IMI - Myopia control reports overview and introduction. Invest. Ophthalmol. Vis. Sci. 60, M1–M19 (2019).
Baird, P. N. et al. Myopia. Nat. Rev. Dis. Primers. 6, 99 (2020).
Jonas, J. B. et al. IMI prevention of myopia and its progression. Invest. Ophthalmol. Vis. Sci. 62, 6 (2021).
Youn, D. H., Yu, Y. S. & Park, I. W. Intraocular pressure and axial length in children. Korean J. Ophthalmol. 4, 26–29 (1990).
Axer-Siegel, R. et al. Early structural status of the eyes of healthy term neonates conceived by in vitro fertilization or conceived naturally. Invest. Ophthalmol. Vis. Sci. 48, 5454–5458 (2007).
Rozema, J. J., Herscovici, Z. & Snir, M. Axer-Siegel, R. Analysing the ocular biometry of new-born infants. Ophthalmic Physiol. Opt. 38, 119–128 (2018).
Lam, C. S. Y. et al. Defocus incorporated multiple segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br. J. Ophthalmol. 104, 363–368 (2020).
Yam, J. C. et al. Effect of Low-Concentration Atropine Eyedrops vs placebo on myopia incidence in children: the LAMP2 randomized clinical trial. JAMA 329, 472–481 (2023).
Rose, K. A. et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 115, 1279–1285 (2008).
Guggenheim, J. A. et al. Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort study. Invest. Ophthalmol. Vis. Sci. 53, 2856–2865 (2012).
Grey, R. H., Perkins, E. S. & Restori, M. Comparison of ultrasonic and photographic methods of axial length measurements of the eye. Br. J. Ophthalmol. 61, 423–427 (1977).
Jin, G. et al. Corneal biometric features and their association with axial length in high myopia. Am. J. Ophthalmol. 238, 45–51 (2022).
Roy, A., Das, S., Sahu, S. K. & Rath, S. Ultrasound biometry vs. IOL Master Ophthalmology. 119, 1937e1–1937e2 (2012).
Akduman, E. I., Nacke, R. E., Leiva, P. M. & Akduman, L. Accuracy of ocular axial length measurement with MRI. Ophthalmologica 222, 397–399 (2008).
IMI Prevention of Myopia and Its Progression. - PubMed. https://pubmed.ncbi.nlm.nih.gov/33909032/
Yam, J. C. et al. The association of choroidal thickening by Atropine with treatment effects for myopia: Two-Year clinical trial of the Low-concentration Atropine for myopia progression (LAMP) study. Am. J. Ophthalmol. 237, 130–138 (2022).
Li, Z. et al. Choroidal thickness and axial length changes in myopic children treated with orthokeratology. Cont. Lens Anterior Eye. 40, 417–423 (2017).
Xu, A., Sun, G., Duan, C., Chen, Z. & Chen, C. Quantitative assessment of Three-Dimensional choroidal vascularity and choriocapillaris flow signal voids in myopic patients using SS-OCTA. Diagnostics 11, 1948 (2021).
Mutti, D. O. et al. Axial length as a function of age, sex, and ethnicity: results from the CLEERE study. Optom. Vis. Sci. https://doi.org/10.1097/OPX.0000000000002304 (2025).
Chen, S. et al. Axial growth driven by physical development and myopia among children: A two year cohort study. J. Clin. Med. 11, 3642 (2022).
Truckenbrod, C. et al. Longitudinal analysis of axial length growth in a German cohort of healthy children and adolescents. Ophthalmic Physiol. Opt. 41, 532–540 (2021).
Ostrin, L. A. et al. IMI—The dynamic choroid: new Insights, Challenges, and potential significance for human myopia. Invest. Ophthalmol. Vis. Sci. 64, 4 (2023).
Gao, Y. et al. Retinal microvascular changes in white matter hyperintensities investigated by swept source optical coherence tomography angiography. BMC Ophthalmol. 22, 77 (2022).
Chua, W. H. et al. Atropine for the treatment of childhood myopia. Ophthalmology 113, 2285–2291 (2006).
Kunert, K. S. et al. Repeatability and agreement in optical biometry of a new swept-source optical coherence tomography-based biometer versus partial coherence interferometry and optical low-coherence reflectometry. J. Cataract Refract. Surg. 42, 76–83 (2016).
Zeng, J. et al. [Relationship between gender and posterior pole choroidal thickness in normal eyes]. Zhonghua Yan Ke Za Zhi. 48, 1093–1096 (2012).
Bafiq, R. et al. Age, Sex, and ethnic variations in inner and outer retinal and choroidal thickness on Spectral-Domain optical coherence tomography. Am. J. Ophthalmol. 160, 1034–1043e1 (2015).
Deng, J. et al. Distribution of scleral thickness and associated factors in 810 Chinese children and adolescents: a swept-source optical coherence tomography study. Acta Ophthalmol. 97, e410–e418 (2019).
Huang, L. C. et al. Choroidal thickness by handheld Swept-Source optical coherence tomography in term newborns. Transl Vis. Sci. Technol. 10, 27 (2021).
Fontaine, M., Gaucher, D., Sauer, A. & Speeg-Schatz, C. Choroidal thickness and ametropia in children: A longitudinal study. Eur. J. Ophthalmol. 27, 730–734 (2017).
Jin, P. et al. Longitudinal changes in choroidal and retinal thicknesses in children with myopic shift. Retina 39, 1091–1099 (2019).
Liu, Y., Wang, L., Xu, Y., Pang, Z. & Mu, G. The influence of the choroid on the onset and development of myopia: from perspectives of choroidal thickness and blood flow. Acta Ophthalmol. 99, 730–738 (2021).
Jiang, Z. et al. Inter-Individual topographic variation of choroidal thickness in healthy eyes on Swept-Source optical coherence tomography. Trans. Vis. Sci. Tech. 13, 24 (2024).
Song, D. et al. Age and gender-related changes in choroidal thickness: insights from deep learning analysis of swept-source OCT images. Photodiagnosis Photodyn Ther. 52, 104511 (2025).
Read, S. A., Alonso-Caneiro, D., Vincent, S. J. & Collins, M. J. Longitudinal changes in choroidal thickness and eye growth in childhood. Invest. Ophthalmol. Vis. Sci. 56, 3103–3112 (2015).
Koo, T. K. & Li, M. Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 15, 155–163 (2016).
Acknowledgements
This study acknowledges the following four interns, Xiangjie Tian, Jiaxin Wan, Hong Xie, Jiahui Wan, from Hubei University of Science and Technology. We thank Ellen Knapp from Scribendi (www.scribendi.com) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
***Conception and design: *** Zhikuan Yang, Weizhong Lan, Xiaoning Li, Guangyao Ran***Data collection: *** Guangyao Ran, Zhiwei Luo, Xiangzhong Tang, Yao Lu***Analysis and interpretation: *** Guangyao Ran, Xiaoning Li, Zhikuan Yang***Manuscript preparation: *** Guangyao Ran, Zhiwei Luo, Xiaoning Li, Zhikuan Yang**Overall responsibility: ** Guangyao Ran, Zhiwei Luo, Xiaoning Li, Xiangzhong Tang, Yao Lu, Weizhong Lan, Zhikuan Yang. Guangyao Ran and Zhiwei Luo contributed equally to this study, shared first authorship.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Disclosure
All authors have completed and submitted the ICMJE disclosures form. All authors have no proprietary or commercial interest in any materials discussed in this article. This work was supported by the Hunan major R&D project (2019SK2051), Key scientific research project of Aier Eye Hospital Group (AR2003D2); Hunan Province Optometry Engineering and Technology Research Center (2020TP2003); Hunan Province International Cooperation Base for Optometry Science and Technology (2020CB1002). Subjects: Human subjects were included in this study. The trial was approved by the ethics committee of Changsha Aier Eye Hospital (ID: 2022KYPJ008) and adhered to the tenets of the Declaration of Helsinki. Written informed consent for each child was obtained from a parent/guardian.No animal subjects were used in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ran, G., Luo, Z., Li, X. et al. Real axial length (RAL): a novel choroid-inclusive metric for myopia management. Sci Rep 16, 1830 (2026). https://doi.org/10.1038/s41598-025-31568-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-31568-z