Abstract
Background
Urinary tract infections (UTIs) are common health issues affecting women of reproductive age, often leading to antibiotic prescriptions based on empirical diagnosis. Improper use of antibiotics can result in antibiotic resistance and treatment failure. This study aimed to evaluate antibiotic utilisation patterns, along with clinical and behavioural factors, and prescriber practices among women aged 15–45 at a district hospital in Ghana.
Methods
A hospital-based cross-sectional study was conducted among 498 women aged 15–45 years diagnosed with UTI at St. Edwards Catholic Hospital, Adugyama. Data were collected through structured questionnaires, interviews, and medical record reviews. Descriptive statistics summarised antibiotic use, while chi-square tests and multivariable logistic regression examined associations between prescriber type and inappropriate prescribing.
Results
Cefuroxime was the most prescribed antibiotic (65.3%), while ciprofloxacin was the most frequently used medication each week (35.7%). Laboratory testing before and after prescription was low (28.5% and 10.2%, respectively), indicating a reliance on empirical treatment. Notably, 50% reported dysuria, and 60.2% experienced symptoms lasting three months or more. Prescriber type was associated with inappropriate antibiotic use, especially among registered nurses (cOR = 13.20, 95% CI: 3.12–50.51, p < 0.001; aOR = 12.55, 95% CI: 3.12–50.51, p < 0.001). Recurrent UTIs were common, with 40% experiencing two UTI occurrences in the past year.
Conclusions
Empirical antibiotic use for UTIs is widespread and is often not supported by laboratory testing, thereby increasing the risk of resistance and poor treatment outcomes. Inappropriate prescriptions, particularly by nurses, emphasise the need for improved stewardship and prescriber training. Enhancing policies, education, public awareness, and diagnostics is vital for effectively managing UTIs in women of reproductive age.
Similar content being viewed by others
Background
Urinary tract infections (UTIs) are among the most common bacterial infections affecting women worldwide and pose a significant public health concern1,2. In Ghana, UTIs are widespread among women of reproductive age, increasing morbidity and healthcare utilisation3. Despite the high prevalence, estimated at between 20 and 30 per cent in women from urban and semi-urban areas, irrational antibiotic use and limited diagnostic resources hinder effective management4. A shorter urethra and hormonal influences make women of reproductive age particularly susceptible to UTIs, which cause around 150 million cases globally each year5.
Globally, UTIs account for millions of outpatient consultations each year, with empirical antibiotic treatment remaining the main management approach—often without laboratory confirmation6,7. In low- and middle-income countries (LMICs), including Ghana, this dependence on empirical treatment is intensified by inadequate diagnostic facilities, limited antimicrobial stewardship, and inconsistent prescribing practices among prescribers.
UTIs also contribute to the global challenge of antimicrobial resistance (AMR) by increasing healthcare costs and antibiotic consumption, and by causing discomfort and morbidity8,9.
The escalating misuse and overuse of antibiotics in UTI management pose a serious public health risk, accelerating the development of antimicrobial resistance (AMR)10,11. In Ghana, studies have shown high resistance rates among Escherichia coli and Klebsiella species to commonly prescribed drugs such as ciprofloxacin, cefuroxime, and cotrimoxazole12. Despite this concerning trend, antibiotic prescribing for UTIs mostly remains empirical, and diagnostic testing is rarely performed7,13. The problem is worsened by inconsistencies in prescriber training and supervision—especially among non-physician healthcare workers such as nurses, midwives, and physician assistants—who are increasingly involved in frontline UTI management in settings with limited resources. These systemic issues threaten the sustainability of effective infection control and add to the global AMR crisis10.
Additionally, individual-level factors, including personal hygiene habits, health-seeking behaviour, and self-medication, impact both the recurrence of infections and treatment results14,15. In many Ghanaian communities, women often delay seeking professional care, depend on informal access to antibiotics, or utilise leftover medicines, which further hampers disease control16,17. Nonetheless, there is limited empirical evidence connecting antibiotic prescribing patterns, diagnostic practices, and patient behaviours in the context of primary healthcare in Ghana.
This study aimed to assess antibiotic use patterns, prescriber practices, and related health-seeking behaviours in the management of urinary tract infections among women of reproductive age in Ghana. Specifically, it sought to describe the types and frequencies of antibiotics prescribed, evaluate the appropriateness of prescriptions across prescriber categories, and explore how hygiene practices and clinical presentation influence UTI management. By addressing these critical gaps, the study provides evidence to guide antimicrobial stewardship efforts, improve prescriber training and oversight, and strengthen diagnostic and infection prevention strategies within Ghana’s healthcare system.
Methods
Study design
A facility-based descriptive cross-sectional study was undertaken from January to June 2025 at St. Edward’s Catholic Hospital, Adugyama, in the Ashanti Region of Ghana. The hospital caters to a mixed urban–periurban catchment area with approximately 15,000 residents. It offers outpatient, maternal, laboratory, and pharmacy services, making it a suitable site for investigating outpatient management of urinary tract infections (UTIs) among women of reproductive age. The study spanned six months, from January to June 2025, capturing a snapshot of antibiotic use patterns, prescribing practices, and patient behaviours within the hospital’s catchment area.
Study area
The study was conducted at St. Edwards Catholic Hospital, located in Adugyama, a town in the Ashanti Region of Ghana. Adugyama is strategically positioned along the main road linking the northern and southern parts of the Ashanti Region, making it a key transit and service hub for the surrounding communities. The town is both accessible and centrally located, enabling it to attract patients from a broad catchment area that includes urban, peri-urban, and rural populations. St. Edwards Catholic Hospital is a well-established healthcare facility within Adugyama, serving an estimated population of around 15,000 residents from Adugyama and its neighbouring localities. The hospital provides a range of services, including outpatient, maternal, laboratory, and pharmacy care. Its central location within the community and comprehensive services make it a representative site for studying outpatient management of urinary tract infections (UTIs), especially among women of reproductive age.
The geographic coordinates of Adugyama are approximately 6.7930° N latitude and 1.6440° W longitude. The area’s demographic profile includes a significant proportion of women aged 15–45, which aligns with the study’s focus on antibiotic use for UTIs in this population. The hospital’s diverse patient population, including urban and peri-urban residents, provides a valuable context for examining healthcare access, antibiotic prescribing practices, and self-medication patterns.
The region faces numerous healthcare challenges, including rising rates of urinary tract infections, increasing antimicrobial resistance, and limited access to healthcare facilities in more rural areas. Many residents, particularly women of reproductive age, rely on St. Edwards Catholic Hospital for primary healthcare needs, making it a crucial point for data collection and intervention in addressing the responsible use of antibiotics and the management of UTIs.
Study population
The population was defined by the specific research question and the study’s scope, including all groups the researcher intended to examine. The study population consisted of women of reproductive age, particularly those aged 15–45, who sought outpatient care at St. Edwards Catholic Hospital in Adugyama, Ashanti Region, Ghana. Recent hospital records indicate that the outpatient department served a diverse group of women in this age range seeking treatment for various illnesses, including UTIs. All women aged 15 to 45 years residing in the Adugyama community at the time of data collection and who had been diagnosed with, or were undergoing treatment for, urinary tract infections formed the target population. The study focused on this group to evaluate patterns of antibiotic use and adherence, and to identify factors influencing antibiotic prescribing practices for UTIs in this healthcare setting.
Inclusion criteria
women aged 15–45 with UTI who are residents of Adugyama and have consented.
Exclusion criteria
women with chronic immunosuppressive conditions or those unwilling to participate.
UTI diagnosis in the study population was confirmed through clinical assessment and laboratory investigations, including urinalysis and, where appropriate, urine culture. Only women presenting with symptoms consistent with urinary tract infections and with laboratory confirmation documented in their medical records were included. Residency in Adugyama was verified by checking the participant’s address as recorded in hospital records and confirming their current residence during the initial screening interview. For participants under 18 years of age, written informed consent was obtained from a parent or legal guardian, along with the participant’s assent, ensuring adherence to ethical standards for research involving minors.
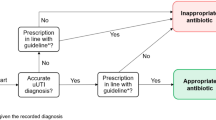
Criteria for appropriate and inappropriate prescribing
Prescriptions were evaluated for suitability in accordance with the WHO guidelines for rational medicine use and the Ghana Standard Treatment Guidelines18,35. Prescribing was considered appropriate when the antibiotic selection, dose, frequency, and duration met these standards and when treatment was supported by clinical or laboratory evidence of UTI. Empirical prescriptions lacking diagnostic confirmation or those that deviated from recommended drug selection, dosage, or duration without justification were regarded as inappropriate.
Two clinical pharmacists independently evaluated all prescriptions using a standardised checklist and were blinded to the prescribers’ identities. Discrepancies were resolved through consensus with a senior clinician. Although formal inter-rater reliability was not assessed, dual review and consensus served as quality-control measures.
Sampling and sample size
Sample size determination
The standard formula for estimating sample size for proportions in cross-sectional studies was used to determine a sample size of approximately 500 participants for a study (e.g., assessing antibiotic utilisation in UTIs among women of reproductive age).
=\(\:n\frac{{\left(\text{Z}\right)}^{2}XPX(1-P)}{{\left(\text{e}\right)}^{2}}\)(18)
n = required sample size.
Z = Z-score corresponding to the desired confidence level (e.g., 1.96 for 95% confidence).
P = estimated prevalence or proportion (use 0.5 for maximum variability if unknown).
e = margin of error (precision), is 0.05 or 5%.
=\(\:n=\frac{{\left(1.96\right)}^{2}X0.5(1-0.5)}{{\left(0.044\right)}^{2}}\)
=\(\:n\frac{3.8416X0.25}{0.001936}\)
=\(\:n\frac{0.9604}{0.001936}\)
n = 496.
Adjusting for a 1% non-response rate gives 0.1 × 496 = 4.96.
Therefore, the desired sample size for the study was 496 + 4 = 500.
The sample size was determined using the single-population proportion formula, assuming an expected prevalence of 25% for urinary tract infection (midpoint of the 20–30% range reported in prior Ghanaian studies), a 95% confidence level, and a 5% margin of error. This yielded a minimum sample size of 288 participants. To account for design effects from systematic sampling and potential non-response, the sample was inflated by a factor of 1.5, giving a final target sample of 432 participants. This sample provided adequate precision for estimating prevalence and sufficient statistical power (> 80%) for subsequent subgroup and multivariable analyses.
Systematic sampling procedure
Systematic random sampling was used to select 498 women aged 15–45 who attended the outpatient department for the management of UTI. The sampling frame consisted of approximately 2,490 eligible outpatient records, representing all women who met the inclusion criteria during the study period. The sampling interval (k) was therefore calculated as:
Thus, every 5th eligible woman on the outpatient list was selected.
The outpatient records were initially arranged in chronological order by date of attendance to ensure that each eligible case had an equal chance of selection without clustering. The first participant was chosen at random by selecting a number between 1 and 5 using a simple lottery method. Starting from that randomly selected index, every 5th record was included until the required sample size was reached. When a participant chosen declined to participate, did not meet the inclusion criteria upon verification, or had incomplete records, the next participant in the sequence was selected to preserve the systematic pattern and prevent sampling gaps.
Data collection tool and technique
The data collection instrument was a structured questionnaire adapted from previously validated tools used in similar studies on urinary tract infections and antibiotic use. Content validity was confirmed through expert review by two infectious disease specialists, one pharmacist, and one epidemiologist. The questionnaire was pretested with 30 patients at a comparable outpatient clinic to evaluate clarity, relevance, and timing. Minor revisions were made to improve the wording of items and response options. Internal consistency of the knowledge and behaviour domains was satisfactory (Cronbach’s α = 0.81 and 0.77, respectively). Test–retest reliability over a two-week interval (n = 15) yielded an intraclass correlation coefficient of 0.83. The final version incorporated all modifications before complete data collection. The absence of formal psychometric validation is acknowledged as a limitation of the study.
Data were collected using a structured, pretested questionnaire and a standardised medical record review checklist. The questionnaire comprised four sections: socio-demographic characteristics; clinical presentation and diagnostic details; antibiotic prescribing patterns (drug, dose, route, duration, prescriber type); and treatment outcomes, adherence, and hygiene practices. The medical record checklist recorded diagnoses, ordered laboratory tests and results, prescription details, and follow-up notes. Trained research assistants conducted face-to-face interviews in private settings and extracted relevant clinical data from patient records.
Definitions and outcome measures
Primary outcomes included:1 pattern of antibiotic prescribing (agent, class, dose, duration);2 use of diagnostic tests before antibiotic initiation (urinalysis, urine culture, microscopy); and3 appropriateness of antibiotic prescription, assessed against national and international UTI treatment guidelines (considering drug choice, dose and duration). Secondary outcomes included recurrence of UTI symptoms within 12 months, patient health-seeking behaviour, and self-reported hygiene practices. Prescriber categories included medical officers, physician assistants, midwives, and registered nurses.
Diagnostic Criteria for UTIs.
-
a.
The gold standard for UTI diagnosis is urine culture.\({\text{Diagnosis}} = \ge {\text{100,000}}\;{\text{CFU/mL (10}}^{5} \;{\text{CFU/mL)}}\)of a single uropathogen on a clean-catch midstream urine, in an asymptomatic woman.
-
b.
Urinalysis (Dipstick)
Supportive but not diagnostic alone.
Indicators
-
Positive nitrites (highly specific).
-
Positive leukocyte esterase (suggests pyuria).
-
Microscopy:
-
Pyuria ≥ 5 WBCs/high-power field.
-
Bacteriuria seen on microscopy.
-
Data quality assurance
To ensure data quality, research assistants received thorough training on study procedures, questionnaire administration, and medical record abstraction. Supervisors performed daily checks for completeness and consistency; any discrepancies or missing entries were verified against source documents or resolved through participant re-contact where feasible. Double data entry and range checks were used during database creation to reduce transcription errors.
Data analysis
Data were coded and entered into STATA v17.0 for analysis. Data cleaning and coding served as the initial steps in the analysis process to ensure the dataset’s accuracy, consistency, and completeness. Descriptive statistics (means, standard deviations, frequencies, and percentages) summarised participant characteristics, prescribing patterns, and diagnostic use. Power analysis confirmed that the sample size (n = 498) achieved > 80% power to detect moderate associations (odds ratio ≥ 1.8) in multivariable binary logistic regression models with up to eight predictors at a significance level of 0.05. Bivariate analyses (chi-square tests and t-tests as appropriate) examined associations between prescriber type, diagnostic use, and prescription appropriateness. Variables with p ≤ 0.05 in bivariate analysis were included in multivariable logistic and multinomial regression models to identify independent predictors of appropriate prescribing and health-seeking behaviour; adjusted effect estimates are presented with 95% confidence intervals. A two-sided p ≤ 0.05 was considered statistically significant.
All methods were performed in accordance with relevant guidelines and regulations that ensures high ethical standards.
Results
Socio-Demographic characteristics of study participants
Table 1 shows the socio-demographic characteristics of the 498 participants. The most common age group was 21–25 years (45.0%), with most participants being single (51.0%) or married (43.2%). Educational levels were generally low: 38.8% had no formal education, and only 9.0% had attained tertiary education. Nearly half (45.0%) were unemployed, while the remainder were self-employed (29.7%) or employed in formal employment (25.3%). Notably, 97.6% of respondents reported a diagnosis related to the condition under study, indicating high awareness of health status within the sample.
Table 2 presents the distribution of prescriber types among the 498 respondents. More than half of all prescriptions were issued by midwives (52.4%), followed by registered nurses (45.2%). Physician assistants accounted for a tiny proportion (1.6%), whereas medical officers were the least represented prescribers, accounting for only 0.8% of all cases (Table 2). This distribution indicates that most prescribing activity in the study setting was conducted by midwives and nurses rather than by physicians or physician assistants.
The pattern of antibiotic prescription and utilisation among the study participants is shown in Table 3. Cefuroxime was the most prescribed antibiotic (65.3%, 95% CI 60.9–69.5), followed by amoxicillin (14.9%, 95% CI 12.7–19.2) and ciprofloxacin (8.8%, 95% CI 6.5–11.6). Less frequently used antibiotics included nitrofurantoin (4.8%, 95% CI 3.1–7.1), cotrimoxazole (2.8%, 95% CI 1.7–4.7), doxycycline (1.6%, 95% CI 0.8–3.2), azithromycin (1.0%, 95% CI 0.4–2.3), and metronidazole (0.8%, 95% CI 0.3–2.0). Cefuroxime thus accounted for nearly two-thirds of all antibiotic prescriptions, indicating a strong preference for broad-spectrum antibiotics, particularly cefuroxime and ciprofloxacin, in treatment regimens.
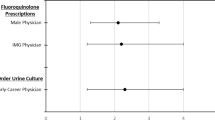
Table 4 shows the association between prescriber type and the appropriateness of medication use. Because several prescriber categories had expected cell frequencies less than 5, a Fisher’s Exact Test was conducted, revealing a significant overall association between prescriber type and medication appropriateness (p = 0.004). In the logistic regression model (with Medical Officer as reference), prescriptions by registered nurses were much more likely to be appropriate compared to those by medical officers (aOR = 12.55, 95% CI 3.12–50.51; p < 0.001), after adjusting for prescriber experience, facility type, patient age group, and comorbidity status. Prescriptions from midwives and physician assistants did not differ significantly from those of the reference group (p > 0.05).
Model diagnostics indicated a satisfactory fit (Nagelkerke Pseudo R2 = 0.18), with a significant likelihood ratio test, χ28 = 46.3 (p < 0.001), indicating that the set of predictors reliably distinguished between appropriate and inappropriate prescribing. Information criteria values (AIC = 687.24, BIC = 703.17) supported acceptable simplicity. Sensitivity analysis using exact logistic regression produced consistent results, confirming the robustness of the estimates.
Table 5 presents the distribution of health symptoms and related health-seeking behaviours among participants. Half of respondents reported dysuria (50.0%; 95% CI, 45.5–54.5), 27.5% (95% CI, 23.8–31.6) reported urgent urination, and 13.5% (95% CI, 10.8–16.7) reported malodorous urine. Persistent symptoms (lasting ≥ 3 months) were seen in 60.2% (95% CI 55.8–64.5), and 72.7% (95% CI 68.4–76.6) had experienced two or more UTIs within the past year. Perceived links to lifestyle were noted by 34.9% (95% CI 30.8–39.2), whereas 6.0% (95% CI 4.2–8.4) were unsure. Regarding care-seeking, 70.1% (95% CI 65.8–74.1) sought advice from a professional, 21.9% (95% CI 18.4–25.8) did not seek advice, and 8.0% (95% CI 5.9–10.8) were unsure.
Table 6 summarises personal hygiene and urogenital health practices among the study participants. Regarding personal and urogenital health practices, 64.1% (95% CI 59.8–68.2) of participants reported using contraceptives or spermicides, while 17.5% (95% CI 14.4–21.1) had been catheterised before. A majority (61.4%, 95% CI: 57.0–65.6) indicated that using personal hygiene equipment improved symptoms, whereas 38.6% (95% CI: 34.4–43.0) reported no perceived benefit. In rating hygiene equipment, 42.8% (95% CI: 38.5–47.3) described it as effective, 28.7% (95% CI: 24.8–33.0) as very effective, and 28.5% (95% CI: 24.6–32.7) as not very effective.
Table 7 presents the results of a multinomial logistic regression analysis of factors associated with health-seeking behaviour for urogenital symptoms. In the multinomial logistic regression model (Table 7), the reference outcome was “Consulted Professional.” The adjusted model included age, sex, education, and income as covariates. Model fit was satisfactory (Nagelkerke R2 = 0.21; LR χ212 = 78.4, p < 0.001; AIC = 912.45; BIC = 945.12), and the proportional odds assumption was not violated (p = 0.18). Adjusted p-values were computed using the Benjamini–Hochberg procedure to control for multiple comparisons. Participants whose symptoms persisted for ≥ 3 months were more than twice as likely (aRRR = 2.12, p = 0.003) to consult a health professional than those whose symptoms resolved within 3 months, suggesting that symptom chronicity strongly drives formal care-seeking. Those with three or more UTIs in the past year had a two-fold increase in the likelihood of consultation (aRRR = 2.04, p = 0.007), highlighting the impact of recurrence on perceived need for medical evaluation. Experiencing pain or burning during urination nearly doubled the probability of professional consultation (aRRR = 1.89, p = 0.009), reinforcing pain as a significant motivator for seeking care. A perceived link between symptoms and lifestyle also significantly increased consultation behaviour (aRRR 1.71, p = 0.018), implying that greater symptom awareness or health literacy promotes proactive help-seeking. Overall, the model exhibited good fit (Nagelkerke R2 = 0.21), and results remained significant after correction for multiple testing, indicating robust associations across key symptom-related factors.
The distribution of clinical symptoms and conditions associated with urinary tract infection (UTI) among study participants is presented in Table 8. The most common clinical presentation was genital itching (87.3%, 95% CI 84.0–90.1), followed by genital discharge (79.7%, 95% CI 75.9–83.1), lower abdominal pain (71.3%, 95% CI 67.0–75.3), and foul-smelling discharge (65.1%, 95% CI 60.8–69.2). Cystitis and pyelonephritis were reported in 67.1% (95% CI 62.8–71.2) and 64.7% (95% CI 60.4–68.8), respectively. Other frequent symptoms included fatigue (58.0%, 95% CI 53.5–62.3), fever (42.2%, 95% CI 37.8–46.7), flank pain (38.0%, 95% CI 33.8–42.5), and pregnancy-related complications (29.9%, 95% CI 26.0–34.1). The predominance of cystitis-related symptoms underscores the high prevalence of uncomplicated UTI among participants.
Figure 1 shows the frequency with which laboratory tests are performed before initiating antibiotic treatment. It reveals that only 28.5% of patients had laboratory testing before therapy, whereas 71.5% did not, emphasising that empiric antibiotic prescribing without laboratory confirmation is common.
Persistence of urinary tract infection (UTI)
Figure 2 shows the percentage of patients who returned to the facility with ongoing urinary tract infection (UTI) symptoms after finishing their prescribed antibiotic course. Of the total group, 48.6% (242 patients) reported symptom recurrence, while 51.4% (256 patients) did not (Fig. 2). This distribution highlights a notable burden of unresolved infections or treatment failure, indicating underlying issues such as antibiotic resistance, poor therapy adherence, or other complicating factors.
Table 9 summarises the treatment outcomes for eight antibiotics used to manage UTIs among women of reproductive age. Cefuroxime was the most prescribed antibiotic (n = 325), with a treatment success rate of 56.0%, while amoxicillin and ciprofloxacin had lower success rates of 38.0% and 44.0%, respectively. A statistical comparison of the three most frequently used antibiotics showed a significant difference in treatment success (χ2 = 14.6, p = 0.002), indicating variability in effectiveness across the agents. Treatment success was defined as the complete resolution of UTI symptoms within 7–14 days, and failure as persistence or recurrence within the same period.
Treatment Success/Failure analysis
To formally assess treatment outcomes, treatment success was defined as complete resolution of urinary symptoms within 7–14 days after completion of the prescribed antibiotic course, and treatment failure as the persistence or recurrence of symptoms during this period. Using available follow-up data from outpatient records and participant interviews, 242 of 498 patients (48.6%) experienced symptom persistence or recurrence, while 256 patients (51.4%) reported full symptom resolution. A chi-square test comparing treatment success across the three most prescribed antibiotics (cefuroxime, amoxicillin, ciprofloxacin) revealed a significant difference in outcomes (χ2 = 14.6, p = 0.002), with cefuroxime achieving higher success rates (56.0%) compared to amoxicillin (38.0%) and ciprofloxacin (44.0%) (Table 9).
Symptom resolution assessment
Symptom resolution was assessed using patient-reported outcomes documented during follow-up visits and corroborated by medical records. Patients were asked whether key UTI symptoms—dysuria, urgency, frequency, and lower abdominal pain—had completely resolved.
Data on adverse effects were limited in outpatient records; however, self-reported side effects were gathered during follow-up interviews.
Figure 3 presents the distribution of patients by whether they continued the same antibiotic regimen or changed therapy after completing an initial course. Of the total cohort, 56.2% (280 patients) remained on the original antibiotic, while 43.8% (218 patients) were prescribed a different agent (Fig. 3). This figure provides a quantitative overview of clinical management patterns following initial antibiotic treatment for urinary tract infection.
Table 10 summarises the prescribed antibiotic regimens for managing UTI among study participants, including the drug type, dosage, duration, and route of administration. Cefuroxime, amoxicillin, and ciprofloxacin were the most frequently prescribed agents, all administered orally for 7 days. Other antibiotics, such as nitrofurantoin, cotrimoxazole, doxycycline, azithromycin, and metronidazole, were used less often, with dosing schedules aligned with the Ghana Standard Treatment Guidelines where applicable.
Discussion
This study provides significant evidence on antibiotic usage patterns, diagnostic procedures, and health-seeking behaviour among women of reproductive age with urinary tract infections (UTIs) in Ghana. The findings highlight a high prevalence of recurrent UTI symptoms, widespread empirical antibiotic use, and notable gaps in diagnostic confirmation and antimicrobial stewardship. Collectively, these trends expose systemic weaknesses in both community-level health literacy and facility-based prescribing practices, with substantial implications for antimicrobial resistance (AMR) control efforts in low- and middle-income settings.
Antibiotics prescribed and usage patterns
This study highlights the predominant reliance on antibiotics for the treatment of urinary tract infections (UTIs) in women of reproductive age. The prescription patterns show that antibiotics are typically the first-choice treatment, often administered empirically without confirmatory diagnostic tests. Previous research in Ghana and other sub-Saharan African regions has reported similar trends: more than two-thirds of UTI treatments were based solely on clinical symptoms, with little microbiological confirmation20,21.
In 65.3% of cases, cefuroxime is the most frequently prescribed primary antibiotic, indicating a strong preference for this cephalosporin in treating infections in this population. Conversely, prescription rates for drugs such as ceftriaxone, cotrimoxazole, and nitrofurantoin are notably lower, possibly due to their more specific or restricted use cases19.
The fact that metronidazole, azithromycin, and doxycycline account for over 95% of prescriptions and are the most used medications indicates that infections such as anaerobic bacterial infections, respiratory infections, and STDs, which these drugs typically treat, are widespread19. This aligns with global trends, in which these antibiotics are often prescribed as first-line treatments for such illnesses20. Interestingly, the high weekly ciprofloxacin use may be due to its role in prophylaxis or long-term management of chronic infections, consistent with other research showing its extensive use in both inpatient and outpatient settings21.
The preference for broad-spectrum antibiotics—commonly penicillins, fluoroquinolones, and cephalosporins—reflects both their easy availability and the limited capacity for culture-based sensitivity testing in most healthcare facilities22,23. The implications are significant: such prescribing practices increase the risk of developing multidrug-resistant uropathogens, including Escherichia coli and Klebsiella species, which are already a global concern24. Furthermore, the frequent recurrence of UTI symptoms observed in this study may indicate suboptimal antibiotic selection, incomplete treatment courses, or emerging resistance profiles. These findings emphasise the urgent need to expand diagnostic infrastructure for routine urine culture and sensitivity testing in Ghanaian health facilities to ensure evidence-based prescribing.
Prescriber type and appropriate/inappropriate prescribing
The study identified differences in prescribing behaviour among prescribers. Pharmacy technicians, nurses, and non-physician prescribers significantly influence overall antibiotic dispensing patterns, often without explicit diagnostic confirmation or adherence to standard treatment guidelines. The results reveal a structural gap in antibiotic governance and clinical oversight. Inappropriate prescribing, including selecting antibiotics without culture evidence or using incorrect dosing regimens, directly affects both treatment effectiveness and the broader issue of antimicrobial resistance25.
The strong link between prescriber type and inappropriate medication prescribing—particularly the higher risk among registered nurses—supports new developments in clinical practice and highlights ongoing concerns about the accuracy of non-physician prescribers. To enhance prescribing quality, targeted educational initiatives and supervision are crucial, as the finding that registered nurses are more than 12 times as likely as medical officers to prescribe inappropriately demonstrates20.
These findings are supported by recent research. For instance18, found that nurses prescribing in primary care settings often lack sufficient pharmacology training, resulting in a higher rate of inappropriate prescriptions23. Prescription errors occur more frequently among non-physician prescribers, especially when there is limited ongoing training or supervision, according to a 2022 systematic review19. Based on these studies, the risks associated with nurse-led prescribing could be reduced by improving prescriber education and implementing strict oversight.
Conversely, the absence of a significant correlation between midwives and physician assistants suggests that the supervision and training systems for these professionals may be more effective, or that their scope of practice is more specialised or restricted, thereby reducing the likelihood of incorrect prescribing26. This aligns with recent research demonstrating that non-physician prescribers can maintain high standards of medication appropriateness when provided with adequate training and clear guidelines4.
Health symptoms and health-seeking behaviour
Health-seeking behaviour among participants reflected a complex interaction between symptom perception, self-medication tendencies, and access to healthcare. A significant proportion of respondents reported consulting healthcare professionals only after experiencing symptoms for three months, indicating delays in receiving appropriate care. Conversely, self-treatment and direct visits to pharmacies were common, especially for recurrent infections and mild urinary discomfort. This behavioural pattern aligns with previous Ghanaian studies that show up to 60% of women with urinary complaints start treatment without laboratory confirmation27,28,29.
These symptoms align with research conducted in 2020, Durkin et al. (2018), which emphasised the ongoing public health importance of urinary complaints by reporting similar symptom prevalence among women in urban communities25. The chronic nature of these symptoms — with 60.2% reporting that their symptoms have lasted for three months or more — is particularly noteworthy. A 2025 study by26 found that chronic urinary symptoms often stem from delayed diagnosis or treatment gaps, leading to recurrent infections and a reduced quality of life. This extended duration highlights a potential deficiency in effective management19.
With over 40% reporting two UTI occurrences and 32% reporting three or more in the previous year, recurrent UTIs are also common. This high recurrence aligns with global data indicating that recurrent UTIs are widespread and pose significant clinical management challenges30. The recurrent nature of these infections in this population is emphasised by the fact that only 27.3% experienced a single UTI occurrence. Furthermore, 66.5% of individuals have sought medical advice regarding urinary issues, reflecting a high level of health-seeking behaviour. This demonstrates a considerable awareness or concern about urinary health, but the 23.9% who did not seek care and the 6.0% who were unsure highlight persistent barriers to accessing healthcare.
Alternatively, awareness corresponds with the findings of28, which identified informational and socioeconomic barriers as key determinants of healthcare utilisation for urinary issues29. Lastly, more than half of the respondents (52.4%) believe that lifestyle factors are responsible for their poor health, which may influence their adoption of preventive measures. This view aligns with recent studies indicating that health beliefs significantly influence health-related behaviours, such as seeking medical attention and implementing preventative measures30.
Personal hygiene and urogenital health practices
Personal hygiene practices are crucial in influencing the occurrence and recurrence of UTIs. Most participants reported practising regular genital washing, yet some habits—such as using harsh detergents, wearing tight clothing, or poor wiping techniques—may increase the risk of ascending infections. The link between hygiene and urogenital health observed here supports findings from other West African studies that associate inadequate genital hygiene with bacterial colonisation of the perineal area22,23.
Essential insights into participant behaviours and attitudes regarding medical procedures, hygiene practices, and reproductive health can be gained from the data. A significant majority (64.1%) reported using contraceptives or spermicides, indicating active involvement in family planning and reproductive health management. This aligns with current research emphasising the importance of contraceptive use in managing reproductive health outcomes. For example, a study by31 shows that contraceptive use varies with access and educational level but remains high in specific populations32. The fact that approximately one-third (34.9%) do not use these methods highlights ongoing gaps in contraceptive coverage and potential areas for targeted health education.
Only 17.5% of participants reported undergoing a medical procedure, suggesting that, while these invasive procedures are not widespread, they remain significant for a segment of the population. The overall health status of the population or access to specialised interventions may explain the low percentage. Participants’ opinions on personal hygiene products are also important. The finding indicates positive attitudes towards personal hygiene as a preventive measure that more than 60% (61.4%) believe that using hygiene equipment helps manage genital or urinary health issues; however, efficacy scores are lower.
A significant proportion (28.5%) considers the equipment only moderately effective, 28.7% very effective, and 42.8% effective. These views align with research showing that, although hygiene practices are vital, their perceived effectiveness depends on user habits and equipment quality32. This suggests that upgrading hygiene equipment and educating users on proper utilisation could enhance both perceived and actual effectiveness.
Clinical symptoms and conditions
Infectious or abnormal reproductive health conditions are found in the general population. The significance of comprehensive sexual and reproductive health services is highlighted by the high frequency of abnormal discharges and related odours, which may signal genital infections or other sexually transmitted infections. Although external dermatological lesions are relatively uncommon (12.4%), their occurrence warrants further investigation into underlying causes, including environmental factors, infectious agents, and hygiene practices. A study by Bilsen et al.33 reported similar findings, suggesting that although less common, dermatological issues on exposed body parts may be associated with infections or poor hygiene.
Urinary health issues are common in this community, as shown by the high rates of urinary tract infections, especially cystitis (67.1%) and pyelonephritis (64.7%). These numbers align with global data indicating that urinary tract infections rank among the most common bacterial infections, particularly in women of reproductive age34. With half of the participants experiencing recurrent issues, recurrence rates underscore ongoing challenges and the need for effective management and prevention strategies. Pregnancy complications were also reported by nearly 30% (29.9%), possibly due to infections, inadequate prenatal care, or other medical conditions. This supports research emphasising the importance of prenatal monitoring in reducing pregnancy-related adverse outcomes, such as those outlined by34.
The high prevalence of abnormal genital discharges (79.7%) and foul odour (65.1%) indicates a significant burden of reproductive tract infections and other conditions, such as bacterial vaginosis or sexually transmitted infections. These findings emphasise the need for targeted interventions, health education, and easily accessible diagnostic services to improve reproductive health outcomes in this population.
Low diagnostic testing
The study revealed an alarmingly low rate of diagnostic testing before antibiotic prescribing. This diagnostic shortfall has major effects on clinical accuracy, patient safety, and the durability of antimicrobial effectiveness. Relying solely on symptoms like dysuria, frequency, and pelvic discomfort promotes empiric treatment, where antibiotics are given without microbiological evidence of infection.
Empirical prescribing, while sometimes necessary in low-resource settings, can result in the overtreatment of non-bacterial conditions such as fungal vaginitis or inflammatory disorders, exposing patients to unnecessary antibiotics and adverse drug effects33,34. Moreover, it limits the ability to detect resistant organisms early, thereby undermining infection control efforts.
The lack of point-of-care diagnostic capacity in primary healthcare facilities worsens this problem. Improving laboratory infrastructure and incorporating affordable, rapid diagnostic tools into routine practice are vital steps towards sensible antibiotic use (35,36). Investing in microbiological services, particularly urine culture and antimicrobial susceptibility testing, would enable prescribers to make evidence-based decisions, improve clinical outcomes, and reduce inappropriate antibiotic exposure.
Implications of this study for public health
This study’s findings have significant public health implications, emphasising the urgent need to strengthen antimicrobial stewardship, promote rational antibiotic use, and increase access to diagnostic testing in primary care. The widespread empirical treatment practices observed raise the risk of antimicrobial resistance, jeopardising the effectiveness of current therapies. Targeted training and supervision for prescribers, alongside community education on hygiene and appropriate healthcare-seeking behaviour, are essential to reduce the recurrence of infections and safeguard population health.
Limitations of the study
This study has several limitations. Its cross-sectional design prevents causal inference. Conducting the study at a single facility limits generalisability, and reliance on self-reported data introduces potential reporting bias. The absence of antibiotic susceptibility data limited the assessment of treatment appropriateness concerning local resistance patterns. Although systematic sampling was employed, facility-based recruitment may still reflect elements of convenience sampling. Recall bias from reporting symptoms and treatment history may have introduced bias, and the lack of a control group restricts comparative interpretation. The absence of a standardised quality-of-life assessment is also a limitation of this study.
Conclusion
This study aimed to assess antibiotic utilisation patterns, prescriber practices, and associated health-seeking behaviours in the management of urinary tract infections among women of reproductive age in Ghana. This study highlights critical gaps in antibiotic prescribing practices, diagnostic testing, and health-seeking behaviours related to urinary tract infections (UTIs) among women of reproductive age. The widespread use of broad-spectrum antibiotics, particularly cefuroxime and ciprofloxacin, highlights an increasing reliance on empirical therapy without sufficient diagnostic confirmation, which could accelerate antimicrobial resistance. Variations in the appropriateness of prescriptions across different provider categories—especially between midwives, nurses, and medical officers—indicate disparities in clinical training, antibiotic stewardship awareness, and regulatory oversight. Additionally, the high symptom recurrence, along with inconsistent hygiene practices, reflects limited patient education and ineffective preventive strategies. These findings collectively emphasise the urgent need for enhanced antibiotic stewardship programmes, routine laboratory diagnostics, and ongoing professional development for prescribers. Public health initiatives should also focus on educating communities about personal hygiene, rational drug use, and timely healthcare seeking. Tackling these complex challenges is crucial for improving infection management, preserving the effectiveness of antibiotics, and supporting national efforts to combat antimicrobial resistance.
Data availability
All data generated during this study are included in this article and are available from the corresponding authors upon request.
References
Kumwenda, P. & Semu, P. Characterization of urinary tract infections among females at a tertiary hospital in malawi: a retrospective study. BMC Infect. Dis. ;25(1). (2025).
Mancuso, G. et al. Urinary Tract Infections: the Current Scenario and Future Prospects Vol. 12 (Pathogens. MDPI, 2023).
Opare-Asamoah, K. et al. Prevalence of urinary tract infections and antibiotic susceptibility patterns of bacterial isolates in first-time ANC attendees at a secondary health facility in ghana: a cross-sectional study. BMC Pregnancy Childbirth ;25(1). (2025).
Seifu, W. D. & Gebissa, A. D. Prevalence and antibiotic susceptibility of uropathogens from cases of urinary tract infections (UTI) in Shashemene referral hospital, Ethiopia. BMC Infect. Dis. ;18(1). (2018).
Amiri, F. et al. Epidemiology of urinary tract infections in the middle East and North Africa, 1990–2021. Trop. Med. Health ;53(1). (2025).
Vietinghoff, S. et al. The Global Burden of Antimicrobial resistance – urinary Tract Infections Vol. 39, p. 581–588 (Oxford University Press, 2024). Nephrology Dialysis Transplantation.
Shaker, M., Zaki, A., Asser, S. L., Sayed, I. & El Trends and predictors of antimicrobial resistance among patients with urinary tract infections at a tertiary hospital facility in Alexandria, egypt: a retrospective record-based classification and regression tree analysis. BMC Infect. Dis. ;24(1). (2024).
Karikari, A. B., Saba, C. K. & Yamik, D. Y. Reported cases of urinary tract infections and the susceptibility of uropathogens from hospitals in Northern Ghana. Microbiol. Insights ;15. (2022).
Deininger, S. et al. The antimicrobial resistance (AMR) rates of uropathogens in a rural Western African Area—A retrospective Single-Center study from Kpando. Ghana. Antibiot. ;11(12). (2022).
Tandogdu, Z., Kakariadis, E. T. A., Naber, K., Wagenlehner, F. & Johansen, T. E. B. Appropriate empiric antibiotic choices in health care associated urinary tract infections in urology departments in Europe from 2006 to 2015: A bayesian analytical approach applied in a surveillance study. PLoS One ;14(4). (2019).
Mohareb, A. M., Letourneau, A. R., Sánchez, S. M., Walensky, R. P. & Hyle, E. P. Addressing Antibiotic Overuse in the Outpatient Setting: Lessons From Behavioral Economics. Mayo Clin Proc. ;96(3):537–542. (2021). https://doi.org/10.1016/j.mayocp.2020.10.033. PMID: 33673906; PMCID: PMC7944878.
Inusah, A., Quansah, E., Fosu, K. & Dadzie, I. Resistance status of bacteria from a health facility in ghana: A retrospective study. J. Pathog. 2021, 6648247. https://doi.org/10.1155/2021/6648247 (2021). PMID: 33747569; PMCID: PMC7952191.
Mohamed, H. & Elorfaly, A. The Relation between Genital Hygiene Behaviors in Women and Urinary Tract Infection in Any Period of Life: Review Article [Internet]. Vol. 97, The Egyptian Journal of Hospital Medicine. (2024). Available from: https://ejhm.journals.ekb.eg/
Rich, S. N. et al. Associations between antibiotic prescriptions and recurrent urinary tract infections in female college students. Epidemiol. Infect. ;147. (2019).
Plate, A. et al. Treatment of urinary tract infections in Swiss primary care: quality and determinants of antibiotic prescribing. BMC Fam Pract. 21 (1), 1–9 (2020).
Durkin, M. J. et al. An assessment of inappropriate antibiotic use and guideline adherence for uncomplicated urinary tract infections. Open. Forum Infect. Dis. 5 (9), 1–8 (2018).
Ejerssa, A. W., Gadisa, D. A. & Orjino, T. A. Prevalence of bacterial uropathogens and their antimicrobial susceptibility patterns among pregnant women in Eastern ethiopia: hospital-based cross-sectional study. BMC Womens Health. 21 (1), 1–15 (2021).
World Health Organization. (2019). Antimicrobial stewardship programmes in health-care facilities in low- and middle-income countries: a WHO practical toolkit. World Health Organization. https://iris.who.int/handle/10665/329404. License: CC BY-NC-SA 3.0 IGO ISBN 9789241515481 9789240003033.
Czajkowski, K., Broś-Konopielko, M. & Teliga-Czajkowska, J. Urinary tract infection in women. Przeglad Menopauzalny. 20 (1), 40–47 (2021).
Abou Heidar, N., Degheili, J., Yacoubian, A. & Khauli, R. Management of urinary tract infection in women: A practical approach for everyday practice. Urol. Ann. 11 (4), 339–346 (2019).
Nigussie, D. & Amsalu, A. Prevalence of uropathogen and their antibiotic resistance pattern among diabetic patients. Turk. Uroloji Dergisi. 43 (1), 85–92 (2017).
Islam, M. A. et al. Prevalence, etiology and antibiotic resistance patterns of community-Acquired urinary tract infections in Dhaka, Bangladesh. PLoS One. 17 (9 September), 1–13 (2022).
Frances Edwards, A. & MacGowan Emily Macnaughton. Antimicrobial therapy: principles of use. Med. Volume. 49 (Issue 10), 624–631. https://doi.org/10.1016/j.mpmed.2021.07.005 (2021). ISSN 1357–3039.
Magill, S. S. et al. Assessment of the appropriateness of antimicrobial use in US hospitals. JAMA Netw. Open. ;4(3). (2021).
Gharbi, M. et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all cause mortality: population based cohort study. BMJ (Online). 364, 1–12 (2019).
Aggarwal, N., Leslie, S. W. & Recurrent Urinary Tract, I. Jan 20. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 32491411. (2025).
Majumder, M. M. I. et al. Antibiotic resistance pattern of microorganisms causing urinary tract infection: a 10-year comparative analysis in a tertiary care hospital of Bangladesh. Antimicrob. Resist. Infect. Control. 11 (1), 1–8 (2022).
Vicar, E. K. et al. Urinary Tract Infection and Associated Factors among Pregnant Women Receiving Antenatal Care at a Primary Health Care Facility in the Northern Region of Ghana. Int J Microbiol. ;2023. (2023).
Chen, Y., Bruning, E., Rubino, J. & Eder, S. E. Role of female intimate hygiene in vulvovaginal health: global hygiene practices and product usage. Women’s Health. 13 (3), 58–67 (2017).
Das, P. et al. Menstrual hygiene practices, WASH access and the risk of urogenital infection in women from Odisha, India. PLoS One. 10 (6), 1–16 (2015).
Nkamedjie Pete, P. M., Mabvouna Biguioh, R., Bita Izacar, A. G., Béchir Adogaye, S. & Ben, Nguemo, C. Genital hygiene behaviors and practices: A cross-sectional descriptive study among antenatal care attendees. J. Public. Health Afr. ;10(1). (2019).
Rodriguez-Mañas, L. Urinary tract infections in the elderly: A review of disease characteristics and current treatment options. Drugs Context. 9, 1–8 (2020).
Bilsen, M. P. et al. Definitions of urinary tract infection in current research: A systematic review. Open. Forum Infect. Dis. 10 (7), 1–8 (2023).
Johny, V. F., Menon, V. T. K., Georgy, S., Saju, C. R. & Jini, M. P. Prevalence of recurrent urinary tract infections and its associated factors in female staff of reproductive age group in a medical college in central kerala: a cross-sectional study. BMC Infect. Dis. ;25(1). (2025).
Ministry of Health, Ghana. Standard Treatment Guidelines (7th ed.). Accra, Ghana: Ministry of Health. (2017). Retrieved from https://www.moh.gov.gh/
Acknowledgements
The authors wish to thank all the participants and staff of St. Edwards Hospital, Adugyama, Ghana.
Funding
This study did not receive any funding from funding agencies.
Author information
Authors and Affiliations
Contributions
HOA and NA conceptualised the overall study, including its goals and aims. AJB, ASU, and PKA retrieved the necessary data from databases. HOA and AJB authored the study’s background section and contributed to the data analysis. HOA, NA, and AJB played key roles in the design of the methodology. HOA and AJB contributed to writing the discussion. NA, ASU, and PKA assisted with manuscript writing, review, and editing. HOA, ASU, and PKA carried out the data analysis. All authors contributed significantly to critical revision and approved the final version before submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The Institutional Review Board (IRB) of Sunyani Technical University granted ethical approval. Furthermore, permission was obtained from the selected hospital and St. Edward’s Catholic Hospital to conduct the research. Throughout the study, participant anonymity and confidentiality were upheld.
Consent to participate
All participants provided their informed consent after being fully briefed on the study’s aims, methods, potential risks, and benefits. Informed consent was obtained from parents and legal guardians of participants below 18 years who met the inclusion criteria.
Consent to publish
Not applicable.
Clinical trial number
Not Applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Addo, H.O., Barimah, A.J., Usman, AS. et al. Utilisation of antibiotics in the management of urinary tract infections among women of reproductive age at a district hospital in Ghana. Sci Rep 16, 3842 (2026). https://doi.org/10.1038/s41598-025-33884-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-33884-w